Abstract
Background
Child and adolescent psychopathology has been linked to increased sleep problems, but there has been less investigation of this relationship in younger samples with early-onset psychopathology. This study examined three specific but commonly observed aspects of sleep behaviors in young children-- 1. Sleep onset latency, 2. Refusal to sleep alone, and 3. Nighttime awakenings -- measured during preschool, and investigated whether these sleep problems predicted anxiety and/or depression across the next six years until school age (ages 9–13).
Methods
Data were analyzed from N = 292 participants from a prospective longitudinal study of preschool-age children (ages 3–6). At baseline, parent-reported clinical interviews of psychiatric symptoms, as well as sleep problems were conducted using the Preschool-Age Psychiatric Assessment (PAPA). Follow-up clinical interviews were also conducted annually through school-age using the Childhood and Adolescent Psychiatric Assessment (CAPA).
Results
Parent reported sleep onset latency and refusal to sleep alone were significant independent predictors of MDD and anxiety severity, but not ADHD severity across time, even after controlling for family income-to-needs ratio and maternal internalizing psychopathology. In exploratory analyses using only healthy preschoolers, parent reported sleep onset latency and refusal to sleep alone also predicted anxiety severity.
Conclusions
We demonstrate that specific, yet relatively common sleep problems predict diagnostic severity of depression and anxiety across time, but not ADHD. Increased clinical attention to and screening for sleep onset latency and refusal to sleep alone during preschool may be warranted.
Keywords: Psychopathology, longitudinal, preschool, sleep
INTRODUCTION
Recent reviews highlight concurrent, longitudinal, and bidirectional links between sleep problems and psychopathology in children (Alvaro, Roberts, & Harris, 2013; Gregory & Sadeh, 2012, 2015; Sadeh, Tikotzky, & Kahn, 2014; Tesler, Gerstenberg, & Huber, 2013). Although findings generally link psychopathology with increased sleep problems in school aged children and adolescents, there has been less investigation of younger samples, particularly those with early-onset psychopathology. This may be particularly important as sleep problems are more common in younger children and there is a need to distinguish between developmental norms and early markers of psychopathology. There is also a need for a developmentally informed longitudinal approach to the study of childhood sleep problems. Thus, the purpose of this study was to examine three specific and most commonly observed aspects of sleep behaviors in preschool aged young children (Anders & Dahl, 2007; Mindell et al., 2006) -- 1. sleep onset latency, 2. refusal to sleep alone, and 3. nighttime awakenings -- measured during preschool and to investigate whether these sleep problems predict depression, anxiety, and ADHD symptomatology across the next six years to school age.
When compared to sleep problems during later childhood, much less is known about the longitudinal psychiatric outcomes of preschool-onset sleep problems (Goodlin-Jones, Tang, Liu, & Anders, 2009). Gregory and colleagues (Gregory et al., 2005; Gregory, Eley, O’Connor, & Plomin, 2004; Gregory & O’Connor, 2002) used several large, longitudinal datasets to examine psychiatric outcomes in adolescence and adulthood among youth with preschool-onset sleep problems. Overall, their results indicated that parent-reported, preschool-onset sleep problems predicted a broad range of psychopathology during adolescence and anxiety during adulthood, even after controlling for symptoms present during preschool and later childhood. Other work also demonstrates that sleep difficulties during preschool years are predictive of later internalizing problems. Specifically, preschoolers who are poor sleepers (i.e., compared to normal and good sleepers as characterized by actigraph measurements) reported greater internalizing but not externalizing symptoms one year later (Hatzinger et al., 2014). Preschoolers characterized as having ‘persistent sleep problems’ on a caregiver-reported questionnaire exhibited greater aggression, somatic complaints, and anxious/depressed mood symptoms four years later (Simola et al., 2012).
However, these studies are limited by the use of general items to assess global sleep problems. For instance, items encompassing different sleep problems such as ‘Does your child have sleep problems?’ ‘Nightmares,’ and/or ‘Talks or walks in sleep,’ were combined into a composite variable, precluding the investigation of more specific sleep problems. Since a variety of sleep problems were combined into a single measure of global sleep disturbances, the specific types of the sleep problems that occurred during preschool are largely unknown. In addition, baseline (e.g., preschool) symptoms of internalizing and externalizing pathology were not included as control variables in several of these analyses (Hatzinger et al., 2014; Simola et al., 2012), so it is unclear whether the findings represent an increase in symptoms of psychopathology over time or a continuation of already elevated symptoms associated with poor sleep. Furthermore, past work relied heavily on self-reported symptoms of internalizing and externalizing disorders in relatively healthy community samples.
The current study addresses several of these limitations by focusing on the most commonly reported sleep problems occurring during the preschool period (Anders & Dahl, 2007; Mindell et al., 2006) in a sample with significant psychiatric illness. We chose this approach for several reasons. First, sleep onset latency is the most prevalent sleep difficulty in psychiatric samples of preschoolers, with 23% of a preschool clinical sample demonstrating difficulties falling asleep (Boekamp, Williamson, Martin, Hunter, & Anders, 2014) and a recent meta-analysis demonstrated longer sleep onset latency to be the most robust difference between adolescents with and without depression (Augustinavicius, Zanjani, Zakzanis, & Shapiro, 2014). In addition, refusal to sleep alone is one of the most common sleep disturbances in children with anxiety disorders (Alfano, Ginsburg, & Kingery, 2007) and refusal to sleep alone is often the reason children with symptoms of anxiety are brought in/referred for clinical treatment (Eisen & Schaefer, 2007). Second, recent work with toddlers highlights the predictive validity of such an approach (Sivertsen et al., 2015). Specifically, short sleep duration and nocturnal awakenings at 18-months predicted internalizing and externalizing problems at age 5, even after controlling for symptoms of internalizing and externalizing problems during infancy (Sivertsen et al., 2015).
Given that psychiatric disorders and sleep disorders are highly comorbid in children and adolescence (Gregory & Sadeh, 2012; Ivanenko & Johnson, 2008), it is imperative to understand the longitudinal relationships between specific sleep problems and psychiatric disorders, and in doing so, identify the unique predictive power preschool sleep disturbance may have on depression, anxiety, and/or ADHD. More research is needed not only on specific sleep problems occurring during preschool but also whether there is any specificity to these associations in the prediction of psychiatric diagnoses later in life. Building on findings in older children, we hypothesized that both sleep onset latency and refusal to sleep alone during preschool would predict the symptom severity of depression and anxiety across time. Given that most preschool-age children experience nighttime awakenings, we did not anticipate that this sleep behavior would predict later psychopathology. As a secondary test of our hypothesis, we also explored whether sleep onset latency, refusal to sleep alone, and nighttime awakenings would predict increases in depression and/or anxiety symptoms in a subsample of preschoolers who were healthy at the baseline assessment.
