Abstract
Objective: Patient access to their electronic health care record (EHR) and Web-based communication between patients and providers can potentially improve the quality of health care, but little is known about patients' attitudes toward this combined electronic access. The objective of our study was to evaluate patients' values and perceptions regarding Web-based communication with their primary care providers in the context of access to their electronic health care record.
Methods: We conducted an online survey of 4,282 members of the Geisinger Health System who are registered users of an application (MyChart) that allows patients to communicate electronically with their providers and view selected portions of their EHR. To supplement the survey, we also conducted focus groups with 25 patients who were using the system and conducted one-on-one interviews with ten primary care clinicians. We collected and analyzed data on user satisfaction, ease of use, communication preferences, and the completeness and accuracy of the patient EHR.
Results: A total of 4,282 registered patient EHR users were invited to participate in the survey; 1,421 users (33%) completed the survey, 60% of them female. The age distribution of users was as follows: 18 to 30 (5%), 31 to 45 (24%), 46 to 64 (54%), 65 and older (16%). Using a continuous scale from 1 to 100, the majority of users indicated that the system was easy to use (mean scores ranged from 78 to 85) and that their medical record information was complete, accurate, and understandable (mean scores ranged from 65 to 85). Only a minority of users was concerned about the confidentiality of their information or about seeing abnormal test results after receiving only an explanatory electronic message from their provider. Patients preferred e-mail communication for some interactions (e.g., requesting prescription renewals, obtaining general medical information), whereas they preferred in-person communication for others (e.g., getting treatment instructions). Telephone or written communication was never their preferred communication channel. In contrast, physicians were more likely to prefer telephone communication and less likely to prefer e-mail communication.
Conclusion: Patients' attitudes about the use of Web messaging and online access to their EHR were mostly positive. Patients were satisfied that their medical information was complete and accurate. A minority of patients was mildly concerned about the confidentiality and privacy of their information and about learning of abnormal test results electronically. Clinicians were less positive about using electronic communication than their patients. Patients and clinicians differed substantially regarding their preferred means of communication for different types of interactions.
Good communication between patients and providers is an essential component of high-quality health care. Communication between patients and providers has traditionally occurred through in-person, telephone, or paper-based encounters. The evolution of technology now allows patients and providers to communicate electronically to obtain follow-up of test results, ask questions, collect information before a visit, schedule appointments, send reminders, and renew prescriptions.
Background
Survey data demonstrate that more than two-thirds (69%) of adults living in the United States use a computer, with 51% reporting use at home, 47% reporting use at work, and 26% reporting use at a college, library, or other location.1 These computer users spend an average of 15 hours per week on their computers, with an average of six hours per week spent using the Internet. Approximately 126 million adult Americans (63% of the U.S. adult population) use the Internet, with 87% having access at home and 48% having access at work. Approximately 102 million Americans use e-mail, and 52 million use instant messaging.2 Of particular significance in health care, the number of Americans aged 65 and older who used the Internet increased by 25% to almost 10 million.3 The number of women age 65 and older who used the Internet grew faster than any other group, with an increase of 30% to 4.6 million users in 2003, whereas the number of male Internet users over 65 increased by 20% to 5 million. Those in the 55 to 64 age range increased their numbers by 15% to almost 16 million. In comparison, Americans aged 35 to 49 and 25 to 34, who represent the largest number of Internet users, only experienced year-to-year increases of 1% and 3%, respectively.3
Survey data reveal that the majority of physicians use a computer or the Internet for business or personal reasons. In a 1998 survey by the American College of Physicians–American Society of Internal Medicine, 82% of the physicians were using computers. Of these, 67% of the physicians who had the technology to connect to the Internet at home used it on a weekly or daily basis, and 69% used it at the office on a weekly or daily basis.4 In the office, 58% of physicians reported using the computer daily for e-mail, yet only 7% reported using e-mail daily or weekly to communicate with patients. At home, the findings were similar: 69% of physicians reported using the computer daily or weekly for personal e-mail, but only 2.6% reported using it to communicate with patients. In another survey conducted by the American Medical Association, 70% of physicians said they were using the Internet, whereas 25% were using e-mail to communicate with their patients.5 In a more recent survey by Harris Interactive, 93% of physicians reported using the Internet, with 87% reporting use at home, 56% in their offices, and 40% in the clinical work area.6 Fifty-five percent of practicing physicians used e-mail to communicate with professional colleagues, and 34% used e-mail to communicate with their support staff. However, only 14% of physicians used e-mail to send patient-specific clinical information (e.g., clinical consultation with another physician, prescriptions), and only 13% of physicians communicated with their patients by e-mail.
