Abstract
Background
The results of ceramic-on-ceramic (CoC) total hip arthroplasty (THA) in younger patients were not univocal. This study aims to evaluate the results of CoC bearing THA in patients younger than 50 years.
Methods
A total of 90 younger patients performed CoC THAs during March 2003 and May 2008 were included in this study. Hip function and activity were evaluated with Harris hip score and University of California Los Angeles activity score. We had discussed survival rates, radiological findings of component loosening or osteolysis, and ceramic-related complications in these patients.
Results
The mean Harris hip score increased from 46.3 ± 12.0 points (range, 28-70 points) before surgery to 92.5 ± 5.6 points (range, 78-100 points) at the final follow-up. The mean preoperative University of California Los Angeles activity score was 4.2 ± 1.1 points (range, 2-6 points), which improved to a mean of 7.2 ± 1.3 points (range, 4-10 points). At the time of the last follow-up, there was found to be 1 occurrence of hip dislocation, 1 squeaking, and 2 “sandwich” ceramic liners fractured during normal activity of daily living. No hips showed osteolysis or required revision for aseptic loosening. Kaplan-Meier survivorship with revision due to loosening or osteolysis was 100% and with revision due to ceramic fracture was 97.3% (95% confidence interval, 93.7%-100%) at a mean of 9.4 years.
Conclusions
This study with the use of CoC bearings THAs in younger patients have shown promising results and higher rate of survivorship without evidence of osteolysis.
Keywords: Ceramic-on-ceramic bearings, Total hip arthroplasty, Younger patients, Activity level
Introduction
Total hip arthroplasty (THA) is among the most successful surgical operations because it relieves pain and restores hip function and mobility for various end-stage degenerative conditions of the hip joint [1], [2]. Although THA was initially designed for elderly low-demanding patients, the benefit of this procedure in younger populations has also been well documented; thus, long-term results have increasingly improved over the last decades [3], [4], [5]. However, the consequences of bearing surface wear, including osteolysis and aseptic loosening, have been a leading reason of late revision THA, especially in younger and more active patients. Therefore, extended longevity of bearing can meet the increasing demand among younger and more active patients requiring hip replacement; such demand is increasingly becoming an important issue.
Hard-on-hard bearing couples, including metal-on-metal (MoM) and ceramic-on-ceramic (CoC), which are regarded as the optimal choice for the younger and more active patients [6], [7], [8], offer the potential to decrease the prevalence of revision THA caused by bearing surface-related failures. However, concerns on the use of MoM bearings exist because they are associated with elevated metal ion levels and adverse local tissue reactions [9]. Conversely, the advantage of CoC bearing is not only the complete avoidance of metal debris but also the reduced risk of wear-induced osteolysis over ultrahigh molecular weight polyethylene. Many studies have reported that the long-term clinical and radiographic results of CoC bearings were promising. However, the long-term results of CoC THAs in younger patients have not been univocal [10], [11]. Therefore, the purposes of this study were to summarize the following: (1) the clinical results with CoC cementless THA in younger and more active patients; (2) the survival rate of the CoC bearing THAs; and (3) the results of the activity level, work experience, and career choice.
Material and methods
We retrospectively reviewed the medical records of patients who underwent THA from March 2003 to March 2008. Inclusion criteria consisted of patients aged <50 years undergoing primary THAs without cement. A total of 100 primary THAs performed in 93 patients qualified for this study. Of these, 3 patients (3 hips) were lost to follow-up. The remaining 90 patients (97 hips) were available for a complete analysis. The mean patient age at surgery was 39.0 ± 8.2 years (range, 19-50 years old). Forty (44.4%) patients were male and 50 (55.6%) were female. The mean body weight (and standard deviation) was 64.5 ± 9.9 kg (range, 40-89 kg), and the mean body mass index was 23.25 ± 2.95 kg/m2 (range, 16.65-30.44 kg/m2). The preoperative diagnostic reasons were avascular necrosis of femoral head in 36 hips, developmental dysplasia of the hip in 23 hips, ankylosing spondylitis in 5 hips, posttraumatic arthritis in 6 hips, primary degenerative arthritis in 15 hips, femoral neck fracture in 7 hips, and rheumatologic disease in 5 hips (Table 1). This study was approved by our institute’s ethics committee.
Table 1.
