Abstract
Background
There is now a clear trend with increased usage of cementless femoral stems for all ages and most patients. As the number of total hip arthroplasties (THAs) performed annually continues to increase with expanding indications for THA and demands for improved quality of life, so will the prevalence of THA in the elderly and aging populations. This is worrisome as the risk of complications with cementless femoral stems increases in elderly patients and those with poor bone quality. The purpose of this study is to analyze the available data from comparative studies to determine whether cementless femoral stems are overused and whether cemented stems warrant increased consideration.
Methods
Using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, searches were performed to find original studies comparing cementless and cemented femoral stems; large population registry studies and reports were also included.
Results
This systematic review documents that older patients with cementless fixation increase the risk of revision, there is no clear fixation advantage in midaged patients, and younger patients fare better with cementless fixation. Complications after THA create burdens on the health care system and on patients.
Conclusions
Using evidence-based data should be better guidance in selecting the most reliable implants for THA. Although cementless femoral fixation for THA has evolved to the “new standard,” it has not been proven to be the “gold standard” for all patients.
Keywords: Hip, Arthroplasty, Cement, Uncemented, Femoral stems
Introduction and background
Cementless femoral component use in primary total hip arthroplasty (THA) has increased substantially over the last 3 decades. It was recently reported that in 2012, 93% of THAs in the Orthopedic Research Network, a group of 174 hospitals in the United States, were cementless [1]. With the adoption of press-fit cementless femoral implants, the incidence of early complications, especially femoral periprosthetic fracture, resulting in early revision continues to increase [2], [3]. Other known risk factors for periprosthetic fracture include elderly patients, female gender, osteoporotic bone, and metabolic bone disease [2], [3], [4], [5], [6], [7].
It is clear that the number of THAs performed annually will continue to increase because of aging populations with improvement in life expectancy [2], [8]. The aging of the baby boomer generation along with expanding indications for THA and demands for improved quality of life, as well as policies to improve access to THA, all ensure that the numbers of THA will continue to grow [2], [8], [9]. Adding the effects of increased use of cementless femoral stems to the growing prevalence of elderly patients and patients with poor bone quality, the absolute number and relative risk of periprosthetic fractures are likely to increase both intraoperatively and postoperatively [10]. In 2013, periprosthetic fracture was one of the most common complications globally of primary THA, accounting for 6% of all THA revisions [11]. Revision of THA due to early complications is associated with a higher risk of wound complications, deep periprosthetic infection, decreased function, increased morbidity and mortality, and significant health care costs [8], [12].
Cemented femoral stems are not without their own risks such as bone cement implantation syndrome, fat embolism syndrome, and the difficulty of removing cement during explantation or revision surgery. Bone cement implantation syndrome is characterized by hypoxia, hypotension, or both and/or the unexpected loss of consciousness and is most commonly associated with cemented THA [13]. Cemented femoral stems also have certain benefits; they have been shown to minimize the risk of early complications, as well as having excellent long-term survivorship, and are cost-effective implants [14], [15].
There is no clear and compelling body of evidence we are aware of to support the routine use of cementless femoral component fixation over cemented stems in all patients, especially elderly patients or those with poor-quality bone for primary THA. However, despite this, cementless femoral stem use prevails in much of North America and is increasing globally in that patient population [16]. The purpose of this study is to analyze the available data from comparative studies evaluating cementless and cemented femoral components in primary THA with a focus on rates of complications, survivorship, and risk factors for periprosthetic fracture.
Material and methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were used to conduct this review [17], [18]. Original studies in the English language that involved THA in which cementless femoral stems were compared to cemented femoral stems are included. Large population registry studies and reports are also included. Review articles, case series, and case reports were excluded.
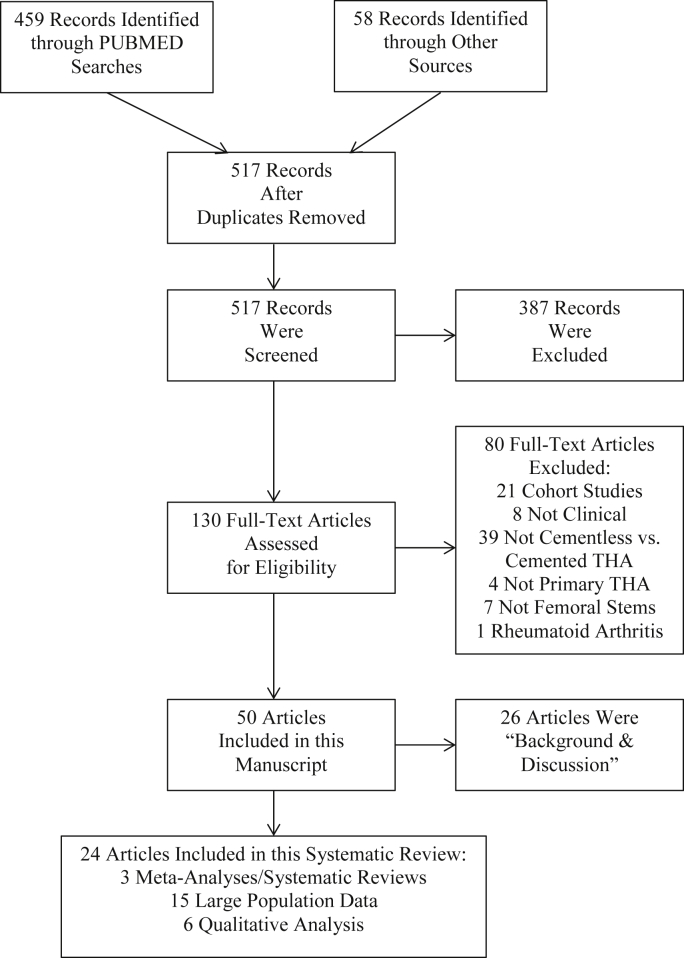
The PubMed database was interrogated for articles from January 2000 to April 2015, using 4 search strings: (1) “cemented femoral stems” and “cementless femoral stems,” (2) “meta analysis” and (“femoral” or “femur”) and (“stem” or “component”), (3) “primary” and “total hip” and (“arthroplasty” or “replacement”) and (“cement” or “cementless” or “press-fit”) and “femoral” and (“component” or “stem”), and (4) “registry” and (“cemented” or “cementless”) and “total hip” and (“arthroplasty” or “replacement”). In addition, other articles were sourced from the reference lists of meta-analyses and reference lists of included articles. In total, 517 records were found and screened (Fig. 1). First, 382 records were excluded based on titles and abstracts and an additional 85 full-text articles after further review (Supplementary Material). This article is composed of the remaining 50 articles: 26 as background/discussion material, 3 meta-analyses/systematic reviews, 15 large population data (arthroplasty registries and insurance databases), and 6 included in qualitative analyses.