As health care continues to evolve to a more patient-centered approach, patient expectations and demands will be a major force in driving the use of electronic communication. Many patients are interested in using e-mail to communicate with their physicians and are interested in receiving online health information from their doctor's office.7,8,9 In one study, 81% of the online population said they would like to receive e-mail reminders for preventive care, 83% said they would like to receive follow-up e-mails after visits to their doctors, and 84% said they would like their doctors to be able to access and monitor their laboratory tests online.10 In addition, many of the study participants expressed frustration before, during, and after they saw their doctors. For example, 60% said they forgot to ask all their questions, 41% expressed frustration because they had to see their doctor in person to ask questions that could have been answered by telephone or e-mail, and 35% were concerned about getting through to someone who could answer their questions.
For both patients and providers, Web messaging, in which commonly occurring types of messages (such as requests for appointments) are prestructured and directed to the appropriate recipients (e.g., scheduling personnel) offers many potential advantages. The asynchrony inherent in electronic communication allows users to send and read messages at their convenience and alleviates the problem of multiple handoffs and engaging in “telephone tag.” Electronic communication also allows the user to document, track, and verify that messages were sent and received and distribute or link to educational materials and other resources. Electronic communication can also be stored electronically or printed out for personal record keeping and future referral (e.g., instructions for taking medication).
For increasing numbers of patients and providers, Web messaging linked to a patient EHR is likely to become the preferred communication channel for routine clinical communications (e.g., reporting home blood pressures and adjusting medical regimens, renewing prescriptions, managing administrative activities such as scheduling). It shares the convenience of asynchrony with standard e-mail. It can be conveniently stored as part of the patient's EHR. It has the potential to be more efficient for both patients and providers than telephone, letters, in-person visits, or even standard unstructured e-mail. It is also more secure than telephone, standard e-mail, or U.S. mail.11
There are limited data in the peer-reviewed literature on the use of electronic communication in health care. Most of these articles consist of guidelines for the use of electronic communication12,13,14; surveys on attitudes about the use of electronic communication, mostly by patients and clinicians who are not actually using electronic communication4,8,15,16,17,18,19; and patients' experiences and attitudes about having electronic access to their medical records, most of which come from the United Kingdom.20,21,22,23,24 In a recent study, Liederman et al.25 evaluated the use of Web messaging in a primary care clinic affiliated with the University of California, Davis, that involved eight clinicians, nine medical assistants, four clerical staff, 869 enrolled patients, and 238 survey respondents. More than 85% of patients were satisfied with the use of the Web-messaging system, 88% found it easy to use, 78% thought it improved access to their provider, and 79% said it was better than calling their providers on the phone. Because of the small number of clinicians involved, it is difficult to draw conclusions from their provider survey. However, 62% thought that it improved communication between them and their patients, 75% of them said that they would be “somewhat likely” or “very likely” to keep using the Web-messaging system after completion of the study, and 75% of them stated that it was important that they be reimbursed for the time spent communicating with patients online.
Despite the potential benefits of Web messaging, there are also potential drawbacks. One is that it provides a less robust means of communication, which can result in missing not only the visual/audio cues of in-person contact and audio cues of telephone calls but also the interactivity of real-time communication. This makes Web messaging less appropriate for complex and sensitive topics. For example, although Web messaging may be well suited for patients communicating with their providers about home blood pressure measurements or renewing prescriptions, it may be less appropriate for discussing complex issues such as whether a patient should undergo prostate cancer screening, informing a patient about a new chronic condition, or discussing complicated medical management issues. Other concerns include the fact that Web messaging is not appropriate for urgent medical issues, it might threaten patient privacy and confidentiality, it might disrupt current clinical workflow and increase provider workloads, it might decrease office visits and revenue, it is not reimbursed, it might expose providers to increased liability, technical infrastructure and support might be expensive and difficult to provide, and the art of medicine might be marginalized. The American Medical Association and American Medical Informatics Association have developed guidelines for e-mail communication between physicians and patients that address some of these issues.12,13,14
Despite these concerns, there is considerable interest among patients, providers, payers, and policy makers in understanding how patient access to their electronic health record (EHR) and Web messaging can be optimally integrated into health care delivery to improve safety, quality, and efficiency. In an attempt to shed light on some of these issues, we conducted a study of patients who were early adopters of a patient EHR and Web messaging to learn more about their experiences and attitudes.
Methods
Setting
The study was conducted at Geisinger Health System. Geisinger, founded in 1915, is an integrated provider network located in 31 counties of north central Pennsylvania, with 52 clinic sites, two hospitals, 600 employed physicians, and 1.5 million outpatient visits per year. The associated health maintenance organization (HMO) is the largest rural HMO in the nation. Geisinger uses an EHR from Epic Systems Corporation, called EpiCare.
