Abstract
The AMIA 2003 Spring Congress entitled “Bridging the Digital Divide: Informatics and Vulnerable Populations” convened 178 experts including medical informaticians, health care professionals, government leaders, policy makers, researchers, health care industry leaders, consumer advocates, and others specializing in health care provision to underserved populations. The primary objective of this working congress was to develop a framework for a national agenda in information and communication technology to enhance the health and health care of underserved populations. Discussions during four tracks addressed issues and trends in information and communication technologies for underserved populations, strategies learned from successful programs, evaluation methodologies for measuring the impact of informatics, and dissemination of information for replication of successful programs. Each track addressed current status, ideal state, barriers, strategies, and recommendations. Recommendations of the breakout sessions were summarized under the overarching themes of Policy, Funding, Research, and Education and Training. The general recommendations emphasized four key themes: revision in payment and reimbursement policies, integration of health care standards, partnerships as the key to success, and broad dissemination of findings including specific feedback to target populations and other key stakeholders.
The AMIA 2003 Spring Congress, entitled “Bridging the Digital Divide: Informatics and Vulnerable Populations,” convened 178 experts, including medical informaticians, health care professionals, government leaders, policy makers, researchers, health care industry leaders, consumer advocates, and others specializing in health care provision to underserved populations. The primary objective of this working congress was to develop a framework for a national agenda in information and communication technology to enhance the health and health care of underserved populations. In this article, the authors summarize the societal context for the congress, the process of the congress, an ideal vision for informatics in vulnerable populations, barriers to achieving the ideal vision, and the recommendations related to policy, funding, research, and informatics education.
The societal context for the congress included vulnerable and underserved populations, digital divide, and current use of informatics innovations in underserved populations.
Vulnerable Populations
According to the Advisory Commission on Consumer Protection and Quality in the Health Care Industry, individuals are vulnerable to health care quality problems for one or more underlying reasons, including financial circumstances, place of residence, health, age, functional status, developmental status, ability to communicate effectively, race, ethnicity, and gender.1 The Commission also noted that “characteristics of the evolving health system—such as an eroding safety net—can interact with personal characteristics to contribute to vulnerability.”
Vulnerable populations often reflect diversity from a number of perspectives. Diversity is frequently defined by social and demographic characteristics such as age, gender, race, ethnicity, and socioeconomic status. The Committee on Communication for Behavior Change in the 21st Century noted the limitations of such definitions and urged communication interventions, including those that are technology based, to focus on more meaningful ways of describing heterogeneity, such as cultural process, understanding the life experiences of the communities and individuals being served, sociocultural environment, economic contexts and community resources, and commonly held attitudes, norms, efficacy beliefs, and practices related to a particular health issue.2
The term underserved population is often used synonymously with vulnerable population. However, in contrast to definitions of vulnerability that denote high risk for health care problems, underserved populations are those that specifically receive fewer health care services than required for actual or potential health care problems. The Health Resources Services Administration defines medically underserved populations as those with “economic barriers, or cultural and/or linguistic access barriers to primary medical care services.”3 Consequently, although there is considerable overlap among vulnerable and underserved populations, an individual may be vulnerable and yet not underserved (e.g., a premature African-American infant in a neonatal intensive care unit who is receiving high-quality care). However, members of consumer populations who are both underserved and vulnerable are at greater risk for adverse health outcomes and are particularly in need of health information support.
Recent reports present overwhelming evidence that health care disparities continue to exist in the United States among underserved populations, which usually include ethnic minorities, people in lower socioeconomic groups, lower educational and reading levels, rural areas, elders, and people with disabilities.4,5 Within the context of these definitions, the primary focus of the AMIA Spring Congress was on vulnerable populations that reflect broad diversity and are considered to be underserved from the perspective of health care services. A key assumption of the Spring Congress was that these vulnerable populations that typically suffer from disparities in health outcomes could be assisted by increased access to relevant health information resources and support.