Figure 1.
Search history and selection of studies.
Results
Results are in 3 distinct categories: meta-analysis and systematic reviews, large population data, and qualitative analysis of primary research. This is done because the probability for bias is different in each category. Meta-analyses and systematic reviews should have less bias, especially when conducted on randomized controlled trails (RCTs), than either of the other categories. Large population data may be biased because of the homogeneity of the population itself. Primary research may be biased because of the homogeneity of the population and the homogeneity of surgical technique and surgical experience. Using these categories seems to be a logical way to present data that are not standardized with regard to reporting technique or variables being reported. Data are summarized in Table 1.
Table 1.
Data summary table.
| Reference | Classification | Relevant outcomes |
|---|---|---|
| Morshed et al. [19] | Meta-analysis Primary THA Subgroup analysis by age |
|
| Abdulkarim et al. [20] | Meta-analysis Primary THA Randomized controlled trials only |
|
| Ni et al. [21] | Systematic review Femoral stems |
|
| Hailer et al. [22] | Swedish Registry Data Primary THA |
|
| Eskelinen et al. [23] and Mäkelä et al. [24] | Swedish Registry Data Primary THA |
|
| Engesaeter et al. [25] | Norwegian Registry Data Primary THA |
|
| Colas et al. [26] | French Health Insurance Information System Primary THA |
|
| Eskelinen et al. [23] | Finnish Registry Data Primary THA Younger patients (aged ≤55 years) |
|
| Jämsen et al. [27] | Finnish Registry Older patients (aged ≥80 years) |
|
| Mäkelä et al. [24] | Finnish Registry Intermediate patients (aged 55-64 years) |
|
| Mäkelä et al. [28] | Swedish, Norwegian, Danish, and Finnish Registries Intermediate patients (aged 55-64 years) |
|
| Havelin et al. [29] | Norwegian Registry Patients aged <60 years |
|
| Mäkelä et al. [30] | Finnish Registry Evolution of cementless femoral stems |
|
| Strom et al. [31] | Level I study Femoral stem fixation |
|
| Lindalen et al. [32] | Level I Study Femoral stem fixation Cemented femoral stems were collared |
|
| Kim [33] | Level I study Bilateral THA comparison |
|
| Emerson et al. [34] | Level III Femoral stem fixation |
|
Meta-analysis and systematic reviews
There are 2 meta-analyses/systematic reviews concerning the difference between cemented and cementless fixations in THA that do not specifically discuss femoral components [19], [20]. Owing to the nature of published data, it is not possible for these reviews to draw conclusions about the performance of individual femoral stem designs nor is it possible to draw conclusions about the causes of THA failure.
Morshed et al. [19] examined failure of THA defined as (1) revision of either or both components or (2) revision of a specific component and found no advantage for either cemented fixation or cementless fixation in their meta-analysis. Subgroup analysis by patient age found cemented fixation to have superior survival in studies containing patients of all ages but not in studies focused on younger patients (aged ≤55 years; P = .004) [19]. They found that neither the size of the study population nor the level of evidence of the study influences revision rates [19]. The authors looked further into the possible connection between year of publication and survival and found that cementless fixation showed a relative superiority over time, suggesting improvements in that technique and general cementless implant design [19].
Abdulkarim et al. [20] performed a meta-analysis of RCTs that compared cemented and cementless fixations in THA; the fixation method for both the femoral stem and the acetabular cup was the same, that is, there was no discussion of hybrid fixation in which the femoral stem is cemented and the acetabular cup is cementless. They found no significant difference between cemented and cementless fixations when implant survival was measured by revision rate (P = .14, n = 719) [20]. There was no difference in patient mortality (P = .77, n = 725) or postoperative complication rate (P = .67, n = 391) when comparing cemented and cementless fixations [20]. However, short-term clinical outcomes, particularly pain, were improved with cemented fixation (P = .04, n = 695) [20]. The results for long-term clinical and functional outcomes remain unclear based on the data available [20].