Demographic patient data and preoperative diagnosis for this study.
| Characteristic | Number |
|---|---|
| Number of patients (hips) | 90 (97) |
| Gender (male/female) | 36/54 |
| Age (, y) | 39.0 ± 8.2 (17-45) |
| Weight (, kg) | 64.5 ± 9.9 (40-89) |
| BMI (, kg/m2) | 23.25 ± 2.95 (16.65-30.44) |
| Preoperative diagnosis (number of patients/hips) | |
| Avascular necrosis of femoral head | 33/36 |
| DDH | 21/23 |
| Posttraumatic arthritis | 6/6 |
| Ankylosing spondylitis | 4/5 |
| Femoral neck fracture | 7/7 |
| Primary degenerative arthritis | 15/15 |
| Rheumatoid arthritis | 4/5 |
DDH, developmental dysplasia of the hip.
All recorded cementless THAs were performed by the same surgeon through a modified Harding approach. The acetabular component were the SPH Contact acetabular component (Lima-Lto, Italy; n = 57) or Duraloc (DePuy, Warsaw, IN, USA; n = 40). The acetabular cup was fixed with an inclination angle at 40°-45° and anteversion at 15°-25° after the acetabular had been reamed. On the femoral side, the femoral components were the C2 stem (Lima-LTO, Italy) or Corail stem (DePuy) in 57 and 40 hips, respectively. Sizes of femoral heads were 28 mm in all hips. The third-generation CoC bearing THAs, including the “sandwich” (Lima-Lto) and the BIOLOX Forte ceramic (Biolox Forte, CeramTec, Germany), were 57 and 40 hips, respectively.
The patients received antibiotic prophylaxis at 0.5 hours before surgery and continued for 48 hours after surgery. Patients were instructed to walk with crutches for toe-touch partial weight bearing for 3 weeks after surgery, except for developmental dysplasia of the hip patients who had femoral shortening osteotomy. Afterward, they were allowed to bear their weight as tolerated using 2 crutches for the next 4-6 weeks.
Clinical and radiographic evaluations were performed at 6 weeks, 3 and 6 months, and 1 year after surgery and annually thereafter. Patients were clinically evaluated for pain, walking, and range of motion using the Harris hip scores (HHSs) system [12]. The level of activity of the patients after THA was assessed with the University of California Los Angeles (UCLA) activity score [13] and Devane activity level scale [14]. Job and occupational choice was assessed by a questionnaire [15] (Table 2).
Table 2.
A questionnaire regarding job and occupation choice.
|
Radiographic postoperative evaluation consisted of anteroposterior and lateral views of the hip and pelvis and a true lateral view of the hip for cup position, osteolysis, implant loosening, and ceramic fracture. Cup position was assessed according to the acetabular abduction angle and the anteversion angle on the picture archiving and communication system, digital radiograph system with use of the method of Murray [16] and Levinnek et al. [17]. Osteolysis was recorded at the acetabulum according to the zone described by DeLee and Charnley [18] and at the femoral component as described by Gruen et al. [19]. Loosening of the acetabular and femoral components was categorized according to previously accepted criteria [20], [21]. Bony ingrowth was described according to the criteria of Engh et al. [21]. Heterotopic ossification was classified according to the system of Brooker et al. [22].
Statistical methods
The statistical analysis was performed using the SPSS19.0 (Chicago, Illinois, USA) statistical software system. Survivorship analysis was performed with the Kaplan-Meier method. Revision for osteolysis and loosening was regarded as one end point, and revision due to ceramic fracture at the time of follow-up was regarded as another end point. We determined differences in continuous variances between the preoperative and postoperative scores using a t-test for independent samples. The level of significance was set at P < .05.
Results
Ninety patients (100 hips) were available for analysis. The mean patient follow-up was 9.4 ± 1.6 years (range, 7-12 years). All wounds healed uneventfully. No postoperative incisional infections and nerve and vascular injuries were observed. Two “sandwich” ceramic liners were fractured during normal activity of daily living after 7 and 9 years, respectively. One patient reported postoperative falling events at their bedside. A squeaking noise was heard in the left hip of a bilateral THA after 18 months, and it disappeared after 4 days. Acetabular abduction and anteversion were 37°and 17°, respectively. Heterotopic ossification developed in 10 hips by the time of the last follow-up. Six hips had grade I ossification, whereas 4 hips had grade II ossification.
