Abstract
Background
To study different imaging criteria for prediction of lymph node metastases (Stage III disease) in colon cancer using CT.
Methods
In a retrospective setting, 483 consecutive patients with histology proven colon cancer underwent elective primary resection during 2008–2011, a cohort of 119 patients were included. Contrast enhanced CT examinations, in portal-venous phase, were reviewed with assessment of the number of lymph nodes, their anatomical distribution, size, size ratio, internal heterogeneity, presence of irregular outer border and attenuation values. Sensitivity, specificity, PPV and NPV for each studied criteria for prediction of stage III disease was calculated.
Results
According to histopathology 80 patients were stage I-II and 39 were stage III. Of the studied CT-criteria for lymph node metastases per patient, internal heterogeneity in at least one lymph node resulted in the best performance with sensitivity, specificity, PPV and NPV of 79, 84, 70 and 89%, Odds ratio (OR) 20. Presence of irregular outer border resulted in a sensitivity, specificity, PPV and NPV of 59, 81, 61 and 82%, OR 6.2. If both internal heterogeneity and/or irregular outer border was used as a criterion this resulted in a sensitivity, specificity, PPV and NPV of 85, 75, 62 and 91%, OR 16.5. None of the size criteria used were predictive for stage III disease.
Conclusions
When performing preoperative CT in patients with colon cancer, the imaging criteria that allow best prediction of stage III disease on CT are either presence of at least one lymph node with internal heterogeneity or internal heterogeneity and/or irregular outer border. These criteria have to be validated in a prospective study.
Keywords: Colon cancer, Computed tomography, Staging, Stage III, Lymph nodes
Background
Colon cancer is the third most common malignancy in the western world. In Sweden the incidence is increasing with an aging population while the mortality is slowly decreasing [1].
The treatment is surgical removal of the tumour containing segment of the bowel together with local and regional lymph nodes. In addition, adjuvant chemotherapy is standard treatment for patients with stage III disease and in some patients with stage II disease, depending on presence of additional histological risk factors.
Well-known important prognostic factors in colon cancer are tumour stage (T), extramural vascular invasion (EMVI) and lymph node involvement (N) [2]. Even the total number of harvested lymph nodes at surgery and lymph node ratio (the ratio between lymph node metastases and examined lymph nodes, LNR) assessed by the pathologist has a prognostic importance [3–5].
A complete preoperative evaluation of patients with colon cancer includes staging of the primary tumour and evaluation of distant metastases in the liver and lungs with computed tomography (CT). In recent years, some studies advocate and support the use of CT also for local staging of colon cancer including treatment planning and selection of patients for neoadjuvant treatment [6–8]. If selection of patients for neoadjuvant treatment is being used routinely in the clinic, pretreatment knowledge of regional lymph node involvement will be even more important.
To date, there are no validated imaging criteria for the assessment of lymph node metastases in colon cancer. Previous studies have applied different criteria based on either size and/or morphology. Lymph node size >1 cm, short-long axis diameter ratio, internal heterogeneity (IH), irregular outer border (IOB), attenuation values >100 Hounsfield units (HU) and cluster of three or more normal sized lymph nodes, or any combination of the above, have all been used as a single criterion or combined criteria [6, 9–14]. In a systematic review by Leufkens et al. including 753 patients with colon cancer in altogether 11 studies a sample sized weighted sensitivity and specificity of CT for N-staging of 76 and 55% was reported [15]. Most of the studies included were performed with older CT-technology that is no longer used and that does not allow true multiplanar assessment. Furthermore, the studies did not consider the distribution and location of lymph nodes within the colonic mesentery adjacent to the cancer as a potential marker of lymph node involvement.
Today, when CT scanners are configured with multiple rows of detectors, multiplanar assessment can be performed allowing for more detailed assessment of size and morphology of pathological lesions [16].
The aim of this study was to assess whether the number of lymph nodes, their anatomical distribution, size, size ratio, internal heterogeneity, irregular outer border and attenuation values on preoperative CT, either alone or in combination, were predictive for stage III disease.