METHODS
Participants
Data from N = 292 participants in the Preschool Depression Study (PDS)(Luby, Si, Belden, Tandon, & Spitznagel, 2009) were included in this analysis. The PDS is a prospective longitudinal study of preschool-age children (N=306) designed to investigate the validation and longitudinal course of preschool depression, conducted at the Washington University School of Medicine Early Emotional Development Program in St. Louis. For the PDS, 3.0- to 5.11-year-old children and their primary caregivers were recruited from daycares, preschools, and primary care sites in the St. Louis area, using the Preschool Feelings Checklist (Luby, Heffelfinger, Koenig-McNaught, Brown, & Spitznagel, 2004) to oversample children with depression or at risk for depression. Healthy preschoolers and those with other psychiatric disorders were also included. Approximately 6000 checklists were distributed to sites between May 2003 and March 2005. In daycares and preschools, from which approximately 3/4 of sample was ascertained, checklists were handed out to all parents of children in the target age range. Checklists were made available in waiting areas of primary care settings next to a poster describing a study of early emotion development. Completed checklists were collected by the sites and returned. Using this method, N=1474 checklists were returned and those with scores of 0 (presumed healthy) or >3 (above established cut-off) were sought for participation. Among those returned N=335 were ineligible due to being out of the age range and N=240 had PFC scores out of range. The remaining N=899 met all initial screening and inclusion criteria and were contacted by phone for further screening. Based on phone screening, subjects with chronic illness, marked speech and language delays and/or neurologic or Autistic Spectrum Disorders were excluded. Those without exclusions (N=416) were invited for study participation and N=305 agreed and presented for the assessment (Luby, Belden, Pautsch, Si, & Spitznagel, 2009). Children underwent annual diagnostic and developmental assessments (i.e., approximately every 12 months). Parental consent and child verbal assent were obtained before study participation. The Institutional Review Board at Washington University approved all procedures in accordance with institutional ethical guidelines. PDS participants who met all inclusion criteria based on data quality and availability were included in the current analyses. Of the 306 children in the PDS, n=292 had complete data on all sleep variables in the current analyses
Measures
DSM psychiatric diagnoses
Trained staff conducted up to six in-person diagnostic assessments with children and their primary caregivers from study enrollment through the final follow-up assessment. Interviews were audiotaped, reviewed for reliability, and calibrated for accuracy using methods previously described (Luby, Si, et al., 2009).
Depression, anxiety, and attention deficit hyperactivity disorder (ADHD.) Severity Scores
Depression, anxiety, and ADHD severity scores (i.e., the total number of core DSM based symptoms endorsed) were created when children were preschoolers using the Preschool-Age Psychiatric Assessment (PAPA; Egger et al., 2006). Depression and anxiety severity scores when children were school age were calculated at each assessment using the Childhood and Adolescent Psychiatric Assessment (CAPA; Angold et al., 1995; Angold & Costello, 2000), which includes child-report and caregiver report of psychiatric symptoms. The depression severity score was the sum of 9 total possible depression symptoms that are used as DSM-IV Major Depressive Disorder (MDD) criteria (Luby, Mrakotsky, Heffelfinger, Brown, & Spitznagel, 2004). The anxiety severity score was the combined sum of core symptoms endorsed as part of the separation (SAD) and generalized anxiety (GAD) modules of the PAPA or CAPA. Preschool age ADHD severity scores were the total number of endorsed symptoms from the inattentive and hyperactive ADHD modules of the PAPA (Luby, Mrakotsky, et al., 2004).
Specific preschool sleep problem
Preschool sleep was assessed using three variables from the sleep module of the PAPA obtained during the baseline assessment. The first item assessed children’s reluctance to initiate sleep alone. The parent was asked, ‘Does [your child] go to sleep on his/her own?’ and ‘Does s/he need you or another adult close by while s/he falls asleep?’ with follow-up questions assessing contextual, frequency details when appropriate. The item addressed whether children require a primary caregiver in the room/in the bed before the child will fall asleep. The variable was dichotomized (0 = child falls asleep alone with no problems, or 1 = 50% of the time or greater to almost always child refuses to sleep alone unless a caregiver is present while child falls asleep). Children who refuse to sleep alone less than 50% of the time were grouped with children who fall asleep alone without problem. The coding for this question explicitly excluded sleeping in a ‘family bed’ with parents, thus excluding cultural norms of co-sleeping patterns. The second item of interest was children’s latency to sleep onset. This question asked parents, ‘Once [your child] is settled down for the night, is it hard for him/her to fall asleep? How long does it take for him/her to fall asleep?’ with follow-up questions concerning contextual and frequency details assessed when appropriate. This PAPA item assesses the average amount of time that passes from when a parent says goodnight to the child until the child falls asleep, measured in hours:minutes:seconds based on parental report. The third item of interest was children’s nighttime awakening. The parent was asked, ‘Does [your child] wake up during the night? Or does [your child] sleep through the night? Follow-up questions concerning contextual and frequency details were assessed and the item was coded dichotomously (0 = child sleeps through the night, or 1 = child wakes up during the night).’
Income-to-needs ratio
Mothers reported family income at each annual assessment. The income-to-needs ratio was computed as the total family income at baseline divided by the federal poverty level, based on family size, at the time of data collection (McLoyd, 1998).
Maternal depression and anxiety
The Family Interview for Genetic Studies (FIGS; Maxwell, 1992) assessed for the presence of psychopathology in mothers. This is a widely-used and well-validated fully structured measure of family history of psychiatric disorders. A senior psychiatrist (JLL), blind to the child’s diagnostic status, reviewed questions about the diagnostic status of mothers. This report combined the presence or absence of maternal history of depression and anxiety, coded as 0 ‘no’ and 1 ‘yes.’
Statistical Analyses
All statistical analyses were conducted using IBM SPSS 21.0 for Macintosh (SPSS, Inc., Chicago, IL). The first author and study P.I.’s had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
We analyzed change in depression, anxiety, and ADHD severity across time (e.g. using all available behavioral assessment waves) using multilevel linear mixed (MLM) models (Peugh, 2010; West, 2009) to account for intra-individual dependency due to repeated measurements across time. Each model examined the three specific preschool sleep problems (e.g., reluctance to sleep alone, sleep onset latency, and nighttime awakenings) as predictors of both the main effect and slope (rate of change) in depression, anxiety, and ADHD severity scores across time. Fixed effects were included in each MLM for age (e.g, within-individual change over time in symptom severity) and preschool sleep problems, as well as the interactions between age and preschool sleep problems. All models included family income-to-needs ratio and maternal internalizing psychopathology (depression and anxiety) as covariates. All continuous predictors were mean-centered. Random effects for the symptom severity intercept and slope for age were included to account for individual variability in mean symptoms levels and rate of change in symptoms.
