Abstract
One of the most important and feared complications of thyroid and parathyroid surgery is injury to the recurrent laryngeal nerve. The main reason for this type of injury is anatomical variations. Currently, nerve monitoring is being widely used to reduce complications due to the high variation rate. However, it is not being used extensively in our country, due to cost related issues. In this case, we present a left sided double recurrent laryngeal nerve.
Keywords: Double, left, recurrent nerve
INTRODUCTION
One of the most important and the most feared complications of thyroid and parathyroid surgery is recurrent laryngeal nerve injury. Recurrent laryngeal nerves are located on both sides of the trachea and just lateral to the ligament of Berry at the point where they enter the larynx (1, 2). Rarely, the inferior recurrent laryngeal nerve can be non-recurrent. This anomaly’s rate is reported as 0.6% on the right and 0.04% on the left. As a result of these variations in anatomical course, complete dissection is essential to visualize and protect the nerve (3). In this case report, we presented a patient who underwent total thyroidectomy and central neck dissection due to multinodular goiter in whom a left-sided double recurrent laryngeal nerve was identified during nerve exploration.
CASE PRESENTATION
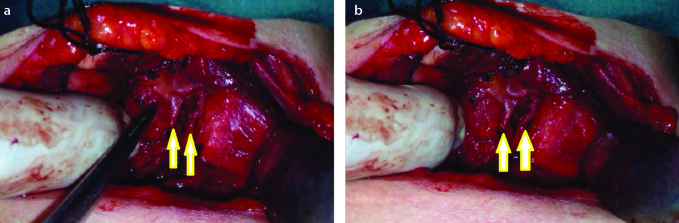
A 58 -year-old woman presented to the general surgery department due to neck swelling. She had been diagnosed with malignant melanoma 10 years ago and had undergone radiotherapy to the face and left side of the neck. Her physical examination revealed a palpable mass in the left thyroid lobe. The neck ultrasound (USG) showed a dominant, 23 × 20 mm solid, hypoechoic nodule with increased vascularity in the left lobe as well as several nodules in the right lobe, and was diagnosed as multinodular goiter. There were no lymphadenopathies. Thyroid function tests were normal, and there was no previous history of thyroiditis. Two fine needle aspiration (FNA) biopsies of the 23 × 20 mm nodule in the left lobe showed atypia of unidentified significance, and the patient was discussed at the multidisciplinary endocrinology meeting. Due to the past medical history of radiotherapy and the family history of papillary cancer in her mother, she was planned to undergo total thyroidectomy and central neck dissection. The patient underwent surgery after obtaining written informed consent and completing required preoperative preparations. During surgery, standard recurrent laryngeal nerve dissection was performed in both the right and left lobe. First the right then the left lobectomy was completed. After completion of the thyroidectomy, left central neck dissection was begun. During left central neck dissection a second recurrent laryngeal nerve was observed. It was determined that there is a left sided double recurrent laryngeal nerve abnormality (Figure 1a, b). Bilateral total thyroidectomy and central neck dissection was completed. The patient was discharged on postoperative day 1 without any complications. The pathology report revealed papillary microcarcinoma.
Figure 1. a,b.
Left-sided double recurrent nerve (the nerves are shown with arrows)
DISCUSSION
The recurrent laryngeal nerve is known to have about 30 variations (2, 4). Due to these variations, the risk of nerve injury during surgery is reported to be 1–2% even in experienced hands. That is why conducting surgery without fully observing the nerve by dissection is considered to be unsafe (5). The recurrent laryngeal nerve gives off its branches in various forms. There are many cadaver and clinical studies in this respect. The recurrent laryngeal nerve has been reported to give off 2–8 branches that are asymmetric at the right and left sides (6). The publications on branching have reported the rates of a single main branch as 0–65.8%, two branches as 52–94%, three branches as 0.8–48%, four branches as 0–25%, and five branches as 0–10% (7). Holt et al. (8) have determined that there were two or more branches in 43%, while Thompson et al. (9) have reported that 43–78% of branches originated before entering the larynx. Kratz (6) have emphasized that branching occurred before entering the larynx and that an injury is encountered mainly in this region since bleeding occurs during surgery at this site. Nemiroff et al. (10) reported the branching distance as approximately 0.6 to 4 cm from the lower border of the cricoid cartilage. Sun et al. (11) reported a 100% branching ratio in their study and stressed that the recurrent laryngeal nerve formed a ring shape in 13%. The easiest area to explore the inferior laryngeal nerve is near the lower pole where it courses close to the inferior thyroid artery. Although its dissection is more difficult, the recurrent laryngeal nerve can also be observed at the level of Berry ligament due to its fixed anatomic location (12). Rarely the recurrent laryngeal nerve is separated from the vagal nerve in the cervical region and is called the non-recurrent laryngeal nerve. A non-recurrent laryngeal nerve is detected on the right at a rate of 0.5–1% while it is rare on the left (2). These anomalies are accompanied by vascular anomalies that occur during embryonic life (1, 13).
