Abstract
Background
Psychiatric symptoms typically cut across traditional diagnostic categories. In order to devise individually tailored treatments, there is a need to identify the basic mechanisms that underlie these symptoms. Behavioral economics provides a framework for studying these mechanisms at the behavioral level. Here, we utilized this framework to examine a widely ignored aspect of trauma-related symptomatology—individual uncertainty attitudes—in combat veterans with and without posttraumatic stress disorder (PTSD).
Methods
Fifty-seven combat veterans, including 30 with PTSD and 27 without PTSD, completed a risk and ambiguity decision-making task that characterizes individual uncertainty attitudes, distinguishing between attitudes toward uncertain outcomes with known (“risk”) and unknown (“ambiguity”) probabilities, and between attitudes toward uncertain gains and uncertain losses. Participants’ choices were used to estimate risk and ambiguity attitudes in the gain and loss domains.
Results
Veterans with PTSD were more averse to ambiguity, but not risk, compared to veterans without PTSD, when making choices between possible losses, but not gains. The degree of aversion was associated with anxious arousal (e.g., hypervigilance) symptoms, as well as with the degree of combat exposure. Moreover, ambiguity attitudes fully mediated the association between combat exposure and anxious arousal symptoms.
Conclusions
These results provide a foundation for prospective studies of the causal association between ambiguity attitudes and trauma-related symptoms, as well as etiologic studies of the neural underpinnings of these behavioral outcomes. More generally, these results demonstrate the potential of neuroeconomic and behavioral economic techniques for devising objective and incentive-compatible diagnostic tools, and investigating the etiology of psychiatric disorders.
Keywords: PTSD, decision making, uncertainty, ambiguity, aversion, anxious arousal
INTRODUCTION
Growing consensus exists regarding the insufficiency of the Diagnostic and Statistical Manual of Mental Disorders (DSM[1]) categorical diagnoses for psychiatric disorders in guiding etiologic and treatment models[2,3]. On the one hand, many different combinations of symptoms may lead to the same diagnosis (e.g., see ref.[4]), suggesting that some of the categorical definitions may be arbitrary. On the other hand, high levels of comorbidity between various mental disorders suggest that psychopathology is dimensional and transdiagnostic in nature. The National Institute of Mental Health has recognized the need to investigate alternative classification models for mental disorders based on their underlying basic mechanisms, and to identify biomarkers of the various dimensions of psychopathology, which can inform the development of more targeted treatments (Research Domain Criteria, RDoC[5]).
Behavioral economics provides a useful framework for identifying behavioral markers using measures independent of the pathology itself[6–8]. By observing individuals’ actual choices rather than asking them what they would do in a given situation, behavioral economics methods can tap into the behavioral processes, eliminating biases that can result from subjective self-reports or interviews. Based on the choices participants make under parametrically varying conditions, various components of behavioral processes can be deduced. Associations between these components and clinical symptoms can then be examined to assess the relation of the particular behavior to a particular facet of psychopathology.
Here, we employed a behavioral economic framework to posttraumatic stress disorder (PTSD). We chose this disorder as a test case for the behavioral economic approach to psychiatric research for three reasons. First, it is the single psychiatric disorder that requires an event for its classification—exposure to trauma[1]. Second, PTSD is a heterogeneous disorder, encompassing a wide range of psychological symptoms that are present in other disorders, such as major depressive and generalized anxiety disorders. Third, despite the heterogeneity of symptoms, studies of PTSD and trauma-related psychopathology primarily focus on fear learning and emotional processing[9,10]. While these are certainly important components to examine in relation to such pathology, other cognitive processes are likely to play a part in the development, maintenance, and consequences of trauma-related psychopathology. One such key component that has rarely been studied is how trauma-exposed individuals deal with uncertainty, which is often pronounced in circumstances leading to traumatic events[11,12]. Soldiers in combat, for example, typically face widespread uncertainty about the possible adverse outcomes of battle. Individual variability in uncertainty attitudes may therefore contribute to individual differences in the expression of PTSD symptoms.
Neurobiological findings also suggest an association between decision making under uncertainty and trauma-related psychopathology. Current models of PTSD implicate a number of neurobiological systems and structures, including the amygdala, ventro-medial prefrontal cortex, and the striatum[13–16]. These same brain regions are also involved in decision-making processes in general,[17] and specifically under uncertainty,[18] and their activity reflects attitudes toward uncertainty[19]. However, although both these decision traits and PTSD symptoms are reflected in activation patterns in similar brain areas, a direct link between the two has never been made. This may be partly due to the difficulty in parsing out the various basic components of the complex processes of decision making under uncertainty.