As a follow up analysis and in effort to better address the specificity of the findings, we repeated the above analyses using a subsample (n = 81) of the healthy children who had no psychiatric diagnoses during the preschool period (i.e., prior to age 6). However, children could have had one or more psychiatric diagnoses once they were school age (i.e., age 6 years or older)
RESULTS
Demographic and Clinical Characteristics
Table 1 provides demographic and clinical descriptions of key demographic and clinical information used in analyses. Bivariate correlations between measures demonstrated that reluctance to sleep alone and sleep onset latency were positively correlated with each other and clinical symptoms while nighttime awakening was negatively correlated with the other sleep variables and with anxiety symptoms (see Table 2 for full correlation table).
Table 1.
Demographic and Clinical Characteristics of the Sample
| Total Sample N=292 | |
|---|---|
| Child Demographic Factors | |
| Gender; % Female (n) | 48% (145) |
| Age (years) at Baseline; Mean (SD) | 3.99 (.76) |
| Ethnicity; % Caucasian (n) | 54% (163) |
| Family Demographic Factors | |
| Family Income-to-Needs Ratio; Mean (SD) | 2.05 (1.18) |
| Maternal internalizing psychopathology %yes | 44% (132) |
| Clinical Variables | |
| Preschool Baseline | |
| MDD; % Diagnosed (n) | 25% (75) |
| MDD severity; Mean (SD) | 2.45 (1.82) |
| MDD symptom severity range | 0 to 8 |
| GAD/SAD; % Diagnosed (n) | 24% (74) |
| GAD/SAD severity; Mean (SD) | 3.21 (2.49) |
| GAD/SAD symptom severity range | 0 to 10 |
| ADHD; % Diagnosed (n) | 16% (48) |
| ADHD severity; Mean (SD) | 4.09 (4.56) |
| ADHD symptom severity range | 0 to 18 |
| Preschool Sleep Variables | |
| Time to sleep initiation (HH:MM:SS); Mean (SD) | 00:26:57 (00:36:12) |
| Refusal to sleep alone; % yes (n) | 38% (114) |
| Nighttime Awakenings %yes (n) | 61% (184) |
Note: MDD- major depressive disorder; GAD/SAD- generalized anxiety disorder/separation anxiety disorder; ADHD- attention deficit hyperactivity disorder. Clinically significant thresholds for severity scores are as follows: MDD ≥ 5, ADHD ≥ 6, GAD/SAD are combined diagnosis so a clear clinical cutoff has not been established.
Table 2.
Bivariate Correlations between Clinical and Demographic Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Age | 1 | ||||||||||
| 2.Gender | −.12 | 1 | |||||||||
| 3.Income | −.02 | − .006 |
1 | ||||||||
| 4.Preschool MDD Severity |
.12 | −.06 | − .20** |
1 | |||||||
| 5.Preschool GAD/SAD Severity |
.09 | −.07 | − .19** |
.59** | 1 | ||||||
| 6.Preschool ADHD Severity |
.05 | −.09 | − .20** |
.50** | .46** | 1 | |||||
| 7.School Age MDD Severity |
.14 | − .16* |
− .26** |
.35** | .33** | .31** | 1 | ||||
| 8.School Age GAD/SAD Severity |
.08 | −.08 | −.15* | .33** | .35** | .23** | .67** | 1 | |||
| 9. Nighttime Awakening |
.07 | −.07 | −.08 | −.09 | −.20** | −.03 | .03 | .02 | 1 | ||
| 10.Sleep Initiation (time) |
−.06 | .03 | −.16* | .36** | .31** | .21** | .29* | .18* | −.18* | 1 | |