Digital Divide
The term Digital Divide has typically been used to describe decreased access to information technologies, particularly the Internet, for racial and ethnic minorities, persons with disabilities, rural populations, and those with low socioeconomic status. Falling Through the Net: Toward Digital Inclusion reported that Hispanics and blacks are significantly less likely than the national average to own a computer, to have Internet access, and to access the Internet at home.6 More recently, the Pew Internet and American Life Project reported that Hispanics' use of computers (75%) exceeds that of whites (73%) and blacks (62%), although Hispanics lag slightly behind whites in Internet use (63% vs. 64%).7 Internet access is increasing at all income levels, but continues to be significantly higher for those with higher incomes. For example, 89% of households earning more than $75,000 have Internet access at home compared with 55% with household incomes less than $30,000.7 Urban use of the Internet continues to be higher than that in rural areas (65% vs. 48%).7 The number of “wired” seniors is increasing, with 22% using the Internet, and 66% of “wired” seniors have used the Internet to search for health information.8
As access has increased, other aspects of the digital divide have surfaced, e.g., computer literacy, health literacy, and mismatch between desired and available e-health services. The Children's Partnership reported that at least 50 million Americans (20%) face one or more content-related barriers to the benefits of the Internet such as lack of local information (21 million), literacy barriers (44 million), language barriers (32 million), and lack of cultural diversity (26 million).9 Of particular relevance to the topic of the Spring Congress, the IOM Committee on Health Literacy noted “health literacy comes from a convergence of education, cultural and social factors, and health services”, i.e., it is not simply a characteristic of an individual.10
Governmental agencies and cooperative partnerships are taking steps to close the gap of access to health care information and communication. National, regional, state, and medical center partnerships are evaluating the effects of information technology use on health and health care outcomes.11,12,13,14,15 However, a substantial portion of underserved populations continues to face barriers in access to or use of health information. Although digital access is rising rapidly for almost all groups, a digital divide remains for vulnerable populations most likely to be underserved. This is a significant problem that was a major focal point at the Spring Congress.
Informatics as a Strategy for Reducing Health Disparities in Underserved Populations
The IOM Committee on Quality of Health Care in the United States of America identified the critical role of information technology in designing a health system that produces care that is “safe, effective, patient centered, timely, efficient, and equitable.”16 A number of other reports identified the potential role of informatics in reducing health disparities in underserved populations. For example, elimination of health disparities is one of the major goals for the next decade identified in Healthy People 2010, and one way in which the Healthy People 2010 program strives to accomplish elimination of health disparities is by increasing access to the Internet—and therefore access to health care—to 80% of households (Objective 11-1).5 The Advisory Commission on Consumer Protection and Quality in the Health Care Industry suggested that “telemedicine and similar innovations … should be assessed as approaches for improving the access to care of those facing geographic barriers to appropriate care.”1
Projects such as Baby CareLink, the Columbia University Informatics for Diabetes Education and Telemedicine (IDEATel) Project, and the Comprehensive Health Enhancement Support System (CHESS) have demonstrated the feasibility and acceptability of e-health interventions for information and communication in populations typically considered underserved.13,15,17,18,19 Moreover, some studies have found differential benefits. For example, in a randomized trial of 246 women with breast cancer, inner city black women used CHESS as often as more affluent white women. However, the two groups used CHESS resources differently. Black women used information services more frequently and communication services less frequently than white women. The CHESS group had significantly better social support and greater information competence, and interactions with indicators of medical underservice suggested that CHESS benefits were greater for those traditionally considered underserved.19
Despite promising results from studies such as these, the use of informatics strategies to decrease health disparities in underserved populations is still in its infancy. Many knowledge gaps remain. These gaps were addressed at the Spring Congress.
Methods
Congress activities included an opening session, a dinner speaker, and plenary speakers, followed by breakout sessions and reports of breakout sessions during the closing session (▶). Breakout sessions for each track addressed the four areas: (1) issues and trends—discussion of key issues regarding the potential for information and communication technologies to improve health and provision of health to underserved populations, such as individual privacy and confidentiality concerns, literacy, and other barriers to adoption; (2) strategies—lessons learned, presentations by renowned experts who have implemented successful programs in reaching specific underserved populations for the improvement of their health and health care; (3) evaluation—presentations and discussions on methodologies for measuring the impact of informatics on improving the health of underserved populations; and (4) dissemination—exploration of efforts in deploying information and communication technologies to assist in the provision of health care to the underserved and a discussion of the issues involved in replicating these successes in other settings.
Table 1.