Behavioral economics offers tools for examining the components of behavior under uncertainty. Economic analysis distinguishes between two types of uncertainty: “risk,” in which the probabilities of possible decision outcomes are known, and “ambiguity,” in which these probabilities are partially or completely unknown. Studies in healthy populations have revealed high variability in individual attitudes toward risk and ambiguity, with little correlation between these measures across individuals[19–21], suggesting that risk and ambiguity attitudes may contribute independently to decision making under uncertainty. Based on these data, we have previously developed an experimental paradigm[19,22] and have successfully used it in psychiatrically healthy individuals from a broad age spectrum[21,23]. In this paradigm, participants make a series of choices between gains and between losses, under conditions of risk or ambiguity. No feedback about choice outcome is provided during the task in order to avoid learning effects. The paradigm thus allows an objective characterization of risk and ambiguity attitudes in the gain and loss domains, as well as an overall assessment of the quality of the decision making. In the current study, we used this paradigm to characterize behavior under uncertainty in a sample of Iraq/Afghanistan combat veterans presenting with a broad dimensional range of trauma-related psychopathology, including approximately half diagnosed with combat-related PTSD. Our results reveal a specific association between trauma-related symptomatology and ambiguity, but not risk, attitudes in the loss, but not the gain, domain. We propose that a similar approach will be useful for the study of other psychiatric disorders and other decision traits.
MATERIALS AND METHODS
PARTICIPANTS
Sixty-three (52 male; 82.5%) combat veterans participated in the study. Thirty-two were diagnosed with PTSD based on the Clinician-Administered PTSD Scale (CAPS)[24] and 31 were Combat Controls (CC). For each group (PTSD, CC), the number of participants was balanced by age and sex. Six participants (two PTSD and four CC) were excluded from analysis due to poor task understanding (see below), leaving a final sample of 57 participants (eight female; aged 20–53, mean = 32.9, SD = 8.0). The Human Investigation Committee of Yale University and Human Subjects Subcommittee of the VA Connecticut Healthcare System approved the study; all participants provided written informed consent. See Supporting Information Material for recruitment procedures and additional measures.
PROCEDURE
Risk and Ambiguity Task
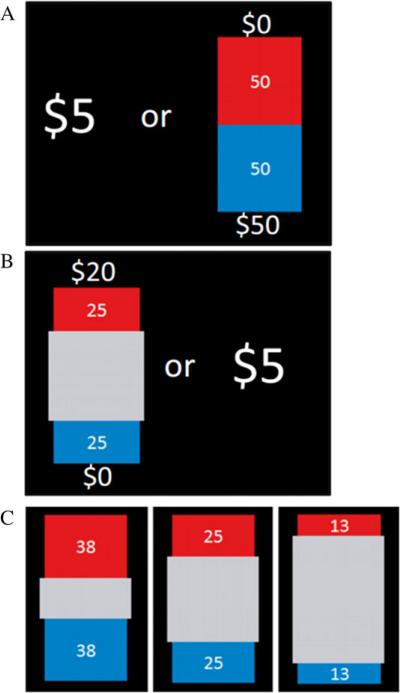
Following task instructions and practice, participants made a series of 320 binary choices between different monetary options. In gain trials, each choice was between a sure gain of $5 and a lottery that offered some chance for gaining a variable amount. Loss trials were identical, except the choice was between a sure loss of $5 and a lottery that offered some chance of losing a variable amount. Probability and ambiguity levels were communicated through visual displays of lottery bags, each containing 100 red and blue plastic chips. In risky trials (Fig. 1A), the red and blue areas of the bag represented the numbers of red and blue chips, such that participants knew the precise probability for drawing either from the bag. In ambiguous trials (Fig. 1B), a gray occluder covered a part of the bag, so the exact probability was unknown (See Supporting Information Methods for more details on experimental design and payment). To encourage participants to reveal their true preferences, one trial was randomly selected at the end of the experiment and participants were paid based on their choice in that trial (see Supporting Information Methods). In a separate session, participants completed a demographic form and psychological tests relevant to risk and ambiguity preferences (see Supporting Information Methods).
