Abstract
Background:
Diagnostic and treatment hierarchical reductionisms have resulted in an oversight of anxiety syndromes in schizophrenia.
Aim:
The aim of this study was to find the prevalence of different anxiety disorders in schizophrenia patients.
Materials and Methods:
The study was conducted on inpatients of a tertiary care psychiatric hospital using a prospective, purposive sampling technique. The study consisted of 93 schizophrenia patients and a similar number of normal controls. The schizophrenia patients and controls were evaluated for psychopathology and the presence of anxiety disorder.
Results:
The prevalence of anxiety disorder was significantly higher in schizophrenia patients (45.16%) compared to controls (16.12%). Further, the prevalence of panic disorder, social anxiety disorder, and obsessive-compulsive disorder (OCD) was significantly higher in schizophrenia patients. No significant correlation was observed between anxiety disorder scores and psychopathology scores.
Conclusions:
The prevalence of comorbid anxiety disorders (panic disorder, social anxiety disorder, and OCD) in schizophrenia is significantly higher in the general population. The onset of anxiety disorder commonly precedes the onset of schizophrenia.
Keywords: Comorbid anxiety disorders, obsessive-compulsive disorder, panic disorder, schizophrenia, social anxiety disorder
In psychiatry, comorbidity more often applies to the co-occurrence of two or more different mental disorders, which are defined in terms of their characteristic symptoms rather than their underlying causes. This co-occurrence has been reported to be very frequent.[1] People with dual diagnoses are more likely to experience a range of negative outcomes including increased levels of medication noncompliance, poorer treatment outcome, psychosocial problems, suicidal behavior, re-hospitalization, homelessness, poorer mental health, and higher family burden.[2,3] Anxiety at the onset of psychosis is central to the neuropsychological account of the condition, and arousal is implicated in the formation of delusional beliefs.[4] If anxiety is an important precursor of psychotic symptoms, one would expect that the various anxiety disorders would be common in schizophrenia. Earlier in the last century, Bleuler described nonpsychotic abnormalities including somatic complaints, obsessions and compulsions, anxiety, panic, and depressive symptoms present before the onset of schizophrenia.[5] Fish also recognized the occurrence of anxiety in schizophrenia.[6] Thus, whether as a symptom or a syndrome, anxiety is common and its identification in people with schizophrenia is not surprising. Anxiety could also be a part of the premorbid personality of the person with schizophrenia and this in turn could be the result of the same neurodevelopmental process that may lie behind the emergence of schizophrenia.[7]
Thus, although a high association is thought of between schizophrenia and various anxiety disorders, the actual prevalence of such an association is not much in clinical settings. The reasons could be the fact that clinicians often dismiss evidence of such conditions and the dismissal may seem to be simple common sense, but these ideas rest on hierarchical notions. If such cases are seen, the symptoms of the comorbid condition are attributed to schizophrenia alone as if no other disturbances were present. Psychotic symptoms may also interfere with the assessment of associated anxiety disorders in schizophrenia because they are dramatic phenomena and thus are judged to be a more urgent clinical priority. Patients may also psychotically interpret physiological symptoms and may communicate these experiences in a distorted way, thereby making them harder to recognize. In addition, cognitive impairment and negative symptoms may also make it difficult to assess the patients for these conditions. Neuroleptic effects may also obscure anxiety syndromes. Akathisia may mimic anxiety interfering with the recognition of panic attacks in schizophrenia. Finally, some of the newer antipsychotics have been implicated in the provocation of obsessive-compulsive symptoms,[8] panic symptoms,[9] and social anxiety symptoms.[10]
All these effects create potential clinical confounds that may add to the clinical difficulty in assessing associated anxiety disorders in schizophrenia. In more recent years, studies examining comorbid anxiety in schizophrenia have found increasing prevalence of such conditions.[11,12,13,14,15,16,17,18,19,20,21,22,23] Despite this, little work has been done to establish the clinical validity and practical utility of this phenomenon. In view of the paucity of Indian work in this field, the present study was undertaken to find the prevalence of different anxiety disorders in schizophrenia patients.