Topics and Speakers for Plenary Sessions
| Topic | Speaker |
|---|---|
| Consumer Empowerment | Laura Landro, Wall Street Journal |
| Health Literacy: Can Technology Help Patients Understand? | Mark V. Williams, MD, FACP, Emory University |
| Track 1: Issues and Trends | |
| Where We Are Now: Current Trends and Issues? | Holly Jimison, PhD, Kaiser Permanente Center for Health Research |
| The Ideal: What Should the Future Look Like? | Gary L. Kreps, PhD, National Cancer Institute |
| How Do We Get to the Ideal Future? | Marcy Campbell, PhD, MPH, University of North Carolina at Chapel Hill |
| Track 2: Strategies | |
| Evidence-based Approaches to Childbirth Decision-making after Cesarean: Incorporating Preferences of Different Cultures | Karen B. Eden, PhD, Oregon Health and Science University |
| Bridging the Digital Divide in the Informatics for Diabetes Education and Telemedicine (IDEATel) Project | Steve Shea, MD, Columbia University |
| The Youthbuilders Corps: Addressing the Emerging Diabetes Epidemic Among African Teens Through a Faith-based Public/Private Community Partnership Model | Sherrell M. Nicholson, American Management Systems, Inc. |
| Tribal Connections: Partnerships for Health Information Access | Sherrilynne Fuller, PhD, University of Washington |
| NLM's Strategic Framework for Bridging the Health Information Divide | Elliot Siegel, PhD, National Library of Medicine |
| Track 3: Evaluation | |
| Web-based Decision Support System to Improve Quality of Care for Vulnerable Populations: Outcomes Evaluation Perspective | Peter A. Messeri, PhD, Columbia University |
| Web-based Decision Support System to Improve Quality of Care for Vulnerable Populations: Informatician Perspective | Charles P. Friedman, PhD, University of Pittsburgh |
| Web-based Decision Support System to Improve Quality of Care for Vulnerable Populations: Humanist Perspective | Bonnie Kaplan, PhD, Yale University and Kaplan Associates |
| Track 4: Dissemination | |
| Information Technology in Virginia Health and Human Resources | Jane H. Woods, Secretary of Health and Human Resources, State of Virginia |
| Using Partnerships to Enhance Provider and Community Education Through Technology | Robyn Gabel, Illinois Maternal and Child Health Coalition |
| The Comprehensive Health Enhancement Support Systems and the Cancer Information Service: Collaboration in Progress | David H. Gustafson, PhD, University of Wisconsin |
| Funding Opportunities Panel | |
| National Library of Medicine | Milton Corn, MD |
| Robert Wood Johnson Foundation | Stephen J. Downs, SM |
| National Cancer Institute | Gary L. Kreps, PhD |
| Agency for Healthcare Research and Quality | Eduardo Ortiz, MD, MPH |
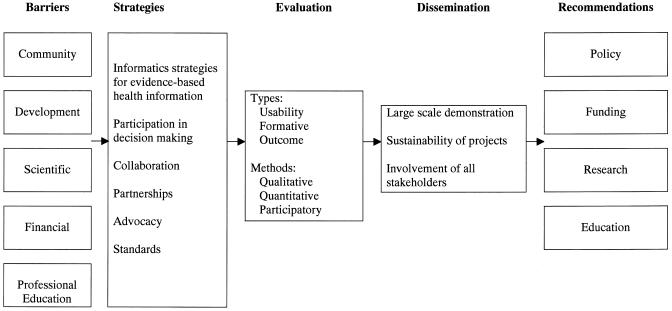
Each Breakout Track had one or two program committee members serving as coordinators in addition to three facilitators. Each track used a similar framework (▶) to guide discussions, including current status, ideal state, barriers, strategies, and recommendations. They began with a vision of an ideal state of health informatics for underserved populations and moved to identifying barriers and enablers to achieving the ideal state. These sessions ended their discussions by providing strategies and recommendations for policy, funding, research, and education for informatics communities in general and specifically for AMIA.
Figure 1.
Framework for examining informatics in vulnerable, underserved populations. This framework served as an organizing structure for the processes of the Spring Congress: (1) identification of barriers to achievement of the ideal vision; (2) generation of strategies for decreasing barriers and achieving the vision; (3) comparison of evaluation approaches that ensure that strategies and tools are congruent with community needs and incorporate rigorous and relevant methods; (4) discussion of dissemination strategies; (5) creation of recommendations for decreasing knowledge gaps and achieving the ideal vision.
Program committee members summarized results from each individual breakout session. The authors combined these results to generate major themes for visions of the ideal state, barriers to reaching the ideal state, and recommendations for addressing these barriers. Recommendations were developed related to the overarching themes of policy, funding, research, and education and training. These recommendations were divided further into general recommendations and recommendations for AMIA.
Results
Vision of the “Ideal State” of Informatics for Vulnerable Populations
Spring Congress participants envisioned that all people in the United States, regardless of literacy level, culture, functionality, or socioeconomic status, will be able to effectively use and act on health information and consumer-oriented e-health tools. The ideal state of informatics for vulnerable populations was divided into four themes: development and provision of services, access, evaluation, and informatics education.
Development and Provision of Services
All stakeholders will be involved in the development and implementation of consumer-oriented e-health tools: consumers and families; third-party payers; health care workers; community and religious leaders; librarians; educators; and technology, industry, and corporate representatives. Consumers will be involved from the beginning in determining the needs for and design of health information content and intervention strategies. All health information will be of high quality, reliable, authoritative, and up to date. Criteria for quality and accuracy of content will be based on the best available evidence, the qualification of the authors, its sponsorship, and the timeliness of the information. Providing e-health tools that contain appropriate health information will be a reimbursable service. Innovative reimbursement initiatives by private and governmental insurance systems will be established to encourage the use of technology and virtual consultations.
Access
There will be universal, private, secure, and timely access to health information and communication, decision support, and disease management tools that are evidence based, adaptive, and empowering to the individual consumer. A universally accessible national health information infrastructure will be affordable, reliable, and current with advances in technology. Health information messages will be conveyed in multiple formats (Web, journals, compact disk) using video, audio, text to voice, graphic, animation, and other communication technologies as needed in the specific situation to decrease barriers to information access and use.