There is one systematic review with sufficient details to draw conclusions about fixation techniques for femoral stems: Ni et al. [21] performed a systematic review of literature comparing cemented and cementless femoral stems; the results were further subgrouped by study classification: random controlled trial, matched pairs, nonmatched pairs, and comparison in a single patient (bilateral studies, one side cemented and one side cementless). In general, short-term clinical and functional outcomes are better with cemented femoral stems [21]. For the random controlled trials, health-related quality of life and heterotopic ossification rates were not different when comparing cemented and cementless femoral stems, but the cementless group demonstrated increased thigh pain and reduced walking ability without support [21].
Results from meta-analyses/systematic reviews show that the differences between cemented and cementless fixations of primary THA are limited; cemented fixation has superior short-term clinical and functional outcomes [20], [21]. The usefulness for clinical application is not clear.
Large population data
Conclusions about revision rates, and to some extent the causes of revision, are possible by examining arthroplasty registry data and large insurance databases; there are 11 articles in our review that do so [22], [23], [24], [25], [26], [27], [28], [29], [30], [35], [36]. In addition, there are 3 recent registry reports that contain similar data [37], [38], [39].
Hailer et al. [22] found in the Swedish Registry that 10-year implant survival was better for cemented THA (94%) than for cementless THA (85%); this was mainly due to the high rate of aseptic loosening of cementless acetabular cups (P < .001). At 15-years, implant survival continued to favor cemented THA (88%) over cementless THA (70%). The risk of stem revision because of periprosthetic fracture within 2 years of primary THA was 8 times higher for cementless femoral stems than for cemented femoral stems (P < .001). The authors pointed out that unrecognized intraoperative femoral fractures might be an important reason for early failure of cementless femoral stems. Analysis of the Finnish Registry by other researchers found that overall implant survival at 10 years was better with proximally and extendedly porous-coated cementless femoral stems (91% and 89%) than with uncoated cementless (80%) or cemented stems (87%) [23], [24]. None of these 3 studies focused on specific implant designs although they did look at certain design elements such as the extent and type of coating on cementless femoral stems. In a different study, Engesaeter et al. [25] looked specifically at the interaction of cement technique and the risk of infection using data from the Norwegian Registry; cemented THA without antibiotic-impregnated cement was 1.8 times more likely to have revision because of infection than cementless THA (P = .04). There was no significant difference between cemented THA with antibiotic-impregnated cement and cementless THA (P = .5) [24]. Colas et al. [26] used the French National Health Insurance Information System to examine the differences in revision rates for THA, comparing cementless fixation, cemented fixation with and without antibiotic-impregnated cement, and hybrid fixation. The data set contained 100,191 patients aged at least 40 years who received their THA between April 2010 and December 2011. There was a significant decrease in the risk of revision in cemented THA with antibiotic-impregnated cement (2.4%, n = 21,467) vs cementless THA (3.3%, n = 74,917; P < .001).
The remaining articles discuss revision rates for age groups by comparing cemented and cementless fixations. The consensus across all national and 2 community registries is that older age and cementless fixation together increase the risk of revision [23], [24], [27], [28], [35], [36]. There is no absolute agreement on what constitutes “older age”—some registries define it as >65 years and others as 75 years. Jämsen et al. [27] looked at patients in the Finnish Registry who were of age ≥80 years at the time of THA. They found that for these patients during the first postoperative year, cementless femoral stems are associated with a 2.9 times higher rate of revision, especially female patients. The leading cause of failure is periprosthetic fracture in the first 12 months. After that initial year, there is no significant difference in survival rates of cemented and cementless femoral stems; however, the 10-year survival for THA is slightly lower for cementless (93.9%) than for cemented (97.4%) and hybrid (98.1%) constructs [27]. The authors note that they were unable to identify failures that did not result in revision surgery or intraoperative periprosthetic fractures which were treated during the primary THA because of quality of their data [27]. Examination of the Finnish Registry found that modern cementless femoral stems, proximally circumferentially porous coated, had a lower risk of aseptic loosening failure than cemented femoral stems in younger patients of age <55 years (relative risk: 5.5, P < .001) [23].
Mäkelä et al. have 2 articles looking at patients of intermediate age (55-64 years old), one based on data solely from the Finnish Registry and the other using data from 4 national registries: Sweden, Norway, Denmark, and Finland [24], [28]. In the study looking at data from the Finnish registry (published in 2008), the authors found that cementless femoral stems had a better 15-year survival than cemented femoral stems (91% cementless straight stems vs 77% cemented loaded-taper stems, P < .001) [24]. In the more recent study (published in 2014), using data from 4 registries, the fixation method did not make a difference for 15-year survival in patients 55-64 years of age (cemented fixation: 84.1% and cementless fixation: 82.8%) [28].
Patients in the younger age group (typically, aged <55 years) generally fare better with cementless femoral stems; however, date of index THA has an impact in the revision risk [23], [29], [30]. Havelin et al. [29] used the Norwegian Register and found that for patients aged <60 years, cementless femoral stems with circumferential porous coating, hydroxyapatite coating, or rough-blasted surface have better survival rates than cemented femoral stems (P < .0001). Eskelinen et al. [23] found that data in the Finnish Register showed that cementless femoral stems were better for patients aged <55 years, both for the risk of all revision (P < .002) and for the risk of revisions due to aseptic loosening (P < .001). The last article in this group also used the Finnish Register; Mäkelä et al. [30] found that the success of cementless femoral stems depended on when they were implanted: from 1987 to 1996, survival was better for cemented femoral stems and from 1997 to 2006, there was no difference in the survival of cemented and cementless femoral stems.