| 11.Refusal to sleep Alone |
−.07 | −.04 | −.006 | .17* | .38** | .10 | .17* | .11 | −.17* | .14* | 1 |
Do preschool sleep problems predict school age depression and/or anxiety severity?
Depression severity at school age
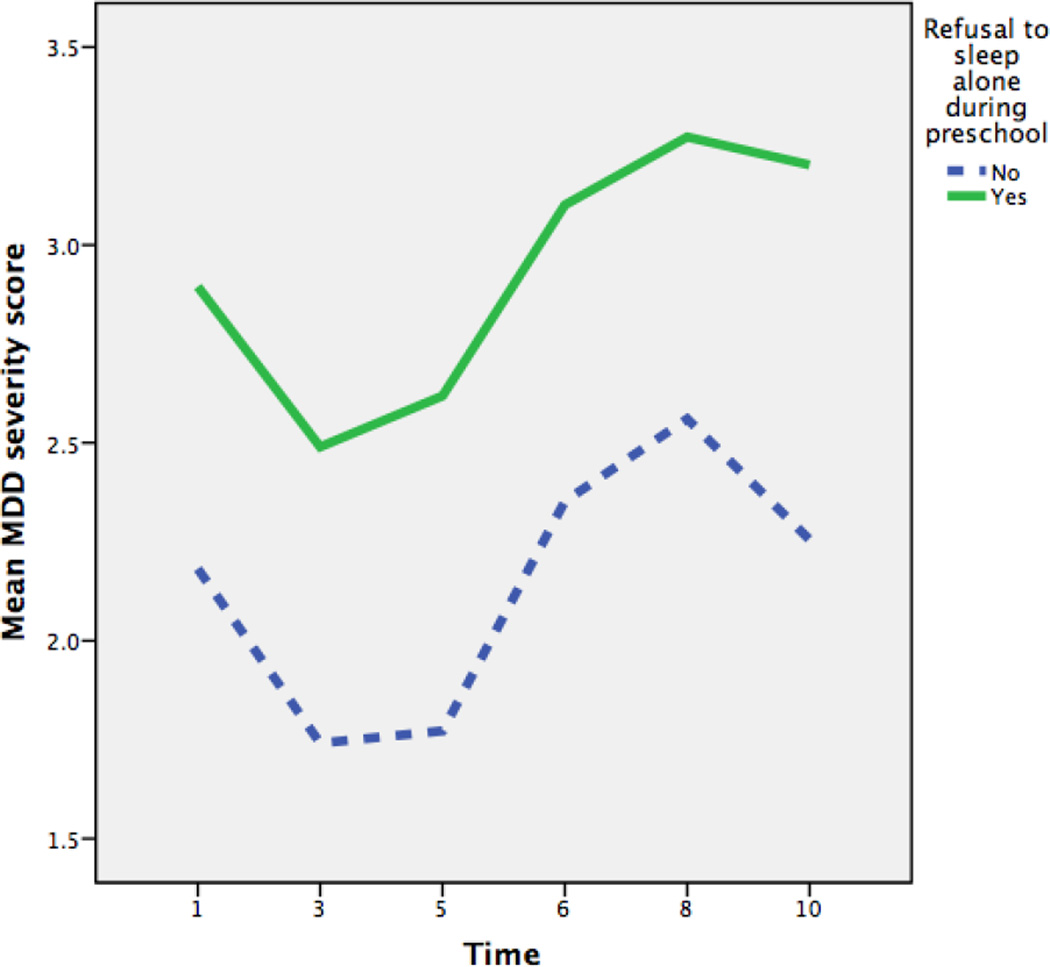
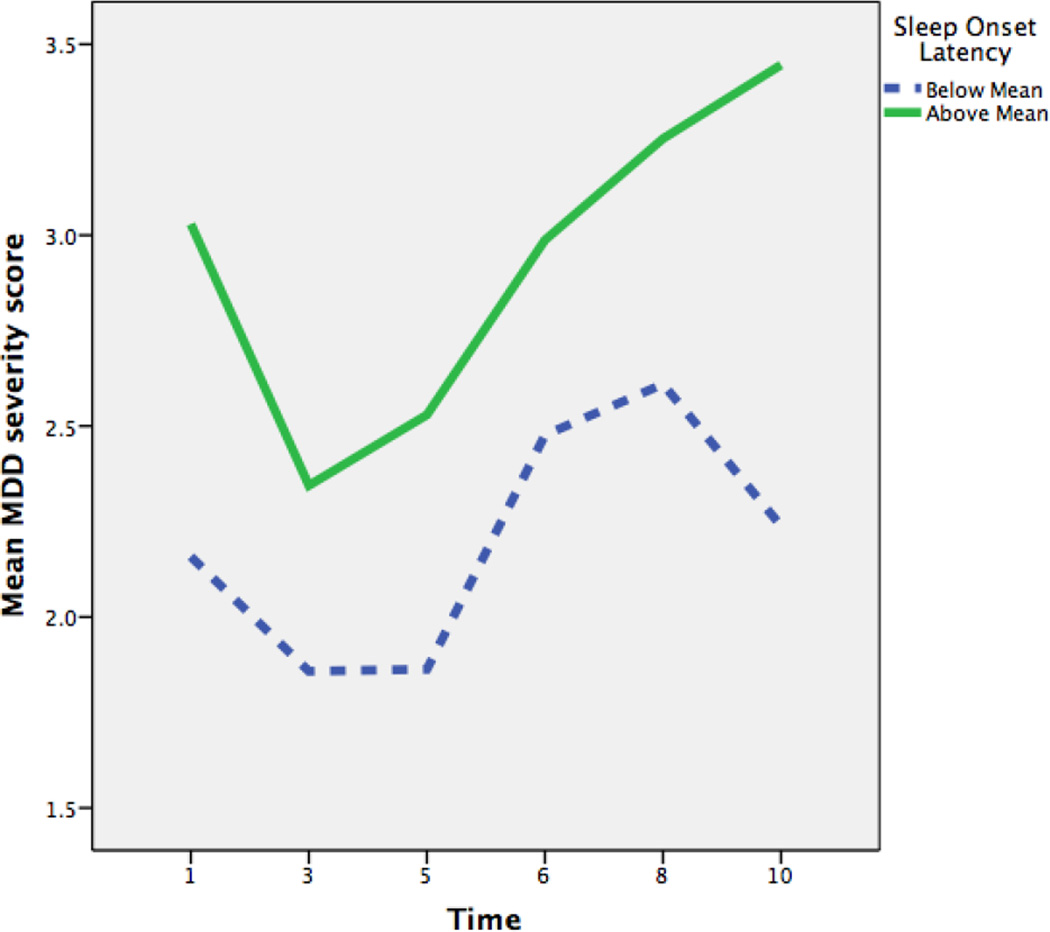
We examined reluctance to sleep alone, sleep onset latency, and nighttime awakenings as predictors of the level and change in depressive symptom severity across time in a MLM controlling for the covariates above (Table 3). There were main effects of sleep onset latency and refusal to sleep alone indicating a positive association with average depressive symptom severity across time (Figures 1 and 2). Nighttime awakenings were not associated with depressive symptom severity across time. There was no significant interaction between any of the three sleep variables and child age, indicating that preschool sleep problems did not influence the rate of increase or decrease in depressive symptom severity across time.
Table 3.
Fixed Effect Estimates from Multilevel Models Predicting Change in Symptom Severity from Preschool Sleep Problems (n= 292)
| B | SE | t | p | |
|---|---|---|---|---|
| DV: MDD Severity | ||||
| Intercept | 2.91 | 0.25 | 11.58 | 0.000 |
| Child Age | 0.09 | 0.23 | 3.22 | 0.001 |
| Family Income-to-Needs | −0.17 | 0.06 | −2.85 | 0.005 |
| Maternal Internalizing | −0.75 | 0.14 | −5.37 | 0.000 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 2.34 | 0.020 |
| Refusal to Sleep Alone *y/n | −0.68 | 0.27 | −2.53 | 0.012 |
| Nighttime Awakenings | 0.06 | 0.14 | 0.41 | 0.685 |
| Age*Sleep initiation time | 0.00 | 0.00 | 0.15 | 0.879 |
| Age*Refusal to sleep alone | −0.00 | 0.04 | −0.11 | 0.915 |
| DV: GAD/SAD Severity | ||||
| Intercept | 5.87 | 0.33 | 17.56 | 0.000 |
| Child Age | −0.24 | 0.03 | −7.68 | 0.000 |
| Family Income-to-Needs | −0.17 | −.08 | −2.17 | 0.031 |
| Maternal Internalizing | −0.75 | 0.19 | −3.99 | 0.000 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 2.97 | 0.003 |
| Refusal to Sleep Alone *y/n | −2.30 | 0.35 | −6.59 | 0.000 |
| Nighttime Awakenings | −0.09 | 0.19 | −0.45 | 0.653 |
| Age*Sleep initiation time | −0.00 | 0.00 | 01.35 | 0.177 |
| Age*Refusal to sleep alone | 0.15 | 0.04 | 3.63 | 0.000 |
| DV: ADHD severity | ||||
| Intercept | 6.64 | 0.66 | 10.05 | 0.000 |
| Child Age | −0.03 | 0.06 | −0.50 | 0.62 |
| Family Income-to-Needs | −0.59 | 0.17 | −3.58 | 0.000 |
| Maternal Internalizing | −1.78 | 0.39 | −4.48 | 0.000 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 1.96 | 0.05 |
| Refusal to Sleep Alone *y/n | −0.24 | 0.67 | −0.36 | 0.721 |
| Nighttime Awakenings | 0.09 | 0.41 | 0.23 | 0.819 |
| Age*Sleep initiation time | 0.00 | 0.00 | 0.14 | 0.890 |
| Age*Refusal to sleep alone | −0.13 | 0.07 | −1.79 | 0.074 |
Note: MDD- major depressive disorder; GAD/SAD- generalized anxiety disorder/separation anxiety disorder; ADHD- attention deficit hyperactivity disorder
Figure 1.
Main Effect of Refusal to Sleep Alone on MDD Severity Scores over Time
Figure 2.