MATERIALS AND METHODS
This was a cross-sectional, hospital-based study with purposive sampling technique conducted at Ranchi Institute of Neuropsychiatry and Allied Sciences (RINPAS), which is a 500-bedded postgraduate teaching psychiatric hospital and tertiary referral center for the patients with psychiatric disorders. The study sample comprised 93 consecutively admitted inpatients fulfilling ICD-10 DCR criteria for schizophrenia.[24] In addition, the study group also fulfilled the condition of being drug naïve or off drugs for 1 month for oral drugs and 3 months for depot preparations. A similar number of age- and sex-matched participants without any present, past, or family history of psychiatric illness and suitably matched with the sociodemographic variables to the study sample constituted the control group. The study was approved by the Ethics Committee of the institute. The inclusion and exclusion criteria for the study and control groups are given below.
Inclusion and exclusion criteria for the study group
Inclusion criteria for the study group
Inpatients of RINPAS meeting ICD-10 DCR criteria for schizophrenia
Patients in the age range of 18–55 years
Patients who are drug naïve or off drugs for 1 month or off-depot preparation for at least 3 months
Cooperative for the interview.
Exclusion criteria for the study group
Patients not willing to give informed consent
History of mental retardation
History of substance abuse/neurological disorder/head injury/major physical illness.
Inclusion and exclusion criteria for the control group
Inclusion criteria for the control group
Falling in the age group of 18–55 years
Belonging to the same region as that of the patient (Bihar, Jharkhand)
Belonging to the same socioeconomic strata as that of the patient group
Cooperative for the interview
Not suffering from any psychiatric or medical disorder at present or in the past.
Exclusion criteria for the control group
Patients not willing to give informed consent
History of any mental disorders, substance abuse, or neurological disorder in their families.
After explaining the purpose of the study and obtaining informed consent from the schizophrenia patients and the control group, their sociodemographic characteristics were recorded in a specially prepared pro forma. All the patients were then assessed using Mini International Neuropsychiatry Interview[25] for the assessment of psychopathology. In addition to this, the relation of the anxiety disorder to the onset of schizophrenia was also recorded. The two groups were then compared for the prevalence of anxiety disorders.
The obtained results were then tabulated for evaluation using the aid of computer program SPSS 17. The tests used were Student's t-test for continuous data and Chi-square test (with Yates correction) for frequency data.
RESULTS
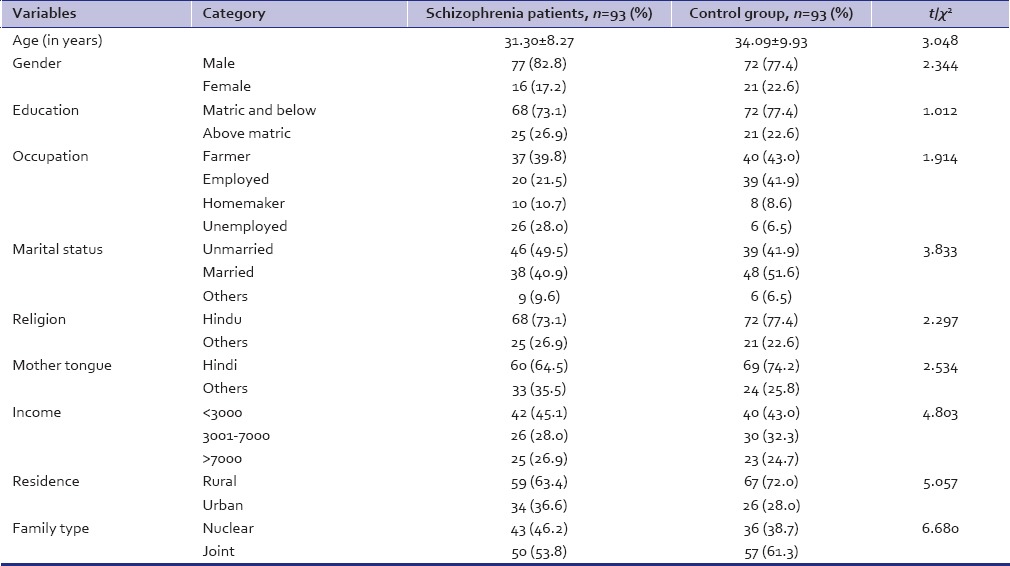
There was no significant difference between the two groups on the sociodemographic variables (age, gender, education, occupation, marital status, religion, mother tongue, income, residence, and family type) [Table 1]. The study group constituting schizophrenia patients had a mean age of onset at 26.22 years (standard deviation [SD] 7.97) and a mean duration of illness of 4.76 years (SD 5.23), majority belonged to the paranoid subtype (65.0%), with an insidious mode of onset (90.3%), no precipitating factor (84.9%), no past history (91.4%), no family history (73.1%), and though drug free had received some treatment earlier (64.5%).