Evaluation
An evaluation plan will be in place at the inception of consumer-oriented informatics interventions; designs will include mechanisms for continuous evaluation and data acquisition. Funding agencies will support outcomes research on evidence-based health information interventions. Informaticians will advance a multidisciplinary, outcomes-driven, adequately funded national program of consumer health informatics research, development, and evaluation. This program of research will identify barriers, enablers, and problems and implement strategies to overcome them. Usability testing and formative and outcome evaluation will be an integral part of the research plan. Aspects of evaluation will include cost effectiveness, sustainability, and dissemination plans.
Informatics Education
Informatics education curricula will comprehensively examine the health information needs of underserved populations and identify effective strategies for disseminating relevant health information to diverse health care consumers. Education curricula will also examine the use of interdisciplinary and community-based research strategies for addressing disparities in health care that are amenable to consumer-oriented e-health interventions.
Barriers to Reaching the “Ideal State” of Health Information Technology Access for Vulnerable Populations
Participants in the breakout sessions identified many barriers to reaching the ideal state of health information technology access for vulnerable populations. These barriers were categorized as community factors, consumer literacy, developer knowledge, field maturity, financial incentives, and professional education.
Community Factors
Understanding and incorporating community perceptions of need for health information and consumer-oriented e-health tools are critical to achieving our ideal vision. Currently, major stakeholders may not be represented in the determination of community needs and may not have incentives to implement e-health technologies such as those focused on health information. Many applications are developed without involving the community, often using information about online users obtained from biased community samples that may not be representative of underserved populations. Consequently, consumer-oriented e-health applications are not well targeted to underserved populations, and members of these communities may not be sensitive to the value of such applications in their lives. Another issue is that members of underserved populations may mistrust health care providers, health care institutions, and technology in general. This lack of trust may make these disenfranchised consumers less likely to use health information and e-health tools.
Consumer Literacy
Low computer literacy and health literacy pose barriers to accessing and using health information and consumer-oriented e-health tools.9,20 Moreover, the relationship between health literacy and health is poorly understood. Consequently, the Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association identified four significant research issues: (1) literacy screening and measurement; (2) methods of health education including those that are computer based; (3) costs and outcomes of poor literacy; and (4) understanding association between health literacy and health.21
Developer Knowledge
Developers may not understand the needs and cultures within target communities or the strategies for seeking input from members of these communities. In addition, application developers may lack the appropriate skills to translate health information for use in underserved populations. The diversity among individuals (even within specific communities) makes developing standard, uniform systems difficult.
Field Maturity
Consumer health informatics is a young science in which the scientific bases for effective informatics for underserved populations are not well articulated. Hence, there is limited evidence for usability and effectiveness in improving outcomes of consumer health informatics interventions for the underserved. There are several issues in this regard. First, ivory tower world views may be myopic and may lack commitment to reaching the ideal vision proposed in this report. There is a need to look past technology to projects that reflect important health access questions and to take advantage of cross-fertilization of various stakeholders, including those from the target community. Second, different investigators may conduct small, redundant pilot studies that do not contribute generalizable knowledge. Third, there is a lack of valid, reliable evaluation instruments. Fourth, time for evaluation often is insufficient because of length of time required to observe the effect of an informatics innovation, changes in technology, and community needs. There is also a lack of institutional understanding of issues that affect research involving underserved populations, for example, obtaining informed consent in underserved populations often requires different mechanisms in line with environment, beliefs, and perceptions.
Financial Incentives
Financial incentives to encourage the development and dissemination of health information and consumer-oriented e-health tools for the underserved are limited. To begin with, the amount of available funding for development and research is low. Second, providers lack a reimbursement structure for using or facilitating use of technology by patients. Third, informaticians, health care professionals, and others often embark on program development without a business plan for serving the disenfranchised. Finally, difficulty in finding appropriate partnerships has contributed to the lack of progress in promoting informatics for underserved populations.
Professional Education
A number of professional education factors present a barrier to achievement of the ideal vision. Informaticians typically do not receive education related to topics such as health communication, health literacy, and cultural competence. Other disciplines (e.g., health communication and health behavior, medicine, nursing, public health) may lack relevant consumer health informatics competencies. Consequently, recognition of the value of and the need for multidisciplinary collaborations may be limited.
Additional issues in educational settings are the lack of senior informatics faculty, especially those with behavioral and communications cross training, to mentor new researchers and minimal understanding of the role of informatics experts in the research process.
Successful strategies in overcoming identified barriers were discussed and incorporated in the recommendations.
Recommendations
Recommendations of the breakout sessions are summarized under the overarching themes of policy, funding, research, and education and training. An outline of the general recommendations is shown in ▶. Recommendations specific to AMIA are shown in ▶.
Table 2.
