Abstract
Objectives
Anorexia nervosa (AN) is a life‐threatening mental health condition. A core feature is a disturbance of body image, such that sufferers see themselves as fatter than they actually are.
Design
We tested the effectiveness of a novel training programme to recalibrate our participants’ perception of body size.
Methods
In a novel adaptation of a cognitive bias training programme, participants judged the body size of a series of female bodies and were given feedback to improve their accuracy over four daily training sessions. In Study 1, we recruited young women with high concerns about their body size for a randomized controlled study. In Study 2, we then applied the training programme to a case series of women with atypical AN.
Results
In Study 1, the training programme significantly improved the body size judgements of women with high body concerns compared to controls. We also found evidence of improved body image and reduced eating concerns in this group. In Study 2, the programme again recalibrated the body size judgements of women with atypical AN. We also saw evidence of a clinically meaningful reduction in their body size and eating‐disordered concerns.
Conclusions
This training has the potential to be a valuable treatment used together with more traditional talking therapies.
Statement of contribution.
What is already known on this subject?
A core feature of anorexia nervosa (AN) is an overestimation of body size; sufferers believe themselves to be larger than they are in reality. This study shows that an individual's perceptual boundary between what they classify as a fat versus a thin body is not immutable; it can be changed through a cognitive bias training programme.
What does this study add?
This means that body size overestimation may now be treatable.
Critically, as well as improving the accuracy of body size judgements, we also found a clinically significant improvement in participants’ eating‐disordered concerns.
This demonstrates that a targeted behavioural training regime can change body perception, and the central role that body overestimation has in eating‐disordered beliefs.
Keywords: body size training, body size judgements, anorexia nervosa syndrome disorder, anorexia nervosa
Background
Anorexia nervosa (AN) is a serious psychiatric illness with significant psychological and physiological impacts, affecting up to 1% of the female population (Treasure, Claudino, & Zucker, 2010). Current therapeutic regimes have only limited success in treating this condition where long‐term mortality can reach 10% and the relapse rate may be as high as 40% over the first 12‐month post‐discharge (Berkman, Lohr, & Bulik, 2007; Carter et al., 2012). Diagnostic criteria for AN include a distorted evaluation of personal body size (American Psychiatric Association, 2013), which is a core component of psychological models of the disorder (Cash & Deagle, 1997; Fairburn, Cooper, & Shafran, 2003). Body image distortion is one of the most persistent of all eating disorder symptoms, its severity predicts long‐term treatment outcome, and its persistence increases the risk of relapse (Channon & DeSilva, 1985; Fairburn et al., 2003). Most studies have found that people with AN overestimate body size, have negative feelings towards their body, and classify lower weight bodies as fat relative to controls (Cornelissen, Bester, Cairns, Tovée, & Cornelissen, 2015; Cornelissen, Johns, & Tovée, 2013; Gardner, Jones, & Bokenkamp, 1996; George, Cornelissen, Hancock, Kiviniemi, & Tovée, 2011; Probst, Vandereycken, Vanderlinden, & Van Coppenolle, 1998; Tovée, Benson, Emery, Mason, & Cohen‐Tovée, 2003; Tovée, Emery, & Cohen‐Tovée, 2000; Williamson, Cubic, & Gleaves, 1993). This overestimation extends to judgements of other women's bodies (Cornelissen, Gledhill, Cornelissen, & Tovée, 2016). It is this overestimation and disparagement of body size, coupled with a morbid dread of becoming overweight, which may fuel a drive for thinness through abnormal eating patterns and associated behaviours (such as excessive exercise and purging).
The principal treatment for body image disturbance is cognitive behavioural therapy (CBT), to modify dysfunctional thoughts, feelings, and behaviours that contribute to a negative body image. Previous studies in eating‐disordered and non‐eating‐disordered women have suggested that being exposed to their own body in a mirror (mirror exposure therapy) can help desensitize a patient to their body appearance (Delinsky & Wilson, 2006; Key et al., 2002; Vocks, Wachter, Wucherer, & Kosfelder, 2008). However, this does not directly tackle the issue of body size overestimation. Other interventions include the following: fitness training to improve physical capacity and shift attention from appearance to functionality (Farrell, Shafran, & Lee, 2006; Jarry & Cash, 2011), media literacy to challenge the impact of images of thin bodies (Ginis & Bassett, 2011; Martin & Lichtenberger, 2002), self‐esteem enhancement to improve self‐worth (Grabe, Ward, & Hyde, 2008; Irving & Berel, 2001), and psychoeducation (O'Dea, 2004;. O'Dea & Yager, 2011). However, a recent meta‐analysis suggested that once corrections for bias (both within and across studies) in the data were applied, the effect sizes of these treatments were relatively small, strongly suggesting the need for new additional therapies to address negative body image (Alleva, Sheeran, Webb, Martijn, & Miles, 2015).
Therefore, in the current study, we tested the effectiveness of a novel body training programme to increase individual participants’ categorical boundaries for thin/fat bodies towards fatter bodies, and we tested whether this reduced participants’ body size and eating concerns. This approach has been developed from a face training programme, used to modify biases in emotion recognition in order to encourage the perception of happiness over anger in ambiguous expressions in adolescents who are at high risk of criminal offending and delinquency (Penton‐Voak et al., 2013). In the original study, participants were presented images of faces and had to make a two‐alternative forced choice (2‐AFC) decision whether a particular face was happy or angry. The face stimuli were selected at random from a sequence of images which morphed smoothly from clearly happy at one end of the continuum to clearly angry at the other end. Images in the middle of the sequence (intermediate in their expression) could be judged either way. In such a task, any given individual will tend to perceive a category boundary somewhere along this continuum, which, for them, constitutes a transition from happy to angry. However, there is no absolute location in the continuum, which corresponds to a ‘correct’ category boundary; instead, the location of this perceptual boundary is subjective and varies across different individuals. Indeed, adolescents at high risk of offending, unlike controls, tend to categorize even the intermediate faces as angry. However, by giving appropriately structured feedback, their angry–happy categorical boundary can be shifted towards the ‘happy’ end of the spectrum. Penton‐Voak et al. (2013) found that this resulted in a decrease in self‐reported anger and aggression and in independently rated aggressive behaviour. The same training algorithm has also been used to recalibrate the perception of happiness over sadness in ambiguous facial expressions in people reporting high levels of depressive symptoms to improve mood (Adams, Penton‐Voak, Harmer, Holmes, & Munafò, 2013; Penton‐Voak, Bate, Lewis, & Munafò, 2012).