System Description
The EHR was implemented in the first outpatient clinic in 1997 and gradually rolled out to the entire system, with implementation in the primary care clinics completed in June 2001. In 2001, Geisinger added a special EpiCare software application called MyChart that allows patients to view selected portions of their EHR and exchange electronic messages with their physician's practice. The application is Web based and password protected and uses secure 128-bit encryption. Using this tool, patients can do the following:
View the 25 most frequently ordered laboratory tests with an explanation of the results
Review their allergies, medications, and health care problem list
View their past and future office visits
Review their health-related histories
Send messages and queries to their providers
Request an appointment
Request prescription renewals
Request referrals
At the time of the study, patients who wanted to use MyChart filled out a registration form at their clinic and received a user ID number and a temporary password, which they changed when they logged in the first time. Although MyChart had not been marketed aggressively to patients or providers, the number of Geisinger patients using the system nearly doubled during the six-month period between November 2002 and April 2003, from 2,365 to 4,245 registered users.
Study Design
We conducted an online survey of active MyChart users who had registered, activated their account, and logged on to the system at least once since January 2001. We sent an e-mail inviting all these users to participate in the survey. The e-mail included an embedded URL link that took patients directly to the survey, which resided on the Geisinger Web site. The site contained a research consent form, which included background information on the project. The project was approved by the Geisinger and Abt institutional review boards. Respondents were blocked from sending their replies to other respondents (i.e., they could not “reply to all” when responding), and blind copying of all invitees hid the recipient list. Respondents were allowed to skip a survey question entirely or enter a response of “N/A” (not applicable). A repeat e-mail was sent to the same mailing list (approximately 2½ weeks after the first e-mail) to solicit additional responses. After 21 days, the survey was closed to new participants.
Data were collected on patient demographics; ease of use; and completeness, accuracy, and usability of the information presented in the patient views of the EHR. Except for demographic information, responses were based on a continuous scale, which ranged from 1 (hard to use or strongly disagree, depending on the question) to 100 (easy to use or strongly agree).* We also conducted an online survey of clinicians. Two types of inducements were used to increase clinician participation: two letters of invitation from their medical director and an offer of $25 for participation. Even with these inducements, the clinician survey response rate was too low for meaningful analysis, and we report the results from the clinician survey as anecdotal.
Two 90-minute focus groups were conducted with a total of 25 active users to learn about their use of the system, satisfaction, perceived problems using the system, and suggested improvements. Participants were identified as patients whose primary care provider practiced at a Geisinger clinic located in the geographic area being studied, who were registered MyChart users, who had activated their accounts at least six months before the study, and who had logged in at least once since January 1, 2001. A third 90-minute focus group was conducted with six patients who had registered but not activated their accounts within 30 days, so we could learn why they did not use MyChart. These participants met the same geographic criteria as other participants. Geisinger staff sent an e-mail invitation to all qualifying patients for whom an e-mail address was available. Those who wished to participate were given a telephone number at Abt Associates so they could initiate the call and volunteer. For privacy and confidentiality reasons, the institutional review boards thought it important that Abt staff did not have access to the names, addresses, or other identifying information of Geisinger patients until those patients had actually volunteered to participate. The institutional review boards also did not want Geisinger staff to know which patients had agreed to participate in the focus groups. Therefore, the researchers arranged for the patients to initiate contact with Abt if they wanted to participate. Volunteers were accepted until all slots were filled, with an effort made to include persons of differing ages and both genders. Each of the three focus groups was held in different communities within the Geisinger service area.
Telephone interviews were also conducted with ten Geisinger clinicians. Geisinger staff sent an e-mail invitation to all clinicians (e.g., physicians, case managers, physician assistants) who had their own patient panels and practiced in outpatient clinics where MyChart was available. Clinicians who wanted to participate were asked to contact Abt researchers in the same manner as described previously for recruiting patients. Again, this meant that Abt staff did not have access to the names, addresses, or other identifying information of participating clinicians until they initiated the call and volunteered to participate, and Geisinger staff did not know the identities of the clinicians who agreed to be interviewed. All focus group and interview participants signed consent forms before participation.
Focus groups and interviews were administered by an experienced nurse/researcher and followed structured protocols. The topics discussed in the focus groups were more extensive and detailed than the online surveys. Many of the findings from the focus groups and interviews led to modifications in Geisinger's configuration of both the patient EHR and the Web messaging function.
Results
Of 4,282 users who were e-mailed an invitation to participate in the survey, 1,421 (33%) completed the online survey. We were not able to determine how many of the 4,282 invitations were not delivered because e-mail addresses had changed, cancelled, or incorrect from the outset. We were also not able to determine how many potential respondents were unable to access the survey because they did not use a browser supported by the survey software.