Methods
From the Swedish colorectal cancer registry (SCRCR), 483 consecutive patients having a histology proven colon cancer and operated between the years 2008 and 2011 and examined with abdominal CT (64 detector CT-scanner) before surgery at our institution were included. A cohort of 119 patients was determined, after the following patients were excluded: insufficient CT examination (no iv contrast, CT-Colonography, no 64-slice) including examination performed outside the University hospital (n = 80), patients having emergency colonic surgery (n = 78), patients with T4 tumours (n = 68), metastatic disease (n = 67), no detectable tumour on the preoperative CT (n = 18), co-malignant disease (n = 15), CT examination >60 days prior to surgery (n = 13), patients with neo-adjuvant chemotherapy (n = 11), previous colon cancer surgery (n = 9), CT after treatment with colon stenting (n = 3) and perforated tumour or abscess (n = 2).
In the remaining cohort with histologically proven colon cancer there were 63 women and 56 men with a median age of 69 (range 32–91 years).
Most of the tumours were located in the sigmoid colon (Table 1). The majority of the tumors were classified on histopathology as T3 tumours (Table 1). Thirty-nine out of 119 patients had lymph node positive (stage III) disease (28 patients N1 and 11 patients N2) (Table 1). The median age for patients with stage I-II disease was 70 years, and the median age for patients with stage III disease was 63 years.
Table 1.
Demographics table of 119 patients/tumours
| Characteristics | Number (%) |
|---|---|
| Sex (female/male) | 63/56 |
| Age (median) | 69 (32–91) |
| Histopathological evaluation | |
| Tumour localization | |
| Caecum | 23 (19%) |
| Ascending colon | 22 (18%) |
| Hepatic flexure | 8 (7%) |
| Transverse colon | 11 (9%) |
| Splenic flexure | 4 (3%) |
| Descending colon | 6 (5%) |
| Sigmoid colon | 45 (38%) |
| Tumor Stage | |
| T1 | 10 (8%) |
| T2 | 16 (13%) |
| T3 | 93 (78%) |
| Positive lymph node status | |
| T1 tumours | 2/10 (20%) |
| T2 tumours | 2/16 (12%) |
| T3 tumours | 35/93 (38%) |
| Stage | |
| Stage I | 22 (18%) |
| Stage II | 58 (49%) |
| Stage III | 39 (33%) |
| Lymph nodes, total number | |
| Harvested lymph nodes PAD | 2542 |
| Positive lymph nodes PAD | 123 |
| CT evaluation | |
| Detected lymph nodes ≥4 mm/tot | 442/1312 (34%) |
| Region 1 | 261/835 (31%) |
| Region 2 | 161/389 (41%) |
| Region 3 | 20/88 (23%) |
All patients had preoperative investigations with CT of the abdomen with intravenous contrast (0.5 mg Iodine/kg) in portal-venous phase (delay 90 s) on one of four different 64 slice CT scanners (Lightspeed VCT, General Electric, Milwaukee, USA). All examinations were performed at 120 kV and with tube current modulation. For abdomen the median dose length product (DLP) was 583 mGy-cm (range 393 to 878 mGy-cm). Median pitch factor was 1.375 (range 0.516 to 1.50). Medium noise index was 30 (range 26 to 42). The variation in both pitch factor and noise index are due to differences in the four CT scanners that were used. In 56 CT examinations arterial phase imaging of the abdomen at the tumour location and liver was also performed. After the examination, reformatted images in axial, coronal and sagittal planes with 5 mm thickness (increment 2.5 mm) were routinely generated together with the original (thin slices) 0.625 mm images.
CT evaluation
All CT examinations were retrospectively reviewed by one radiologist (E.R.) with more than 15 years of experience in cross sectional imaging of colorectal cancer and blinded for the histology and surgical reports. Examinations were assessed according to a dedicated evaluation proforma.
All measurements and assessments were performed on a Sectra Workstation IDS7 (version 15.1.14.41) using the 5 mm reformatted images with 2.5 mm increment. The original thin slices (0.625 mm) were used for detection of small lymph nodes (≤4 mm).
Anatomical distribution
The colonic mesentery, 5 cm oral and aboral from the tumour site, was divided in three anatomical regions (region 1–3), as a modified variant of the guidelines of the Japanese Society for Cancer in the Colon and Rectum [17]. Region 1 was defined as the region most adjacent to the tumour (+/−5 cm) and 3 cm proximal along the vessels to the branch artery divides covering the pericolonic and marginal lymph nodes. Region 3 was defined as the most proximal part of the mesentery including the undivided mesenteric artery from the aorta (proximal lymph nodes). Region 2 was defined as the region between region 1 and 3 (Fig. 1).