We have previously shown that body size judgements are also made in a categorical manner; observers show a clear categorical boundary in making 2‐AFC judgements about whether a body is fat or thin (Tovée, Edmonds, & Vuong, 2012). Moreover, observers show a clear enhancement in discriminating between bodies in matching‐to‐sample tasks if the discrimination is between bodies at the categorical boundary compared to discriminating between bodies from within the same category (Tovée et al., 2012). Therefore, we tested the effectiveness of a modified version of the training paradigm from Penton‐Voak et al. (2013) to shift participants’ thin–fat categorical boundary and asked whether this shift would lead to a general improvement in body image concerns. It is important to emphasize that this is not the same as trying to train participants to achieve some fixed, normative goal, constituting a ‘normal’ body size. Instead, the intention was to move an individual's thin–fat categorical boundary towards fatter bodies, irrespective of their starting point on the thin‐to‐fat continuum.
We hypothesize that our training will shift a persons’ thin–fat categorical boundary, so that they will categorize as thin, bodies that they had previously categorized as fat and that this categorical shift will be accompanied by a significant reduction in their body image and eating‐disordered concerns. To test these hypotheses, we carried out two studies. In the first, we recruited young women with high concerns about their body size for a randomized controlled study to determine whether the training alters the perceptual position of the thin–fat categorical boundary with associated improvements in body image and eating concerns. In the second study, we then applied the training to a case series of women with atypical anorexia nervosa (aAN) to determine whether the training would also lead to a change in categorical boundary in this population and their more deep‐seated body image concerns.
STUDY 1
Participants
Forty participants for this study were recruited from undergraduate students at Newcastle University. Potential participants, who self‐reported no history of eating disorders, were asked to provide their height and weight and to fill in the 16‐item Body Shape Questionnaire (BSQ; Evans & Dolan, 1993). This psychometric tool indexes the degree of preoccupation and negative attitude towards body weight and body shape. Only those who achieved a BSQ score of 60 or greater (i.e., substantial body shape concerns) were eligible to participate. Participants were randomly assigned to two conditions. Twenty female participants (mean age: 18.15 years; SD: 0.37) were assigned to the intervention condition, while 20 females (mean age: 19.00 years; SD: 1.26) were assigned to the control condition. Data from previous studies of similar training programmes indicate an effect size of d ~ 1 for the effect of training on perceptual position of the categorical boundary, suggesting a total sample size of n = 34 would be sufficient to achieve 80% power at an alpha level of 5%. Table 1 describes the participants’ characteristics. Multiple t‐tests were computed, using both Satterthwaite's correction for unequal variance and Bonferroni's correction for multiple comparisons, to compare characteristics between the intervention and control groups. None exceeded the critical value of p < .0083. Ethical approval for this study was granted by the Faculty of Medical Sciences ethics committee at Newcastle University (00620/2013). All procedures contributing to Study 1 and Study 2 comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Table 1.
Demographic and questionnaire data from the participants in Study 1
| Intervention (n = 20) | Control (n = 20) | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age (years) | 18.20 | 0.37 | 19.00 | 1.27 |
| BMI | 25.40 | 5.12 | 23.90 | 3.01 |
| Screening BSQ | 68.20 | 7.25 | 73.00 | 11.52 |
| EDE‐Q | 3.09 | 1.01 | 3.67 | 0.83 |
| BDI | 16.70 | 9.04 | 17.80 | 12.01 |
| RSE | 16.00 | 4.83 | 13.90 | 4.45 |
BMI = Body Mass Index; BSQ = Body Shape Questionnaire; BDI = Beck Depression Inventory; EDE‐Q = Eating Disorder Examination Questionnaire global score; BDI = Beck Depression Inventory; RSE = Rosenberg Self‐Esteem scale.
Measures
Psychometric and anthropometric measurements
To assess participants’ attitudes to body shape, weight, and eating, we used the Eating Disorders Examination Questionnaire (EDE‐Q), which is a self‐report version of the Eating Disorder Examination (EDE) structured interview (Fairburn & Beglin, 1994). This is commonly used as a screening questionnaire for eating‐disordered behaviour and has been normed for young women and undergraduates (Luce, Crowther & Pole, 2008; Mond, Hay, Rodgers, & Owen, 2006). The questionnaire contains four subscales reflecting the severity of aspects of the psychopathology of eating disorders: (1) the Restraint (EDE‐restraint) subscale investigates the restrictive nature of eating behaviour; (2) the Eating Concern (EDE‐eating concerns) subscale measures preoccupation with food and social eating; (3) the Shape Concern (EDE‐shape concerns) subscale investigates dissatisfaction with body shape; and (4) the Weight Concern (EDE‐weight concerns) subscale assesses dissatisfaction with body weight. The EDE‐Q (range 0–6) also measures overall disordered eating behaviour. Furthermore, it provides frequency data on key behavioural features of eating disorders. We also used the Beck Depression Inventory (BDI; range 0–63; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) that measures participants’ level of depression and the Rosenberg Self‐Esteem Scale (RSE; range 0–30; Rosenberg, 1965) that measures self‐esteem. In addition, we calculated the participants’ body mass index (BMI) from their weight obtained with a set of calibrated scales and their height obtained with a stadiometer.
Stimulus image preparation
We used computer‐generated imagery (CGI) methods to create a sequence of 3D images of a model whose body shape changes systematically with increasing BMI (for details see Cornelissen et al., 2015). The advantages of the CGI stimuli are as follows: (1) the identity of the person in the image is maintained over a wide BMI range; (2) the body shape changes at different BMI levels are realistic; and (3) the 3D rendered stimulus images are high definition and photorealistic. We used a set of 15 images ranging in BMI from 15.4 to 33.7 (drawn from the image database in Cornelissen et al., 2015).
Perceptual training paradigm
An E‐Prime (http://www.pstnet.com/eprime.cfm) script was modified from Penton‐Voak et al. (2012) and Penton‐Voak et al. (2013) to run the training paradigm on a Windows PC with a 19″ LCD monitor panel (1,600 × 1,200 native pixel resolution, 32‐bit colour depth). Each trial of the baseline and training conditions began with a central fixation cross which was shown for 1,500–2,500 ms (randomly jittered). This was replaced by an image of a body for 150 ms followed immediately by a mask of visual noise for 150 ms. Finally, the mask was replaced by a prompt screen, containing a ‘?’, to indicate that participants should make their judgement of ‘fat’ or ‘thin’ (a 2‐AFC) and respond by key‐press. No time limits for the response were imposed on the task. The baseline condition comprised 45 trials in all (three presentations of each of the 15 stimulus images) in randomized order. Participant responses were used to calculate the categorical boundary/mid‐point at which they shifted from perceiving thinness to perceiving fatness in the body sequence 50% of the time (see upper row of Figure 1). Each training session typically took 30–45 min.