There are 3 recent national registry reports that provide results regarding the causes of revision [37], [38], [39]. The first, the Registro dell'implantologia Protesica Ortopedica (Register of the Orthopaedic Prosthetic Implants), known as the RIPO Report from the Emilia-Romagna region of Italy, reports the rates of revision for THA from 2000 to 2013; the rate of revision for cementless THA was higher than for cemented THA for aseptic loosening of the femoral stem, recurrent dislocation/subluxation, and periprosthetic fracture (Table 2) [37]. The difference in revision rates for recurrent dislocation and/or subluxation was very small (cementless: 16.8% vs cemented: 16.0%); dislocation of THA is somewhat dependent on surgical accuracy and may be less influenced by fixation [40]. The second, from the National Joint Registry of England, Wales and Northern Ireland, found similar results; revision for aseptic loosening, dislocation, and periprosthetic fracture was higher for cementless THA (Table 3); again, the smallest difference was for revision due to dislocation [38]. The Australian Orthopaedic Association (AOA) Registry Report found that cementless THA has a 2.2 times higher rate of revision in the first month than cemented THA [39]. The cumulative percent revision of primary THA is higher for cementless constructs than for cemented or hybrid constructs throughout the 11 years of data in the AOA Registry Report [39].
Table 2.
Rates of revision, as percent of failure cases for fixation method, from 2000 to 2013, RIPO 2013 Annual Report of Emilia-Romagna Region of Italy.
| Fixation method | Aseptic loosening of femoral stem (%) | Recurrent dislocation/subluxation (%) | Periprosthetic fracture (%) |
|---|---|---|---|
| Cemented | 11.7 | 16.0 | 6.8 |
| Uncemented | 15.6 | 16.8 | 12.4 |
Table 3.
Revision rates, expressed as number per 1000 patient-years, from the National Joint Registry of England, Wales and Northern Ireland.
| Fixation method | Aseptic loosening | Dislocation/subluxation | Periprosthetic fracture |
|---|---|---|---|
| Cemented | 0.96 (0.90-1.02) | 0.88 (0.83-0.94) | 0.33 (0.30-0.37) |
| Uncemented | 1.92 (1.82-2.01) | 1.20 (1.13-1.28) | 0.81 (0.76-0.88) |
The data are presented as % (95% CI).
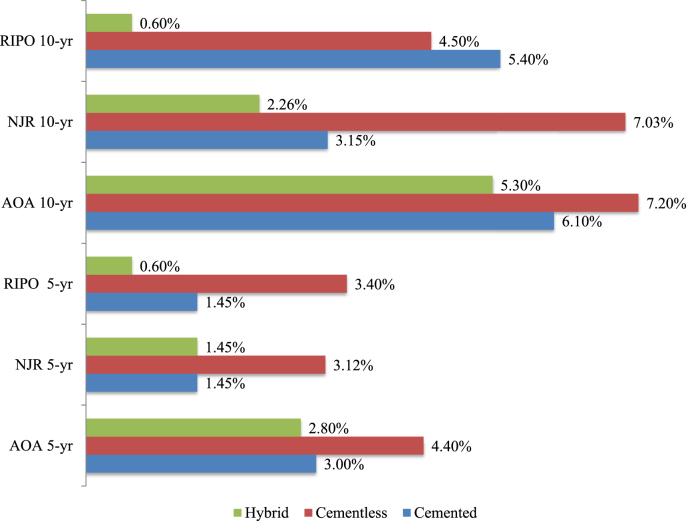
Both the RIPO and the National Joint Registry reports provide limited information that allows comparison of risk of failure for implant designs; the most popular constructs are the cementless Corail femoral stem and Pinnacle acetabular cup (DePuy, Warsaw, IN), the cemented Exeter femoral stem, and Contemporary acetabular cup (Stryker, Kalamazoo, MI), and the hybrid construct with the cemented Exeter femoral stem and the cementless Trident cup (Stryker, Kalamazoo, MI). The AOA Registry Report, while noting that the Exeter is the most common cemented implant and the Corail is the most common cementless femoral stem, the details surrounding the most common hybrid construct are not available. The most common cemented femoral stem, whether in a totally cemented construct or in a hybrid construct, was a highly-polished, double-taper, and collarless stem. Interestingly, the failure rates for hybrid constructs (cemented femoral stems and cementless acetabular cups) were consistently lower than those for the totally cemented and totally cementless constructs at 5 years and at 10 years (Fig. 2). Cementless THA has a higher cumulative revision rate than other constructs with one exception, cemented THA at 10-years in the RIPO Registry Report (Fig. 2).
Figure 2.
Cumulative percent revision for 3 major registry reports. NJR, National Joint Registry.