Fig. 1.
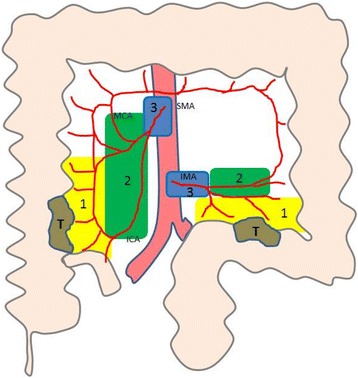
Assessment of right and left sided tumours (T) and their corresponding anatomical distribution of lymph nodes. Region 1 (yellow) is +/− 5 cm oral and aboral near the tumour site and approximately 3 cm along the feeding arterial branch to the nearest arterial vessel division. Region 3 (blue) is the undivided artery from the aorta (superior mesenteric artery (SMA) or inferior mesenteric artery (IMA)) to the first artery division. Region 2 (green) is between regions 1 and 3
Number, size and size-ratio of lymph nodes
All lymph nodes ≥2 mm in size were separately registered in total and in each anatomical region. For lymph nodes ≥4 mm in shortest diameter, the short axis and the long axis were also separately measured and the ratio between the short and long axis diameter was calculated. The size ratio (ratio between two orthogonal (short/long) axis diameters) was used to test whether a more rounded shape was predictive for metastasis. A >0.8 ratio between diameter was used as cut off point according to a previous study [18]. The presence of a cluster (within a range of the lymph node diameter) of three or more lymph nodes was also separately noted in every region.
Internal heterogeneity and irregular outer borders
As possible morphological predictors of metastases, the internal heterogeneity (IH, mixed attenuation within the lymph node) as well as the irregular outer border (IOB, indistinct demarcation of the lymph node) were evaluated both on reformatted and thin sections (Figs. 2 and 3).
Fig. 2.

Coronal reformation (5 mm section post iv contrast portal phase) CT image illustrating the apperance of 10 × 15 mm lymph node (white arrow) in region 1 with internal heterogeneity thus well defined borders in a patient with pT3 tumour in the ascending colon. At histopathology, 4 metastatic lymph nodes out of 43 were harvested
Fig. 3.
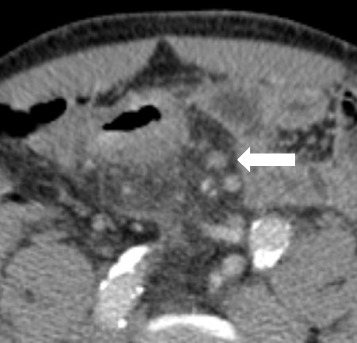
Transaxial reformation (5 mm section post iv contrast portal phase) CT image illustrating the apperance of a 7 × 7 mm mesocolic lymph node (white arrow) in region 2 with irregular outer border and internal heterogeneity in a patient with a pT3 tumour in the sigmoid colon with 1 metastatic lymph nodes out of 16 harvested at histopathology
Attenuation values
Attenuation measurements of each lymph node in the portal venous phase and, when available, in the arterial phase were also performed. All density measurements (using HU) were performed by placing as large a region of interest (ROI) as possible (>2 mm2) on the lymph node in the portal venous phase and in the arterial phase when available. Attenuation values of ≥50 and ≥100 HU in the portal venous phase were separately noted as well as ratio portal venous/arterial phase. Inhomogeneous contrast enhancement as indicative for tumour involvement was separated from either presence of a fatty lymph node hilum or a contrast filled vessel in the vicinity of a lymph node.
Surgery
All patients in the study were operated in an elective setting and according to colorectal surgery praxis. The resection of colon cancer was made by clear lateral margins, resection of the loco-regional lymph node bearing mesentery.
Histopathology
Histopathology was performed according to standard procedures at the university hospital pathology department by a specialized GI pathologist (initially using TNM version 6 and later TNM version 7) [19, 20]. From the pathologists’ original report the T- and N-stage, the total number of harvested and metastatic lymph nodes served as reference standard.
Statistics
Data were evaluated using statistical analysis software SPSS, IBM. Descriptive statistics were applied to the different lymph node characteristics calculating sensitivity, specificity, PPV, NPV and Odds ratio for the prediction of stage III disease. Mann–Whitney U test were used to test significance which was set to p ≤ 0.05. Univariate and multiple logistic regression analyses were performed for categorical data. Receiver operating characteristics (ROC) and area under the curve (AUC) were used to compare the optimal lymph node size criterion.