Figure 1.

The middle row shows part of the body sequence varying in body mass index. The top row illustrates the results from a baseline assessment and the position of the categorical boundary prior to training. The bottom row illustrates the results from the post‐training test session, showing that the categorical boundary has shifted relative to the pre‐training result.
Trials from the training phase differed from the baseline procedure in that feedback (i.e., ‘Incorrect! That body was fat’ or ‘Correct. That body was thin’) was provided to the participant following their keyboard response. The training phase was made up of six blocks, with 31 trials in each block. From pilot testing, bodies 1–2 and 14–15 were almost always classified as ‘thin’ and ‘fat’, respectively, so these were only presented once in training. Bodies 3–5 were responded to less frequently as being ‘thin’, and 11–13 less frequently as being ‘fat’ and were therefore presented twice. The remaining bodies, 6–10, were presented three times each as responses to these bodies were the least clear‐cut.
In the intervention condition, the nature of the feedback given was ‘inflationary’ and was designed to shift a participant's categorical boundary by two bodies higher up along the image sequence (from low to high BMI) than their baseline measure. In this way, participants were retrained to judge bodies near their categorical boundary, which they had previously judged as fat during baseline measurement, to be thin. By contrast, in the control condition, the feedback to participants was consistent with their categorical boundary as measured at baseline, and was intended merely to reinforce their existing categorical boundary.
Procedure
The training took place over 4 days. On Day 1, participants first completed the EDE‐Q, RSE, and BDI questionnaires and had their height and weight measured. Then, they carried out the first baseline and training sequences for the categorical perception task. On Days 2 and 3, participants carried out the baseline and the training sequences only. On Day 4, participants completed the baseline and training sequences, followed by the EDE‐Q questionnaire. To test retention of the training on Day 14, participants carried out the baseline sequence and then completed the EDE‐Q questionnaire.
Results
We used PROC MIXED in the SAS software Version 9.3 (SAS Institute Inc., Cary, NC, USA) to fit a multilevel model to the perceptual training data which included three main effects (i.e., group: intervention vs. control; training: baseline vs. post‐training threshold; test day: 1, 2, 3, 4, 14) and all possible two‐ and three‐way interactions. In addition, based on significant reductions in −2log likelihood, we permitted both individual slope and intercept variation for each subject and specified an ‘unstructured’ variance–covariance structure for the G‐matrix. This model allowed us to compute post‐hoc pairwise tests, which were controlled for multiple comparisons, as illustrated in Figure 2A,B. We found statistically significant main effects of test day, F(4, 304) = 6.69, p < .0001, and training, F(1, 204) = 15.11, p = .0001, on perceptual thresholds, but not for group, F(1, 38) = 1.46, p = .23. In addition, we found statistically significant interactions: group × test day, F(4, 304) = 16.62, p < .0001, and group × training, F(1, 304) = 15.93, p < .0001, but not training × test day, F(3, 304) = 0.14, p = .93, nor training × group × test day, F(3, 304) = 0.08, p = .97.
Figure 2.
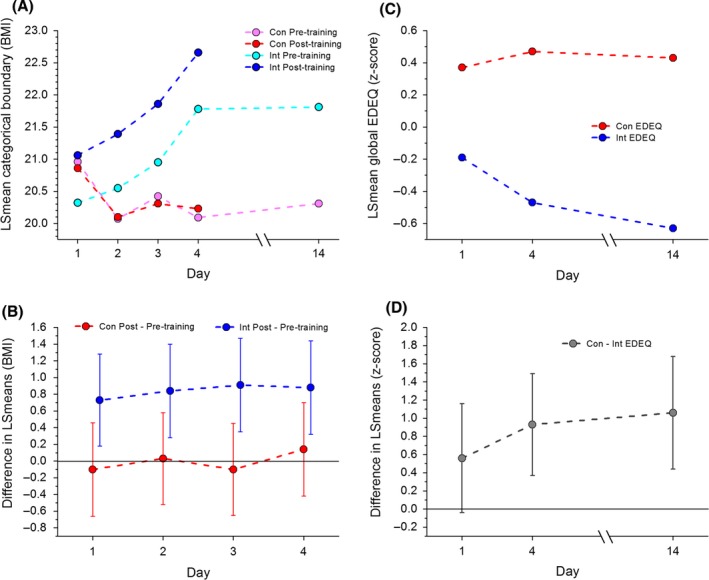
(A) A plot of the mean value of body mass index at the categorical boundary, predicted from the multilevel model as a function of measurement day. Pink and red circles represent control group pre‐ and post‐training thresholds, respectively. Cyan and blue circles represent intervention group pre‐ and post‐training thresholds, respectively. (B) A plot of the predicted differences between pre‐ and post‐training categorical threshold, with 95% CIs, as a function of training day. Confidence intervals that straddle zero are not significant at p < .05. Blue circles represent the intervention group, and red circles the control group. (C) A plot of predicted global EDE‐Q z‐scores as a function of measurement day. Blue circles represent the intervention group and red circles the control group. (D) A plot of the predicted differences in global EDE‐Q z‐scores between the control and training groups as a function of measurement day, with 95% CIs, as a function of training day. Confidence intervals that straddle zero are not significant at p < .05.
Figure 2A shows a plot of the LSmeans for the categorical boundary, derived from the multilevel model, as a function of training day. The data are plotted separately for the control (red and pink) and intervention groups (blue and cyan), each split according to whether the measurement was the pre‐training baseline (cyan and pink) for that day or the post‐training value (red and blue). We found negligible difference between the baseline and post‐training thresholds for the controls, as illustrated in Figure 2B. This plot shows the LSmean difference between baseline and post‐training measurements as a function of training day, separately for the intervention and control groups. The error bars represent the 95% CIs for the pairwise comparisons. By contrast, Figure 2B shows a significant effect of training on each training day for the intervention group. This result, together with the significant group × test day and group × training interactions, shows that training causes an accumulating shift in participants’ categorical boundary towards heavier bodies for the intervention group, but not the control group. Finally, we found that the comparison between Day 1 baseline and Day 14 baseline showed a statistically significantly increase in BMI at the category boundary for the intervention group, t(53.7) = 4.42, p < .0001. In comparison, the controls showed a small reduction that was marginally statistically significant, t(53.7) = −1.86, p = .07. This suggests that, in this sample of non‐eating‐disordered participants, all of whom have high body shape concerns, the perceptual training effect on their categorical boundaries persisted in the intervention group for at least 2 weeks.