A significant improvement in function was observed as measured with the HHS and UCLA scores. Mean preoperative HHS was 46.3 ± 12.0 points (range, 28-70 points) and improved to 92.5 ± 5.6 points (range, 78-100 points) at the final follow-up (P = .00 < .05). Of the patients, 83 showed excellent results (80-100), whereas 7 had fair result (70-79). Mean preoperative UCLA scores were 4.2 ± 1.1 points (range, 2-6 points) and this improved to 7.2 ± 1.3 points (range, 4-10 points) at the last follow-up (P = .00 < .05). According to the activity level scale of Devane et al., 13 patients were graded as level 5, 53 were graded as level 4, 20 were graded as level 3, and 4 were graded as level 2 in our series. About 95.6% of patients were able to participate regularly in leisure activities, such as gardening, swimming, and daily routines; 14.4% of them could perform strenuous manual labor. Eight patients had changed their work involving heavy labor before the operation to light manual work after it. Twelve patients were unemployed after operation. The remaining 70 patients were back to work after operation, and most of them engaged in sedentary work, such as office and manual work.
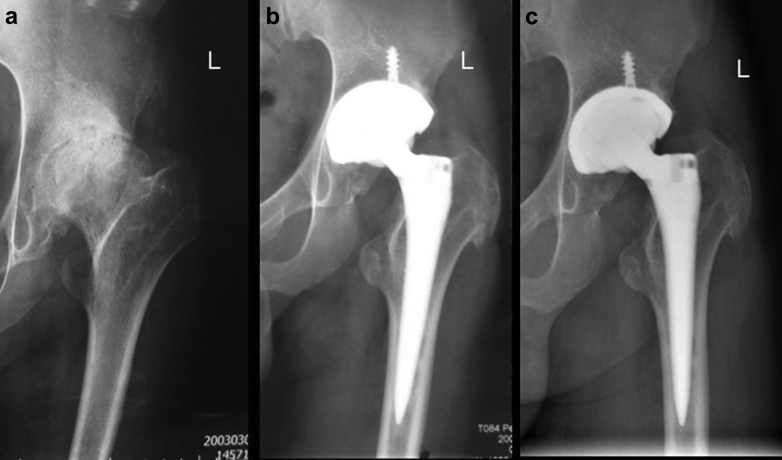
All 97 hips showed radiographic evidence of osseointergration at last follow-up. The mean abduction angle and anteversion of the acetabular component were 39.9° ± 6.3° (range, 26°-56°), 15.2° ± 4.51° (range, 8°-26°), respectively. No acetabular component or femoral stem showed radiographic signs of loosening, and no periprosthetic osteolysis was observed around any acetabular cup or femoral stem (Fig. 1).
Figure 1.
Preoperative anteroposterior radiograph of a left femoral head necrosis in a 37-year-old man (a). Anteroposterior radiograph at 7 days after operation with the third CoC bearing THA (b). Anteroposterior radiograph at 11 years postoperatively showing no evidence of osteolysis or loosening (c).
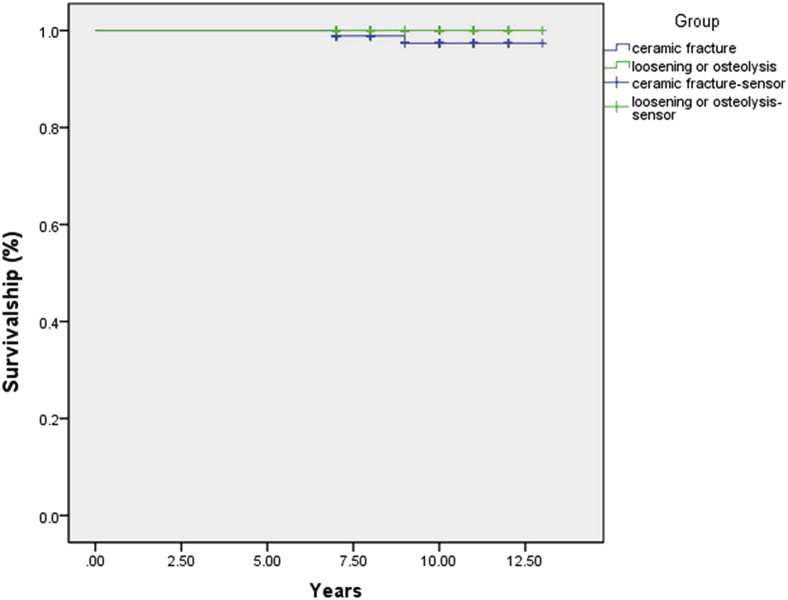
Kaplan-Meier survivorship as an end point of revision for loosening or osteolysis was 100% at mean 9.4 years. Survivorship rate with revision for ceramic fracture was 97.3% (95% confidence interval, 93.7%-100%) (Fig. 2).