Results
Patients and histopathology
The median time interval between pre-operative CT examination and surgery was 28 days (range 4 – 59 days), mean 29 days (standard deviation 13 days).
A total of 2542 lymph nodes were harvested (median 19 lymph nodes/patient, range 4–69) and of those 123 were assessed as metastases (median, 2 lymph nodes/patient, range 1–10). The change from TNM 6 to TNM 7 did not affect the result.
CT evaluation
Number, anatomical distribution, size and size-ratio of lymph nodes
At CT, most of the lymph nodes were located in region 1. Region 2 had higher proportion of lymph nodes ≥4 mm (41%) compared to the other regions (Table 1). The mean number of lymph nodes found was 7.2 for pT1 tumours, 8.6 for pT2 tumours and 11.8 for pT3 tumours (not shown in Table).
Evaluation of lymph nodes
Using size thresholds of ≥4, 5, 6, 7, 8 and 10 mm as criteria for lymph node metastases, the results are presented as a ROC-curve in Fig. 4.
Fig. 4.
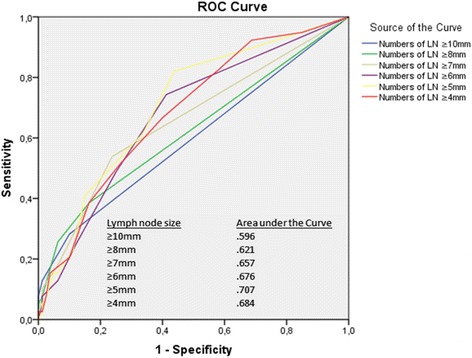
Size criteria (≥4, 5, 6, 7, 8, 10 mm) in shortest diameter according to CT presented as receiver operating characteristics, ROC, and Area under the curve, AUC
Size ratio with a cutoff point of 0.8 had an overall sensitivity and specificity of 85 and 30% (Table 2). If divided into the three anatomical regions, the sensitivity and specificity were as follows: region 1, 80 and 35%; region 2, 54 and 74% and region 3, 5 and 94%, respectively.
Table 2.
Sensitivity, specificity, PPV and NPV (%) for the different CT characteristics of lymph nodes > 4 mm in shortest diameter
| Variables | Number | Sensitivity | Specificity | PPV | NPV | OR | p-value |
|---|---|---|---|---|---|---|---|
| Size ≥5 mm | 287 | 90 | 31 | 39 | 86 | 1.33 | 0.002 |
| Size ≥10 mm | 29 | 28 | 90 | 58 | 72 | 2.67 | 0.009 |
| Ratio cut off 0.8 | 244 | 85 | 30 | 37 | 80 | 2.36 | 0.090 |
| Internal heterogeneity (IH) | 94 | 79 | 84 | 70 | 89 | 20.0 | <0.001 |
| Irregular outer border (IOB) | 73 | 59 | 81 | 61 | 82 | 6.23 | <0.001 |
| IH and/or IOB | 67 | 85 | 75 | 62 | 91 | 16.5 | <0.001 |
| HU ≥50 | 396 | 95 | 20 | 37 | 89 | 4.63 | 0.049 |
| HU ≥100 | 81 | 44 | 68 | 40 | 71 | 1.60 | 0.239 |
| Cluster of three | 14 | 13 | 89 | 36 | 68 | 1.16 | 0.803 |
Note: HU Hounsfield units, OR Odds ratio
Internal heterogeneity and irregular outer border
Forty-four out of 119 patients had at least one (range 1–6) lymph node with internal heterogeneity according to CT and a total number of 94 lymph nodes with this morphological feature were detected. Compared to histopathology, the sensitivity and specificity for predicting stage III disease with this criterion was 79 and 84%, respectively, p ≤ < .001, OR = 20 (Table 2). If divided by anatomical region, the sensitivity and specificity were as follows: region 1, 64 and 91%; region 2, 51 and 92% and region 3, 3 and 97%, respectively.
Thirty-eight patients had at least one (range 1–8) lymph node with an irregular outer border.
