Abstract
Distally anchored uncemented modular tapered porous stems are often the preferred treatment in total hip arthroplasty revisions and failed subtrochanteric fractures. These conditions mainly affect elderly osteoporotic patients, with an increased risk of later fractures below the well-fixated implant. Treatment in secondary fractures with long looking plates is the recommended treatment, where stability is a key to fracture healing. We report a complicated case in which this was achieved by an innovative technique combing the trochanteric attachment bolt of the stem system and a locking plate with polyaxial screws.
Keywords: Locking plate, Modular tapered porous stem, Periprosthetic fracture, Subtrochanteric fracture, Total hip arthroplasty
Introduction
Complex hip fractures and periprosthetic fractures often occur in elderly, weak, and hospitalized patients. Treatment should be focused on early mobilization and return to their daily activities. Distally anchored modular tapered stems are designed for axial and rotational stability with subsequent osseointegration and are often a good choice in periprosthetic fractures with loose stems and in failed subtrochanteric treatment. The problem occurs when these well-integrated distally anchored hip implants are simultaneously compromised with both an unanticipated infection and a traumatic periprosthetic fracture in distal femur.
Case history
An overweight 85-year-old woman with congestive heart failure, diabetes, and osteoporosis suffered a pertrochanteric fracture in her nursing home in January 2014. She was treated with internal fixation with a plate and a sliding screw. The osteosynthesis was insufficient, and she was reoperated 2 months later with an AO (DepuySynthes, West Chester, PA) condylar plate, but the femoral head and the acetabulum were destroyed by screw and plate cutout without any signs of fracture healing (Fig. 1a and b). A total hip arthroplasty with a trochanteric osteotomy was performed with the Arcos Modular Femoral Revision System (Biomet Inc., Warsaw, IN) without any complications during surgery (Fig. 2a and b), and 5 cultures from the previous plate were negative. The hip system has been used at our institution since March 2012, and we participated in an international multicenter study on hip revisions 2013-2014 (Ethical Committee GU # 575-13, 2013-09-10), although this elderly lady did not fit the inclusion criteria.
Figure 1.
(a) Anteroposterior radiograph of the left proximal femur after failure of a dynamic hip screw and (b) subsequent AO 95° condylar blade plate fixation of a pertrochanteric fracture.
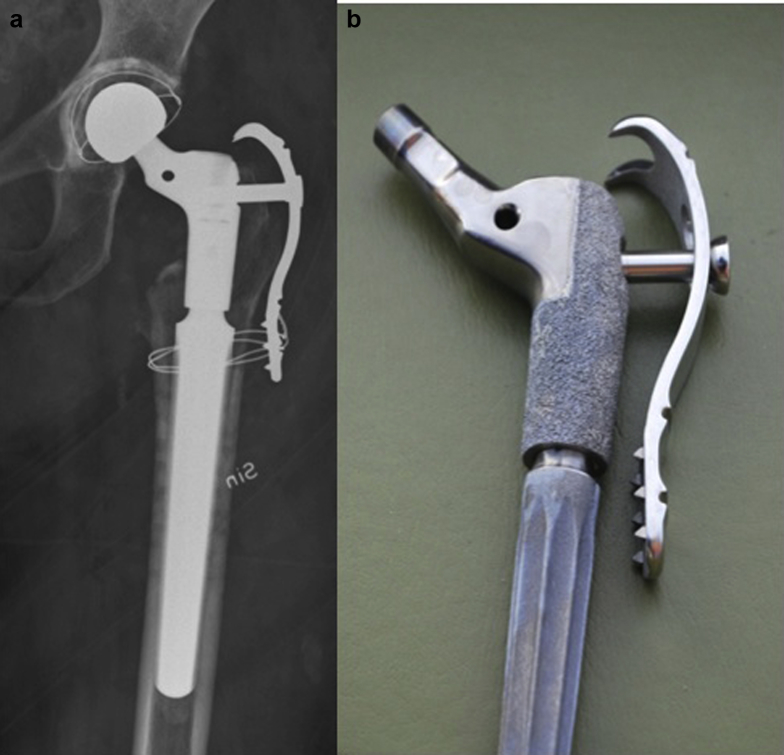
Figure 2.
(a) Anteroposterior radiograph of the left proximal femur after removal of the plate and conversion to total hip arthroplasty with an Arcos modular STS stem, claw plate with trochanteric reattachment bolt, and a Lubinus/Link cemented acetabulum cup articulating against a 32-mm Cr-Co-Mo head. (b) Photograph of a proximal Arcos hip prosthesis with claw plate and trochanteric reattachment bolt.
Four months later, she fell at her rehabilitation facility and sustained a periprosthetic Vancouver B1 fracture with the prosthesis in place (Fig. 3a and b). There were no signs of subsidence, osteolysis, or zones around the hip implant, but her erythrocyte sedimentation rate was 99. The wound had healed, but the skin was red and edematous, and we suspected a deep infection.