Figure 2.
Kaplan-Meier survival curves with revision due to loosening or osteolysis and ceramic fracture as an end point, respectively.
Discussion
CoC bearing THA has been developed first in the 1970s by the French orthopaedic surgeon Pierre Boutin [23], [24]. To date, the ceramic component has developed for 4 generations. The early generation of ceramic component has a high failure rate because of flaws of the design and technology. O’leary et al. [25] reported 69 hips, of which 19 hips (27.2%) were revised and with an average time to revision of 26.2 months. With the development of the design and manufacturing process of ceramics, contemporary CoC bearings have shown better mechanical and superior wear characteristics compared with the early generation ceramics [2]. Wear rate was calculated to be 1000 times less than metal-on-polyethylene and 40 times less than MoM bearing surfaces. In our study, we used the third-generation CoC bearing, resulting in no osteolysis induced by ceramic debris. Capello et al. [26] reported a prospective, randomized, multicenter study of alumina ceramic-on-alumina ceramic bearing couples, where osteolysis was seen in only 4 (1.4%) of 287 hips with ceramic bearings compared with 25 (30.5%) of the control group with a traditional mental-on-polyethylene bearing surfaces. Topolovec et al. [27] compared 4 different bearing couples with a detailed radiographic analysis from the same period. Osteolysis was observed in 13 hips (2.95%, 13/441 hips) in the metal-on-polyethylene group compared with 2 hips (0.76%, 2/263 hips) in the CoC group. Kim et al. [28] also investigated a retrospective study that no acetabular or femoral osteolysis was detected in any hip through radiograph and computed tomography scan for an average of 11.1 years (follow-up). Some clinical data also demonstrated that CoC bearing couples had no adverse reaction to wear debris at 10-20 years [29]. The study by Yoon et al. [30] reported that the histological examination has identified wear debris with individual macrophages in the periprosthetic tissue of CoC bearings at revision, but the limited quantity or relative inertness of debris did not generate the foreign body granuloma necessary to trigger the osteolytic reaction. Therefore, CoC bearing THAs significantly reduces the wear rate because it avoids osteolysis, which is common in traditional polyethylene wear debris and improves the longevity of the component.
When THA success has been confirmed, returning to work and taking exercises became our clinical goal and the patients’ expectation, especially among younger and more active patients [31], [32]. Sechriest et al. [33] found that UCLA scores were positively correlated with postoperative HHSs (r = 0.52, P = .001). Ollivier et al. [32] indicated that the clinical outcomes and functional improvement were greater in high-impact sport group compared with the low-activity group. Lubbeke et al. [34] also noticed that patients with the highest activity (as evaluated by UCLA score) had the best outcome and highest satisfaction after surgery. In this study, UCLA scores were significantly improved from preoperative to postoperative (P < .05). Patients with high UCLA scores also have high HHS, and this result was similar to results obtained by Lubbeke et al. [34] and Sechriest et al. [33]. In addition, the results from our study also showed that THA affects patients’ occupation choice. Eight patients (8.9%) changed their job from heavy labor to light manual labor because they were worried about their hip problems. Eighteen patients (13.3%) did not work after THA because of their hip condition, although most of them stated that they considered THA when choosing a job.