Figure 1.
Experimental design. Examples of risk (A) and ambiguity (B) trials. (C) The ambiguity levels used in the experiment.
Data Analysis
To estimate the risk and ambiguity attitudes of each participant in the gain and loss domain, we modeled the subjective value of each option, based on a theoretical model of decision making under uncertainty[25], successfully employed by our group[19,21,23]. The choice of data of each participant was fit to a logistic function,
where PL is the likelihood that the participant chose the lottery, SVC and SVL are the subjective values of the certain and lottery options, respectively, and γ is a subject-specific parameter representing noise in each participant's choices.
Subjective values were modeled using the following function,
where P represents the objective outcome probability, A is the ambiguity level, and V is the outcome magnitude.
Risk attitude (α) and ambiguity attitude (β) parameters, constrained for the task range, were estimated for each participant individually. A risk-neutral participant will have an α of 1. In the gain domain, a risk averse participant will have an α < 1 (α > 1 in the loss domain), while a risk-seeking participant will have an α > 1 (α < 1 in the loss domain). A participant who is not affected by ambiguity will have a β of zero. In the gain domain, an ambiguity averse participant will have a β > 0 (β < 0 in the loss domain), while an ambiguity-seeking participant will have a β < 0 (β > 0 in the loss domain). For convenience, in the presentation of the results (Fig. 3), we transfer all the parameters such that negative values indicate aversion, whereas positive values indicate seeking. Our main statistical analysis used these model-based parameters, and consisted of 2-way analyses of variance (ANOVAs), one for risk attitudes and another for ambiguity attitudes, with group (PTSD and CC) and domain (gains and losses) as factors. To ensure that the results do not depend on the functional form of this model, we also conducted complementary model-free analysis based on proportion of lottery choices (see Supporting Information Methods). To assess the level of correlation between pairs of parameters, we computed Pearson correlations. Given that correlation analysis is highly sensitive to outliers, we first excluded data points that differed by more than two standard deviations from the mean of the relevant parameter in the relevant sample. Finally, to evaluate the relationship between ambiguity attitudes, symptom clusters, and combat exposure, we conducted multiple regression analysis using Mplus Version 7.11, as well as Bayesian analyses (see Supporting Information Methods).
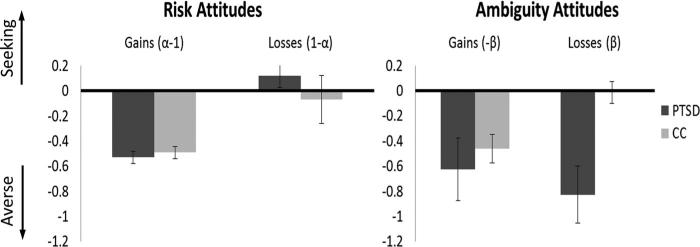
Figure 3.
Estimates of risk and ambiguity attitudes in the gain and loss domains. Mean parameter estimates based on the model fitting. Error bars denote SEM. There was a significant group by domain interaction in ambiguity attitudes (F = 4.54, P = .04), driven by higher aversion to ambiguous losses in PTSD compared to CC (Tukey's HSD test, P = .02). The groups did not differ in attitudes toward ambiguous gains or in risk attitudes.
RESULTS
SAMPLE CHARACTERISTICS
Fifty-seven participants were included in the analysis, 30 PTSD and 27 CC. The groups did not differ with respect to age, gender, level of education, income, IQ, or numeracy (Supporting Information Table S1), yet differed significantly on numerous clinical measures, with PTSD scoring higher than CC on the CAPS (61.1 vs. 4.1, t = 12.89, P < .0001), Combat Exposure Scale (CES[26]; 18.3 vs. 8.9, t = 3.52, P < .001), and each of the five PTSD symptom clusters[27,28], most notably anxious arousal symptoms (14.1 vs. 1.6, t = 11.05, P < .0001; Table S2 (Supporting Information) provides additional details of how the PTSD and CC groups differed on clinical measures).
PTSD SYMPTOMS AND DECISION MAKING UNDER UNCERTAINTY
Decision Quality
As a basic estimate of task competence, we calculated two measures of decision quality: choice consistency and choice effectiveness (see Supporting Information Methods and Results). No significant group difference was observed in either measure (choice consistency: t = 0.56, P = .58; effectiveness: t = 1.61, P = .12).