For the psychological measures, we used PROC MIXED in the SAS software Version 9.3 (SAS Institute Inc.) to fit separate multilevel models to participants’ global EDE‐Q scores, as well as the EDE‐restraint, EDE‐eating concerns, EDE‐shape concerns, and EDE‐weight concerns subscale scores, measured on: Day 1 before the perceptual training, Day 4 after perceptual training, and on Day 14 after the baseline perceptual measurement. Each model contained group and test day as main effects, together with the interaction group × test day. Continuous outcome and explanatory variables were centred for these analyses by converting them to z‐scores. As before, based on significant reductions in −2log likelihood, we permitted both individual slope and intercept variation for each subject and specified an ‘unstructured’ variance–covariance structure for the G‐matrix. Each model allowed us to compute post‐hoc pairwise comparisons, all of which are controlled for multiple comparisons, and they are all reported in Table 2. The LSmeans for the global EDE‐Q scores for the intervention (blue) and control (red) groups, derived from the multilevel model, are plotted as a function of training day in Figure 2C. The LSmean differences in global EDE‐Q scores between the control and intervention groups, together with their 95% CIs, are plotted as a function of training day in Figure 2D.
Table 2.
Summary table of the psychological scores from Study 1
| Measure | Test day | Intervention raw score Mean (SD) | Control raw score Mean (SD) | Difference Z‐score | 95% CI Z‐score | p‐value |
|---|---|---|---|---|---|---|
| EDE‐Q | 1 | 3.09 (1.01) | 3.67 (0.83) | 0.56 | −0.012 to 1.13 | .06 |
| 4 | 2.81 (0.97) | 3.77 (0.82) | 0.93 | 0.37 to 1.49 | .002 | |
| 14 | 2.64 (1.08) | 3.73 (0.91) | 1.04 | 0.44 to 1.68 | .001 | |
| EDE‐restraint | 1 | 2.55 (1.31) | 3.36 (1.41) | 0.58 | −0.04 to 1.21 | .07 |
| 4 | 2.31 (1.23) | 3.41 (1.31) | 0.79 | 0.20 to 1.38 | .01 | |
| 14 | 2.13 (1.18) | 3.41 (1.38) | 0.92 | 0.33 to 1.51 | .003 | |
| EDE‐eating concerns | 1 | 2.30 (1.43) | 3.00 (1.54) | 0.50 | −0.18 to 1.18 | .14 |
| 4 | 1.94 (1.19) | 2.81 (1.15) | 0.62 | 0.09 to 1.16 | .12 | |
| 14 | 1.82 (1.37) | 2.59 (1.44) | 0.55 | −0.09 to 1.19 | .09 | |
| EDE‐shape concerns | 1 | 3.42 (1.13) | 4.13 (1.00) | 0.63 | 0.03 to 1.23 | .04 |
| 4 | 3.29 (1.19) | 4.21 (0.78) | 0.81 | 0.24 to 1.38 | .006 | |
| 14 | 3.00 (1.24) | 4.18 (0.83) | 1.04 | 0.45 to 1.64 | .001 | |
| EDE‐weight concerns | 1 | 4.08 (1.00) | 4.18 (0.81) | 0.09 | −0.50 to 0.68 | .75 |
| 4 | 3.70 (1.02) | 4.66 (0.82) | 0.97 | 0.37 to 1.57 | .002 | |
| 14 | 3.59 (0.94) | 4.73 (0.81) | 1.15 | 0.58 to 1.72 | .0002 |
EDE‐Q = Eating Disorder Examination Questionnaire global score; EDE‐Q res = Eating Disorder Examination Questionnaire eating restraint subscale; EDE‐Q eat = Eating Disorder Examination Questionnaire eating concern subscale; EDE‐Q sc = Eating Disorder Examination Questionnaire body shape concern subscale; EDE‐Q wc = Eating Disorder Examination Questionnaire weight concern subscale.
Table 2 shows that, with the exception of the EDE‐eating concerns scores, we found statistically significant reductions in EDE‐Q, EDE‐restraint, EDE‐weight concerns, and EDE‐shape concerns scores for the intervention group compared to controls for Days 4 and 14 but not Day 1. Broadly, these results suggest the training has a positive effect on participants’ attitudes to body shape, weight, and some aspects of their eating behaviour. Finally, we compared Day 1 with Day 14 scores on the EDE‐Q and its subscales. Overall, the EDE‐Q global score showed a modest, albeit marginally significant, reduction for the intervention group, t(75.5) = −1.81, p = .07, and no difference for controls, t(75.5) = 0.24, p = .81. The EDE‐weight concerns subscale of the EDE‐Q also showed a marginally significant reduction for the intervention group, t(73.3) = −1.94, p = .06, and a significant increase for controls, t(73.3) = 2.16, p = .03. This suggests that, in a non‐eating‐disordered sample of women, all of whom have high concerns about body shape, the perceptual intervention shifts attitudes to body shape, weight, and eating in a way that would be beneficial for people with eating disorders.
Discussion
Study 1 demonstrates that the training programme significantly shifts the thin–fat categorical boundary in individuals with high body concerns. This change is specific to the intervention group who received inflationary feedback. There was a significant reduction in the EDE‐Q scores, particularly on the restraint, weight, and shape subscales, suggesting that the training not only shifts categorical boundary but also generalizes to impact on body size and shape concerns and eating restraint. These changes were retained at 2 weeks post‐training, suggesting that these represent statistically significant and long‐lasting changes to attitudes to body size and eating. This suggests that the training has the potential to be used to improve body image. However, it can be argued that women with an eating disorder have more deep‐seated concerns that may be harder to modify. To test the training's effectiveness and feasibility, we therefore recruited an eating‐disordered population for Study 2.