Respondents' demographic characteristics are displayed in ▶. More than three-fourths of the respondents were 31 to 64 years of age, with the majority (54%) in the 46 to 64 year age group. The smallest percentage of respondents came from the 18 to 30 year age group (at the time of this study, patients younger than 18 years old could not have their own account or respond to this survey). One-third had a high school education or less, whereas more than one-fourth had at least a four-year college degree. Almost all respondents were non-Hispanic whites, reflecting the ethnically homogeneous population in the Geisinger service area. Most had been using the system for an average of four to 12 months, and most had used it more than four times during the five-month period before the survey was conducted.
Table 1.
Respondent Demographics and MyChart Use
| Age (yr) | N = 1,421 |
| 18–30 | 5% |
| 31–45 | 24% |
| 46–64 | 54% |
| ≥65 | 16% |
| Gender | |
| Male | 40% |
| Female | 60% |
| Education | |
| High school or less | 33% |
| Beyond high school, less than 4 years college | 40% |
| 4-year college graduate or beyond | 27% |
| Race | |
| White, non-Hispanic | 98% |
| Other | 2% |
| Duration of MyChart use | |
| Less than 1 mo | 6% |
| 1–3 mo | 24% |
| 4–12 mo | 53% |
| >1 yr | 17% |
| Use MyChart for* | |
| Self | 97% |
| A child | 4% |
| A parent | 2% |
| Spouse | 23% |
Percentages do not total 100% because a respondent could access MyChart for more than one person's care.
Nearly every respondent was using the patient EHR and Web messaging for their own care, but approximately 3% were using it on behalf of a spouse or parent rather than for themselves. Others used it for both themselves and another person. Among the 97% who used it for their own care, 23% also used it for a spouse and 2% for a parent. Several focus group participants said that when the husband was more computer savvy than his wife, she would often give her husband her user ID and password so he could access the system on her behalf. Although this practice raises confidentiality and privacy issues and was not encouraged by Geisinger, few physicians or patients expressed concern about this during the focus groups and interview sessions. In an upgraded version of the software, which was installed after the study, patients can assign access rights to proxy users. This allows others to assist patients while providing a clear record of who is communicating with the physician's practice.
Ease of Use
Respondents were asked how easy it was for them to use various aspects of the patient EHR and Web messaging, using the scale from 1 (hard) to 100 (easy). Respondents found the system easy to use, with average ratings in the 78 to 85 range (▶). There were few differences according to user demographic characteristics except for the fact that women consistently rated the various functions as being slightly easier to use (i.e., higher scores) than men (e.g., registration 85 vs. 80; prescription refills 82 vs. 76; e-mail 80 vs. 76, respectively). The only exception to this trend was in the ease of logging in, where no differences were noted. Virtually all respondents expressed comfort with using computers and the Internet, and most intended to use the system in the future. Focus group participants noted difficulty with using the long preassigned temporary passwords, which has since been rectified by a software upgrade.
Table 2.
Ease of Use
| Function | Mean Rating |
|---|---|
| Ease of registering | 83 |
| Ease of logging in | 83 |
| Ease of renewing prescriptions | 80 |
| Ease of e-mail first time | 78 |
| Ease of e-mail subsequent times | 85 |
Scale: 1 = hard; 100 = easy.
Information Completeness, Accuracy, and Understandability
Respondents were asked whether they were able to understand the medical information and test results in the EHR and whether their personal health information and medical histories were complete and accurate (▶). All respondents felt that they could understand their medical information and test results, with scores averaging more than 80 (of a maximal score of 100). Respondents with less formal education (i.e., those who did not finish high school) had more difficulty understanding medical information and test results than did high school graduates, but even among this group, the scores averaged above 70.
Table 3.
Completeness, Accuracy, and Understandability Ratings*
| Medical Information Understandable | Test Results Understandable | Personal Health Information Complete | Medical History Accurate | Data Confidentiality Concerns | |
|---|---|---|---|---|---|
| Age (yr) | |||||
| 18–30 (n = 71) | 86 | 81 | 69 | 82 | 25 |
| 31–45 (n = 332) | 86 | 83 | 69 | 78 | 31 |
| 46–64 (n = 735) | 85 | 83 | 64 | 75 | 31 |
| ≥ 65 (n = 216) | 80 | 80 | 65 | 74 | 24 |
| Educational level completed | |||||
| 9th grade or less (n = 6) | 78 | 75 | 72 | 81 | 38 |
| Some high school but did not graduate (n = 36) | 71 | 72 | 62 | 74 | 34 |
| High school graduate or GED (n = 404) | 84 | 81 | 67 | 78 | 34 |
| Completed business, trade, or vocational school (n = 135) | 85 | 84 | 62 | 76 | 30 |
| Some college but no degree (n = 279) | 85 | 82 | 68 | 77 | 28 |
| Completed 2-yr degree (n = 124) | 88 | 84 | 67 | 78 | 25 |
| Completed 4-yr degree (n = 162) | 87 | 86 | 60 | 73 | 23 |
| More than 4-yr college graduate (n = 203) | 84 | 84 | 61 | 71 | 28 |
| Gender | |||||
| Male (n = 539) | 83 | 81 | 66 | 77 | 28 |
| Female (n = 813) | 86 | 83 | 64 | 75 | 30 |
Scale: 1 = strongly disagree; 100 = strongly agree.