General Recommendations Related to Informatics for Underserved Populations
| Policy |
| • Create a policy of universal, lifelong health information technology for all people and associated funding for ubiquitous access |
| • Increase partnerships among many organizations |
| • Involve key community and industry members early in partnership |
| • Encourage the development of business plans for informatics programs for underserved populations |
| • Encourage the development of plans for marketing and dissemination |
| • Examine the cost and benefit of information systems serving the health needs of the underserved |
| • Involve members from community, local, state and federal organizations to identify data models that define relationships between common lay language and medical terminology |
| • Standardize mappings between various health vocabulary medical terms |
| • Examine heath information needs of underserved consumers and develop standards for meeting these needs |
| • Include appropriate data elements in data sets to capture and measure characteristics most important to conducting research in underserved populations in the National Health Information Infrastructure (NHII) |
| • Broaden the National Institutes of Health (NIH) policies to increase sensitivity to funding studies using methods for obtaining patient consent in populations that are unable to understand the traditional informed consent procedures |
| • Increase the capacity for the development of open source technology |
| • Increase NHII to address specific risks for underserved populations, as well as preventative health education networks |
| Funding |
| • Re-engineer provider financial incentives to promote patient-specific health education |
| • Fund initiatives to improve the health of the underserved |
| • Encourage collaboration among health insurance providers, health care professionals, philanthropic organizations, businesses, and the community |
| • Fund projects that incorporate evaluation methods of various appropriate designs as well as large-scale longitudinal studies and demonstration networks |
| • Include potential funders in working groups |
| • Use successful social marketing strategies to fund informatics programs addressing the needs of underserved populations |
| Research |
| • Consider the characteristics of unique populations when designing research |
| • Ensure target community representation in the planning process |
| • Coordinate collaboration and dissemination |
| • Include broad array of research designs |
| • Provide feedback to communities as part of evaluation plan |
| • Include a cost-effectiveness/cost-benefit component |
| • Increase research on natural language processing |
| • Increase research on technical standards for interoperability and access |
| Education and Training |
| • Emphasize reading and health literacy in primary level education |
| • Include an awareness of health literacy issues of patients in health care professionals' education |
| • Develop curricula and in-service training programs to sensitize health care providers to issues of health literacy |
| • Adopt anticipatory action research principles in designing a human interface for programs that would meet needs of underserved populations |
| • Develop content and formats for health information for varying literacy levels |
| • Include principles of behavioral change in health care professionals' education |
| • Include media literacy and critical thinking to judge quality of e-health information in healthcare professionals' education |
| • Develop new standards and mechanisms for quality evaluation |
| • Include research and design methods appropriate to underserved populations in graduate education of all informatics students |
Table 3.
Specific Recommendations for AMIA's Role Related to Informatics for Underserved Populations
| Policy |
| • Advocate standards to support accessible health information that is appropriate to age, language, and culture |
| • Establish priorities related to the use of informatics and communicate them to funding agencies |
| • Showcase best practices for providing relevant health information to vulnerable populations |
| • Disseminate strategies for fostering best practices to policy makers |
| • Integrate the efforts of other organizations in addressing policies related to health information for underserved populations |
| Funding |
| • Develop priorities in funding |
| • Advocate for partnership collaborations in funding |
| • Articulate the critical need for reimbursement for health informatics |
| Research |
| • Identify and advocate research priorities to appropriate organizations |
| • Encourage working groups to provide leadership in the evaluation of current standards and development of additional standards for effective e-health communication with underserved populations |
| • Expand AMIA's Web-based database focusing on underserved populations |
| • Showcase effective interventions |
| • Devote special sections of JAMIA to highlight informatics for underserved populations |
| Education and Training |
| • Incorporate as a strategic priority the inclusion of evaluation methods for the underserved in informatics educational programs |
| • Feature evaluation methods of underserved population research during a preconference |
| • Partner with other organizations to collaborate on projects and advocate for educational issues of mutual interest |
General Recommendations
Policy
Participants identified a number of policy recommendations necessary for addressing the barriers and achieving the ideal vision. First, there should be a policy of universal, lifelong health information technology for all people. As a corollary, there needs to be increased funding for ubiquitous access at current and additional locations such at libraries, churches, community centers, malls, and clinics. Because many stakeholders have an interest in improving health care information and health care in underserved populations, there should be increased partnerships among the many types of organizations (community, faith-based organizations, health care delivery, libraries, schools, industry, academia, media, advertising). Key community members and industry representatives in particular, need to be involved earlier in the partnerships than is currently practiced. Also, business plans for informatics programs for underserved populations should be encouraged. Marketing and other plans should be made for dissemination and continued funding to maintain service. Clearly, cost and benefit of the information systems serving the health needs of underserved populations should be examined closely.
Participants in the breakout sessions recognized the importance of standards for vocabularies that address the needs of underserved populations. Consumers often do not understand the terms used in health care education, and health care providers may not be knowledgeable about which terms are often misunderstood. Representatives from community, local, state, and federal organizations should be involved to identify data models that define the relationships between common lay language and medical terminology. The resulting mappings between lay terms and medical terms should be standardized, widely available, and low cost.