Main Effect of Sleep Onset Latency on MDD Severity Scores over Time
Anxiety severity at school age
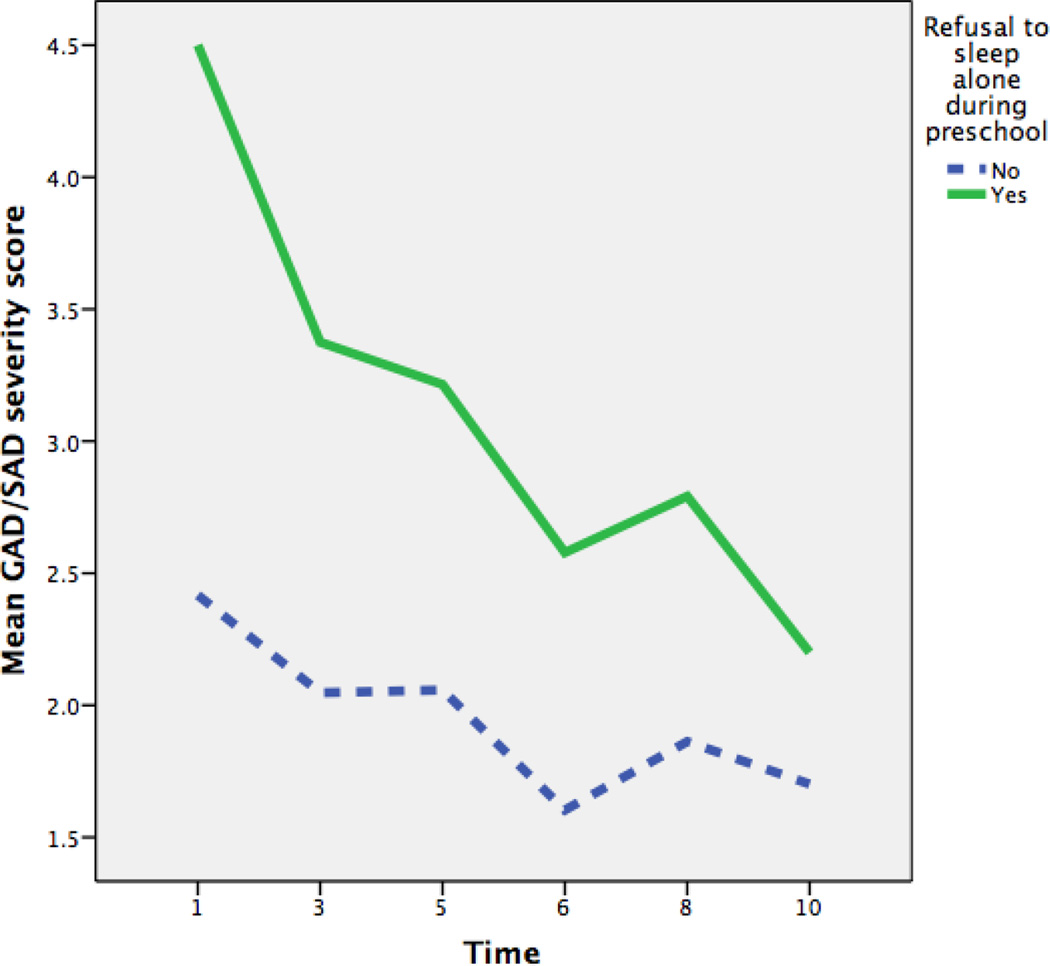
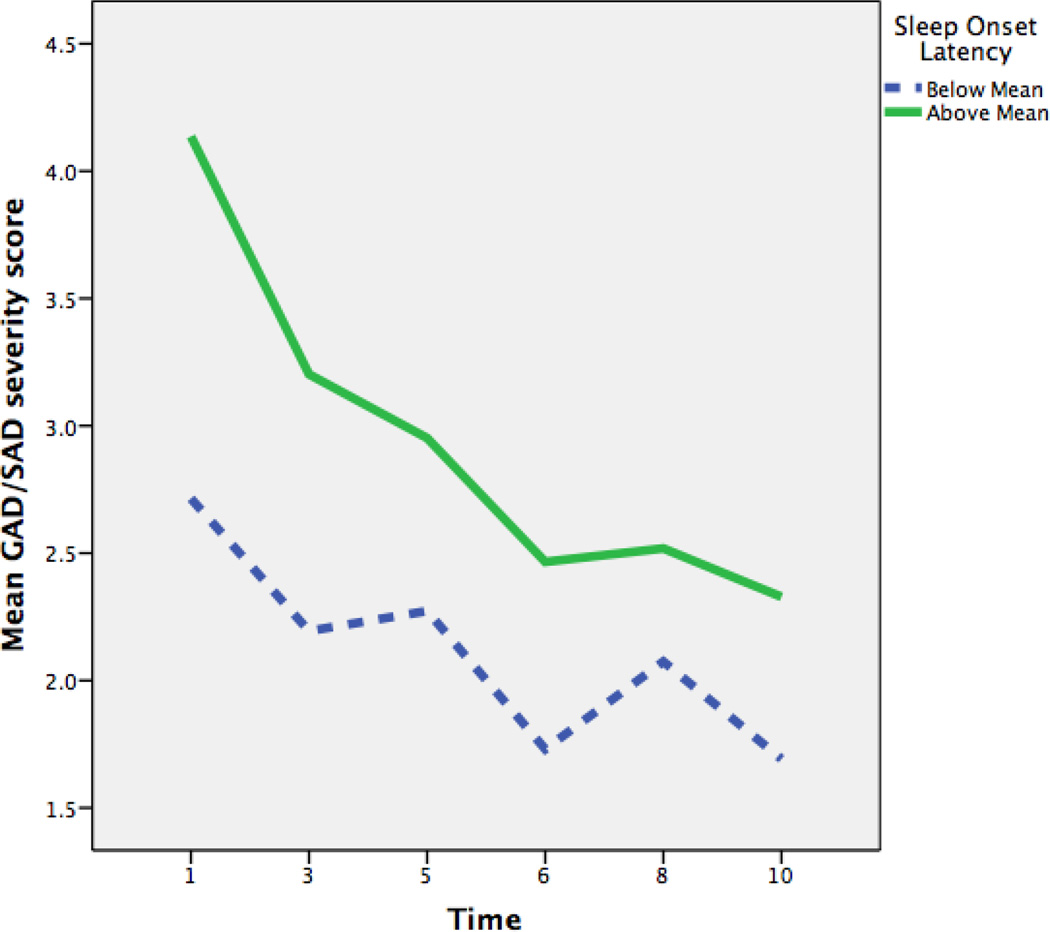
We examined reluctance to sleep alone, sleep onset latency, and nighttime awakenings as predictors of the level and change in anxiety symptom severity across time in an MLM controlling for the covariates above (Table 3). As shown in Figures 3 and 4, there were main effects of sleep onset latency and refusal to sleep alone in predicting average levels of anxiety symptom severity across time. Nighttime awakenings were not associated with GAD/SAD severity across time. In addition, there was an interaction between child age and refusal to sleep alone. In order to aid in the interpretation of these interactions, we tested the significance of the simple slopes for children who did and did not refuse to sleep alone. Overall both groups of children had significant decreases in their GAD/SAD symptoms over time, however children who refused to sleep alone had a faster decrease in GAD/SAD symptoms.