STUDY 2
Rationale
In Study 2, we recruited an eating‐disordered cohort of women to determine whether it was also possible to alter their thin–fat categorical boundary and whether there would be an associated positive change in their mental state. In the absence of a control group, we wanted to control for the possibility that changes in the psychological scores over time might occur merely as a result of habituation to the task, given that the EDE‐Q was repeated over multiple test days. For this reason, we included another cognitive task, the Wechsler Adult Intelligence Scale (WAIS‐II) Digit Span, the responses to which should not be influenced by concerns about body shape and weight. Nevertheless, because we administered this task as many times as the psychological questionnaires about body shape, weight, and eating, we should also expect there to be changes in participants’ responses which are related to practice effects. Therefore, we included Digit Span as a covariate in our analyses of the psychological data, on the grounds that it should control for such influences, and any real changes in attitude towards body image should survive this statistical control.
Participants
We recruited 21 female outpatients into the study (mean age M = 27.71, SD = 7.48), all of whom had a current diagnosis of AN, but whose BMI tends to be higher than is typically the case for inpatients (mean BMI M = 19.51, SD = 3.30) and so no longer fit the strict DSM‐5 diagnostic criteria with respect to BMI, although they still have very high body size concerns and eating‐disordered behaviours. Means and standard deviations for BSQ and EDE‐Q were as follows: 62.48 (18.77) and 3.63 (1.60), respectively. We therefore refer to this group as suffering from aAN, following Cornelissen et al. (2015). Data from previous studies of similar training programmes indicate an effect size of dz > 1 for the pre‐ to post‐training change in perceptual position of the categorical boundary, suggesting a total sample size of n = 10 would be sufficient to achieve 80% power at an alpha level of 5%.
Three aAN participants failed to adhere to the training regime; therefore, we ran two different analyses. In the first, based on an intention to treat, we included all 21 participants. In the second analysis, we excluded these three participants.
The experimental procedures and methods were approved by the local ethics committee at Northumbria University. Participants were recruited through two third sector organizations: the Beating Eating Disorders Organisation and the Northern Initiative on Women and Eating Organisation.
Measures
We used the same psychometric, anthropometric, and psychophysical measures as in Study 1. However, we did not include the BDI and RSE because Experiment 2 included one more measurement point than Study 1, and we did not want to overburden participants. We also modified the EDE‐Q. Participants filled in the EDE‐Q at Day 1 (before the training), at Day 4 (after the training), at Day 7, and Day 30. The EDE‐Q asks participants to report concerns/behaviours which occurred over the previous 28 days. This time scale was retained on Day 1 and 30, but on Day 4, we altered the time to the last 24 hr, and on Day 7, we altered the scale to the last 7 days. This allowed us to detect the changes the training may have had on body image and eating concerns, and which might otherwise be masked by the longer time frame which also covered the pre‐training period. In addition, as mentioned above, we included the Digit Span task from the WAIS‐R IQ test battery (Wechsler, 1981), which assesses short‐term memory (mean Digit Span on initial testing was M = 13.85, SD = 3.82).
Procedure
On Day 1, participants first completed the Digit Span task, the BSQ and EDE‐Q questionnaires and had their BMI measured. They then carried out the first baseline and training sequences for the categorical perception task. On Days 2 and 3, participants carried out the baseline and the training sequences only. On Day 4, participants completed the Digit Span task and the EDE‐Q questionnaire, followed by the baseline and training sequences. On Days 7 and 30, participants completed the Digit Span task and the EDE‐Q questionnaire and carried out the baseline sequence only.
Results
Based on intention to treat, PROC MIXED in the SAS software Version 9.3 (SAS Institute Inc.) was used to fit a multilevel model to the perceptual training data for all 21 participants. This included two main effects (i.e., training: baseline vs. post‐training threshold; test day: 1, 2, 3, 4, 7, 30) and the two‐way interaction between them. Based on significant reductions in −2log likelihood, we permitted both individual slope and intercept variation for each subject and specified an ‘unstructured’ variance–covariance structure for the G‐matrix. As before, this allowed us to compute post‐hoc pairwise tests, which were controlled for multiple comparisons, and these are illustrated in Figure 3A,B. We found statistically significant main effects of test day, F(5, 16.6) = 4.07, p = .01, and pre‐/post‐training, F(1, 64) = 21.53, p < .0001, on perceptual thresholds, but no significant interaction between them, F(3, 64) = 1.13, p = .35.
Figure 3.
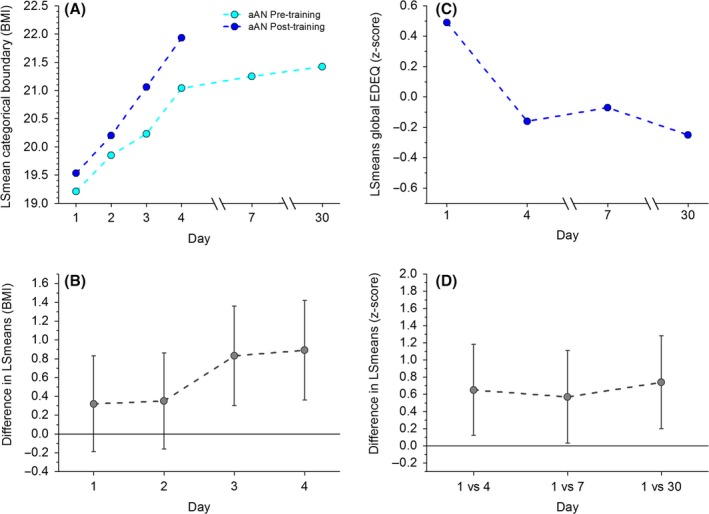
(A) A plot of the mean value of body mass index at the categorical boundary, predicted from the multilevel model as a function of measurement day. Cyan and blue circles represent pre‐ and post‐training thresholds, respectively, for the atypical anorexia (aAN) participants in experiment 2. (B) A plot of the predicted differences between pre‐ and post‐training categorical threshold, with 95% CIs, as a function of training day. Confidence intervals that straddle zero are not significant at p < .05. (C) A plot of the mean predicted global EDE‐Q z‐scores as a function of measurement day for aAN participants in experiment 2. (D) A plot of the predicted differences in global EDE‐Q z‐scores between the baseline measurement on Day 1 and the post‐training measurements on Days 4, 7, and 30, with 95% CIs. Confidence intervals that straddle zero are not significant at p < .05.