Compared to histopathology, lymph nodes with an irregular outer border showed sensitivity and specificity for prediction of stage III disease of 59 and 81%, respectively, p ≤ < .001, OR = 6.3 (Table 2). If divided by anatomical region, the sensitivity and specificity were as follows: region 1, 49 and 89%; region 2, 33 and 91%, and region 3, 0 and 99%, respectively.
In patients with at least one lymph node with internal heterogeneity and a lymph node with an irregular outer border, regardless of location, the sensitivity and specificity for stage III disease was 54 and 90%, respectively.
Patients with any lymph node showing internal heterogeneity and/or irregular outer borders, meaning that either one of the criteria were present or both in combination, showed an overall sensitivity and specificity for stage III disease of 85 and 75%,respectively, p ≤ < .001, OR = 16.5 (Table 2).
Contrast enhancement
The overall sensitivity and specificity prediction of stage III disease for lymph nodes having a HU value ≥50 or ≥100 post contrast in portal venous phase were, 95 and 20%, and 44 and 68%, respectively (Table 2).
Cluster of three or more normal shaped and sized lymph nodes
This criterion resulted in an overall sensitivity of 13% and a specificity of 89% (Table 2).
Combination of different variables using multivariate logistic regression analyses
The strongest predictor for stage III disease in our study was internal heterogeneity. No other variable contributed significantly when the variable internal heterogeneity was included in the multivariate regression model (Fig. 5).
Fig. 5.
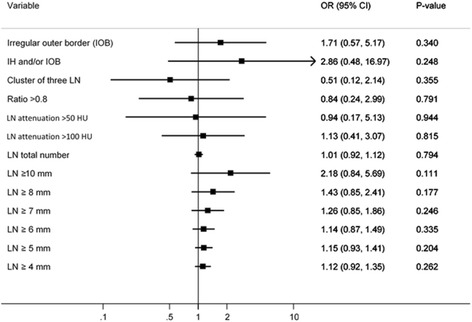
Multivariate logistic regression analyses for odds ratio of different lymph node characteristics when internal heterogeneity is included in the model
Discussion
To our knowledge, this report is the first to study previously reported criteria for lymph node metastases on CT separately or in comparison as a predictor for stage III disease in colon.
Of all the studied imaging criteria in this study, morphological criteria was superior to size criteria. Internal heterogeneity and irregular outer borders were the two variables that display best, both alone or combined, with reasonable sensitivity and specificity. The combination of internal heterogeneity and/or irregular outer borders still resulted in a moderate sensitivity of 85% and specificity of 75%. The strongest predictor in our study for stage III disease was internal heterogeneity both alone or combined with other variables (Fig. 5). Our results using CT are inferior, but for sensitivity comparable with previous work by Brown et al., which used morphological predictors for mesorectal lymph node status in magnetic resonance imaging (MRI) of rectal cancer where mixed signal intensity or irregular border resulted in a sensitivity of 85% and specificity of 97% [21].
The majority (64%) of lymph nodes that were detected, regardless of N-stage, were located in region 1, but presence of lymph nodes in this region were not predictive for nodal disease (stage III) (p = 0.182). In region 2 there was a slightly higher proportion of lymph nodes in favour of stage III (160 out of 471 lymph nodes (34%)) vs stage II (229 out of 841 lymph nodes (27%)) (p = 0.006). In the whole cohort, only 39 patients had lymph nodes in region 3, and there was no difference between the two groups regardless of T-stage. The high specificity in region 3 for the criteria internal homogeneity, irregular outer border and size ratio cut off <0.8 is due to a very limited number of lymph nodes fulfilling those criteria.
In a study, with 106 patients and up to date computed tomography technique using >1 cm and/or cluster of ≥3 lymph nodes as criteria for nodal disease resulted in a sensitivity of 71% and specificity of 41% [22]. In the present study, only 19 patients had lymph nodes ≥10 mm and only 14 patients had lymph nodes in a cluster of three, thus reducing the impact of these criteria for prediction of stage III.
Regarding lymph node size, lymph nodes >5 mm and/or irregular outer border were considered positive for nodal disease in the study by Dighe et al. with sensitivity and specificity of 64 and 53%, respectively [8]. In our study, this criterion showed a similar sensitivity of 56% but a higher specificity of 84%. We have no explanation for this difference.