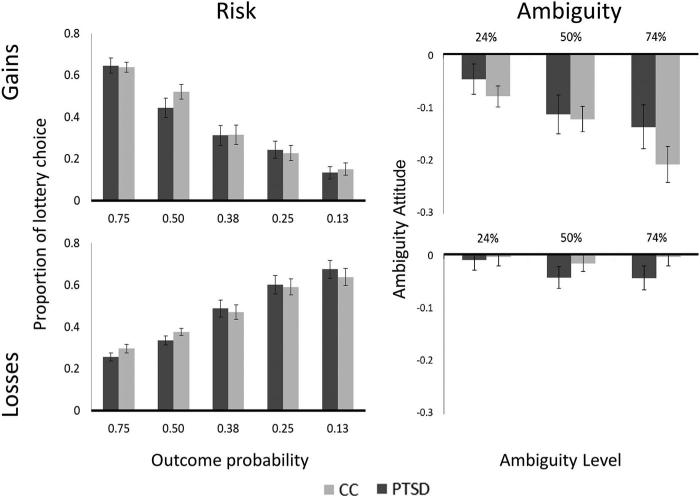
Risk and Ambiguity Attitudes
Figure 2 presents the average choice patterns in each group in risky (left) and ambiguous (right) trials involving gains (top) and losses (bottom). The risk graphs depict the proportion of trials in which participants chose the risky option rather than the certain amount. Both groups were similarly affected by outcome probability, exhibiting comparable risk attitudes for both gains (Fig. 2, top left) and losses (Fig. 2, bottom left). The ambiguity graphs plot the effect of each level of ambiguity on participants’ willingness to accept the lottery. Ambiguity averse participants would choose ambiguous lotteries less than risky lotteries of the same objective probability, whereas ambiguity seeking participants would choose such lotteries more (see Supporting Information Materials for details). Both groups exhibited similar degree of ambiguity aversion when making choices between gains (Fig. 2, top right). Choice patterns diverged, however, in the ambiguous loss condition. While CC showed no ambiguity aversion, similar to what we observed in an earlier study[21], PTSD participants exhibited ambiguity aversion by choosing the 50% and 74% ambiguity options less than the risky options of the same objective outcome probability.
Figure 2.
Lottery choices under risk and ambiguity. Left: proportion of trials in which participants chose the uncertain option rather than the certain amount in risky trials involving gains (top) and losses (bottom). Right: the effect of each level of ambiguity on participants’ willingness to accept the lottery in gains (top) and losses (bottom). The level of ambiguity is defined as the percentage of the bag image that was occluded. Error bars denote SEM.
To quantify the group difference, we fit each individual's behavior to a choice model that we have previously used[19,21], based on a widely used economic model[25] (see the section Materials and Methods). This process produced four participant-based uncertainty estimates, namely risk and ambiguity attitudes in the gain and loss domains (Fig. 3). These estimates were used in two 2-way ANOVAs, one for risk attitudes and another for ambiguity attitudes, each with group (PTSD and CC) and domain (gains and losses) as factors. The ANOVA on risk attitudes revealed, as expected, a significant effect of domain (F = 26.7, P = .00006), but no effect of group (P = .30), and no group by domain interaction (P = .30). Conversely, the ANOVA on ambiguity attitudes revealed main effects of both domain (P ≤ .00006) and group (P = .03), as well as a group by domain interaction (P = .04). Post hoc Tukey tests revealed that this interaction was driven by a group difference in ambiguity attitudes under losses (PTSD: −0.827 ± 0.22 SEM; CC: −0.0136 ± 0.08; P = .02, Cohen's d = 0.87), whereas no such difference was observed under gains (PTSD: −0.62 ± 0.25; CC: −0.46 ± 0.11; P = .92, Cohen's d = 0.15). For completion, we also conducted Bayesian analysis[29,30], which reached the same conclusions, as well as model-free analysis, i.e., with no assumptions regarding the functional form of the choice model, which revealed similar trends (see Supporting Information Results). Thus, the results did not strongly depend on either the model or the ANOVA assumptions. Importantly, the ambiguity attitudes observed in the CC group were similar to our previous results in participants of similar ages from the general population[21]. Also consistent with previous results[20,21,31], ambiguity attitudes in the loss domain were only weakly correlated with ambiguity attitudes in the gain domain, both across the entire sample (r = .26, N = 51, P = .07) and within each group (CC: r = .066, N = 25, P = .75; PTSD: r = .20, N = 25, P = .33). Similarly, attitudes toward ambiguous losses were only weakly correlated with attitudes toward ambiguous gains across the entire sample (r = −.24, N = 51, P = .09) and in the PTSD group r = −.20, N = 27, P = .3). Interestingly, this correlation was slightly higher in the CC group (r = −.43, N = 24, P = .03); however, the difference in correlation strength between groups was not significant (Fisher Z = −.85, P = .39).