In recent years, improvements in manufacturing process have made modern ceramic material stronger and have decreased the risk of fracture; however, ceramic fracture complication has not yet resolved. Yoo et al. [35] evaluated 93 primary alumina-on-alumina THAs after a minimum duration of 5 years follow-up. One patient (one hip) had experienced alumina femoral head fracture because of a major motor-vehicle accident. In addition, Kawano et al. [36] recently reported a set of sandwich ceramic fracture in 50 hips (50/270 hips), and the 13-year survival rate was only 68.0%. In our study, sandwich ceramic liners (3.5%, 2/57 hips) fracture occurred in two patients 7 and 9 years after surgery, respectively. The main cause of implant failure was the design defects of the sandwich ceramic implant, notably the impingement between the femoral stem and acetabular. As a result, we no longer used “sandwich” ceramic articulation in patients who are at risk of ceramic fracture. As for alumina-on-alumina ceramic prosthesis, no ceramic fracture occurred in any hips. In addition to the improvement of prosthetic design and ceramic materials, we also considered appropriately reducing the acetabular abduction angle to avoid edge loading to reduce the ceramic fracture rate. Some authors also speculated the existence of other possible reasons for ceramic fracture, such as implant misalignment [37], rim impingement [38], and stripe wear [39]. Sugano et al. [38] observed impingement in 7 (6%) of 111 cases and suggested that impingement might provide the potential for ceramic fractures. Poggie et al. [39] found that striped wear damage of the head occurred because of edge loading and rim wear, thereby ultimately leading to ceramic liner fracture.
Squeaking was defined as a specific frequency, which was high pitched and audible noise perceived by the patient [40]. Squeaking was interpreted as a minor complication and was largely ignored in CoC bearing THAs. However, many authors have reported that squeaking occurs with an incidence ranging from 0.3% to 20.9% [41], [42], [43], and it gained much public attention. Stanat et al. [43] found that squeaking sounds occurred in 2.4% in a meta-analysis on all clinical outcome studies on the third and fourth CoC bearing surfaces implanted. Tozun et al. [44] reported in a review of 540 patients with ceramic bearings that incidence of squeaking was 2.8% at a mean follow-up of 8.2 years. The incidence of squeaking in this study was 1%. Although all hips were in the safe zone, squeaking noise was detected in one hip. Recently, a definitive etiology for squeaking in CoC bearing hips has been elusive and controversial. Stanat et al. [43] and Walter et al. [45] demonstrated that squeaking hips were more common in taller, heavier, younger, and more active patients. Other potential causes of squeaking have also been highlighted, including surgical and implant design [42], [46], component malposition [45], femoral neck-acetabular rim impingement [47], edge loading, and stripe wear [48], [49]. In our study, one hip, which was in the safe zone, showed intermittent squeaking under heavy load, but squeaking disappeared in the absence of heavy load. Therefore, we considered that edge loading may have caused squeaking in the hip under extreme conditions and resolved on the avoidance of these activities. Recently, some studies have suggested that squeaking may be an early sign of ceramic fracture [44], [50]. However, ceramic fracture was not detected in this hip, and further results might be confirmed for long-term follow-up.
This study has some limitations. First, it is a small cohort, single-center, retrospective study with a short follow-up period. Second, multiple implants were included in the study (different stems and acetabular cups), and this may influence the survivorship of implants independently of the bearing surface used. Third, we did not use a control group of elderly patients who had THA performed on them using the same devices.
Conclusions
Our results with the use of CoC bearings THAs in younger patients aged 50 years or younger have promising midterm results and provide a high rate of survivorship without evidence of osteolysis. Ceramic fracture could be associated with the design of the component.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.04.004.