Table 1.
Demographic characteristics of schizophrenia patients and controls
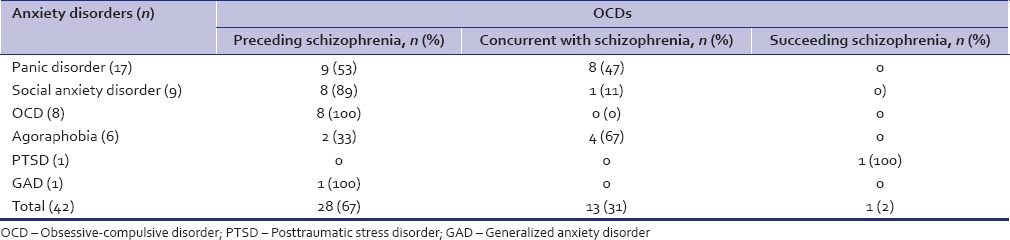
The prevalence of anxiety disorder was 45.16% (n = 42) in the schizophrenia patients and 16.12% (n = 15) in the controls. This difference was highly statistically significant [Table 2]. Further analysis revealed that the prevalence of social anxiety disorder, obsessive-compulsive disorder (OCD), and panic disorder in the schizophrenia group was significantly higher (P ≤ 0.05, P ≤ 0.05, and P ≤ 0.01, respectively) than the control group [Table 2]. The relation of onset of comorbid anxiety disorder with respect to the onset of schizophrenia is shown in Table 3.
Table 2.
Distribution of anxiety disorders in schizophrenia patients and controls
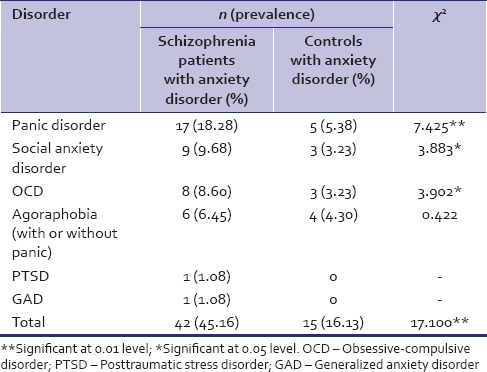
Table 3.
Onset of anxiety disorders with respect to the onset of schizophrenia
DISCUSSION
The present study revealed the prevalence of 45.16% for anxiety disorders in schizophrenia population which was significantly higher than the prevalence of 16.2% in the control group. This finding is in agreement with some studies which reported rates for the anxiety disorders in schizophrenia between 43%–45%.[14,15] Comparatively higher prevalence of anxiety disorders in schizophrenia population of 50.8%–74% has also been reported,[13,18,20,21,22] while still other studies have reported lower prevalence rates of 20%–31.5%.[11,17] This wide range for the prevalence of various anxiety disorders in schizophrenics may be explained by the differences in the sample, place of study as well as the methodology. For example, studies that included schizophrenic outpatients,[18,19] being cross sectional, frequently reported a relatively higher prevalence of anxiety disorders as compared to the studies which had taken inpatients for their study.[14,16] Furthermore failure to apply strict diagnostic criteria for anxiety disorders may have led to overestimation of anxiety symptoms as anxiety syndromes, i.e., without fulfilling the diagnostic criteria for anxiety disorder.[13] A further possibility in the Indian context is that the Indian population is not well versed with the symptoms of mental illness, especially the anxiety spectrum disorders, misinterpreting them as physical symptoms and ignoring them.[26] Other factors that may affect the study of anxiety disorders in schizophrenia are that anxiety may be intermittent and may occur in response to symptoms of psychosis or as a side effect of antipsychotic drugs.[21]
Even after applying strict diagnostic procedures, people with schizophrenia are themselves less focused on their anxiety disorders and thus less likely to report them, feeling their main problem lies elsewhere. Moreover, the data were obtained by direct interview of the patients and not from someone else like the primary caregivers leading to misidentification of the symptoms by the schizophrenic patients themselves who suffer impairments in self-observation and might also be abulic.[27]
Prevalence of specific anxiety disorders
Panic disorder
The prevalence of panic disorder in schizophrenia patients in the present study was 18.28%, which is in close agreement with the other studies.[21,23] Prevalence rates <10%[17,18] as well as more than 20%[13,14,15,19,20,22,28] have also been reported. This discrepancy in the prevalence rates for panic disorder most likely would have occurred because the patients evaluated had different clinical profiles and different methodologies implemented. The most widely reported symptoms among the patients suffering from panic disorder in the present study were palpitations, chest pain, dizziness, and the fear of dying. This was in concordance with other studies.[17]
Social anxiety disorder