Size criteria alone can really be questioned and not supported by our study. It has been reported that up to 70% of lymph nodes with metastases in colorectal cancer are ≤5 mm in diameter [23]. The majority of the detected lymph nodes (n = 870, 66%) in our study were <4 mm and thus could not be further assessed because of their small size and uncertainty in characterization using CT.
In the study of Kwak et al., a combination of criteria regarding assessment of lymph node metastases, including a cluster of more than three nodes along the loco-regional vascular pedicle, spiculated and indistinct node borders, and a mottled heterogeneous pattern were all integrated in the assessment and together with the size threshold of ≥10 mm reporting a sensitivity and specificity of 87 and 29%, respectively, with CT alone [24]. The specificity was surprisingly low maybe due to the large threshold size. The results with positron emission tomography/computed tomography (PET/CT), with a slightly different setting of defined criteria, did not markedly improve the overall results with a sensitivity and specificity of 66 and 60%, respectively.
Other studies using fluoro-2-deoxy-D-glucose-PET (FDG-PET) reported low sensitivities (29–37%) but higher specificity (87%) for nodal staging, suggesting that PET/CT is of limited additional value in detecting metastatic regional lymph nodes surrounding the primary tumour due to high false negative rate [25, 26]. Some authors argues that routine use of PET/CT can alter or change the management in stage III patients (6.5%) and stage IV patients (12.7%) while other authors claim that it does not [27, 28].
Regarding contrast enhancement/attenuation features, this does not seem to increase diagnostic accuracy. Arterial or portal venous phase attenuation post contrast was not predictive for stage III disease in this study. The differences in attenuation between arterial and portal-venous phase was not predictive for stage III disease.
Furthermore, regarding lymph node size ratio, Kanamoto et al. reported both high sensitivity and specificity of 87 and 80%, respectively, using the criteria of cutoff point of 0.8 or greater in short/long axis diameter ratio measured in the axial plane of the CT images [18]. In this current study the reformatted images were used to measure the true short and long axis and found similar sensitivity (85%) for this criterion but much lower specificity (30%) due to a high rate of false positive findings (70%). Benign lymph nodes can be either oval or rounded, which is a limitation using this criterion.
The use of CT assessed lymph node status alone as predictor of prognosis is still premature. If selection for neoadjuvant chemotherapy was made by the best combination of criteria (heterogeneity and/or irregular border) in this study, 6 patients out of 39 (15%) would potentially be undertreated and 20 patients out of 80 (25%) overtreated. This emphasizes the need to decide on such treatment based on other prognostic factors or use them in combination with the assessed lymph node status.
The strength of this study, beside the use of several imaging criteria for lymph node metastases, is the homogenous patient cohort; all examined with 64-multidetector CT and all having primary surgery allowing histopathology of the resected specimen as reference.
Limitations of the study were the retrospective setting. The assessment by only one observer could reduce the robustness and reproducibility of the imaging criteria. These criteria must be validated in a multi reader setting. There were also a limited number of patients with some of the criteria. Furthermore, the histopathological tissues were not reevaluated and there was no possibility to match individual lymph nodes between imaging and histopathology. Another possible limitation was that we also excluded T4 tumours in the study. We argue that the high rate of lymph node metastases in this group of patients (around 37%) is likely to bias the radiologist when looking on CT and assessing the lymph nodes. No texture analysis software was available at the time of the study. We believe that texture analysis may have a role in the context of characterizing regional lymph nodes on CT in colon cancer although the approach in this setting is rather unexplored and may be subjected to a separate study.
Conclusion
Various imaging criteria for lymph node metastases on CT have been used in previous literature. The results of the present study do not support use of any the commonly used criteria for lymph node metastases. When performing preoperative CT in patients with colon cancer, the imaging criteria that allow the best prediction of stage III disease are either the presence of at least one lymph node with internal heterogeneity or the presence of at least one lymph node with internal heterogeneity and/or irregular outer border. These criteria have to be validated in prospective studies.
Acknowledgements
No acknowledgements.
Funding
Financial support was provided through the regional agreement on medical training and clinical research (ALF) between the Stockholm County Council and Karolinska Institutet.
Availability of data and materials
Not applicable.
Authors’ contributions
Study concepts and design: ER, MA-N, TH, LB. Performing study: ER, LB. Evaluating exams: ER, LB. Collection of data: ER. Analysis of data: ER, MA-N, TH, LB. Manuscript preparation: ER, LB. Manuscript reviewing and editing: ER, MA-N, TH, LB. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Each author has participated sufficiently in the submission and takes public responsibility for its content.