Figure 3A shows a plot of the LSmean categorical boundary from the perceptual task, derived from the multilevel model, as a function of training day. The data are plotted separately for the pre‐training baseline for that day (cyan) or the post‐training value (blue). We found statistically significant differences between the pre‐training baseline and post‐training thresholds for Days 3 and 4, but not 1 and 2, as illustrated in Figure 3B. Figure 3A shows a somewhat surprising difference between the Day 1 post‐training threshold (19.53) and a higher Day 2 pre‐training threshold (19.85). However, this difference was not statistically significant, t(38.8) = 0.95, p = .348. Overall, these results, together with the significant main effects of test day and group, show that training is associated with an accumulating shift in the categorical boundary towards heavier bodies in the aAN participants. Finally, we found that the comparison between Day 1 baseline and Day 30 baseline showed a statistically significant increase in categorical boundary, t(21.9) = 3.06, p = .006. This suggests that, in this sample of aAN participants, the change in perceptual training persisted for at least a month.
For the psychological measures, we used PROC MIXED in the SAS software Version 9.3 (SAS Institute Inc.) to fit separate multilevel models to participants’ EDE‐Q, EDE‐restraint, EDE‐eating concerns, EDE‐shape concerns, and EDE‐weight concerns scores, measured on Days 1, 4, 7, and 30. Continuous outcome and explanatory variables were centred for these analyses by converting them to z‐scores. Each model comprised the main effect of test day, together with chronological age and Digit Span as covariates. As before, based on significant reductions in −2log likelihood, we permitted both individual slope and intercept variation for each subject and specified an ‘unstructured’ variance–covariance structure for the G‐matrix.
The first analysis, based on an intention to treat, and which included the three participants who failed to carry out the training programme as designed, did not produce statistically significant effects of any explanatory variable for EDE‐Q or any of its four subscores. The analysis for the 18 aAN participants, who did complete the programme as required, was more successful. The post‐hoc pairwise comparisons from these models are all reported in Table 3, and the data for EDE‐Q are plotted in Figure 3C,D.
Table 3.
Summary table of the psychological scores on different test days, and the statistical comparisons between them, from Study 2
| Measure | Test day | Mean (SD) (raw score) | Comparison point | Difference (z‐score) | 95% CI (z‐score) | p‐value |
|---|---|---|---|---|---|---|
| EDE‐Q | 1 | 3.43 (1.64) | Day 1 versus 4 | 0.65 | 0.13 to 1.18 | .02 |
| 4 | 2.69 (1.74) | Day 1 versus 7 | 0.57 | 0.02 to 1.12 | .04 | |
| 7 | 2.91 (1.84) | Day 1 versus 30 | 0.74 | 0.20 to 1.28 | .008 | |
| 30 | 2.63 (1.68) | |||||
| EDE‐restraint | 1 | 3.16 (1.69) | Day 1 versus 4 | 0.59 | −0.07 to 1.25 | .08 |
| 4 | 2.50 (1.77) | Day 1 versus 7 | 0.65 | −0.02 to 1.32 | .06 | |
| 7 | 2.44 (1.87) | Day 1 versus 30 | 0.66 | −0.004 to 1.33 | .05 | |
| 30 | 2.45 (1.76) | |||||
| EDE‐eating concerns | 1 | 2.89 (2.09) | Day 1 versus 4 | 0.79 | 0.14 to 1.43 | .02 |
| 4 | 2.03 (1.86) | Day 1 versus 7 | 0.66 | −0.03 to 1.35 | .06 | |
| 7 | 2.37 (2.00) | Day 1 versus 30 | 0.84 | 0.22 to 1.47 | .01 | |
| 30 | 2.06 (1.69) | |||||
| EDE‐shape concerns | 1 | 4.08 (1.47) | Day 1 versus 4 | 0.73 | 0.14 to 1.32 | .02 |
| 4 | 3.15 (1.77) | Day 1 versus 7 | 0.59 | −0.06 to 1.25 | .07 | |
| 7 | 3.45 (1.95) | Day 1 versus 30 | 0.76 | 0.15 to 1.36 | .01 | |
| 30 | 3.18 (1.77) | |||||
| EDE‐weight concerns | 1 | 3.58 (1.97) | Day 1 versus 4 | 0.38 | −0.15 to 0.92 | .16 |
| 4 | 3.10 (2.11) | Day 1 versus 7 | 0.33 | −0.23 to 0.89 | .25 | |
| 7 | 3.26 (2.16) | Day 1 versus 30 | 0.54 | 0.001 to 1.09 | .05 | |
| 30 | 2.83 (1.87) |
EDE‐Q = Eating Disorder Examination Questionnaire global score. EDE‐Q res = Eating Disorder Examination Questionnaire eating restraint subscale. EDE‐Q eat = Eating Disorder Examination Questionnaire eating concern subscale. EDE‐Q sc = Eating Disorder Examination Questionnaire body shape concern subscale. EDE‐Q wc = Eating Disorder Examination Questionnaire weight concern subscale.
Table 3 shows that, in the smaller sample of 18 aAN participants who completed the training regime as prescribed, perceptual training was associated with significant reductions in body shape, weight, and eating concerns (with the exception of EDE‐restraint), even when Digit Span was controlled for. Moreover, these reductions persisted up to a month from initial testing.
A key question in this test of the training regime is whether the perceptual training and the alteration in the categorical boundary may be linked to the observed changes in psychological profile. If so, then the degree to which the categorical boundary is shifted should be proportional to the change in psychological profile. In the case of Study 1, the intervention produced a largely uniform shift in the boundary with comparatively little variation between individuals in the shift (mean change in BMI units: 2.33; SD: 2.32) and the change in the global EDE‐Q score (mean change: −0.28; SD: 0.33), and there was no significant correlation between boundary shift and psychological change. In the case of Study 2, where participants’ body image concerns are more deeply established, there was greater variation in the effect of the training on the categorical boundary position (mean change: 2.75; SD: 3.56) and their psychological scores (mean change: −0.45; SD: 1.03) consistent with a greater resistance to change in some aAN participants. In this case, there was a substantial correlation between how far the boundary shifted and the change in the psychological scores (r = −.63, p = .004), suggesting the two may be linked. This correlation with the categorical shift held for all the EDE‐Q subscales, not just those linked to body size and shape (EDE‐eating concerns, r = −.65; EDE‐restraint, r = −.56; EDE‐shape concerns, r = −.53; EDE‐weight concerns, r = −.52).