Two to five respondents did not provide their age, gender, or educational information.
Approximately one-third of respondents felt that the personal health information contained in their EHR was not complete, and approximately 25% of respondents felt that their medical history was not entirely accurate. Ratings of the completeness of personal health information and accuracy of medical histories were consistent across both genders, all age categories, and all education levels. The one exception to this was that those with the least education (9th grade or less) rated their personal health and medical information as somewhat more complete and accurate than did other respondents. During the focus-group discussions, the medication list was cited as a particularly inaccurate element of the EHR. Patients reported that outdated prescriptions continued to appear in the EHR as active, especially if an end date was not entered into the EHR by the prescribing clinician. In addition, prescriptions written by non-Geisinger providers were not captured in the EHR unless a Geisinger clinician entered them.
Although only routine laboratory test results are available online, system administrators and physicians were concerned that patients might become worried by test results that they could access online, especially if the results were abnormal, if they had not been previously discussed with a provider (either in person or by telephone), or if much time had elapsed since the physician had discussed the results with the patient. In contrast, patients were not concerned about this issue. All patients in this study were eager to have more online test results available to them. Administrators also wondered whether patients would be concerned about the confidentiality and security of their online medical information. Although approximately 30% expressed some concern, the majority of patients had little or no concern about security and confidentiality. Patients who had a high school education or less were somewhat more concerned about this issue (average rating of 34 to 38 out of 100) than were patients who had attended college (average rating of 23 to 28 out of 100).
During interviews, clinicians expressed concern about problems that could arise if patients have access to clinical notes. They believed that they needed to be frank in documenting patient problems and conditions but were concerned that the language and content of their notes could upset patients if they were able to read them. The clinicians consistently noted that care in the use of language is especially important when charting about sensitive issues such as obesity and depression.
Provider Selection Decisions
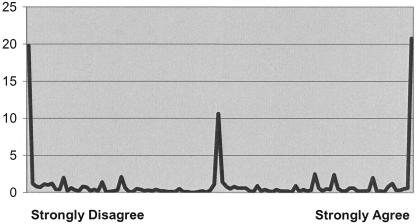
When we asked patients whether access to the patient EHR and Web messaging would be a factor in selecting their physicians, we found a trimodal distribution (▶): 20% of respondents said this system would make no difference whatsoever in their selection decision, 10% were undecided and expressed no opinion in either direction, and 20% thought that availability of this system would be a very important factor in their decision. Other responses were scattered along the continuum.
Figure 1.
Availability of system is a factor in selecting future physicians.
Communication Preferences
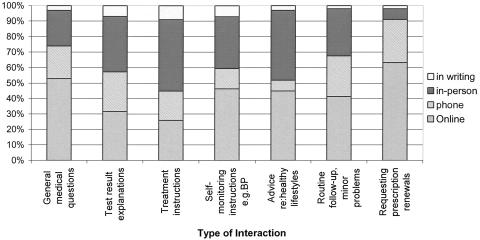
We asked patients and providers whether they prefer online, telephone, in-person, or written modes of communication for a variety of interactions ranging from general medical advice to specific queries about their treatments and test results. A majority of patients preferred online communication for renewing prescriptions and for getting answers to general medical questions (▶). They preferred in-person communication for instructions about treatment. For the other interactions, preferences for online versus in-person communication were approximately the same. They did not prefer telephone or written communication for any of the interactions, with written communication always least preferred. Patients felt that it was difficult to get through to their physician's practice and even harder to reach their physician on the telephone, while clinicians thought that “telephone tag” was extremely inconvenient for their patients and themselves. There were no clear patterns of preferred communication in terms of gender, age, or education.
Figure 2.
Communication mode preferences of patients.
We conducted a similar online survey with primary care providers (PCPs) to obtain their opinions about communication preferences for the health care interactions described previously. Only 31 of 237 (13%) PCPs responded, so the views expressed may not be representative of the majority of physicians in the health plan. ▶ lists these responses separately for patients and physicians.
Table 4.