Qualitative analysis of primary research
The qualitative analysis contains 5 articles that directly compare cemented and cementless femoral stems: 4 are of level I quality (RCTs) and one is of level III quality (retrospective controlled trials), as described in by the Oxford Centre for Evidence-Based Medicine [31], [32], [33], [34], [41], [42]. The reason that this is a qualitative analysis rather than a meta-analysis is due to 2 primary reasons: (1) lack of consistency when reporting outcomes and (2) absence of complete sets of data, for example, sample size, mean, and standard deviation. It should be noted that none of the femoral stem designs in this section are collarless, polished, tapered designs such as those detailed in the previous section.
The objective of Strom et al. [31], a level I study, was to compare femoral stem fixation in young patients of age <65 years. Two femoral stem designs were used: the Cone stem was used in all cementless cases (n = 22) and the Bimetric (Biomet, Warsaw, IN) grit-blasted femoral stem was used in all cemented cases (n = 23). All the femoral stems were radiographically stable, regardless of cement fixation. There were no radiolucent lines in the cemented group but the cementless group had six (27%).
In a different level I study, Lindalen et al. [32] did not discuss revisions; instead, they examined surgical variables and hip scores. The cemented collared femoral stems were Spectron EF (Smith and Nephew, London, UK; n = 24), and the cementless stems were Taperloc (Biomet, Warsaw, IN) (n = 22). Both groups had improvements in Harris Hip Scores and Oxford Hip Scores at the minimum 2-year follow-up, and there was no difference in the final scores. Operating time was slightly longer in the cemented femoral stem group (85 minutes vs 77 for the cementless group, P = .05); however, blood loss was lower in the cemented stem group (674 vs 740 mL for the cementless group, P = .3).
Kim [33] performed bilateral cemented and cementless THAs on 70 patients aged <50 years (mean age, 39.9) and followed the patients for a minimum of 6 years (mean follow-up, 7.8 years) in this level I study. Cementless Profile femoral stems (DePuy, Leeds, UK) were used in 70 hips, and the contralateral side was implanted with Cemented Elite Plus femoral stems; neither of these are collarless nor smooth (DePuy, Leeds, UK). There were no incidents of transitory thigh pain at last follow-up, and there were no reoperations due to aseptic loosening in either group. The cemented group had more radiolucent lines (n = 9, 12.86%) than the cementless group (n = 3, 4.29%), but the cementless group had a higher incidence of osteolysis (n = 9, 12.86%) than the cemented group (n = 6, 8.57%). Each group experienced 3 dislocations after surgery, but fractures of the calcar and displaced fractures of the femur were only reported in the cementless group (3 each, 4.29%).
In a level III study with a minimum 2-year follow-up, Emerson et al. [34] followed 102 cemented and collared stems (Mallory-Head Interloc; Biomet, Warsaw, IN) and 78 cementless femoral stems (Mallory-Head circumferential porous coated; Biomet, Warsaw, IN). There were no trochanteric fractures and no revisions due to infection in either group. There was a higher incidence of femoral osteolysis in the cemented group (n = 22, 21.6%) than with the femoral implant used in the cementless group (n = 7, 8.97%; P = .016). The cementless group experienced no revisions, whereas the cemented group had a single revision for femoral fracture and 9 revisions for aseptic loosening. The survivorship of the cementless group was 100% and 84% for the cemented group at 10-year follow-up.
Discussion
The results of our systematic review do not provide conclusive evidence that one form of femoral stem fixation is demonstratively better for all patients. However, when stratified by age, older patients with cementless fixation demonstrate an increased risk of revision [19], [22], [24], [26], [27], [28], [35], [36]. Taking into account revision rates in midaged patients, 55-64 years, our results do not present a clear advantage for either mode of fixation [24], [28]. Younger patients, aged <55 years typically, fare better in terms of revision rates with cementless fixation [19], [23], [29], [30]. Short-term outcomes such as pain and independent walking ability are improved with cemented fixation [20], [21]. Multiple sources agree that cementless fixation increases the risk of periprosthetic fracture [22], [37], [38], [39], [43], [44], [45]. However, the risk of revision due to aseptic loosening does not demonstrate dominance for either fixation method [23], [24], [37], [38], [39].
The direct cost of primary THA is made up of many factors including implant costs, hospital costs, and professional fees. After primary THA, there are often secondary costs associated with complications, readmissions, infections, reoperations, and revisions. Some of these are not too difficult to calculate, but the impact on patient welfare, their families, and their caregivers is difficult to quantify.
The direct costs of primary THA are somewhat easier to calculate. The 8th Annual National Joint Registry Report found that the cost of a primary cemented femoral component plus the associated cement and accessories is £820 per THA, whereas the cost of a primary cementless femoral component was £915 per THA [46], [47]. Similar data from the United States agree that cementless femoral prostheses are consistently more expensive than cemented femoral prostheses even when including the cost of cement plus accessories [14]. The indirect primary costs such as quality of life and patient satisfaction should be combined with the direct primary THA costs to fully determine value. A further study of the costs and quality of life for THA looked at data from the National Health Service of England and found that cemented THA has the lowest lifetime costs, hybrid THA has the highest quality of life and the highest quality-adjusted life years making it the most cost-effective fixation option, and cementless THA does not provide sufficient improvement to justify the higher cost [48].