Discussion
In this set of studies, we tested the use of a novel cognitive bias modification technique to shift body size perception and reduce body image concerns which are a core feature of AN. We have already shown that bodies are judged in a categorical manner (Tovée et al., 2012) and the first step in testing this training was to determine whether it could shift the categorical boundary in thin–fat judgements of bodies varying in BMI. In Study 1, we recruited young women with high body size concerns (but without a formal diagnosis of AN) to test whether their thin–fat categorical boundary could be altered. The results showed a significant shift in the categorical boundary in the intervention group relative to the controls, and this shift was retained 2 weeks after the training. The EDE‐Q scores (a general measure of eating‐disordered concerns which is often used as a screening questionnaire) showed a significant reduction in the intervention condition relative to controls, and this reduction persisted 2 weeks after the end of training.
In Study 2, we recruited a cohort of women with aAN. These women have long‐standing problems with body image and eating‐disordered behaviour and thus potentially might be more resistant to the training altering their thin–fat categorical boundary and therefore any associated improvement in body and eating‐disordered concerns. The follow‐up period was also extended from 2 weeks to a month to test retention of the training. This second study did not have a control group, but we compensated for this using a Digit Span task as a control task. As this task is unrelated to body image and eating disorders and should be unaffected by the body training, it can act as a proxy for any habituation/practice effects caused by repeating the questionnaire measures. As in Study 1, there was a significant shift in the categorical boundary during training that was retained a month later. There was also a significant change in the EDE‐Q scores over the course of training and which was also retained a month later. These changes were still statistically significant even when variance in the Digit Span task was taken into account. What is important here is not that women with aAN can be trained to alter the categorical boundary at which they classify a body to be ‘fat’, but that this change is retained and seems to generalize to other aspects of their body image and eating‐disordered concerns. The degree to which the categorical boundary shifts is significantly correlated with the change in the EDE‐Q score, which is consistent with a causal relationship between the boundary change and the psychological scores. This relationship is true for all the subscales, not just those related to body size or shape. This suggests an effect of the training beyond simply changing the participants’ judgements of body size, but has a more global effect on body and eating concerns. It also provides support for the hypothesis that biases in the perception of body size play a causal role in the maintenance of body image concerns and eating‐disordered behaviour. One interpretation of these results is that this modification establishes a virtuous cycle, whereby the change in perception of body size may lead to changes in behaviour that are then reciprocated and reinforced.
Three of the women with AN recruited into Study 2 did not complete the training. This may represent resistance to treatment that might change their body perception (an interpretation consistent with the lack of statistical significance of the intention to treat analysis if these women are included). Alternatively, it is possible that the requirement to attend the training on four consecutive days may have proved too difficult.
A key question is whether the reductions that we observed in psychological concerns over a month in the aAN participants are clinically meaningful. With respect to EDE‐Q, Bardone‐Cone et al. (2010) operationalize recovery in eating‐disordered patients as a reduction in all four subscale scores to within 1 SD of age‐matched community norms. Mond et al. (2006) report such norms for the age group 23–27 years based on a sample of 908 women: EDE‐Q M = 1.56, SD = 1.26; EDE‐restraint M = 1.34, SD = 1.39; EDE‐eating concerns M = 0.81, SD = 1.10; EDE‐shape concerns M = 1.84, SD = 1.50; EDE‐weight concerns M = 2.24, SD = 1.61. The mean EDE‐Q and subscale scores from our aAN sample (mean age 26.8 years) at Day 30 were, respectively, as follows: EDE‐Q M = 2.63; EDE‐restraint M = 2.45; EDE‐eating concerns M = 2.06; EDE‐shape concerns M = 2.83; EDE‐weight concerns M = 3.18. Therefore, with the exception of EDE‐eating concerns, which missed the criterion by only 0.15 units, the perceptual training regime reported here produced reductions in EDE‐Q scores that were clinically meaningful, when defined in this way.
Although the statistical results of these two exploratory studies should be treated with caution with respect to clinical outcomes due to low power, they indicate robust perceptual effects that suggest an exciting new way of treating biases in the judgement of female body size that are characteristic of AN, and provide evidence that perceptual biases play a causal role in AN as has been suggested for some other disorders (e.g., depression, Harmer, Goodwin, & Cowen, 2009). As such, perceptual training has the potential to be a valuable cost‐effective adjunctive treatment for AN used together with more traditional talking therapies (cognitive behavioural therapy, mindfulness etc.). The training programme could be given at six monthly intervals to reinforce these benefits, as our research has suggested that body image concerns increase as BMI increases during treatment which potentially could undermine recovery (Cornelissen et al., 2015). This ‘top‐up’ training could be accomplished by adapting the body training for use through a mobile‐friendly website to run on a patient's PC, laptop, tablet or smartphone, or through a downloadable app. Additionally, this programme could be used in non‐clinical groups. Body dissatisfaction is widespread amongst girls and young women in Western countries, where around 50% report being dissatisfied with their bodies and this dissatisfaction is a key predictor of the development of low self‐esteem, depression, and eating disorders (e.g., Bearman, Presnell, & Martinez, 2006; Monteath & McCabe, 1997). A downloadable form of the training could be used to improve body image judgements in this general population. However, a limitation of the current studies for clinical use is that the training has only be tested on a single cohort of women with aAN. A larger scale randomized control trial is needed to properly test its feasibility and effectiveness in a clinical environment.
Conflict of interest
I. S. P.‐V. and M. R. M. are directors of Jericoe Ltd., which develops software for assessing and modifying emotion perception. The other authors declared that they had no conflict of interests with respect to their authorship or the publication of this article.