Figure 3.
Main Effect of Refusal to Sleep Alone
Figure 4.
Main Effect of Sleep Onset Latency on GAD/SAD Severity Scores over Time
ADHD severity at school age
We examined reluctance to sleep alone, sleep onset latency, and nighttime awakenings as predictors of the level and change in ADHD symptom severity across time in an MLM controlling for the covariates above. None of the preschool sleep problems predicting average ADHD severity or change across time in ADD severity.
Exploratory Analyses in Healthy Preschoolers
In order to test whether similar effects could be detected in healthy preschoolers, we repeated the above analyses but using only the subsample of n = 81 children who had no psychiatric diagnoses during the preschool period of development (e.g., healthy controls). Preschool sleep problems did not significantly predict depressive or ADHD symptom severity in previously healthy preschoolers (Table 4). However, sleep onset latency and refusal to sleep alone were significant predictors of GAD/SAD symptom severity. Longer sleep onset latency and refusal to sleep alone were associated with higher average levels of GAD/SAD severity across time.
Table 4.
Fixed Effect Estimates from Multilevel Models Predicting Change in Symptom Severity from Preschool Sleep Problems in Healthy Preschoolers (n= 81)
| B | SE | t | p | |
|---|---|---|---|---|
| DV: MDD Severity | ||||
| Intercept | 1.36 | 0.46 | 2.95 | 0.004 |
| Child Age | 0.14 | 0.05 | 2.78 | 0.006 |
| Family Income-to-Needs | −0.16 | 0.09 | −1.83 | 0.069 |
| Maternal Internalizing | −0.48 | 0.19 | −2.5 | 0.014 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 0.03 | 0.977 |
| Refusal to Sleep Alone *y/n | 0.91 | 0.42 | 0.22 | 0.830 |
| Nighttime Awakenings | −0.18 | 0.18 | −0.98 | 0.327 |
| Age*Sleep initiation time | 0.00 | 0.00 | 0.49 | 0.621 |
| Age*Refusal to sleep alone | −0.04 | 0.06 | −0.71 | 0.481 |
| DV: GAD/SAD Severity | ||||
| Intercept | 3.11 | 0.49 | 6.38 | 0.000 |
| Child Age | −0.15 | 0.05 | −3.00 | 0.003 |
| Family Income-to-Needs | −0.13 | 0.08 | −1.47 | 0.147 |
| Maternal Internalizing | −0.41 | 0.19 | −2.11 | 0.038 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 2.05 | 0.043 |
| Refusal to Sleep Alone *y/n | −0.96 | 0.46 | −2.10 | 0.038 |
| Nighttime Awakenings | −0.16 | 0.18 | −0.86 | 0.393 |
| Age*Sleep initiation time | −0.00 | 0.00 | −1.24 | 0.216 |
| Age*Refusal to sleep alone | 0.11 | 0.06 | 1.98 | 0.05 |
| DV: ADHD severity | ||||
| Intercept | 2.74 | 0.76 | 3.62 | 0.000 |
| Child Age | −0.06 | 0.06 | −0.93 | 0.36 |
| Family Income-to-Needs | −0.19 | 0.16 | −1.19 | 0.24 |
| Maternal Internalizing | −0.37 | 0.37 | −1.02 | 0.31 |
| Time it takes until sleep initiation | 0.00 | 0.00 | 0.57 | 0.57 |
| Refusal to Sleep Alone *y/n | −1.03 | 0.63 | −1.62 | 0.11 |
| Nighttime Awakenings | 0.01 | 0.35 | 0.04 | 0.97 |
| Age*Sleep initiation time | −0.00 | 0.00 | −0.53 | 0.59 |
| Age*Refusal to sleep alone | 0.09 | 0.07 | 1.29 | 0.20 |
Note: MDD- major depressive disorder; GAD/SAD- generalized anxiety disorder/separation anxiety disorder; ADHD- attention deficit hyperactivity disorder attention deficit hyperactivity disorder
DISCUSSION
This study provides evidence for the importance of two parent-reported preschool-onset sleep disturbances: difficulty sleeping alone and prolonged sleep onset latency as important predictors for depression and anxiety symptom severity, but not ADHD symptom severity across time. These relatively common preschool sleep difficulties continued to predict depression and anxiety severity, even after controlling for family income-to-needs ratio and maternal internalizing psychopathology. Furthermore, even among healthy preschoolers, parent reported sleep onset latency and refusal to sleep alone predicted greater anxiety symptom severity across time.
Sleep difficulties predicted the continuation of greater diagnostic severity of depression and anxiety symptoms across childhood. Sleep is known to be crucial for adaptive emotion regulation processes, particularly in young children. In a recent study (Miller, Seifer, Crossin, & Lebourgeois, 2015), toddlers who were sleep deprived (e.g., no nap on the day of the study) were less able to engage with a difficult puzzle and were more likely to use relatively immature self-regulation strategies, such as physical self-soothing when compared to toddlers who were not sleep deprived. Extending Miller and colleagues’ (2015) findings to the current study, both sleep onset latency and refusal to sleep alone in slightly older, preschool age children may also result in diminished sleep each night. Over time, this daily reduction in sleep may be associated with cascading effects, such as poor emotion regulatory abilities, circadian dysregulation and other difficulties that all contribute to the continuation in depressive and anxiety symptoms later in childhood. Given that ineffective emotion regulation is characteristic of children and adolescents with depression (Kovacs & Yaroslavsky, 2014) and anxiety (Suveg & Zeman, 2004), early sleep difficulties may be one pathway by which these difficulties emerge and lead to internalizing psychopathology. Future research would benefit from exploring these cascading relationships longitudinally over the course of development.
As a further exploration of the risk trajectory between early sleep problems and the onset of later psychopathology, given that many children in our sample already had clinically significant psychopathology during the preschool period, we ran analyses restricting our sample to healthy preschoolers. In doing so, we assessed whether preschool sleep problems predicted greater depressive and anxiety symptom severity during school age among healthy preschoolers. Similar to the longitudinal results found with the whole sample, neither of the preschool sleep problems predicted increased ADHD symptom severity across time in previously healthy preschoolers. However, parent reported sleep onset latency and refusal to sleep alone did significantly predict anxiety symptom severity, although not at the clinically significant threshold in previously healthy preschoolers. This finding suggests that these two sleep problems may be a unique prodromal risk factor for the development of anxiety later in childhood.