The overall cost of revision THA such as treating complications, readmissions, the associated morbidity and mortality, and the impact on patient welfare and satisfaction are all part of the value equation. According to data from the 8th Annual National Joint Registry Report, there was an annual increase of 9.8% for revision THA and the costs to the National Health System was £1.5B and are expected to rise [15], [47]. Märdian et al. [12] focused on one complication, periprosthetic fracture, and the implications to patient welfare and mortality. Elderly patients, in particular, often have a perceptible decline in function compared to the normal population, remarkably high complication rates (25.4%) after postoperative periprosthetic fracture; many of these patients do not recover preoperative ambulatory status. Periprosthetic fracture was found more frequently in cementless THA than in cemented THA. Most surprisingly, within 3 years of periprosthetic fractures, over 50% of patients have died [12].
The implications of a growing demand for THA coupled with a possible increased incidence of early complications and reoperations are likely to have an increasing adverse effect on the economic sustainability of the current health care system. All of these are now being closely monitored and reported, and soon will be directly linked to reimbursement and compensation, and most likely have an impact on public health care services [9].
The early complications from cementless femoral stems are clear; fibrous ingrowth, aseptic loosening, thigh pain, leg length discrepancy, and periprosthetic fracture contribute to the likelihood of secondary or revision surgery [2], [3], [4], [5], [6], [7], [49], [50]. These early complications have been shown to occur at lower rates with cemented femoral stems in most populations [2], [3], [4], [5], [6], [7], [49], [50]. With these secondary reoperations, there is an increase in the risk for dislocation, wound difficulties, infection and an overall increase in costly health care needs as well as increases in morbidity and mortality. The cost relative to human pain and to risks inherent with repeated surgery is not to be ignored. We should be “getting it right first time” by using the most reliable implants with proven survivorship to contain costs and complications [15].
There is limited information concerning the impact of femoral stem design features [16], [27], [51], [52]. Highly-polished, tapered, collarless cemented stems work well because they are very forgiving in practice and it is easier to achieve accurate leg length, anteversion, and neck offset [16]. The Exeter femoral stem is a highly-polished, collarless, double-taper design that has been in use for many years. There is an indication of “settling-in” from Jämsen et al. [27]; the unadjusted survival of Exeter stems has a weak tendency to be less steep after 4 or 5 months after primary THA. Howie et al. [51] found that the cemented Exeter stem has very good long-term survivorship in young patients: survivorship for loosening at 13 years is 100% and survivorship for all reasons at 13 years is 97% (95% CI: 93%-100%). Ling et al. [52] looked at the original Exeter stem; they found excellent long-term survivorship (over 30 years) for aseptic loosening although old cementing techniques were used (93.5%, 95% CI: 90.0%-97.0%).
The most important limitation of this systematic review is the lack of congruency of available data such as revisions, reasons for revisions, survivorship analysis, complications, and clinical and functional outcomes. The lack of standardized methods of reporting outcomes, even among the various national and international joint registries, makes it rather complex to make comparisons, and thus, creating evidence-based conclusions can be difficult. However, this condition is not limited to this systematic review; these difficulties exist throughout a majority of medical literature.
The second limitation is the difficulty in determining implant and fixation utilization. It is common to discover a good, thorough article but the utilization is “unclear”; there may be a variety of implants used, but the results are comingled so that the effect of implant design cannot be determined or delineated.
A possible third limitation, or perhaps something to consider when looking at registry data, is that cementless fixation of femoral stems is a much younger data set than cemented fixation; thus, there is the possibility that the newer technique is influenced by a shorter evolution of practice.
This literature summary has made an effort to extrapolate as much data as possible from as many sources as possible, and other meta-analyses/systematic reviews, clinical and safety studies of all levels of evidence, and registry reports were scrutinized in efforts to determine what the evidence currently reveals about the use of cemented and cementless femoral stems.
Conclusions
Using evidenced-based data, in conjunction with information provided by joint registries, should help provide better guidance on selecting the most reliable implants with proven survivorship lowering early postoperative complications, readmissions, reoperation and revision burdens, and health care costs, along with improving patient satisfaction and overall outcomes especially in the growing elderly populations, osteoporotic and at-risk subgroup of patients with poor bone quality undergoing THA. The authors feel that despite the apparent observation that cementless femoral fixation for THA has evolved as the accepted “new standard,” it still has not been proven to be the “gold standard” for all patients. Revisiting the use of contemporary cement techniques, in conjunction with proven femoral implant designs that have excellent evidenced-based survivorship, warrants strong consideration for several subgroups of patients undergoing elective THA, thus increasing the likelihood of “getting it right the first time” and decreasing the incidence of early complications and associated morbidity and mortality of reoperations.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.02.001.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.artd.2016.02.001
