Abstract
Idiopathic cecal ulcer or solitary cecal ulcer is a rare entity that can only be diagnosed by histopathological evaluation. Generally, it is diagnosed by histolopathological evaluation of biopsy specimens obtained by colonoscopy that is performed for lower gastrointestinal bleeding. It can also be diagnosed after surgical resection performed for acute abdomen or cecal mass mimicking malignancy. Cecal carcinoid tumor is a rare cause of this condition; however, coexistence of cecal ulcer and appendix carcinoid tumor has not been previously reported. In this case, we present a 73-year-old woman who clinically presented as acute appendicitis with cecal wall thickening, underwent right hemicolectomy and was subsequently diagnosed with cecal ulcer, serosal abscess and coexisting appendix carcinoid tumor.
Keywords: Abscess, appendicitis, carcinoid tumor, idiopathic cecal ulcer
INTRODUCTION
Idiopathic cecal ulcer (ICU) was first described in 1832 by Cruveilhier (1). Today, referred to as solitary cecal ulcer, this disease is often reported in the form of case reports or limited case series. Thus, it is not usually kept in mind in the differential diagnosis of right lower quadrant pain or acute appendicitis. Surgery is inevitable in case of perforation, massive lower gastrointestinal bleeding or a clinical suspicion of malignancy (2, 3). Although resection of the ulcerated area (wedge resection) is adequate, most surgeons perform hemicolectomy to rule out malignancy (4).
Herein we present the coexistence of idiopathic cecal ulcer and incidental appendix carcinoid tumor that clinically presented as acute appendicitis and mimicked malignancy by forming a mass image with subserosal abscess formation in the cecum wall.
CASE PRESENTATION
A 73-year-old woman presented with right lower quadrant pain for the past three days. Her past medical history was uneventful. On physical examination, her general condition was good, she was cooperative and oriented, with an arterial blood pressure: 110/65 mm-Hg, pulse: 85 beats/min, temperature: 37.3° C. She had right lower quadrant tenderness as well as guarding and rebound tenderness. Laboratory values revealed WBC: 15.4×103/mL, hemoglobin 10.9 g/dL, normal routine biochemistry panel, and a C-reactive protein: 8.8 mg/dL (0 to 0.35). Abdominal ultrasonography showed increased wall thickness in the cecum and aperistaltic bowel loops extending medially from the cecum of 9 mm diameter and appendicolith. Abdominal computerized tomography revealed similar findings with ultrasound. Based on cecal wall thickening, an appendix diameter of 9 mm, the heterogeneous appearance of the peri-cecal fatty tissue, and the presence of minimal free fluid the radiologic diagnosis was reported as plastron appendicitis or malignancy (Figure 1). The patient underwent colonoscopy to evaluate her cecal wall thickening, however, the procedure could not be completed due to insufficiency of colon cleansing. Carcinoembryonic antigen levels and other tumor markers were within normal limits. Due to the patient’s ongoing clinical acute abdomen signs she underwent surgery after colonoscopy. An infraumbilical midline incision was used to enter the abdomen. The appendix was found to be normal, but a 3×3 cm mass was palpated on the anti-mesenteric border of cecum, thus it was decided to proceed with right hemicolectomy and a side-to-side ileotransversostomy. The resection and anastomosis were completed successfully, the right paracolic area was drained and the operation was terminated. The cut-surface of the resection specimen showed an inflamed mucosa and a cecal mass that originated from the serosal wall (Figure 2). After surgery, the patient was admitted to the intensive care unit. She was started on clear liquid diet on the 3rd day of surgery and was transferred to the ward. The diet was progressed to soft diet on the 4th day and the drain was withdrawn, and she was discharged on the 6th day. The pathology report of the resection material showed a 0.5 cm cecal ulceration 1.5 cm away from the appendix orifice along with serosal inflammation of 2.5 × 2.5 × 1.5 cm that showed ulceration and abscess formation, there were no signs of cytomegalovirus (CMV). The appendix was reported to have a distally located, 0.3 cm grade 1 (WHO, 2010) neuroendocrine tumor (carcinoid) without serosal or vascular or perineural invasion. The patient is being followed up uneventfully at the 6th postoperative month.
Figure 1.
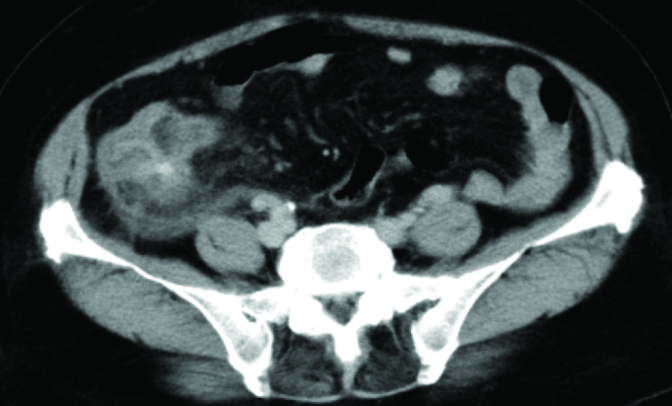
Cecal wall thickening on abdominal tomography
Figure 2. a–d.