In the present study, a significantly higher prevalence of 9.68% for social anxiety disorder was found in schizophrenia patients which was in agreement with earlier studies,[17,22] though few others have reported higher values.[14,18,19,20] Most of the study samples suffering from social anxiety disorder had marked and persistent fear in the social situations as compared to the performance situations which is quite different from the other studies[20] and could be due to the lack of exposure of the Indian population, especially belonging to a rural background to certain social situations leading to frequent reporting of social anxiety in social situations.
Obsessive-compulsive disorder
The prevalence of 8.60% of OCD in the current study was significantly higher than the control group, and it is in close agreement with a few studies[17,19,22] though some studies have reported higher values.[15,20,21] This variability in the prevalence rates might be because of the use of different diagnostic criteria and diagnostic instruments.[29] In addition, in this context, the data in the present study were obtained mainly by the direct interview of the patients and not of the caregivers, which might be the cause of underreporting of OCD as the patients are less focused on such symptoms and therefore less likely to report them, feeling their main problem lies somewhere else. It is also likely that in some studies the frequency of OCD is overrepresented because of inclusion of patients with OC symptoms which are not fulfilling the diagnostic criteria for OCD. The most common obsessions were contamination and sexual images and the compulsions being cleaning and praying which are similar to those reported earlier.[30]
Posttraumatic stress disorder
The prevalence rate of 1.08% for posttraumatic stress disorder (PTSD) in the present study was similar to 1.3% reported by a researchers[19] but less as compared to 17% and 47% reported by others.[21,31,32]
Agoraphobia
The prevalence of 6.45% for agoraphobia in the study sample was not significantly different from the control group [Table 2]. Rates falling in this range have been reported by various investigators,[19,22] but a prevalence rate higher than the current study has also been reported.[18]
Generalized anxiety disorder
The prevalence of 1.08% for generalized anxiety disorder (GAD) in the current study was strikingly low as compared to the other studies which have reported much higher prevalence rates.[18,19,22] Lower prevalence of GAD in Indian context might be because of lack of awareness of such symptoms and misinterpreting them as physical symptoms or panic symptoms and an inappropriate translation of the word 'worry' included in the criteria for GAD.[26,27]
Relation of onset of anxiety disorders to onset of schizophrenia
There was an earlier onset of panic disorder in 9 of the 17 schizophrenic patients suffering from comorbid panic disorder [Table 3], which is in agreement with previous studies.[28] An equal proportion of panic disorder preceding, concurrent, and succeeding the onset of schizophrenia has also been reported.[33] In addition, the development of schizophrenia in three patients with a history of panic disorder during the course of a severe panic attack has also been reported.[34] Moreover, panic attacks after the administration of clozapine in patients being treated for schizophrenia have also been reported.[9] The onset of panic disorder preceded the onset of schizophrenia by a mean duration of 2.23 ± 2.0 years in this study. This is somewhat less as compared to the other studies, with a mean duration of 4.34 ± 3 years prior to the onset of schizophrenia.[16,28]
The onset of OCD was prior to the onset of schizophrenia in all patients in this study, which is in agreement with most of the related studies.[34,35] Whereas in some other studies, there have been mixed reports of onset of OCD. Byerly et al. had reported onset of OCD prior to schizophrenia in only 28% of their sample and the onset of OCD during or after the onset of schizophrenia in rest of them.[36] This variation might be due to the recall bias in the onset of OCD disorders. The mean duration by which the onset of OCD preceded the onset of schizophrenia was 3.01 ± 2.43 years, which was concurrent with other studies.[35]