To ensure that data pertaining to underserved populations are addressed, the National Health Information Infrastructure (NHII) should include appropriate data elements in data sets to capture and measure characteristics most important to conducting research in underserved populations.
While procedures for informed consent and protection of privacy and confidentiality are currently in place through a number of policies and regulations, the National Institutes of Health (NIH) policies should be broadened to increase sensitivity to funding studies using methods that promote fair practices for obtaining patient consent in populations that are unable to understand traditional informed consent procedures. Creative ways of ensuring consumers' communication rights and benefits and the risks entailed in projects and programs should be developed.
Informatics infrastructure must increase to address specific risks to populations (e.g., emerging infection, bioterrorism threats, and other hazards), particularly for underserved populations that have less access to technology. At the same time, preventive health/general health education for the general population should be included.
Funding
It is critical to re-engineer provider financial incentives to promote patient-specific health education integrated into both preventive and therapeutic interventions. Online consultations need to be recognized as educational approaches (similar to “in-person”). Health information and health care using technologies should be reimbursable at the levels of providers and healthcare organizations.
Partnerships between health insurance providers, health care professionals, philanthropic organizations, businesses, and the community may find it advantageous to fund initiatives to improve the health of the underserved. While any one of these entities can contribute individually, collaboration would promote more coherent and effective health communication and less fragmentation of health care and practices for the underserved.
Funding agencies should give priority to funding projects that incorporate evaluation methods that take into account the special needs of underserved populations. Currently, there is an emphasis on randomized control trial studies as the gold standard. Funding agencies should fund pilot studies with evaluation designs that are exploratory, descriptive, correlational, and qualitative. There is also a need to fund population-based longitudinal studies and large-scale, multicenter, multistate demonstration projects such as an information technology research network.
Integrated working group meetings within organizations (e.g., AMIA, American Public Health Association) should include potential financial backers. Successful for-profit strategies should be used to fund informatics programs addressing the needs of underserved populations.
Research
Research pertaining to the information needs of underserved populations is crucial, for example, in looking at various forms in which information is acceptable and effective. Research should take into account characteristics of unique populations when designing recruitment strategies and interventions and selecting outcome measures. It is essential that researchers engage community gatekeepers in defining the need/problem to ensure that the target community is represented in the planning process. Leaders who are knowledgeable about and respected by a particular community should be invited to participate in defining community needs and designing health informatics projects. There should also be better geographical coordination of research to promote collaboration and dissemination.
Research should include a broad array of designs, including feasibility studies of theoretically driven interventions, efficacy trials of the intervention in an optimized setting, effectiveness trials in real world settings, and use of methods appropriate to the maturity of the system. Formative evaluations need to be conducted for intervention studies. Researchers should provide feedback to the community as part of the evaluation plan. Research should also, whenever possible, include a cost–effectiveness/cost–benefit component with the goal of influencing reimbursement policy.
More research needs to be conducted on natural language processing and on developing technical standards that allow interoperability and sharing of information across systems. Natural language processing is necessary for functions such as parsing consumer-generated text and linking it to relevant health information resources. Important standards that need to be considered in designing consumer health informatics applications include standards for the interoperable technologies (specifications, guidelines, software, and tools) developed by the World Wide Web Consortium (W3C) and federal standards for usability (e.g., Section 508 is a federal law that requires federal agencies to make their electronic and information technology accessible to people with disabilities). Open-source tools should be used in the development of programs for greater ease in replication and dissemination.
Education
A range of educational programs to address informatics issues in underserved populations is urgently needed. Informatics students and professionals should adopt participatory action research principles in designing human interfaces for programs that would meet the needs of underserved populations. Participatory action research is also necessary for the development of content and formats for health information that would be appropriate for varying literacy levels. For example, nontextual messages may be used in place of text in programs developed for the subset of vulnerable persons with low levels of health literacy. Furthermore, health information materials should be developed for multiple learning styles; some people are visual learners, whereas others learn better through audio messages. By the same token, different learners may prefer varying levels of abstract and concrete illustrations.
Education accreditation agencies should become more aware of literacy issues and encourage development of curricula and in-service training programs to sensitize health care providers to issues of health literacy.
Health care professionals' educational curricula should include principles of behavioral change. These principles should be evident in the way health information is implemented for patients of underserved populations. Systematic and appropriate use of “Information Prescriptions” should be part of health care practice.
Health care professional education should include media literacy and critical thinking to judge the quality of e-health information. Health care professionals, in turn, need to promote consumer education for judging the quality of Web-based health information. Considerable evidence shows that consumers need not only valid evaluation criteria but, more importantly, specific education relating to the correct utilization of criteria.22,23 Existing standards should be applied while developing new standards and mechanisms for quality evaluation.
Research and design methods appropriate to underserved populations should be included in the graduate education of all informatics students. The curriculum should include methods for assessment of program usability and computer–human interface, as well as participatory research design, measurement theory, survey research, data analysis, and other issues most appropriate to conducting research in underserved populations.