Patient and Physician Preferences about Communication Mode
| In Writing (%) |
Telephone (%) |
E-mail/Online (%) |
In Person (%) |
|||||
|---|---|---|---|---|---|---|---|---|
| Patients | Physicians | Patients | Physicians | Patients | Physicians | Patients | Physicians | |
| Getting answers to general medical questions | 3 | 0 | 21 | 44 | 53 | 15 | 23 | 38 |
| Getting test results | 7 | 44 | 26 | 24 | 32 | 12 | 36 | 18 |
| Getting instructions about treatment | 9 | 24 | 19 | 21 | 26 | 6 | 46 | 47 |
| Getting instructions for self-monitoring (e.g., blood pressure monitoring) | 7 | 15 | 13 | 18 | 46 | 18 | 33 | 47 |
| Discussing healthy lifestyle choices | 3 | 24 | 7 | 6 | 45 | 18 | 45 | 44 |
| Routine follow-up for minor medical problems | 2 | 0 | 26 | 68 | 41 | 18 | 30 | 12 |
| Getting prescription renewals | 2 | 6 | 28 | 38 | 64 | 44 | 7 | 9 |
For every type of health care interaction, more patients than PCPs preferred Web messaging, with patient-to-PCP preference ratios in the different categories ranging from 1.5:1 to 4.3:1. In five of the seven categories, more than 40% of patients preferred e-mail communication, and at least 26% of all patients preferred e-mail communication for any of the interactions.
Other notable findings in which there was at least a twofold difference in patient and PCP preferences include the following:
68% of PCPs preferred telephone communication for routine follow-up of minor medical problems compared with 26% of patients
12% of PCPs preferred in-person communication for routine follow-up of minor medical problems compared with 30% of patients
44% of PCPs preferred written communication for providing test results compared with 7% of patients
18% of PCPs preferred in-person communication for providing test results compared with 36% of patients
44% of PCPs preferred telephone communication for providing answers to general medical questions compared with 21% of patients
Overall, PCPs preferred written communication for providing test results (44%); telephone communication for providing answers to general medical questions (44%) and routine follow-up for minor medical problems (68%); Web messaging for authorizing prescription renewals (44%); and in-person communication for providing instructions about treatment (47%), providing instructions for self-monitoring (47%), and discussing healthy lifestyle choices (44%).
Overall, patients did not prefer written or telephone communication for any category of interaction. Of these two, written communication was the least preferred in all categories, ranging from 2% to 9%. Patients preferred e-mail communication for getting answers to general medical questions (53%), getting instructions for self-monitoring (46%), routine follow-up of minor problems (41%), and getting prescription renewals (64%). They preferred in-person communication for getting test results (36%) and instructions about treatment (46%). E-mail and in-person communication were equally preferred by 45% of patients for discussing healthy lifestyle choices.
Despite survey responses indicating that PCPs preferred Web messaging for only one of the seven categories (prescription renewal), the ten clinicians whom we interviewed expressed optimism that the patient EHR and Web messaging could be a time-saver for both patients and providers. They all felt that clinicians spend too much time trying to reach patients by telephone and sending letters to patients. These clinicians expressed the hope that Web messaging would reduce the amount of time wasted on “telephone tag” and reduce the burden of sending out letters.
Limitations
Some limitations of the study should be noted. Thirty-three percent of those potentially eligible to participate in the survey did so. Although this is considered an acceptable response rate for survey questionnaires, it leaves open the possibility that the participants may not be representative of the population as a whole. Patients without access to computers with browsers other than Internet Explorer 5.x or higher would not have been able to respond to the survey. All the patient participants are early adopters of the patient EHR and Web messaging; therefore, their responses, attitudes, and preferences may not be generalizable to broader patient populations. Physician participation was also limited so that generalizations from their responses are problematic. Finally, EHRs with Web messaging may vary in content, function, and usability, and experiences with this system may not be representative of other systems.
Discussion
We believe this to be among the largest surveys ever conducted of actual users of a linked patient EHR and Web messaging. Users had very little difficulty using the system, even among adults whose education was limited to four years of high school or less. In addition, all the survey questions on ease of use and satisfaction were answered in a strongly positive manner. Given this response, we believe that use of such Web messaging systems linked to a patient EHR have the potential to not only improve the efficiency and effectiveness of health care delivery but to also serve as a market differentiator, which patients will increasingly identify as an important criterion for selecting physicians or health plans.
To realize this potential, the patient EHR must be accessible, accurate, and complete. EHRs provide an obvious advantage over paper-based records because they allow providers to access patient records anytime and anywhere as long as they are able to log into the system. However, like paper-based records, EHRs can have problems with accuracy and completeness. In our study, approximately 65% of patients rated their personal health information as complete and approximately 75% of them rated their medical history as accurate.
There are many possible reasons for this lack of accuracy and completeness: (1) information may be documented incorrectly by providers, (2) information may not be available from patients, (3) information from non-Geisinger providers may not be captured, (4) information that is not traditionally captured in the clinical encounter (e.g., alternative or complementary medical treatments) may be omitted, (5) outdated information may not be deleted, (6) old information may be removed, and (7) providers may have selectively omitted what they believed to be nonessential or sensitive information. Regardless of the reason, the more accurate and complete the medical record, the more useful it becomes for meeting the needs of both patients and providers. Use of a patient EHR linked to Web messaging can overcome some of these problems because patients will be able to identify and point out deficiencies in their health care information. In addition, the fact that patients are able to view their own medical records is likely to motivate providers to inquire and document more carefully.