The onset of social anxiety disorder was prior to the onset of the schizophrenic illness in majority of the cases. This is similar to other studies which have reported an onset of the social anxiety disorder prior to the onset of schizophrenic illness, as a part of the prodrome of the illness.[37] A few have found the onset of social anxiety disorder during or after the treatment of the social anxiety and as a response to the antipsychotic treatment.[38] In majority of the agoraphobia patients, the onset of illness was concurrent with the onset of schizophrenia similar to earlier studies.[39]
The onset of PTSD in the present study was almost 1 year after the onset of a full-blown schizophrenic illness, and as per the patient, this was due to the experience of electroconvulsive therapy that the patient received during the treatment of schizophrenia. Similar phenomenon has also been reported earlier,[40] implying that treatment of psychosis could be traumatic and can lead to PTSD. Many earlier studies have reported the onset of PTSD symptoms in the prepsychotic phase of the illness occurring as a result of childhood trauma or in response to the psychotic symptoms, but this was not observed in the present study.[11,41]
The only schizophrenia patient suffering from GAD had an onset of GAD prior to the onset of schizophrenia which is in agreement with other studies as well who have considered GAD as part of the prodrome of schizophrenia.[42]
Limitations
Limitations of the study include possible selection bias being a tertiary care hospital-based study where patients with more severe illness are more likely to be included. No distinction was made between the clinical correlates of patients with acute schizophrenia and chronic schizophrenia. The sample consisted mostly of men (81%), thus findings of the study may not be generalized to females. Another limitation was that the data in this study were obtained by direct interview of the patients and not from the primary care givers. Further, the patients in the subgroups of anxiety disorders were small [Table 3].
CONCLUSIONS
The prevalence of comorbid anxiety disorders in schizophrenia is significantly higher than the general population. The onset of anxiety disorder commonly precedes the onset of schizophrenia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Loga S, Loga-Zec S. Comorbidity in psychiatry: Its impact on psychopharmacological treatment. Psychiatr Danub. 2009;21:347–9. [PubMed] [Google Scholar]
- 2.Chaudhury S, Tikka SK, Bakhla AK. Impact of substance use disorder on presentation of schizophrenia. Dual Diagn. 2016;1:7. [Google Scholar]
- 3.Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophr Bull. 2000;26:105–18. doi: 10.1093/oxfordjournals.schbul.a033429. [DOI] [PubMed] [Google Scholar]
- 4.Gray JA, Feldon J, Rawlings JN, Hemsley DR, Smith AD. The neuropsychology of schizophrenia. Behav Brain Sci. 1991;14:1–20. [Google Scholar]
- 5.Bleuler E. In: Dementia praecox or the group of schizophrenias. Zinkin J, translator. New York: International Univesities Press; 1950. [Google Scholar]
- 6.Hamilton M. Fish's Schizophrenia. 2nd ed. Bristol, Wright: 1984. [Google Scholar]
- 7.Davies N, Russell A, Jones P, Murray RM. Which characteristics of schizophrenia predate psychosis? J Psychiatr Res. 1998;32:121–31. doi: 10.1016/s0022-3956(97)00027-7. [DOI] [PubMed] [Google Scholar]