Next, we sought to evaluate the relationship between ambiguity attitude, and the degree of specific symptom clusters, as well as the degree of combat exposure, across the entire sample. A regression model that accounted for intercorrelations among the five PTSD symptom clusters revealed that ambiguity attitude in the loss domain was significantly negatively associated with combat exposure (r = −.34, P = .011), as well as severity of anxious arousal symptoms (r = −.32, P = .013). Thus, participants who had greater exposure to combat, or reported more severe anxious arousal symptoms, were more averse to ambiguity when making choices between losses. Ambiguity aversion under losses was unrelated to severity of re-experiencing (r = −.21, P = .14), avoidance (r = −.20, P = .11), numbing (r = −.04, P = .79), or dysphoric arousal (r = −.11, P = .45) symptoms. Incorporation of numeracy scores (see Supporting Information Methods) into the model did not change the results. A Bayesian analysis also corroborated the results (see Supporting Information Results).
Results of a path analysis (Fig. 4) evaluating the role of ambiguity attitude under losses in mediating the relation between combat exposure severity and anxious arousal symptoms revealed that, while combat exposure was positively associated with anxious arousal in a bivariate analysis (r = .31, P = .012), this association was fully mediated by ambiguity attitudes under losses. Thus, more severe combat exposure was associated with stronger aversion to ambiguous losses (more negative ambiguity attitude scores), which was in turn associated with more severe anxious arousal symptoms.
Figure 4.
Standardized coefficients for our model based on path analyses results. The degree of combat exposure was positively associated with anxious arousal severity in a bivariate analysis (standardized coefficient = .31, P = .012), and this association was fully mediated by ambiguity attitudes under losses. Note that more negative ambiguity attitudes denote stronger aversion to ambiguity. Thus, combat exposure severity is associated with stronger aversion to ambiguous losses, which in turn is associated with more severe anxious arousal symptoms.
The observed association between attitudes toward ambiguous losses and PTSD symptomatology suggests that decision making under ambiguity may serve as a diagnostic tool for PTSD. In a final exploratory analysis, we therefore reversed our assumptions and instead of dividing our sample by PTSD status, we divided our participants into quartiles based on their attitudes for ambiguous losses. We found that participants most averse to ambiguous losses had significantly higher CAPS scores (54.4, SD = 28.3) than those most seeking ambiguous losses (29.5, SD = 33.2; t = 2.08, P = .021). This result held for three symptom clusters, with the ambiguity averse group showing significantly greater avoidance (P = .023), anxious arousal (P = .037), and dysphoric arousal (P = .004). In addition, while 85.7% of the subjects in the highest aversion group fit criteria for PTSD diagnosis, only 41.9% of participants in the other groups fit similar criteria (two-tailed Fisher's exact test, P = .0054), demonstrating possible diagnostic potential for such derived uncertainty attitude measurements.
DISCUSSION
This study used behavioral economics tools to examine decision making under risk and ambiguity in combat veterans with and without PTSD. We found that combat veterans diagnosed with PTSD were significantly more averse to ambiguity compared to CC, but only when making choices associated with potentially negative outcomes (losses). A dimensional analysis revealed that attitudes toward ambiguous losses were negatively associated with anxious arousal symptoms, as well as with the degree of combat exposure, and that ambiguity attitudes fully mediated the positive correlation between combat exposure and anxious arousal symptoms. Finally, participants most averse to ambiguous losses were more likely to be diagnosed with PTSD, suggesting a potential independent diagnostic utility of this behavioral measure.