Figure 3.
Anteroposterior radiograph of the left femur (a) proximally and (b) distally. A periprosthetic fracture classified as Vancouver type B1 is noted. The trochanteric osteotomy appears healed.
There was a choice between emergency surgery by 2 experienced surgeons in the afternoon of the admission day (Thursday) or between both further infection diagnostics and ordering the noncontact bridging (NCB) trochanteric extension. This would have delayed surgery well over the weekend with the patient staying in bed with agony and increased risk of cardiopulmonary complications and decubitus ulcers.
Fracture surgery was performed through an extended long lateral incision used in previous hip implant surgery down to the fracture site and was combined with a distal insertion allowing skin bridging. Before fracture reduction, debridement and rinsing of the hip joint was performed and supplemented with 2 resorbable, equine collagen fleeces impregnated with gentamicin in the joint and trochanteric area. Ten cultures were taken and later verified a joint infection with coagulase-negative staphylococci. There was soft callus formation at the site of the trochanteric fractures and the previous osteotomy and no obvious signs of pseudarthrosis.
We found that the longest available NCB Periprosthetic Proximal Femur Plate (Zimmer, Warsaw, IN) with 21 holes and 401 mm long would be sufficient. There is a trochanteric extension with looking screws available for this plate which provides desirable trochanteric support, but we had no such device available at our hospital. To fit the femur, the plate was instead contoured using an AO large plate bending press. While keeping it stable in that tool, the middle of the proximal plate holes was slightly enlarged to fit the 5.5-6 mm stepped bolt screw of the Arcos system, using an Anspach Black Max pneumatic drill (Soma Technology, Cheshire, CT) with a high-speed metal burr to remove the screw threads of the looking plate (Fig. 4a and b). This procedure and cleaning the plate took us <2 minutes once the shape of the plate was accepted.
Figure 4.

(a) Photograph of lateral view of a proximal Arcos hip prosthesis with reattachment bolt and (b) Zimmer noncontact bridging plate with arrow indicating the hole that was enlarged in the plate.
Fracture treatment followed general principles according to the AO manual [1]. We made every effort to let the proximal part of the NCB plate contour the greater trochanter, while the technique with bridge plating allowed us to leave some millimeters between the plate and the rest of the femur. The bolt screw was pulled 55 inch-pounds (6.2 Nm) according to the Arcos Torque Limiting T-handle and was hand driven an additional eighth of a turn to make sure that the bolt was secured and fastening the plate. We used a new Arcos bolt screw of 28 mm that was 8 mm shorter than the original screw in the claw plate. Two cortical 4-mm looking screws were angled to pass beside the cone body of the stem, and one additional blunt tip cortical locking screw completed what we found a very stable proximal plate fixation. We secured the reduced fracture with 2 NCB-plate 1.8-mm wires and then left 7-8 cm of the skin below the fracture before inserting 5 distal bicortical 5-mm screws through a distal skin insertion.
The patient was unable to allow restricted weight bearing and was mobilized in a wheelchair for 7 weeks. A follow-up radiograph then showed less-visible fracture lines, and weight bearing with a walker was permitted. The infection was first treated with intravenous clindamycin postoperatively but changed to oral treatment with fusidic acid and rifampicin until serious side effects on her liver and blood count terminated its use after 10 weeks. Erythrocyte sedimentation rate and C-reactive protein level gradually declined, and the final radiographs after 4 months showed no signs of insufficient fracture healing (Fig. 5a and c). She died from causes unrelated to her hip 8 months after our surgery. In the months before her death, she used her walker for limited distances without notable pain in her nursing home.
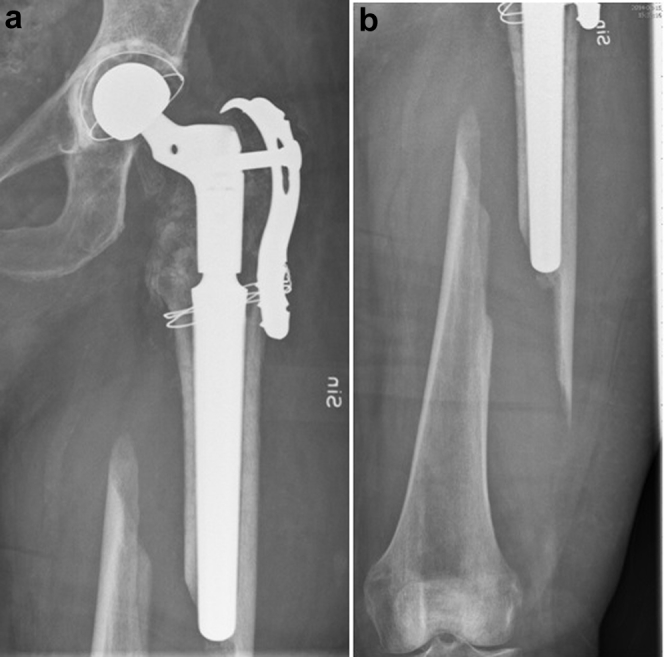
Figure 5.