In our case, a double recurrent nerve abnormality was detected. A second recurrent laryngeal nerve was observed during central lymph node dissection. Dissection was carried as far as the thyrotymic ligament to assess if it was a branch or a separate nerve. Both nerves were observed with their separate courses until the vagal nerve, thus they were accepted as double nerves. We wanted to prove the situation with nerve monitoring. However, the social security insurance in our country reimburses neural monitoring only in cases with proven malignancy by FNAB or recurrent operations. That is why we could not use nerve monitoring and were able to document the case by just taking pictures.
CONCLUSION
All experienced surgeons recommend a good dissection and complete visualization of the recurrent laryngeal nerve, which has many abnormalities, during thyroid and parathyroid surgery. A good dissection will reduce the risk of nerve injury to a minimum in case of double recurrent laryngeal nerve abnormality, although very rare. If possible, the use of nerve monitoring device that is currently becoming popular and being widely used in many centers will help nerve exploration and minimize the likelihood of injury (14).
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - E.M.Y.; Design - E.M.Y., B.M.; Supervision - A.E., M.B.Ö.; Funding - E.M.Y., V.M.Ö.; Materials - V.M.Ö.; Data Collection and/or Processing - V.M.Ö.; Analysis and/or Interpretation - E.M.Y.; Literature Review - E.M.Y., B.M.; Writer - E.M.Y., B.M.; Critical Review - A.E., M.B.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Hanks JB. Tiroid. In: Sabiston, editor. Textbook of surgery. 17th Edition. Nobel Tıp Kitapevleri Ltd.; Şti: 2010. pp. 947–983. [Google Scholar]
- 2.Skandalakis JE, Skandalakis PN, Skandalakis LJ. Cerrahi anatomi ve teknik. İkinci baskı, İstanbul: Nobel Tıp Kitapevi; 2000. [Google Scholar]
- 3.Kocatürk S, Yıldırım A, Kunt T. Tiroidektomide nonrekürren sinir ve klinik önemi: Bir olgu sunumu. KBB-Forum. 2004;3:89–91. [Google Scholar]
- 4.İşgör A. Tiroid hastalıkları ve cerrahisi. İstanbul: Avrupa Kitapçılık; 2000. pp. 551–581. [Google Scholar]
- 5.Sadler GP, Clark OH, Von Heerden JA. Thyroid and parathyroid. In: Schwartz SI, editor. Principles of surgery. Newyork: Mc Graw Hill; 1999. pp. 1661–1715. [Google Scholar]
- 6.Kratz RC. Vocal cord paralysis and thyroid surgery. Ann Otol Rhinol Laryngol. 1978;87:383–385. doi: 10.1177/000348947808700317. [DOI] [PubMed] [Google Scholar]
- 7.Yalçin B, Tuğcu H, Cantürk N, Ozan H. Laryngeal branching pattern of the inferior laryngeal nerve, before entering the larynx. Surg Radiol Anat. 2006;28:339–342. doi: 10.1007/s00276-006-0118-8. https://doi.org/10.1007/s00276-006-0118-8. [DOI] [PubMed] [Google Scholar]
- 8.Holt GR, McMurry GT, Joseph DJ. Recurrent laryngeal nerve injury following thyroid operations. Surg Gynaecol Obstet. 1977;144:567–570. [PubMed] [Google Scholar]
- 9.Thompson NW, Olsen WR, Hoffman GL. The continuing of technique of thyroidectomy. Surgery. 1973;73:913–926. [PubMed] [Google Scholar]
- 10.Nemiroff PM, Katz AD. Extralaryngeal divisions of the recurrent laryngeal nerve. Surgical and clinical significance. Am J Surg. 1982;144:466–469. doi: 10.1016/0002-9610(82)90425-1. https://doi.org/10.1016/0002-9610(82)90425-1. [DOI] [PubMed] [Google Scholar]
- 11.Sun SQ, Zhao J, Lu H, He GQ, Ran JH, Peng XH. An anatomical study of the recurrent laryngeal nerve: its branching patterns and relationship to the inferior thyroid artery. Surg Radiol Anat. 2001;23:363–369. doi: 10.1007/s00276-001-0363-9. https://doi.org/10.1007/s00276-001-0363-9. [DOI] [PubMed] [Google Scholar]
- 12.Friedrich T, Steinert M, Keitel R, Sattler B, Schönfelder M. Incidence of damage to the recurrent laryngeal nerve in surgical therapy of various thyroid gland diseases--a retrospective study. Zentralbl Chir. 1998;123:25–29. [PubMed] [Google Scholar]
- 13.Pisanu A, Pili S, Uccheddu A. Non-recurrent-inferior laryngeal nerve. Chir Ital. 2002;54:7. [PubMed] [Google Scholar]
- 14.Dionigi G, Bacuzzi A, Boni L, Rovera F. What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg. 2008;6:S7–S12. doi: 10.1016/j.ijsu.2008.12.023. https://doi.org/10.1016/j.ijsu.2008.12.023. [DOI] [PubMed] [Google Scholar]