Although the potential link between uncertainty and PTSD has hardly been explored, there is some evidence that increased uncertainty about the outcome of distressing events may increase the psychological effect of those events[12,32,33]. A recent study has also shown that individual intolerance of uncertainty, measured in a self-report questionnaire, may be associated with several PTSD symptoms[12,32,33]. Our results are consistent with these initial studies, but are highly novel in three important ways. First, our task relies on insights from experimental economics, where choice behavior is used to directly infer participants’ uncertainty attitudes in a context that is independent from the trauma. Moreover, participants were paid based on their choices in the experiment, and thus were encouraged to make choices that were based on their true preference. Second, the task allows us to decompose uncertainty attitudes into attitudes toward qualitatively different forms of uncertainty, ambiguity and risk, and to distinguish between these attitudes in two separate domains—gains and losses. Uncertainty attitudes in these different domains tend to be independent in healthy populations[19,20,31], and were independent in our sample of individuals with PTSD, and therefore may be differentially associated with the risk of developing specific psychiatric symptoms. Finally, our dimensional analysis revealed a specific association with anxious arousal symptoms. Anxious arousal, which is characterized by hyperreactivity to specific trauma cues—hypervigilance and exaggerated startle responses—is a key component in trauma-related psychopathology[32] and may contribute to the chronicity of PTSD symptoms[34–36]. Attitudes toward ambiguous losses may therefore serve as a new marker of this diagnostic construct and inform risk models of the development of chronic symptoms. Prospective studies are needed to evaluate this possibility.
The specificity of our finding to the domain of ambiguous losses is important for several reasons. First, the results suggest that veterans with strong symptoms of anxious arousal are not intolerant of any type of uncertainty, but rather avoid ambiguous options whose outcome probabilities are not precisely known and would result in negative outcome. Ambiguity is abundant in the battlefield, as soldiers frequently face situations that they have never experienced before, and this ambiguity is foremost about negative consequences, including the ultimate loss of one's life. It is possible that those individuals who are more averse to ambiguity are more severely impacted by the realization of the same ambiguous possibility. This in turn may make the same individuals less able to inhibit stress responses resulting in chronic anxious arousal. It is also possible that experiencing an adverse outcome following conditions of high ambiguity leads the individual to develop aversion to ambiguity around potential negative outcomes. Interestingly, while ambiguity attitudes were independent from risk attitudes in our PTSD sample, as well as in a general population sample[21], a significant, albeit weak, correlation was observed in the CC group. The current study was not powered to further explore that difference, but an interesting question for future research is whether psychological resilience to combat and other traumas is associated with greater coupling between risk and ambiguity tolerance. Second, the fact that the observed association is unique to expected losses, and does not extend to the gain domain, implies that it is not a general cognitive variation, and may not involve the reward circuitry. While several neuroimaging studies have implicated reward brain structures in encoding subjective values of losses[37,38], behavioral studies increasingly show little or no correlation between choice behavior under gains and losses across individuals[20,21,31], suggesting partially overlapping and partially distinct processing of rewards and punishments. An intriguing possibility is that this specificity is what makes individuals vulnerable to developing anxious arousal symptoms, while variation in the gain domain may predispose individuals to other symptom clusters, such as substance abuse or pathological gambling symptoms, not assessed in this study.
Our study is not without limitations. First, it is important to stress that our results do not allow us to infer causation—ambiguity aversion may predispose the individual to stress-related symptomatology, but may also be a consequence of more severe combat exposure or PTSD symptoms. Prospective studies, for example comparing behavior before and after deployment, are needed to examine causal relations among these variables. Second, our sample consisted entirely of combat veterans, a population who willingly chose to take part in dangerous and highly uncertain situations. While this was an important feature of our design, aimed at equating as much as possible the experience of participants with and without PTSD, whether PTSD in civilians, who experienced trauma without choosing to put themselves in risk, is also associated with aversion to ambiguous losses remains to be seen. Third, our study design employed a single experimental paradigm and relied on a specific, although widely used, choice model. Although the results were reached by several different analyses, including ANOVA, linear regression, and Bayesian analyses, and also supported by model-free analysis, future studies are needed to evaluate whether the results of the current study generalize to more ecologically valid situations.
Notwithstanding these limitations, choice tasks like the one used here may be adopted to expand and improve screening for psychopathology in a variety of contexts. Standardized behavioral tasks are affordable and easy to administer. Rather than rely on subjective evaluations, either by a clinician or by the patients themselves, these tasks provide objective evaluation tools by incentivizing patients to express their true preferences. Results of this study also provide an initial proof-of-concept for the potential utility of computational behavioral methods in psychiatric research[6,39]. The combination of behavioral tasks and model-based analysis provides insights into latent behavioral variables that are not directly observed. This approach can help in elucidating existing symptomatology, or inform the development of new mediating markers, as well as the personalization of treatment.