Strengths and limitations
Several limitations exist in the current study. First, this study presents findings from subjective parental reports of sleep problems, which may be influenced by reporter bias. Objective assessments of sleep using videosomnography and/or actigraphy would provide more quantifiable evidence for the existence and severity of sleep problems in this sample, particularly the duration of time a child takes to fall asleep (Kelly & El-Sheikh, 2014; Pesonen et al., 2014). Current data collection is underway to obtain this type of data among the adolescent participants of the PDS using accelerometers. Although sometimes considered a ‘second-best’ assessment method compared with objective sleep measurement, subjective reports do provide unique and valuable information about the nature of sleep (Gregory & Sadeh, 2015). Further, the parents of young children are generally aware of their child’s sleep habits and behaviors (Acebo et al., 2005). Although this study provides some insight into directional relationships between sleep, depression, and anxiety, we were unable to test bidirectional relationships between preschool disorders and prospective difficulties sleeping alone and sleep onset latency. Given that sleep and internalizing disorders may have bidirectional relationships (e.g., Gregory & Sadeh, 2015), it will be important for future work to further tease how sleep onset latency and refusal to sleep alone bidirectionally influence depressive symptoms in preschool to school aged children. Furthermore, the sleep variables studied here may be influenced by parental attitudes and anxiety around bedtime (Meltzer & Mindell, 2007), particularly since young children are dependent on their caregivers for bedtime routines and structure. Future work should consider incorporating measures of parental bedtime anxiety as potential mediators of the relations between preschool sleep and school-age depressive severity.
Despite these limitations, this study also has several strengths. First, we focused on three precise, yet relatively common sleep problems that occur during the preschool period and as a result, our findings offer enhanced specificity to longitudinal outcomes among preschoolers with and without psychiatric disorders. Our sample included a large number of preschoolers with clinically significant and diagnosable psychopathology, an improvement over past studies that have focused on subclinical symptoms in relatively healthy samples.
Clinical implications
The results from this study indicate that preschool-onset sleep problems, specifically parent reported sleep onset latency and difficulty sleeping alone predict depression and anxiety symptom severity over time. Although there are multiple risk factors that interact to predict later psychopathology, it may be advisable to treat refusal to sleep alone and/or latency to sleep onset earlier in development, and in addition to other known risk factors as they may contribute to the continuation of depressive and anxiety symptoms later in childhood. Moreover, given that rates of depression increase drastically during adolescence (Kessler, Avenevoli, & Ries Merikangas, 2001), identifying treatable precursors to this surge earlier in development may curb this increase and associated negative outcomes. The importance of this recommendation is further underscored by the fact that currently, these problems may be discounted by primary care physicians as self-limited and not clinically concerning (Chervin, Archbold, Panahi, & Pituch, 2001; Meltzer, Plaufcan, Thomas, & Mindell, 2014). Given the importance of sleep for optimal physical and mental health, clinicians may need to more carefully screen and assess for sleep disturbances during preschool. As such, enhanced parental education about sleep benefits, healthy sleep routines, and overall sleep hygiene may help to prevent the continuation of sleep problems from preschool into school age and decrease the impact that these sleep problems may have on emotion functioning.
Key points.
Child and adolescent psychopathology has been linked to increased sleep problems, but there has been less investigation of this relationship in younger samples with early-onset psychopathology.
Three specific but commonly observed aspects of sleep behaviors in young children-- 1. Sleep onset latency, 2. Refusal to sleep alone, and 3. Nighttime awakenings were measured during preschool
Difficulty sleeping alone and prolonged sleep onset latency were important predictors of depression and anxiety symptom severity, but not ADHD symptom severity across time
Identifying children presenting with these sleep problems earlier in development may decrease the likelihood that severe depression and anxiety symptoms continue across time.
Acknowledgments
The authors wish to thank the children, caregivers, and staff of the Preschool Depression Study for their time and dedication to this project. All phases of this study were supported by an NIH grant, R01 MH064769-06A1. D.J.W. was supported by NIH grants: L30 MH108015 (PI: D.J.W.) and T32 MH100019 (PI’s: D.M.B. and J.L.L.). D.M.B. consults for Pfizer, Amgen, Takeda, and Roche on psychosis related work. K.E.G. was also supported by T32 MH100019 (PI’s: D.M.B and J.L.L.). J.L.L. receives royalties from Guilford Press.
Footnotes
The rest of the authors have declared that they have no competing or potential conflicts of interest.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep. 2005;28(12):1568–1577. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- Alfano CA, Ginsburg GS, Kingery JN. Sleep-Related Problems Among Children and Adolescents With Anxiety Disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(2):224–232. doi: 10.1097/01.chi.0000242233.06011.8e. http://doi.org/10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, Harris JK. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep. 2013;36(7):1059–1068. doi: 10.5665/sleep.2810. http://doi.org/10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anders TF, Dahl RE. Classiyfing sleep disorders in infants and toddlers. In: Nafrow WE, First MB, Sirovatka PJ, Regier DA, editors. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-V. 1st. Arlington, VA: American Psychiatric Publishing; 2007. pp. 215–226. [Google Scholar]
- Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):39–48. doi: 10.1097/00004583-200001000-00015. http://doi.org/10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M. The Child and Adolescent Psychiatric Assessment (CAPA) Psychological Medicine. 1995;25(04):739–753. doi: 10.1017/s003329170003498x. http://doi.org/10.1017/S003329170003498X. [DOI] [PubMed] [Google Scholar]
- Augustinavicius JLS, Zanjani A, Zakzanis KK, Shapiro CM. Polysomnographic features of early-onset depression: A meta-analysis. Journal of Affective Disorders. 2014;158:11–18. doi: 10.1016/j.jad.2013.12.009. http://doi.org/10.1016/j.jad.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Boekamp JR, Williamson LR, Martin SE, Hunter HL, Anders TF. Sleep Onset and Night Waking Insomnias in Preschoolers with Psychiatric Disorders. Child Psychiatry & Human Development. 2014;46(4):622–631. doi: 10.1007/s10578-014-0505-z. http://doi.org/10.1007/s10578-014-0505-z. [DOI] [PubMed] [Google Scholar]
- Chervin RD, Archbold KH, Panahi P, Pituch KJ. Sleep Problems Seldom Addressed at Two General Pediatric Clinics. Pediatrics. 2001;107(6):1375–1380. doi: 10.1542/peds.107.6.1375. http://doi.org/10.1542/peds.107.6.1375. [DOI] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Waltr BK, Angold A. Test-Retest Reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. http://doi.org/10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Eisen AR, Schaefer CE. Separation anxiety in children and adolescents: An individualized approach to assessment and treatment. Guilford Press; 2007. [Google Scholar]