Key Themes in General Recommendations
The general recommendations emphasized four key themes: payment and reimbursement policies, health care standards, partnerships, and dissemination.
Payment and reimbursement policies must be adapted to include reimbursement for health professionals for appropriate health education and e-health tool utilization. Financial incentives should be provided to promote culturally sensitive health education as part of both preventive and therapeutic interventions. Government support through grants and other funding mechanisms should be provided to realize the commercial potential of e-health projects that are inclusive of underserved populations.
Standards should be encouraged to enable interoperability and sharing of information across systems designed for use in underserved populations. Technical standards include universal patient information data sets, personal health records, consumer health vocabulary, W3C, and 508 usability standards. The initial focus should be on enhancing awareness of existing and evolving standards.
Partnerships are the key to success. Partnerships begin with participatory action research frameworks, taking special care to involve all stakeholders in the development, conduct, and leveraging of the results of research. Beyond the primary stakeholders of consumers and their families, stakeholders include the government at all levels, corporate and other private concerns, faith-based organizations and other grass roots organizations, health care providers, and third-party payers. Public–private partnerships should be encouraged. Before embarking on health information and communication interventions or other consumer-oriented e-health tools, community and user needs should be evaluated using multidisciplinary team approaches. Approaches for health information and communication should provide for ubiquitous access at locations such as libraries, churches, and community centers. New e-health projects should be scaleable, sustainable, and disseminated widely. These criteria should be integrated into the projects before development; both formative and summative evaluations appropriate to the stage of development should be required. The economic value of developing e-health interventions for diverse populations must be evaluated.
Dissemination of results should not be limited to funding agencies and academics, but, in the spirit of participatory action research, should be disseminated through information technology to underserved populations as well. AMIA, in particular, should continue to showcase effective strategies, perhaps even in the formative stages through special poster presentations.
Projects should be local in concern, but may optimize success as large-scale, multicenter, multistate demonstration projects such as information technology networks. In addition, the public health infrastructure should increase to address new risks, such as emerging infections and bioterrorism, by including preventive health information for the general public. Support mechanisms should extend information access to populations of all generations, cultures, and economic statuses.
Training and education should be an integral part of dissemination and diffusion to develop skills in critical thinking and media literacy and to help consumers and providers assess and make good decisions on information quality. Any development should take into account diverse learning styles and user preferences for media. Nontextual messages appropriate for various print and health literacy levels should be accommodated.
Recommendations for AMIA
Policy
The results of the breakout sessions recommended that AMIA should advocate standards-making groups or organizations to create standards that support accessible health information that is appropriate to age, culture, and language. AMIA should also establish research priorities related to the use of informatics in underserved populations and communicate these priorities to funding agencies.
AMIA should take steps to determine, disseminate, and showcase the best practices for providing relevant health information to underserved populations. A range of strategies for fostering good practices should be developed and disseminated to policy makers. AMIA should also take a leadership role in integrating the efforts of other organizations such as library groups, Medical Library Association (MLA), APHA, and the Association of College and Research Libraries (ACRL) in addressing policies related to health information for underserved populations.
Funding
AMIA should play an important role in developing priorities for funding and in advocating for partnership collaborations in funding for health information and health care for the underserved. AMIA, as the premier organization for health informatics, should articulate the critical need for reimbursement for health informatics at the level of health care professionals, insurance providers, and health care organizations.
Research
AMIA has a number of mechanisms in place to promote and advocate research to support bridging the digital divide for vulnerable populations. AMIA is in an ideal position to identify and advocate research priorities to appropriate organizations and to develop and advocate for standards pertaining to informatics programs for the underserved. Working groups should be encouraged to provide leadership in the evaluation of current standards and the development of additional standards for effective e-health communication with underserved populations.
An expansion of AMIA's Web-based database should include a Web catalog for research project summaries, educational materials, and funding focusing on underserved populations. AMIA should promote mini-poster displays for special topics at meetings, as well as showcase effective tailored interventions in presentations or panels. A special issue of the Journal of the American Medical Informatics Association (JAMIA) or special sections of the Journal should be devoted to research topics highlighting informatics for underserved populations.
Education and Training
AMIA should play a vital role in the education of the informatics workforce by incorporating a strategic priority to increase content related to evaluation methods for the underserved in informatics educational programs. Possible activities include featuring evaluation methods of underserved population research during an AMIA preconference, forming an evaluation special interest group, and/or networking among the working groups. AMIA's current mechanism for coordinating efforts among working groups should include evaluation of projects for underserved populations. AMIA should partner with other organizations such as APHA, MLA, IOM, American Academy of Nursing (AAN), and others to collaborate on projects and to advocate for educational issues of mutual interest.