Supplementary Material
Acknowledgments
We thank Rebecca Garland for her help with data collection and Daniela Schiller for very helpful discussions and comments. This study was supported by the National Institute of Mental Health grant R21MH102634 (to I. L. and I. H.-R.) and by the Clinical Neurosciences Division of the U.S. Department of Veterans Affairs National Center for PTSD. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The work was performed at Yale University, New Haven, CT.
Footnotes
Conflict of Interest. The authors declare no conflict of interest or financial disclosures related to this work.
REFERENCES
- 1.Association AP . Diagnostic and Statistical Manual of Mental Disorders. DSM-5. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- 2.Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry. 2014;13(1):28–35. doi: 10.1002/wps.20087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11(1):126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspect Psychol Sci. 2013;8(6):651–662. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- 5.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 6.Sharp C, Monterosso J, Montague PR. Neuroeconomics: a bridge for translational research. Biol Psychiatry. 2012;72(2):87–92. doi: 10.1016/j.biopsych.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartley CA, Phelps EA. Anxiety and decision-making. Biol Psychiatry. 72(2):113–118. doi: 10.1016/j.biopsych.2011.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monterosso J, Piray P, Luo S. Neuroeconomics and the study of addiction. Biol Psychiatry. 72(2):107–112. doi: 10.1016/j.biopsych.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Milad MR, Pitman RK, Ellis CB, et al. Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder. Biol Psychiatry. 2009;66(12):1075–1082. doi: 10.1016/j.biopsych.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin LM, Wright CI, Cannistraro PA, et al. A functional magnetic resonance imaging study of amygdala and medial prefrontal cortex responses to overtly presented fearful faces in posttraumatic stress disorder. Arch Gen Psychiatry. 2005;62(3):273–281. doi: 10.1001/archpsyc.62.3.273. [DOI] [PubMed] [Google Scholar]
- 11.Brothers D. Toward a Psychology of Uncertainty: Trauma-Centered Psychoanalysis. Taylor & Francis; New York: 2011. [Google Scholar]
- 12.Fetzner M, Horswill S, Boelen P, Carleton RN. Intolerance of uncertainty and PTSD symptoms: exploring the construct relationship in a community sample with a heterogeneous trauma history. Cognit Ther Res. 2013;37(4):725–734. [Google Scholar]
- 13.Elman I, Lowen S, Frederick BB, et al. Functional neuroimaging of reward circuitry responsivity to monetary gains and losses in posttraumatic stress disorder. Biol Psychiatry. 2009;66(12):1083–1090. doi: 10.1016/j.biopsych.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sailer U, Robinson S, Fischmeister FP, et al. Altered reward processing in the nucleus accumbens and mesial prefrontal cortex of patients with posttraumatic stress disorder. Neuropsychologia. 2008;46(11):2836–2844. doi: 10.1016/j.neuropsychologia.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 15.Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research–past, present, and future. Biol Psychiatry. 2006;60(4):376–382. doi: 10.1016/j.biopsych.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Admon R, Lubin G, Stern O, et al. Human vulnerability to stress depends on amygdala’s predisposition and hippocampal plasticity. Proc Natl Acad Sci USA. 2009;106(33):14120–14125. doi: 10.1073/pnas.0903183106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kable JW, Glimcher PW. The neurobiology of decision: consensus and controversy. Neuron. 2009;63(6):733–745. doi: 10.1016/j.neuron.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu M, Bhatt M, Adolphs R, et al. Neural systems responding to degrees of uncertainty in human decision-making. Science. 2005;310(5754):1680–1683. doi: 10.1126/science.1115327. [DOI] [PubMed] [Google Scholar]
- 19.Levy I, Snell J, Nelson AJ, et al. Neural representation of subjective value under risk and ambiguity. J Neurophysiol. 2010;103(2):1036–1047. doi: 10.1152/jn.00853.2009. [DOI] [PubMed] [Google Scholar]