- 8.Zink M. Comorbid obsessive-compulsive symptoms in schizophrenia: Insight into pathomechanisms facilitates treatment. Adv Med 2014. 2014;18 doi: 10.1155/2014/317980. doi: 10.1155/2014/317980.317980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bressan RA, Monteiro VB, Dias CC. Panic disorder associated with clozapine. Am J Psychiatry. 2000;157:2056. doi: 10.1176/appi.ajp.157.12.2056. [DOI] [PubMed] [Google Scholar]
- 10.Scheltema Beduin AA, Swets M, Machielsen M, Korver N Genetic Risk and Outcome of Psychosis Investigators. Obsessive-compulsive symptoms in patients with schizophrenia: A naturalistic cross-sectional study comparing treatment with clozapine, olanzapine, risperidone, and no antipsychotics in 543 patients. J Clin Psychiatry. 2012;73:1395–402. doi: 10.4088/JCP.11m07164. [DOI] [PubMed] [Google Scholar]
- 11.Strakowski SM, Tohen M, Stoll AL, Faedda GL, Mayer PV, Kolbrener ML, et al. Comorbidity in psychosis at first hospitalization. Am J Psychiatry. 1993;150:752–7. doi: 10.1176/ajp.150.5.752. [DOI] [PubMed] [Google Scholar]
- 12.Braga RJ, Reynolds GP, Siris SG. Anxiety comorbidity in schizophrenia. Psychiatry Res. 2013;210:1–7. doi: 10.1016/j.psychres.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 13.Cassano GB, Pini S, Saettoni M, Rucci P, Dell'Osso L. Occurrence and clinical correlates of psychiatric comorbidity in patients with psychotic disorders. J Clin Psychiatry. 1998;59:60–8. doi: 10.4088/jcp.v59n0204. [DOI] [PubMed] [Google Scholar]
- 14.Cosoff SJ, Hafner RJ. The prevalence of comorbid anxiety in schizophrenia, schizoaffective disorder and bipolar disorder. Aust N Z J Psychiatry. 1998;32:67–72. doi: 10.3109/00048679809062708. [DOI] [PubMed] [Google Scholar]
- 15.Bermanzohn PC, Porto LR, Arlow P, Pollack S, Stronger R, Siris SG. Hierarchical diagnosis in chronic schizophrenia: A clinical study of co-occurring syndromes. Schizophr Bull. 2000;26:517–25. doi: 10.1093/oxfordjournals.schbul.a033472. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin R, Lyons JS, McNally RJ. Panic attacks in schizophrenia. Schizophr Res. 2002;58:213–20. doi: 10.1016/s0920-9964(01)00373-5. [DOI] [PubMed] [Google Scholar]
- 17.Goodwin RD, Amador XF, Malaspina D, Yale SA, Goetz RR, Gorman JM. Anxiety and substance use comorbidity among inpatients with schizophrenia. Schizophr Res. 2003;61:89–95. doi: 10.1016/s0920-9964(02)00292-x. [DOI] [PubMed] [Google Scholar]
- 18.Tibbo P, Swainson J, Chue P, LeMelledo JM. Prevalence and relationship to delusions and hallucinations of anxiety disorders in schizophrenia. Depress Anxiety. 2003;17:65–72. doi: 10.1002/da.10083. [DOI] [PubMed] [Google Scholar]
- 19.Pallanti S, Quercioli L, Hollander E. Social anxiety in outpatients with schizophrenia: A relevant cause of disability. Am J Psychiatry. 2004;161:53–8. doi: 10.1176/appi.ajp.161.1.53. [DOI] [PubMed] [Google Scholar]
- 20.Ciapparelli A, Paggini M, Marazziti D, Carmassi C, Bianchi M, Taponecco C, et al. Comorbidity with axis I anxiety disorders in remitted psychotic patients 1 year after hospitalization. CNS Spect. 2007;12:913–9. doi: 10.1017/s1092852900015704. [DOI] [PubMed] [Google Scholar]
- 21.Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35:383–402. doi: 10.1093/schbul/sbn135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McMillan KA, Enns MW, Cox BJ, Sareen J. Comorbidity of Axis I and II mental disorders with schizophrenia and psychotic disorders: Findings from the national epidemiologic survey on alcohol and related conditions. Can J Psychiatry. 2009;54:477–86. doi: 10.1177/070674370905400709. [DOI] [PubMed] [Google Scholar]