Appendix A. Supplementary data
References
- 1.Older J. Charnley low-friction arthroplasty: a worldwide retrospective review at 15 to 20 years. J Arthroplasty. 2002;17:675. doi: 10.1054/arth.2002.31973. [DOI] [PubMed] [Google Scholar]
- 2.Bierbaum B.E., Nairus J., Kuesis D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002:158. doi: 10.1097/00003086-200212000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Torchia M.E., Klassen R.A., Bianco A.J. Total hip arthroplasty with cement in patients less than twenty years old—long-term results. J Bone Joint Surg Am. 1996;78A:995. doi: 10.2106/00004623-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Springer B.D., Connelly S.E., Odum S.M. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24:2. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Finkbone P.R., Severson E.P., Cabanela M.E. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty. 2012;27:213. doi: 10.1016/j.arth.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 6.Bozic K.J., Kurtz S., Lau E. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91A:1614. doi: 10.2106/JBJS.H.01220. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Rey E., Cruz-Pardos A., Garcia-Cimbrelo E. Alumina-on-alumina Total Hip Arthroplasty in Young Patients: Diagnosis is More Important than Age. Clin Orthop Relat Res. 2009;467:2281. doi: 10.1007/s11999-009-0904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nizard R., Pourreyron D., Raould A. Alumina-on-alumina hip arthroplasty in patients younger than 30 years old. Clin Orthop Relat Res. 2008;466:317. doi: 10.1007/s11999-007-0068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liudahl A.A., Liu S.S., Goetz D.D. Metal on metal total hip arthroplasty using modular acetabular shells. J Arthroplasty. 2013;28:867. doi: 10.1016/j.arth.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Seyler T.M., Bonutti P.M., Shen J. Use of an alumina-on-alumina bearing system in total hip arthroplasty for osteonecrosis of the hip. J Bone Joint Surg. 2006;88:116. doi: 10.2106/JBJS.F.00775. [DOI] [PubMed] [Google Scholar]
- 11.D'Antonio J.A., Sutton K. Ceramic materials as bearing surfaces for total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:63. [PubMed] [Google Scholar]
- 12.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg. 1969;51:737. [PubMed] [Google Scholar]
- 13.Zahiri C.A., Schmalzried T.P., Szuszczewicz E.S. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 14.Devane P.A., Horne J.G., Martin K. Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256. doi: 10.1016/s0883-5403(97)90021-8. [DOI] [PubMed] [Google Scholar]
- 15.Yoon H.J., Yoo J.J., Yoon K.S. Alumina-on-alumina THA performed in patients younger than 30 years: a 10-year minimum followup study. Clin Orthop Relat Res. 2012;470:3530. doi: 10.1007/s11999-012-2493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray D.W. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 17.Lewinnek G.E., Lewis J.L., Tarr R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217. [PubMed] [Google Scholar]
- 18.DeLee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976:20. [PubMed] [Google Scholar]
- 19.Gruen T.A., McNeice G.M., Amstutz H.C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979:17. [PubMed] [Google Scholar]
- 20.Sugano N., Takao M., Sakai T. Eleven-to 14-year follow-up results of cementless total hip arthroplasty using a third-generation alumina ceramic-on-ceramic bearing. J Arthroplasty. 2012;27:736. doi: 10.1016/j.arth.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 21.Engh C.A., Massin P., Suthers K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990:107. [PubMed] [Google Scholar]
- 22.Brooker A.F., Bowerman J.W., Robinson R.A. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629. [PubMed] [Google Scholar]
- 23.Boutin P. Total hip arthroplasty using a ceramic prosthesis. Pierre Boutin (1924-1989) Clin Orthop Relat Res. 2000;(379):3. [PubMed] [Google Scholar]
- 24.Boutin P. Total hip arthroplasty using a ceramic prosthesis - P Boutin. Clin Orthop Relat Res. 2000:4. (Reprinted from Rev Chir Orthop, vol. 58, pg 230-246, 1972) [PubMed] [Google Scholar]
- 25.O'Leary J.F., Mallory T.H., Kraus T.J. Mittelmeier ceramic total hip arthroplasty. A retrospective study. J Arthroplasty. 1988;3:87. doi: 10.1016/s0883-5403(88)80057-3. [DOI] [PubMed] [Google Scholar]
- 26.Capello W.N., D'Antonio J.A., Feinberg J.R. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty. 2008;23:39. doi: 10.1016/j.arth.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Topolovec M., Cor A., Milosev I. Metal-on-metal vs. metal-on-polyethylene total hip arthroplasty tribological evaluation of retrieved components and periprosthetic tissue. J Mech Behav Biomed Mater. 2014;34:243. doi: 10.1016/j.jmbbm.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Kim Y.H., Choi Y., Kim J.S. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head osteonecrosis. Int Orthop. 2010;34:1123. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jeffers J.R.T., Walter W.L. Ceramic-on-ceramic bearings in hip arthroplasty: state of the art and the future. J Bone Joint Surg Br. 2012;94B:735. doi: 10.1302/0301-620X.94B6.28801. [DOI] [PubMed] [Google Scholar]