- Goodlin-Jones B, Tang K, Liu J, Anders TF. Sleep problems, sleepiness and daytime behavior in preschool-age children. Journal of Child Psychology and Psychiatry. 2009;50(12):1532–1540. doi: 10.1111/j.1469-7610.2009.02110.x. http://doi.org/10.1111/j.1469-7610.2009.02110.x. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Caspi A, Eley TC, Moffitt TE, O’Connor TG, Poulton R. Prospective Longitudinal Associations Between Persistent Sleep Problems in Childhood and Anxiety and Depression Disorders in Adulthood. Journal of Abnormal Child Psychology. 2005;33(2):157–163. doi: 10.1007/s10802-005-1824-0. http://doi.org/10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Eley TC, O’Connor TG, Plomin R. Etiologies of Associations Between Childhood Sleep and Behavioral Problems in a Large Twin Sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(6):744–751. doi: 10.1097/01.chi/0000122798.47863.a5. http://doi.org/10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- Gregory AM, O’Connor TG. Sleep Problems in Childhood: A Longitudinal Study of Developmental Change and Association With Behavioral Problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(8):964–971. doi: 10.1097/00004583-200208000-00015. http://doi.org/10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews. 2012;16(2):129–136. doi: 10.1016/j.smrv.2011.03.007. http://doi.org/10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Sadeh A. Annual Research Review: Sleep problems in childhood psychiatric disorders – a review of the latest science. Journal of Child Psychology and Psychiatry. 2015;n/a–n/a doi: 10.1111/jcpp.12469. http://doi.org/10.1111/jcpp.12469. [DOI] [PubMed] [Google Scholar]
- Hatzinger M, Brand S, Perren S, Von Wyl A, Stadelmann S, von Klitzing K, Holsboer-Trachsler E. In pre-school children, sleep objectively assessed via actigraphy remains stable over 12 months and is related to psychological functioning, but not to cortisol secretion. Journal of Psychiatric Research. 2014;55:22–28. doi: 10.1016/j.jpsychires.2014.04.008. http://doi.org/10.1016/j.jpsychires.2014.04.008. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Johnson K. Sleep Disturbances in Children With Psychiatric Disorders. Seminars in Pediatric Neurology. 2008;15(2):70–78. doi: 10.1016/j.spen.2008.03.008. http://doi.org/10.1016/j.spen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology. 2014;50(4):1137–1147. doi: 10.1037/a0034501. http://doi.org/10.1037/a0034501. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biological Psychiatry. 2001;49(12):1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Yaroslavsky I. Practitioner review: Dysphoria and its regulation in child and adolescent depression. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2014;55(7):741–757. doi: 10.1111/jcpp.12172. http://doi.org/10.1111/jcpp.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby JL, Belden AC, Pautsch J, Si X, Spitznagel E. The clinical significance of preschool depression: Impairment in functioning and clinical markers of the disorder. Journal of Affective Disorders. 2009;112(1–3):111–119. doi: 10.1016/j.jad.2008.03.026. http://doi.org/10.1016/j.jad.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E. The Preschool Feelings Checklist: A Brief and Sensitive Screening Measure for Depression in Young Children. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(6):708–717. doi: 10.1097/01.chi.0000121066.29744.08. http://doi.org/10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- Luby JL, Mrakotsky C, Heffelfinger A, Brown K, Spitznagel E. Characteristics of depressed preschoolers with and without anhedonia: evidence for a melancholic depressive subtype in young children. The American Journal of Psychiatry. 2004;161(11):1998–2004. doi: 10.1176/appi.ajp.161.11.1998. http://doi.org/10.1176/appi.ajp.161.11.1998. [DOI] [PubMed] [Google Scholar]
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 months. Archives of General Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. http://doi.org/10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell ME. Family Interview for Genetic Studies (FIGS): a manual for FIGS. Clinical Neurogenetics Branch, Intramural Research Program, National Institute of Mental Health, Bethesda, MD. 1992 [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53(2):185–204. doi: 10.1037//0003-066x.53.2.185. http://doi.org/10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: A pilot study. Journal of Family Psychology. 2007;21(1):67–73. doi: 10.1037/0893-3200.21.1.67. http://doi.org/10.1037/0893-3200.21.1.67. [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Plaufcan MR, Thomas JH, Mindell JA. Sleep Problems and Sleep Disorders in Pediatric Primary Care: Treatment Recommendations, Persistence, and Health Care Utilization. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2014;10(4):421–426. doi: 10.5664/jcsm.3620. http://doi.org/10.5664/jcsm.3620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Seifer R, Crossin R, Lebourgeois MK. Toddler’s self-regulation strategies in a challenge context are nap-dependent. Journal of Sleep Research. 2015;24(3):279–287. doi: 10.1111/jsr.12260. http://doi.org/10.1111/jsr.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, Emslie G, Blumer J, Genel M, Glaze D, Ivanenko A, Banas B. Pharmacologic Management of Insomnia in Children and Adolescents: Consensus Statement. Pediatrics. 2006;117(6):e1223–e1232. doi: 10.1542/peds.2005-1693. http://doi.org/10.1542/peds.2005-1693. [DOI] [PubMed] [Google Scholar]
- Pesonen A-K, Martikainen S, Heinonen K, Wehkalampi K, Lahti J, Kajantie E, Räikkönen K. Continuity and Change in Poor Sleep from Childhood to Early Adolescence. Sleep. 2014;37(2):289–297. doi: 10.5665/sleep.3400. http://doi.org/10.5665/sleep.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peugh JL. A practical guide to multilevel modeling. Journal of School Psychology. 2010;48(1):85–112. doi: 10.1016/j.jsp.2009.09.002. http://doi.org/10.1016/j.jsp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Tikotzky L, Kahn M. Sleep in infancy and childhood: implications for emotional and behavioral difficulties in adolescence and beyond. Current Opinion in Psychiatry. 2014;27(6):453–459. doi: 10.1097/YCO.0000000000000109. http://doi.org/10.1097/YCO.0000000000000109. [DOI] [PubMed] [Google Scholar]
- Simola P, Laitalainen E, Liukkonen K, Virkkula P, Kirjavainen T, Pitkäranta A, Aronen ET. Sleep disturbances in a community sample from preschool to school age. Child: Care, Health and Development. 2012;38(4):572–580. doi: 10.1111/j.1365-2214.2011.01288.x. http://doi.org/10.1111/j.1365-2214.2011.01288.x. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Harvey A, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: A longitudinal study. JAMA Pediatrics. 2015;169(6):575–582. doi: 10.1001/jamapediatrics.2015.0187. http://doi.org/10.1001/jamapediatrics.2015.0187. [DOI] [PubMed] [Google Scholar]
- Suveg C, Zeman J. Emotion Regulation in Children With Anxiety Disorders. Journal of Clinical Child & Adolescent Psychology. 2004;33(4):750–759. doi: 10.1207/s15374424jccp3304_10. http://doi.org/10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- Tesler N, Gerstenberg M, Huber R. Developmental changes in sleep and their relationships to psychiatric illnesses: Current Opinion in Psychiatry. 2013;26(6):572–579. doi: 10.1097/YCO.0b013e328365a335. http://doi.org/10.1097/YCO.0b013e328365a335. [DOI] [PubMed] [Google Scholar]
- West BT. Analyzing Longitudinal Data With the Linear Mixed Models Procedure in SPSS. Evaluation & the Health Professions. 2009;32(3):207–228. doi: 10.1177/0163278709338554. http://doi.org/10.1177/0163278709338554. [DOI] [PubMed] [Google Scholar]