- 23.Ulas H, Alptekin K, Akdede BB, Tumuklu M, Akvardar Y, Kitis A, et al. Panic symptoms in schizophrenia: Comorbidity and clinical correlates. Psychiatry Clin Neurosci. 2007;61:678–80. doi: 10.1111/j.1440-1819.2007.01724.x. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders (Tenth Revision): Diagnostic Criteria for Research. Geneva: World Health Organization; 1992. [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 26.Chaudhury S, Saini R, Bakhla AK, Singh J. Depression and anxiety following coronary artery bypass graft: Current Indian scenario. Cardiol Res Pract 2016. 2016:2345184. doi: 10.1155/2016/2345184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trivedi JK, Gupta PK. An overview of Indian research in anxiety disorders. Indian J Psychiatry. 2010;52(Suppl 1):S210–8. doi: 10.4103/0019-5545.69234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baylé FJ, Krebs MO, Epelbaum C, Levy D, Hardy P. Clinical features of panic attacks in schizophrenia. Eur Psychiatry. 2001;16:349–53. doi: 10.1016/s0924-9338(01)00590-9. [DOI] [PubMed] [Google Scholar]
- 29.Achim AM, Maziade M, Raymond E, Olivier D, Mérette C, Roy MA. How prevalent are anxiety disorders in schizophrenia. A meta-analysis and critical review on a significant association? Schizophr Bull. 2011;37:811–21. doi: 10.1093/schbul/sbp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hemrom S, Pushpa, Prasad D, Jahan M, Singh AR, Kenswar DK. Prevalence of obsessive compulsive symptoms among patients with schizophrenia. Ind Psychiatry J. 2009;18:77–80. doi: 10.4103/0972-6748.62263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Calhoun PS, Stechuchak KM, Strauss J, Bosworth HB, Marx CE, Butterfield MI. Interpersonal trauma, war zone exposure, and posttraumatic stress disorder among veterans with schizophrenia. Schizophr Res. 2007;91:210–6. doi: 10.1016/j.schres.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 32.Fan X, Henderson DC, Nguyen DD, Cather C, Freudenreich O, Evins AE, et al. Posttraumatic stress disorder, cognitive function and quality of life in patients with schizophrenia. Psychiatry Res. 2008;159:140–6. doi: 10.1016/j.psychres.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 33.Labbate LA, Young PC, Arana GW. Panic disorder in schizophrenia. Can J Psychiatry. 1999;44:488–90. doi: 10.1177/070674379904400510. [DOI] [PubMed] [Google Scholar]
- 34.Devulapalli KK, Welge JA, Nasrallah HA. Temporal sequence of clinical manifestation in schizophrenia with co-morbid OCD: Review and meta-analysis. Psychiatry Res. 2008;161:105–8. doi: 10.1016/j.psychres.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 35.Shioiri T, Shinada K, Kuwabara H, Someya T. Early prodromal symptoms and diagnoses before first psychotic episode in 219 inpatients with schizophrenia. Psychiatry Clin Neurosci. 2007;61:348–54. doi: 10.1111/j.1440-1819.2007.01685.x. [DOI] [PubMed] [Google Scholar]
- 36.Byerly M, Goodman W, Acholonu W, Bugno R, Rush AJ. Obsessive compulsive symptoms in schizophrenia: Frequency and clinical features. Schizophr Res. 2005;76:309–16. doi: 10.1016/j.schres.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Iyer SN, Boekestyn L, Cassidy CM, King S, Joober R, Malla AK. Signs and symptoms in the pre-psychotic phase: Description and implications for diagnostic trajectories. Psychol Med. 2008;38:1147–56. doi: 10.1017/S0033291708003152. [DOI] [PubMed] [Google Scholar]
- 38.Pallanti S, Quercioli L, Pazzagli A. Social anxiety and premorbid personality disorders in paranoid schizophrenic patients treated with clozapine. CNS Spectr. 2000;5:29–43. doi: 10.1017/s1092852900021635. [DOI] [PubMed] [Google Scholar]
- 39.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 40.Lommen MJ, Restifo K. Trauma and posttraumatic stress disorder (PTSD) in patients with schizophrenia or schizoaffective disorder. Community Ment Health J. 2009;45:485–96. doi: 10.1007/s10597-009-9248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: A systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–79. doi: 10.1093/schbul/sbm121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iyer SN, Boekestyn L, Cassidy CM, King S, Joober R, Malla AK. Signs and symptoms in the pre-psychotic phase: description and implications for diagnostic trajectories. Psychological Medicine. 2008;38:1147–56. doi: 10.1017/S0033291708003152. [DOI] [PubMed] [Google Scholar]