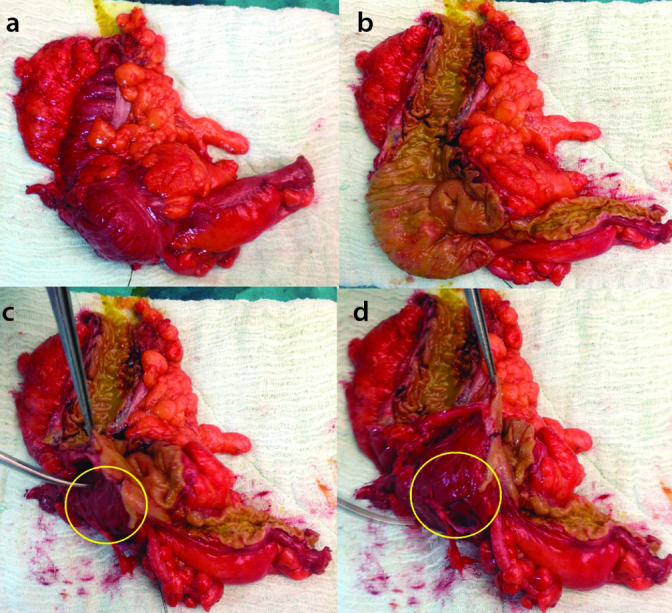
Right hemicolectomy specimen. (a) Resection material. (b) Mucosal appearance. (c,d) Antimesenteric, subserosal mass
DISCUSSION
Benign colonic ulcers are often seen in the cecum and its incidence is increasing parallel with the widespread clinical use of colonoscopy. It has been reported to occur more frequently over fifty years of age and regardless of gender, in hemodialysis or renal transplant patients (5). Although its etiology is unknown, association with infections (CMV), drugs (non-steroidal anti-inflammatory, oral contraceptive drugs), malignancy (adenocarcinoma, cecal carcinoid), ischemia, and cecal diverticulum have been reported (2, 6). Lesions are often 2 cm away from the ileocecal valve at the anti-mesenteric border (5, 6). In our case, the ulcer location was 1.5 cm away from the appendix orifice and at the anti-mesenteric border, while a distally located 0.3 cm appendix carcinoid tumor was also detected. That is why we believe that the appendix carcinoid tumor was not responsible for the cecal ulcer.
Most patients clinically present with right lower quadrant pain mimicking acute appendicitis, as in our case (2, 6, 7). Subserosal abscess formation is a complication of the ulcer and may mimic malignancy by cecal wall thickening, similar to our case.
Definitive diagnosis is achieved by detecting fibrous necrotic granulation tissue including inflammatory cells that are markers of acute or chronic inflammation such as lymphocytes, fibroblasts, plasma cells, and eosinophils on histopathologic examination of the colonoscopic biopsy or resection material. The presence of fibrin thrombus in mucosal and submucosal blood vessels support the hypothesis of localized ischemia (2).
The role of surgery in the treatment of idiopathic cecal ulcer is determined by the clinical situation. Surgery is inevitable in the presence of acute abdomen, peritonitis, uncontrolled bleeding, perforation and suspicion of malignancy. Due to the difficulty in distinguishing between benign and malignant ulcers, most surgeons perform right hemicolectomy. Limited resection with frozen section evaluation is another option (2, 5). Surgery was indicated due to acute abdomen in our patient, and since there was a palpable mass in the cecum wall and the operation was being performed at a time when frozen section evaluation could not be done, we performed right hemicolectomy. The patient was operated on with a preliminary diagnosis of acute appendicitis, and the appendix appeared macroscopically normal during surgery. However, pathological examination of the resected material revealed an incidental 0.3 cm distal appendix carcinoid tumor. Both these pathologies have been addressed with a right hemicolectomy.
CONCLUSION
It should be kept in mind that idiopathic cecal ulcers and ulcer related serosal abscess formation may mimic cecal malignancy in patients with cecum wall thickness. Carcinoid tumors of the appendix can synchronously occur in patients with idiopathic cecal ulcer.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - V.İ.; Data Collection and/or Processing - S.K.; Analysis and/or Interpretation - B.B.; Literature Review - S.K.; Writer - V.İ.; Critical Review - B.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Cruveihier J. Un beau cas de cicatrisation d’un ulc’ere de l’intestin grele datant d’une douzine d’ann’ ees. Bull Soc Anat. 1832;7:102–104. [Google Scholar]
- 2.Chi KD, Hanauer SB. Benign solitary cecal ulcer: a case report and review of the literature. Dig Dis Sci. 2003;48:2207–2212. doi: 10.1023/b:ddas.0000004527.77947.fd. https://doi.org/10.1023/B:DDAS.0000004527.77947.fd. [DOI] [PubMed] [Google Scholar]
- 3.Atila K, Güler S, Gönen C, Sarıoğlu S, Bora S. Benign solitary cecal ulcer: a condition that mimics plastron appendicitis. Ulus Travma Acil Cerrahi Derg. 2010;16:579–581. [PubMed] [Google Scholar]
- 4.Shallman RW, Kuehner M, Williams GH, Sajjad S, Sautter R. Benign cecal ulcers. Spectrum of disease and selective management. Dis Colon Rectum. 1985;28:732–737. doi: 10.1007/BF02560292. https://doi.org/10.1007/BF02560292. [DOI] [PubMed] [Google Scholar]
- 5.Ong J, Lim KH, Lim JF, Eu KW. Solitary caecal ulcer syndrome: our experience with this benign condition. Colorectal Dis. 2011;13:786–790. doi: 10.1111/j.1463-1318.2010.02261.x. https://doi.org/10.1111/j.1463-1318.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- 6.Ateş KB, Şahin T, Gürkaynak G, Boyacıoğlu S. İdiyopatik çekum ülseri. Turkiye Klinikleri J Med Sci. 1991;11:77–80. [Google Scholar]
- 7.Cha JM, Lee JI, Choe JW, Lee SH, Kim KY. A case report of idiopathic cecal ulcer mimicking cecal cancer. Dig Dis Sci. 2008;53:3259–3262. doi: 10.1007/s10620-008-0293-z. https://doi.org/10.1007/s10620-008-0293-z. [DOI] [PubMed] [Google Scholar]