Here the synergy of the patient EHR and Web messaging is particularly apparent. Without both, patients are far less likely either to note errors in their records or to bring those errors to the attention of their providers.
It is interesting to note the differences in preferences in communication channels between patients and physicians. Today, a lot of information exchange occurs between patients and providers via telephone and letters. Yet patients did not rate either of these two channels as their preferred channel for any of the seven transactions that we studied. Written communication was the least preferred, with mean scores ranging from 2% to 9%. Telephone communication was the next least favored channel for six of the seven transactions, with mean scores ranging from 7% to 28%. The only transaction in which telephone communication scored well (second most favored method) was “getting prescriptions renewed,” with a mean of 28%. However, in this category, e-mail communication was the clear favorite, with a mean of 64%. The difficulty of reaching a provider using the telephone appears to be a major contributing factor in our patients' preference for Web messaging.
In contrast, physicians preferred letters for many types of communication. Letters were the preferred channel for providing test results and the second choice for two other transactions. Some of this may stem from the fact that Geisinger's EHR makes it very easy for PCPs to generate and send letters to patients. Telephone communication was the first preference of providers for two types of transactions, and their second choice for three others.
This marked contrast in preferences for communication channels between patients and physicians has several implications. First, as alternative methods of communication continue to develop and become more readily available and easy to use, patient preferences for these alternative methods are likely to drive their adoption. Second, in the near term, these differences in preferences, coupled with the evolution of new technologies, may lead to conflicts between patients and providers, as providers struggle to achieve balance between their clinical workload, reimbursement, patient preferences, costs, and other important factors. Third, given these patient preferences and the overall positive response to the linked patient EHR and Web-messaging system, their use may provide a competitive advantage to health plans that employ such systems within the next few years. Understanding more about patient and provider adoption of Web messaging, including factors that will facilitate uptake and barriers that will need to be overcome, is an important area of our ongoing research.
Conclusion
Our study of 1,421 users of an EHR that provides Web messaging and online access to medical records found that attitudes about the use of these features were mostly positive. The majority of patients were satisfied that the medical information contained in their EHR was complete and accurate, and most patients were not concerned about the confidentiality/privacy of their medical information or about learning of test results before discussing them with their providers. Patients and physicians differed substantially in their preferred means of communication, with patients preferring e-mail communication for most interactions followed by in-person communication, whereas physicians preferred in-person communication followed by telephone communication.
The use of information technology has been identified by the Institute of Medicine as one of the four critical forces necessary to improve the quality of health care in the United States.26 Web messaging and patient access to their EHRs are two of the many important components of a comprehensive clinical information system that are still evolving. As these systems are developed and implemented, more research will be needed to determine the impact of these technologies on important outcomes and whether they lead to improvements in safety, effectiveness, efficiency, satisfaction, and overall quality of care. Patient, provider, and organizational adoption of Web messaging and other e-health services, including factors that serve as facilitators and barriers to widespread use, are important areas for future research as we attempt to optimize the integration of these technologies in health care.
Statements made in this publication do not represent the official policy or endorsement of AHRQ, the Department of Veterans Affairs, or the federal Government. Identifiable information on which this report, presentation, or other form of disclosure is based is confidential and protected by Federal Law, Section 903(c) of the Public Health Service Act, 42 U.S.C. 299 a-1(c). Any identifiable information that is knowingly disclosed is disclosed solely for the purpose for which it has been supplied. No information will be knowingly disclosed except with the prior consent of that individual. Protocols for this study were submitted to the institutional review boards of Geisinger Health System and Abt Associates Inc., and approval was obtained from both institutional review boards.
Supported by the Agency for Healthcare Research and Quality (Contract #290-00-0003).
The authors thank the Information Technology Division of Geisinger Health System for their assistance.
Footnotes
The survey was developed by Geisinger and Abt using an earlier survey instrument developed by Geisinger in 2001, which was adapted for this study. The online survey was developed using the following technologies and scripting languages: Macromedia ColdFusion MX (Web Application Environment), HTML (Hyper Text Markup Language)/DHTML (Dynamic Hyper Text Markup Language), SQL (Structured Query Language), JavaScript 1.1, Sybase Server Enterprise v.12 (database), iPlanet Enterprise Server (Web server), and Lyris Mail-List Server.
References
- 1.Harris Poll. Available at: http://www.harrisinteractive.com/news/allnewsbydate.asp?NewsID=55. Accessed Feb 7, 2000.
- 2.Pew Internet and American Life Project. Available at: http://www.pewinternet.org/reports/toc.asp?Report=106. Accessed Sept 13, 2004.