- 30.Yoon T.R., Rowe S.M., Jung S.T. Osteolysis in association with a total hip arthroplasty with ceramic bearing surfaces. J Bone Joint Surg Am. 1998;80A:1459. doi: 10.2106/00004623-199810000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Cowie J.G., Turnbull G.S., Ker A.M. Return to work and sports after total hip replacement. Arch Orthop Trauma Surg. 2013;133:695. doi: 10.1007/s00402-013-1700-2. [DOI] [PubMed] [Google Scholar]
- 32.Ollivier M., Frey S., Parratte S. Does impact sport activity influence total hip arthroplasty durability? Clin Orthop Relat Res. 2012;470:3060. doi: 10.1007/s11999-012-2362-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sechriest V.F., Kyle R.F., Marek D.J. Activity level in young patients with primary total hip arthroplasty - a 5-year minimum follow-up. J Arthroplasty. 2007;22:39. doi: 10.1016/j.arth.2006.02.083. [DOI] [PubMed] [Google Scholar]
- 34.Lubbeke A., Garavaglia G., Barea C. Influence of patient activity on femoral osteolysis at five and ten years following hybrid total hip replacement. J Bone Joint Surg Br. 2011;93B:456. doi: 10.1302/0301-620X.93B4.25868. [DOI] [PubMed] [Google Scholar]
- 35.Choy W.S., Kim K.J., Lee S.K. Ceramic-on-ceramic total hip arthroplasty: minimum of six-year follow-up study. Clin Orthop Surg. 2013;5:174. doi: 10.4055/cios.2013.5.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kawano S., Sonohata M., Shimazaki T. Failure analysis of alumina on alumina total hip arthroplasty with a layered acetabular component: minimum ten-year follow-up study. J Arthroplasty. 2013;28:1822. doi: 10.1016/j.arth.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 37.Viste A., Chouteau J., Desmarchelier R. Fractures of a sandwich ceramic liner at ten year follow-up. Int Orthop. 2012;36:955. doi: 10.1007/s00264-011-1375-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sugano N., Nishii T., Miki H. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br. 2007;89B:455. doi: 10.1302/0301-620X.89B4.18458. [DOI] [PubMed] [Google Scholar]
- 39.Poggie R.A., Turgeon T.R., Coutts R.D. Failure analysis of a ceramic bearing acetabular component. J Bone Joint Surg Am. 2007;89A:367. doi: 10.2106/JBJS.F.00148. [DOI] [PubMed] [Google Scholar]
- 40.Restrepo C., Parvizi J., Kurtz S.M. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008;23:643. doi: 10.1016/j.arth.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Keurentjes J.C., Kuipers R.M., Wever D.J. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466:1438. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jarrett C.A., Ranawat A.S., Bruzzone M. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91A:1344. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 43.Stanat S.J.C., Capozzi J.D. Squeaking in third- and fourth-generation ceramic-on-ceramic total hip arthroplasty meta-analysis and systematic review. J Arthroplasty. 2012;27:445. doi: 10.1016/j.arth.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 44.Tozun I.R., Ozden V.E., Dikmen G. Mid-term result of ceramic bearings in total hip arthroplasty. Int Orthop. 2014;38:2027. doi: 10.1007/s00264-014-2387-x. [DOI] [PubMed] [Google Scholar]
- 45.Walter W.L., O'Toole G.C., Walter W.K. Squeaking in ceramic-on-ceramic hips - the importance of acetabular component orientation. J Arthroplasty. 2007;22:496. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 46.Walter W.L., Kurtz S.M., Esposito C. Retrieval analysis of squeaking alumina ceramic-on-ceramic bearings. J Bone Joint Surg Br. 2011;93B:1597. doi: 10.1302/0301-620X.93B12.27529. [DOI] [PubMed] [Google Scholar]
- 47.Yang C.C., Kim R.H., Dennis D.A. The squeaking hip: a cause for concern-disagrees. Orthopedics. 2007;30:739. doi: 10.3928/01477447-20070901-33. [DOI] [PubMed] [Google Scholar]
- 48.Taylor S., Manley M.T., Sutton K. The role of stripe wear in causing acoustic emissions from alumina ceramic-on-ceramic bearings. J Arthroplasty. 2007;22:47. doi: 10.1016/j.arth.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 49.Walter W.L., Insley G.M., Walter W.K. Edge loading in third generation alumina ceramic-on-ceramic bearings: stripe wear. J Arthroplasty. 2004;19:402. doi: 10.1016/j.arth.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 50.Abdel M.P., Heyse T.J., Elpers M.E. Ceramic liner fractures presenting as squeaking after primary total hip arthroplasty. J Bone Joint Surg Am. 2014;96:27. doi: 10.2106/JBJS.M.00737. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.