Appendix A. Supplementary data
References
- 1.Lehil M.S., Bozic K.J. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014;29(10):1915. doi: 10.1016/j.arth.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Cook R.E., Jenkins P.J., Walmsley P.J., Patton J.T., Robinson C.M. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res. 2008;466(7):1652. doi: 10.1007/s11999-008-0289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sidler-Maier C.C., Waddell J.P. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop. 2015;39(9):1673. doi: 10.1007/s00264-015-2721-y. [DOI] [PubMed] [Google Scholar]
- 4.Franklin J., Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007;38(6):655. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 5.Katz J.N., Wright E.A., Polaris J.J., Harris M.B., Losina E. Prevalence and risk factors for periprosthetic fracture in older recipients of total hip replacement: a cohort study. BMC Musculoskelet Disord. 2014;15:168. doi: 10.1186/1471-2474-15-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berend M.E., Smith A., Meding J.B. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty. 2006;21(6 Suppl 2):53. doi: 10.1016/j.arth.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Ehlinger M., Bahlau D., Rahme M., Adam P., Bonnomet F. Has a patient type with peri-prosthetic femoral fractures evolved? Int Orthop. 2015;39(9):1833. doi: 10.1007/s00264-015-2873-9. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S.M., Ong K.L., Schmier J. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89 Suppl 3:144. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 9.Maradit Kremers H., Larson D.R., Crowson C.S. Prevalence of total hip and knee replacement in the united states. J Bone Joint Surg Am. 2015;97(17):1386. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thien T.M., Chatziagorou G., Garellick G. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the Nordic arthroplasty register association database. J Bone Joint Surg Am. 2014;96(19):e167. doi: 10.2106/JBJS.M.00643. [DOI] [PubMed] [Google Scholar]
- 11.Sadoghi P., Liebensteiner M., Agreiter M. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013;28(8):1329. doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Märdian S., Schaser K.D., Gruner J. Adequate surgical treatment of periprosthetic femoral fractures following hip arthroplasty does not correlate with functional outcome and quality of life. Int Orthop. 2015;39(9):1701. doi: 10.1007/s00264-015-2673-2. [DOI] [PubMed] [Google Scholar]
- 13.Donaldson A., Thomson H., Harper N., Kenny N. Bone cement implantation syndrome. Br J Anaesth. 2009;102(1):12. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 14.Unnanuntana A., Dimitroulias A., Bolognesi M.P. Cementless femoral prostheses cost more to implant than cemented femoral prostheses. Clin Orthop Relat Res. 2009;467(6):1546. doi: 10.1007/s11999-008-0485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng Man Sun S., Gillott E., Bhamra J., Briggs T. Implant use for primary hip and knee arthroplasty: are we getting it right first time? J Arthroplasty. 2013;28(6):908. doi: 10.1016/j.arth.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Murray D.W. Cemented femoral fixation: the North Atlantic divide. Bone Joint J. 2013;95-B(11 Suppl A):51. doi: 10.1302/0301-620X.95B11.32976. [DOI] [PubMed] [Google Scholar]
- 17.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions. Explanation and elaboration. BMJ. 2009;339:2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D., Altman D.G., Liberati A., Tetzlaff J. PRISMA statement. Epidemiology. 2011;22:128. doi: 10.1097/EDE.0b013e3181fe7825. [DOI] [PubMed] [Google Scholar]
- 19.Morshed S., Bozic K.J., Ries M.D., Malchau H., Colford J.M. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78(3):315. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 20.Abdulkarim A., Ellanti P., Motterlini N., Fahey T., O'Byrne J.M. Cemented versus uncemented fixation in total hip replacement: a systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia) 2013;5(1):e8. doi: 10.4081/or.2013.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ni G.X., Lu W.W., Chiu K.Y., Fong D.Y. Cemented or uncemented femoral component in primary total hip replacement? A review from a clinical and radiological perspective. J Orthop Surg (Hong Kong) 2005;13(1):96. doi: 10.1177/230949900501300119. [DOI] [PubMed] [Google Scholar]
- 22.Hailer N.P., Garellick G., Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish hip arthroplasty register. Acta Orthop. 2010;81(1):34. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eskelinen A., Remes V., Helenius I. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0–22 years. Acta Orthop. 2005;76(1):28. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 24.Mäkelä K.T., Eskelinen A., Pulkkinen P., Paavolainen P., Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90(10):2160. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 25.Engesaeter L.B., Espehaug B., Lie S.A., Furnes O., Havelin L.I. Does cement increase the risk of infection in primary total hip arthroplasty? Revision rates in 56,275 cemented and uncemented primary THAs followed for 0–16 years in the Norwegian arthroplasty register. Acta Orthop. 2006;77(3):351. doi: 10.1080/17453670610046253. [DOI] [PubMed] [Google Scholar]
- 26.Colas S., Collin C., Piriou P., Zureik M. Association between total hip replacement characteristics and 3-year prosthetic survivorship: a population-based study. JAMA Surg. 2015;150:979. doi: 10.1001/jamasurg.2015.1325. [DOI] [PubMed] [Google Scholar]