Conclusion
The AMIA 2003 Spring Congress provided a forum to create an ideal vision, to discuss relevant issues, and to generate a set of recommendations aimed at advancing a national agenda related to bridging the digital divide in vulnerable populations, with the goal of reducing health disparities in the underserved. The recommendations should be evaluated critically by relevant stakeholders and transformed into action by various constituencies within and outside of AMIA. It is vital that AMIA play a leadership role in closing the gap to access to health care and health information and communication for underserved populations.
Committee members Suzanne Bakken, RN, DNSc, S. Scott Brown, MPH, Thomas K. Houston, MD, MPH, Gary L. Kreps, PhD, Rita Kukafka, DrPH, MA, Charles Safran, MD, and P. Zoe Stavri, PhD, MLS are listed in alphabetical order. The views expressed do not necessarily reflect those of any U.S. agencies or institutions but rather the consensus of the participants at the meeting.
The Spring Congress was supported in part by grants from the Robert Wood Johnson Foundation, the National Library of Medicine, and the National Cancer Institute. A grant from the Pfizer Health Literacy Initiative supported Mark V. Williams' presentation on “Health Literacy: Can Technology Help Patients Understand?”
The program committee thanks the facilitators for the breakout sessions: Margaret Cashen, Jonathan Crossette, Karen B. Eden, Ben S. Gerber, Denise Goldsmith, Kenneth W. Goodman, John Holmes, Deborah A. Lewis, David R. Little, Linda Neuhauser, Daniel Z. Sands, Laura Schopp, and Lisa A. Sutherland.
References
- 1.Advisory Commission on Consumer Protection and Quality in the Health Care Industry. Quality First: Better Health Care for All Americans. Available at: http://www.hcqualitycommission.gov/final. Accessed September 13, 2004.
- 2.Committee on Communication for Behavior Change in the 21st Century: Improving the Health of Diverse Populations. Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: National Academy Press, 2002.
- 3.Bureau of Health Professions, Health Resources, and Services Administration. Guidelines for Medically Underserved Area and Population Designation. Available at: http://bhpr.hrsa.gov/shortage/muaguide.htm. Accessed September 13, 2004.
- 4.Smedley B, Stith A, Nelson A, (eds). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press, 2002. [PubMed]
- 5.Office of Disease Prevention and Health Promotion. Healthy People 2010: Understanding and Improving Health. Washington, DC: Office of Disease Prevention and Health Promotion (ODPHP), United States Department of Health and Human Services, 2000.
- 6.Falling Through the Net: Toward Digital Inclusion—A Report on Americans' Access to Technology Tools. Washington, DC: National Telecommunications and Information Administration, 2000.
- 7.Horrigan J. Pew Internet Project Data Memo. Washington, DC: Pew Internet and American Life, 2004.
- 8.Fox S. Older Americans and the Internet. Washington, DC: Pew Internet and American Life, 2004.
- 9.Lazarus W, Mora F. Online Content for Low-Income and Underserved Americans: The Digital Divide's New Frontier. Santa Monica, CA: The Children's Partnership, 2000.
- 10.Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academy Press, 2004.
- 11.Kreps G. Enhancing access to relevant health information. In: Shaping the Network Society: Patterns for Participation, Action, and Change. Palo Alto, CA: CPSR, 2002.
- 12.Brennan P, Moore S, Bjornsdottir G, Jones J, Visovsky C. M.R. HeartCare: an Internet-based information and support system for patient home recovery after coronary artery bypass graft (CABG) surgery. J Adv Nurs. 2001;35:699–708. [DOI] [PubMed] [Google Scholar]
- 13.Gustafson D, Hawkins R, Boberg E, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int J Med Inf. 2002;65:169–77. [DOI] [PubMed] [Google Scholar]
- 14.Safran C. Health care in the information society. Int J Med Inf. 2002;66:23–4. [DOI] [PubMed] [Google Scholar]
- 15.Shea S, Starren J, Weinstock R, et al. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: techical implementation. J Am Med Inform Assoc. 2002;9:25–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.
- 17.Safran C. The collaborative edge: patient empowerment for vulnerable populations. Int J Med Inf. 2003;69:185–90. [DOI] [PubMed] [Google Scholar]
- 18.Starren J, Hripcsak G, Sengupta S, et al. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: technical implementation. J Am Med Inform Assoc. 2002;9:25–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gustafson D, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med. 2001;16:435–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker DW, Parker RM, Williams MV, et al. The health care experience of patients with low literacy. Arch Fam Med. 1996;5:329–34. [DOI] [PubMed] [Google Scholar]
- 21.Health literacy: Report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281:552–7. [PubMed] [Google Scholar]
- 22.Eysenbach G, Kohnler C. How do consumers search for and appraise health information on the world wide web? Qualitative study using focus groups, usability tests, and in-depth interviews. BMJ. 2002;324:573–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kreps G. Evaluating new health information technologies: Expanding the frontiers of health care delivery and health promotion. Stud Health Technol Inform. 2002;80:205–12. [PubMed] [Google Scholar]