- 3.Coombes A. Retired, and more wired: older Americans ramp up Internet use; site designers have yet to catch up. CBS.MarketWatch.com. Available at: http://cbs.marketwatch.com/news/story.asp?guid=%7BE5A6935D%2D1B46%2D4252%2DB07B%2DA58C143ADC50%7D&siteid=mktw. Accessed Nov 23, 2004.
- 4.Lacher D, Nelson E, Bylsma W, Spena R. Computer use and needs of internists: a survey of the American College of Physicians-American Society of Internal Medicine. Proc AMIA Symp. 2000:453–6. [PMC free article] [PubMed]
- 5.American Medical Association. Physician internet use jumps. Available at: http://www.healthdatamanagement.com/html/PortalStory.cfm?type=trend&DID=5704. Accessed Sept 27, 2004.
- 6.Harris Interactive. Available at: http://www.harrisinteractive.com/news/newsletters/healthnews/HI_HealthCareNews2001Vol1_iss8.pdf. Accessed Feb 26, 2001.
- 7.Ferguson T. Digital doctoring—opportunities and challenges in electronic patient-physician communication. JAMA. 1998;280:1361–2. [DOI] [PubMed] [Google Scholar]
- 8.Fridsma DB, Ford P, Altman R. A survey of patient access to electronic mail: attitudes, barriers, and opportunities. Proc Annu Symp Comput Appl Med Care. 1994:15–9. [PMC free article] [PubMed]
- 9.Brown M. Consumer Health and Medical Information on the Internet. New York, NY: FIND/SVP Emerging Technologies Research Group, FIND/SVP Inc., 1996, p 46.
- 10.Taylor H, Leitman R. Study reveals big potential for the internet to improve doctor-patient relations. Available at: http://www.harrisinteractive.com/news/newsletters/healthnews/HI_HealthCareNews-V1-Issue1.pdf. Accessed Sept 28, 2004.
- 11.Mandle KD, Kohane JS. Effect of a triage-based email system on clinic resource use and patient and physician satisfaction in primary care. Proc AMIA Symp. 1999:849–53. [PMC free article] [PubMed]
- 12.American Medical Association's Guidelines for Physician-Patient Electronic Communications. Available at: http://www.ama-assn.org/ama/pub/category/2386.html. Accessed Sept 13, 2004.
- 13.Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet working group, task force on guidelines for the use of clinic-patient electronic mail. J Am Med Inform Assoc. 1998;5:104–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sands DZ. Guidelines for the use of patient-centered e-mail. [Massachusetts Health Data Consortium Web site]. Available at: http://www.mahealthdata.org. Accessed Sept 13, 2004.
- 15.Couchman GR, Forjuoh SN, Rascoe TG. E-mail communications in family practice: what do patients expect? J Fam Pract. 2001;50:414–8. [PubMed] [Google Scholar]
- 16.Sittig DF, King S, Hazlehurst BL. A survey of patient-provider e-mail communication: what do patients think? Int J Med Inf. 2001;61:71–80. [DOI] [PubMed] [Google Scholar]
- 17.Neill RA, Mainous AG 3rd, Clark JR, Hagen MD. The utility of electronic mail as a medium for patient-physician communication. Arch Fam Med. 1994;3:268–71. [DOI] [PubMed] [Google Scholar]
- 18.Kleiner KD, Akers R, Burke BL, Werner EJ. Parent and physician attitudes regarding electronic communication in pediatric practices. Pediatrics. 2002;109:740–4. [DOI] [PubMed] [Google Scholar]
- 19.Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care. Am J Manag Care. 2002;8:427–33. [PubMed] [Google Scholar]
- 20.Pyper C, Amery J, Watson M, Crook C, Thomas B. Patients' access to their online health records. J Telemed Telecare. 2002;8(suppl 2):103–5. [DOI] [PubMed] [Google Scholar]
- 21.Pyper C, Amery J, Watson M, Crook C. Patients' experiences when accessing their on-line electronic records in primary care. Br J Gen Pract. 2004;54:38–43. [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher B, Britten N. Patient access to records: expectations of hospital doctors and experiences of cancer patients. Br J Gen Pract. 1993;43:52–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Jones RB, McGhee SM, McGhee D. Patient on-line access to medical records in general practice. Health Bull (Edinb). 1992;50:143–50. [PubMed] [Google Scholar]
- 24.Masys D, Baker D, Butros A, Cowles KE. Giving patients access to their medical records via the internet: the PCASSO experience. J Am Med Inform Assoc. 2002;9:181–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liederman EM, Morefield CS. Web messaging: a new tool for patient-physician communication. J Am Med Inform Assoc. 2003;10:260–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corrigan JM, Donaldson MS, Kohn LT, editors. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001.