Ethics approval and consent to participate
The study was approved by the regional ethical review board (no 2012/1527-31/1).
Contributor Information
Erik Rollvén, Phone: +46851772210, Email: erik.rollven@ki.se.
Mirna Abraham-Nordling, Email: mirna.abraham.nordling@ki.se.
Torbjörn Holm, Email: torbjorn.holm@karolinska.se.
Lennart Blomqvist, Email: lennart.k.blomqvist@ki.se.
References
- 1.Swedish Colorectal Cancer Study Group. National Colon Cancer Report. 2011. http://www.cancercentrum.se/sv/Kvalitetsregister/-Kolorektalcancer/Rapporter. ISBN 000-91-89048-46-6.
- 2.Dighe S, Swift I, Brown G. CT staging of colon cancer. Clin Radiol. 2008;63:1372–1379. doi: 10.1016/j.crad.2008.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Derwinger K, Carlsson G, Gustavsson B. A study of lymph node ratio as a prognostic marker in colon cancer. Eur J Surg Oncol. 2008;34:771–775. doi: 10.1016/j.ejso.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Ceelen W, Van Nieuwenhove Y, Pattyn P. Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review. Ann Surg Oncol. 2010;17:2847–2855. doi: 10.1245/s10434-010-1158-1. [DOI] [PubMed] [Google Scholar]
- 5.Chang YJ, Chang YJ, Chen LJ, Chung KP, Lai MS. Evaluation of lymph nodes in patients with colon cancer undergoing colon resection: a population-based study. World J Surg. 2012;36:1906–1914. doi: 10.1007/s00268-012-1568-2. [DOI] [PubMed] [Google Scholar]
- 6.Smith NJ, Bees N, Barbachano Y, Norman AR, Swift RI, Brown G. Preoperative computed tomography staging of nonmetastatic colon cancer predicts outcome: implications for clinical trials. Br J Cancer. 2007;96:1030–1036. doi: 10.1038/sj.bjc.6603646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huh JW, Jeong YY, Kim HR, Kim YJ. Prognostic value of preoperative radiological staging assessed by computed tomography in patients with nonmetastatic colon cancer. Ann Oncol. 2012;23:1198–1206. doi: 10.1093/annonc/mdr404. [DOI] [PubMed] [Google Scholar]
- 8.Dighe S, Swift I, Magill L, Handley K, Gray R, Quirke P, et al. Accuracy of radiological staging in identifying high-risk colon cancer patients suitable for neoadjuvant chemotherapy: a multicentre experience. Colorectal Dis. 2012;14:438–444. doi: 10.1111/j.1463-1318.2011.02638.x. [DOI] [PubMed] [Google Scholar]
- 9.Acunas B, Rozanes I, Acunas G, Celik L, Sayi I, Gokmen E. Preoperative CT staging of colon carcinoma (excluding the recto-sigmoid region) Eur J Radiol. 1990;11:150–153. doi: 10.1016/0720-048X(90)90166-9. [DOI] [PubMed] [Google Scholar]
- 10.Burton S, Brown G, Bees N, Norman A, Biedrzycki O, Arnaout A, et al. Accuracy of CT prediction of poor prognostic features in colonic cancer. Br J Radiol. 2008;81:10–19. doi: 10.1259/bjr/19492531. [DOI] [PubMed] [Google Scholar]
- 11.Zbar AP, Rambarat C, Shenoy RK. Routine preoperative abdominal computed tomography in colon cancer: a utility study. Tech Coloproctol. 2007;11:105–109. doi: 10.1007/s10151-007-0338-x. [DOI] [PubMed] [Google Scholar]
- 12.Harvey CJ, Amin Z, Hare CM, Gillams AR, Novelli MR, Boulos PB, et al. Helical CT pneumocolon to assess colonic tumors: radiologic-pathologic correlation. AJR Am J Roentgenol. 1998;170:1439–1443. doi: 10.2214/ajr.170.6.9609150. [DOI] [PubMed] [Google Scholar]
- 13.Gazelle GS, Gaa J, Saini S, Shellito P. Staging of colon carcinoma using water enema CT. J Comput Assist Tomogr. 1995;19:87–91. doi: 10.1097/00004728-199501000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Hundt W, Braunschweig R, Reiser M. Evaluation of spiral CT in staging of colon and rectum carcinoma. Eur Radiol. 1999;9:78–84. doi: 10.1007/s003300050632. [DOI] [PubMed] [Google Scholar]