- 27.Jämsen E., Eskelinen A., Peltola M., Mäkelä K. High early failure rate after cementless hip replacement in the octogenarian. Clin Orthop Relat Res. 2014;472(9):2779. doi: 10.1007/s11999-014-3641-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mäkelä K.T., Matilainen M., Pulkkinen P. Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. BMJ. 2014;348:f7592. doi: 10.1136/bmj.f7592. [DOI] [PubMed] [Google Scholar]
- 29.Havelin L.I., Engesaeter L.B., Espehaug B. The Norwegian arthroplasty register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000;71(4):337. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 30.Mäkelä K.T., Eskelinen A., Pulkkinen P., Paavolainen P., Remes V. Results of 3,668 primary total hip replacements for primary osteoarthritis in patients under the age of 55 years. Acta Orthop. 2011;82(5):521. doi: 10.3109/17453674.2011.618908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ström H., Kolstad K., Mallmin H., Sahlstedt B., Milbrink J. Comparison of the uncemented cone and the cemented Bimetric hip prosthesis in young patients with osteoarthritis: an RSA, clinical and radiographic study. Acta Orthop. 2006;77(1):71. doi: 10.1080/17453670610045713. [DOI] [PubMed] [Google Scholar]
- 32.Lindalen E., Dahl J., Nordsletten L. Reverse hybrid and cemented hip replacement compared using radiostereometry and dual-energy x-ray absorptiometry: 43 hips followed for 2 years in a prospective trial. Acta Orthop. 2012;83(6):592. doi: 10.3109/17453674.2012.742393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim Y. Bilateral cemented and cementless total hip arthroplasty. J Arthroplasty. 2002;17(4):434. doi: 10.1054/arth.2002.31073. [DOI] [PubMed] [Google Scholar]
- 34.Emerson R.H., Head W.C., Emerson C.B., Rosenfeldt W., Higgins L.L. A comparison of cemented and cementless titanium femoral components used for primary total hip arthroplasty: a radiographic and survivorship study. J Arthroplasty. 2002;17(5):584. doi: 10.1054/arth.2002.32696. [DOI] [PubMed] [Google Scholar]
- 35.Troelsen A., Malchau E., Sillesen N., Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013;471(7):2052. doi: 10.1007/s11999-013-2941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stea S., Comfort T., Sedrakyan A. Multinational comprehensive evaluation of the fixation method used in hip replacement: interaction with age in context. J Bone Joint Surg Am. 2014;96(Suppl 1):42. doi: 10.2106/JBJS.N.00463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Report of R.I.P.O. Regional Register of Orthopedic Prosthetic Implantology. 2015. https://ripo.cineca.it/pdf/relazione_2014_inglese_rev1.pdf [accessed 24.08.15] [Google Scholar]
- 38.NJR England, Wale & Northern Ireland: 11th Annual Report. 2014. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/11th_annual_report/NJR%2011th%20Annual%20Report%202014.pdf [accessed 07.05.15] [Google Scholar]
- 39.Australian Orthopaedic Association . 2012. Hip and knee arthroplasty. Annual Report of the National Joint Replacement Registry. https://aoanjrr.sahmri.com/documents/10180/217745/Hip%20and%20Knee%20Arthroplasty. [accessed 12.08.15] [Google Scholar]
- 40.Moskal J.T., Capps S.G., Scanelli J.A. Improving the accuracy of acetabular component orientation: avoiding malpositioning: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95(11):e761. doi: 10.2106/JBJS.L.00685. [DOI] [PubMed] [Google Scholar]
- 41.Laupacis A., Bourne R., Rorabeck C. Comparison of total hip arthroplasty performed with and without cement : a randomized trial. J Bone Joint Surg Am. 2002;84-A(10):1823. doi: 10.2106/00004623-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 42.OCEBM Levels of Evidence Working Group*.“The Oxford Levels of Evidence”. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653. [accessed 26.03.15].
- 43.Abdel MP, Watts C, Lewallen DG, Berry DJ. Characterization of periprosthetic femur fractures in 32,644 primary total hip arthroplasties. Proceedings AAOS 2014, New Orleans, LA. 2014; Paper #307.
- 44.Pivec R, Issa K, Kapadia B, et al. Incidence of projected periprosthetic femoral fracture following THA: an analysis of international registry data. Proceedings AAOS 2014, New Orleans, LA. 2014; Poster No. P035.
- 45.Streit M.R., Merle C., Clarius M., Aldinger P.R. Late peri-prosthetic femoral fracture as a major mode of failure in uncemented primary hip replacement. J Bone Joint Surg Br. 2011;93(2):178. doi: 10.1302/0301-620X.93B2.24329. [DOI] [PubMed] [Google Scholar]
- 46.Griffiths E.J., Stevenson D., Porteous M.J. Cost savings of using a cemented total hip replacement: an analysis of the national joint registry data. J Bone Joint Surg Br. 2012;94(8):1032. doi: 10.1302/0301-620X.94B8.28717. [DOI] [PubMed] [Google Scholar]
- 47.8th Annual Report. National Joint Registry for England and Wales; 2011. http://www.njrcentre.org.uk/njrcentre/portals/0/documents/njr%208th%20annual%20report%202011.pdf. [accessed 07.05.15] [Google Scholar]
- 48.Pennington M., Grieve R., Sekhon J.S. Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ. 2013;346:f1026. doi: 10.1136/bmj.f1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahmad R., Gillespie G., Annamalai S. Leg length and offset following hip resurfacing and hip replacement. Hip Int. 2009;19(2):75. doi: 10.1177/112070000901900210. [DOI] [PubMed] [Google Scholar]
- 50.Whittingham-Jones P., Williams D., Raja S., Bridle S., Bircher M. Negligence claims in UK total hip arthroplasty: a series of 167 consecutive cases. Med Leg J. 2012;80(4):157. doi: 10.1258/mlj.2012.012027. [DOI] [PubMed] [Google Scholar]
- 51.Howie D.W., Costi K., McGee M.A., Standen A., Solomon L.B. Femoral bone is preserved using cemented polished stems in young patients. Clin Orthop Relat Res. 2012;470(11):3024. doi: 10.1007/s11999-012-2327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ling R.S., Charity J., Lee A.J. The long-term results of the original Exeter polished cemented femoral component: a follow-up report. J Arthroplasty. 2009;24(4):511. doi: 10.1016/j.arth.2009.02.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.