- 20.Cohen M, Jaffray JY, Said T. Experimental comparison of individual behavior under risk and under uncertainty for gains and for losses. Organ Behav Hum Decis Process. 1987;39(1):1–22. [Google Scholar]
- 21.Tymula A, Rosenberg Belmaker LA, Ruderman L, et al. Like cognitive function, decision making across the life span shows profound age-related changes. Proc Natl Acad Sci USA. 2013;110(42):17143–17148. doi: 10.1073/pnas.1309909110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levy I, Rosenberg Belmaker L, Manson K, et al. Measuring the subjective value of risky and ambiguous options using experimental economics and functional MRI methods. J Vis Exp. 2012;(67):e3724. doi: 10.3791/3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tymula A, Rosenberg Belmaker LA, Roy AK, et al. Adolescents’ risk-taking behavior is driven by tolerance to ambiguity. Proc Natl Acad Sci USA. 2012;109(42):17135–17140. doi: 10.1073/pnas.1207144109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 25.Gilboa I, Schmeidler D. Maxmin Expected Utility with Non-Unique Prior. J Math Econ. 1989;18(2):141–153. [Google Scholar]
- 26.Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychol Assess. 1989;1:53–55. [Google Scholar]
- 27.Harpaz-Rotem I, Tsai J, Pietrzak RH, Hoff R. The dimensional structure of posttraumatic stress symptomatology in 323,903 US veterans. J Psychiatr Res. 2014;49:31–36. doi: 10.1016/j.jpsychires.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Pietrzak RH, Tsai J, Harpaz-Rotem I, et al. Support for a novel five-factor model of posttraumatic stress symptoms in three independent samples of Iraq/Afghanistan veterans: a confirmatory factor analytic study. J Psychiatr Res. 2012;46(3):317–322. doi: 10.1016/j.jpsychires.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Jeffreys SH. Theory of probability. Oxford Univ. Press; New York: 1961. [Google Scholar]
- 30.Rouder JN, Speckman PL, Sun D, et al. Bayesian t tests for accepting and rejecting the null hypothesis. Psychon Bull Rev. 2009;16(2):225–237. doi: 10.3758/PBR.16.2.225. [DOI] [PubMed] [Google Scholar]
- 31.Abdellaoui M, Bleichrodt H, Paraschiv C. Loss aversion under prospect theory: a parameter-free measurement. Manage Sci. 2007;53(10):1659–1674. [Google Scholar]
- 32.Goto T, Wilson JP, Kahana B, Slane S. The Miyake island volcano disaster in Japan: loss, uncertainty, and relocation as predictors of PTSD and depression. J Appl Soc Psychol. 2006;36(8):2001–2026. [Google Scholar]
- 33.Lee YL, Gau BS, Hsu WM, Chang HH. A model linking uncertainty, post-traumatic stress, and health behaviors in childhood cancer survivors. Oncol Nurs Forum. 2009;36(1):E20–E30. doi: 10.1188/09.ONF.E20-E30. [DOI] [PubMed] [Google Scholar]
- 34.Marshall GN, Schell TL, Glynn SM, Shetty V. The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. J Abnorm Psychol. 2006;115(3):624–628. doi: 10.1037/0021-843X.115.3.624. [DOI] [PubMed] [Google Scholar]
- 35.Schell TL, Marshall GN, Jaycox LH. All symptoms are not created equal: the prominent role of hyperarousal in the natural course of posttraumatic psychological distress. J Abnorm Psychol. 2004;113(2):189–197. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- 36.Pietrzak R, Feder A, Schechter C, et al. Dimensional structure and course of post-traumatic stress symptomatology in World Trade Center responders. Psychol Med. 2014;44(10):2085–2098. doi: 10.1017/S0033291713002924. [DOI] [PubMed] [Google Scholar]
- 37.Tom SM, Fox CR, Trepel C, Poldrack RA. The neural basis of loss aversion in decision-making under risk. Science. 2007;315(5811):515–518. doi: 10.1126/science.1134239. [DOI] [PubMed] [Google Scholar]
- 38.Bartra O, McGuire JT, Kable JW. The valuation system: a coordinate-based meta-analysis of BOLD fMRI experiments examining neural correlates of subjective value. Neuroimage. 2013;76:412–427. doi: 10.1016/j.neuroimage.2013.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Montague PR, Dolan RJ, Friston KJ, Dayan P. Computational psychiatry. Trends Cogn Sci. 2012;16(1):72–80. doi: 10.1016/j.tics.2011.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.