Anteroposterior radiograph of the left femur (a) proximally and (b) distally and (c) lateral radiograph. The fracture appears healed.
Discussions
Distally fixated uncemented tapered porous stems have been used in hip revisions with extended bone loss, periprosthetic fractures, and unhealed subtrochanteric fractures since the Wagner stem was introduced in the late 1980s [2]. Increased modularity and more precise introduction systems have increased their popularity in recent years 3, 4. Revisions and failed subtrochanteric fractures mainly affect elderly patients with deficient bone stock today [5]. This may be causing an increased risk of further periprosthetic fractures of Vancouver B1 and C type [6] below the distally anchored implant. These fractures are preferably treated with open reduction and internal fixation with long plates [5]. After trochanteric fractures, extended osteotomies, thin cortical bone and large proximal bodies of the implants, the area for a stable proximal plate fixation is usually limited.
Bicortical screws are preferred in both ends of these long plates because they represent a much higher biomechanical strength than unicortical screws and cerclage wires [7]. The technique can also be advantageously combined with a structural cortical onlay allograft that we think will improve both fixation and fracture healing [8] but was not used in this case because it would have delayed surgery and we were also suspecting a deep infection.
In a young and healthy patient, we would have diagnosed a potential periprosthetic infection and considered a 1- or 2-stage revision. However, debridement and antibiotic suppression seems to be an alternative in compromised patients who are not suitable for major revision surgery 9, 10.
The long-term results cannot be predicted from a single case. There is a trochanteric extension commercially available for this plate which would have been preferable if available or a patient able to endure a delay of surgery. However, there are femoral looking plates with polyaxiality from other manufactures that lack this trochanteric option. Reconstructing such a plate by enlarging a screw hole may weaken the implant. There is also a risk of corrosion products between the bolt and the hole in the plate. Nevertheless, we present a unique technical solution in our case in which the Arcos hip system was used in combination with a perioperatively slightly modified polyaxial locking plate that achieved our goals for our patient.
Summary
Well-performed surgery with modular distally anchored tapered stems is often a good choice in hip revision surgery and in treatment of failed subtrochanteric fractures. In a growing population of elderly patients with a poor bone stock, the risk of Vancouver type B1 and C fractures below a well-integrated implant may increase. We present a new technical solution in some of these cases, when the Arcos hip system has been used.
Acknowledgments
The case report was funded by the Fyrbodal Research and Development Council Region Västra Götaland Grant # VGFOUFBD-535851—A Health Research Fund of Western Sweden.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.02.002.
Appendix A. Supplementary data
References
- 1.Wagner M., Frigg R. Thieme; New York: 2006. AO manual of fracture management. Internal fixators—concepts and cases using LCP and LISS; p. 521. [Google Scholar]
- 2.Wagner H., Wagner M. Femur revision prosthesis. Z Orthop Ihre Grenzgeb. 1993;131(6):574. doi: 10.1055/s-2008-1040074. [DOI] [PubMed] [Google Scholar]
- 3.Swedish Hip Arthroplasty Register (SHAR) The Annual Report 2012; 67, http://shpr.se/. [accessed 10.01.16]
- 4.Wirtz D.C., Gravius S., Ascherl R. Uncemented femoral revision arthroplasty using a modular tapered, fluted titanium stem: 5- to 16-year results of 163 cases. Acta Orthop. 2014;85(6):562. doi: 10.3109/17453674.2014.958809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yasen A.T., Haddad F.S. Periprosthetic fractures: bespoke solutions. Bone Joint J. 2014;96-B(11 Supple A):48. doi: 10.1302/0301-620X.96B11.34300. [DOI] [PubMed] [Google Scholar]
- 6.Masri B.A., Meek R.M., Duncan C.P. Periprosthetic fractures evaluation and treatment. Clin Orthop Related Res. 2004;420:80. doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Lenz M., Perren S.M., Gueorguiev B. A biomechanical study on proximal plate fixation techniques in periprosthetic femur fractures. Injury. 2014;45(Suppl 1):S71. doi: 10.1016/j.injury.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 8.Haddad F.S., Duncan C.P., Berry D.J., Lewallen D.G., Gross A.E., Chandler H.P. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002;84-A(6):945. [PubMed] [Google Scholar]
- 9.Zimmerli W., Trampuz A., Ochsner P.E. Prosthetic-joint infections. N Engl J Med. 2004;351:1645. doi: 10.1056/NEJMra040181. [DOI] [PubMed] [Google Scholar]
- 10.Whitehouse M.R., Parry M.C., Konan S., Duncan C.P. Deep infection after hip arthroplasty: staying current with change. Bone Joint J. 2016;98-B(1 Suppl A):27. doi: 10.1302/0301-620X.98B1.36294. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.