- 15.Leufkens AM, van den Bosch MA, van Leeuwen MS, Siersema PD. Diagnostic accuracy of computed tomography for colon cancer staging: a systematic review. Scand J Gastroenterol. 2011;46:887–894. doi: 10.3109/00365521.2011.574732. [DOI] [PubMed] [Google Scholar]
- 16.Anderson EM, Betts M, Slater A. The value of true axial imaging for CT staging of colonic cancer. Eur Radiol. 2011;21:1286–1292. doi: 10.1007/s00330-010-2019-9. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1–29. doi: 10.1007/s10147-011-0315-2. [DOI] [PubMed] [Google Scholar]
- 18.Kanamoto T, Matsuki M, Okuda J, Inada Y, Tatsugami F, Tanikake M, et al. Preoperative evaluation of local invasion and metastatic lymph nodes of colorectal cancer and mesenteric vascular variations using multidetector-row computed tomography before laparoscopic surgery. J Comput Assist Tomogr. 2007;31:831–839. doi: 10.1097/RCT.0b013e3180517af3. [DOI] [PubMed] [Google Scholar]
- 19.Sobin LH. TNM, sixth edition: new developments in general concepts and rules. Semin Surg Oncol. 2003;21:19–22. doi: 10.1002/ssu.10017. [DOI] [PubMed] [Google Scholar]
- 20.Sobin LH, Compton CC. TNM seventh edition: what’s new, what's changed: communication from the International Union against cancer and the American Joint Committee on cancer. Cancer. 2010;116:5336–5339. doi: 10.1002/cncr.25537. [DOI] [PubMed] [Google Scholar]
- 21.Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, et al. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227:371–377. doi: 10.1148/radiol.2272011747. [DOI] [PubMed] [Google Scholar]
- 22.de Vries FE, da Costa DW, van der Mooren K, van Dorp TA, Vrouenraets BC. The value of pre-operative computed tomography scanning for the assessment of lymph node status in patients with colon cancer. Eur J Surg Oncol. 2014;40:1777–1781. doi: 10.1016/j.ejso.2014.08.483. [DOI] [PubMed] [Google Scholar]
- 23.Rodriguez-Bigas MA, Maamoun S, Weber TK, Penetrante RB, Blumenson LE, Petrelli NJ. Clinical significance of colorectal cancer: metastases in lymph nodes < 5 mm in size. Ann Surg Oncol. 1996;3:124–130. doi: 10.1007/BF02305790. [DOI] [PubMed] [Google Scholar]
- 24.Kwak JY, Kim JS, Kim HJ, Ha HK, Yu CS, Kim JC. Diagnostic value of FDG-PET/CT for lymph node metastasis of colorectal cancer. World J Surg. 2012;36:1898–1905. doi: 10.1007/s00268-012-1575-3. [DOI] [PubMed] [Google Scholar]
- 25.Abdel-Nabi H, Doerr RJ, Lamonica DM, Cronin VR, Galantowicz PJ, Carbone GM, et al. Staging of primary colorectal carcinomas with fluorine-18 fluorodeoxyglucose whole-body PET: correlation with histopathologic and CT findings. Radiology. 1998;206:755–760. doi: 10.1148/radiology.206.3.9494497. [DOI] [PubMed] [Google Scholar]
- 26.Furukawa H, Ikuma H, Seki A, Yokoe K, Yuen S, Aramaki T, et al. Positron emission tomography scanning is not superior to whole body multidetector helical computed tomography in the preoperative staging of colorectal cancer. Gut. 2006;55:1007–1011. doi: 10.1136/gut.2005.076273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JH, Lee MR. Positron emission tomography/computed tomography in the staging of colon cancer. Ann Coloproctol. 2014;30:23–27. doi: 10.3393/ac.2014.30.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cipe G, Ergul N, Hasbahceci M, Firat D, Bozkurt S, Memmi N, et al. Routine use of positron-emission tomography/computed tomography for staging of primary colorectal cancer: does it affect clinical management? World J Surg Oncol. 2013;11:49. doi: 10.1186/1477-7819-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