References
- Adams, S. , Penton‐Voak, I. S. , Harmer, C. J. , Holmes, E. A. , & Munafò, M. R. (2013). Effects of emotion recognition training on mood among individuals with high levels of depressive symptoms: Study protocol for a randomized controlled trial. Trials, 14, 161. doi:10.1186/1745‐6215‐14‐161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alleva, J. M. , Sheeran, P. , Webb, T. L. , Martijn, C. , & Miles, E. (2015). A meta‐analytic review of stand‐alone interventions to improve body image. PLoS One, 10, e0139177. doi:10.1371/journal.pone.0139177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Bardone‐Cone, A. M. , Harney, M. B. , Maldonado, C. R. , Lawson, M. A. , Robinson, D. P. , Smith, R. , & Tosh, A. (2010). Defining recovery from an eating disorder: Conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behaviour Research and Therapy, 48, 194–202. doi:10.1016/j.brat.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bearman, S. K. , Presnell, K. , & Martinez, E. (2006). The skinny on body dissatisfaction: A longitudinal study of adolescent girls and boys. Journal of Adolescence, 35, 217–229. doi:10.1007/s10964‐005‐9010‐9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. , Ward, C. H. , Mendelson, M. , Mock, J. , & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571.doi:10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- Berkman, N. D. , Lohr, K. N. , & Bulik, C. M. (2007). Outcomes of eating disorders: A systematic review of the literature. International Journal of Eating Disorders, 40, 293–309. doi:10.1002/eat.20369 [DOI] [PubMed] [Google Scholar]
- Carter, J. C. , Mercer‐Lynn, K. B. , Norwood, S. J. , Bewell‐Weiss, C. V. , Crosby, R. D. , Woodside, D. B. , & Olmsted, M. P. (2012). A prospective study of predictors of relapse in anorexia nervosa: Implications for relapse prevention. Psychiatry Research, 200, 518–523. doi:10.1016/j.psychres.2012.04.037 [DOI] [PubMed] [Google Scholar]
- Cash, T. F. , & Deagle, E. A. (1997). The nature and extent of body‐image disturbances in anorexia nervosa and bulimia nervosa: A meta‐analysis. International Journal of Eating Disorders, 22, 107–126. doi:10.1002/(SICI)1098‐108X(199709)22:2<107 [PubMed] [Google Scholar]
- Channon, S. , & DeSilva, W. (1985). Psychological correlates of weight gain in patients with anorexia nervosa. Journal of Psychiatric Research, 19, 267–271. doi:10.1016/0022‐3956(85)90027‐5 [DOI] [PubMed] [Google Scholar]
- Cornelissen, K. K. , Bester, A. , Cairns, P. , Tovée, M. J. , & Cornelissen, P. L. (2015). The influence of personal BMI on body size estimations and sensitivity to body size change in anorexia spectrum disorders. Body Image, 13, 75–85. doi:10.1016/j.bodyim.2015.01.001 [DOI] [PubMed] [Google Scholar]
- Cornelissen, K. K. , Gledhill, L. , Cornelissen, P. L. , & Tovée, M. J. (2016). Visual biases in judging body weight. British Journal of Health Psychology, 21, 555–569. doi:10.1111/bjhp.12185 [DOI] [PubMed] [Google Scholar]
- Cornelissen, P. L. , Johns, A. , & Tovée, M. J. (2013). Body size over‐estimation in women with anorexia nervosa is not qualitatively different from female controls. Body Image, 10, 103–111. doi:10.1016/j.bodyim.2012.09.003 [DOI] [PubMed] [Google Scholar]
- Delinsky, S. S. , & Wilson, G. T. (2006). Mirror exposure for the treatment of body image disturbance. International Journal of Eating Disorders, 39, 108–116. doi:10.1002/eat.20207 [DOI] [PubMed] [Google Scholar]
- Evans, C. , & Dolan, B. (1993). Body Shape Questionnaire: Derivation of shortened “alternate forms”. International Journal of Eating Disorders, 13, 315–321. doi:10.1002/1098‐108X(199304)13:3<315::AID‐EAT2260130310>3.0.CO;2‐3 [DOI] [PubMed] [Google Scholar]
- Fairburn, C. G. , & Beglin, S. J. (1994). Assessment of eating disorders: Inter‐view or self‐report questionnaire? International Journal of Eating Disorders, 16, 363–370. doi:10.1002/1098‐108X(199412)16:4<363::AID‐EAT2260160405>3.0.CO;2 [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41, 509–528. doi:10.1016/S0005‐7967(02)00088‐8 [DOI] [PubMed] [Google Scholar]
- Farrell, C. , Shafran, R. , & Lee, M. (2006). Empirically evaluated treatments for body image disturbance: A review. European Eating Disorders Review, 14, 289–300. doi:10.1002/erv.693 [Google Scholar]
- Gardner, R. M. , Jones, L. C. , & Bokenkamp, E. D. (1996). Comparison of three psychophysical techniques for estimating body‐size perception. Perceptual and Motor Skills, 80, 1379–1390. doi:10.2466/pms.1995.80.3c.1379 [DOI] [PubMed] [Google Scholar]
- George, H. R. , Cornelissen, P. L. , Hancock, P. J. , Kiviniemi, V. V. , & Tovée, M. J. (2011). Differences in eye‐movement patterns between anorexic and control observers when judging body size and attractiveness. British Journal of Psychology, 102, 340–354. doi:10.1348/000712610X52429 [DOI] [PubMed] [Google Scholar]
- Ginis, K. A. M. , & Bassett, R. L. (2011). Exercise and changes in body image In Cash T. F. & Smolak L. (Eds.), Body image: A handbook of science, practice, and prevention (pp. 415–423). New York, NY: Guilford Press. [Google Scholar]
- Grabe, S. , Ward, L. M. , & Hyde, J. S. (2008). The role of the media in body image concerns among women: A meta‐analysis of experimental and correlational studies. Psychological Bulletin, 134, 460–476. doi:10.1037/0033‐2909.134.3.460 [DOI] [PubMed] [Google Scholar]
- Harmer, C. J. , Goodwin, G. M. , & Cowen, P. J. (2009). Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. The British Journal of Psychiatry, 195, 102–108. doi:10.1192/bjp.bp.108.051193 [DOI] [PubMed] [Google Scholar]
- Irving, L. M. , & Berel, S. R. (2001). Comparison of media‐literacy programs to strengthen collage women's resistance to media images. Psychology of Women Quarterly, 25, 103–111. doi:10.1111/1471‐6402.00012 [Google Scholar]
- Jarry, J. L. , & Cash, T. F. (2011). Cognitive‐behavioral approaches to body image change In Cash T. F. & Smolak L. (Eds.), Body image: A handbook of science, practice, and prevention (pp. 415–423). New York, NY: Guilford Press. [Google Scholar]
- Key, A. , George, C. L. , Beattie, D. , Stammers, K. , Lacey, H. , & Glenn Waller, G. (2002). Body image treatment within an inpatient program for anorexia nervosa: The role of mirror exposure in the desensitization process. International Journal of Eating Disorders, 31, 185–190. doi:10.1002/eat.10027 [DOI] [PubMed] [Google Scholar]
- Luce, K. H. , Crowther, J. H. , & Pole, M. (2008). Eating disorder examination questionnaire (EDE‐Q): Norms for undergraduate women. International Journal of Eating Disordorders, 41(3), 273‐276. doi:10.1002/eat.20504 [DOI] [PubMed] [Google Scholar]
- Martin, K. A. , & Lichtenberger, C. M. (2002). Fitness enhancement and changes in body image In Cash T. F. & Pruzinksy T. (Eds.), A handbook of theory, research, and clinical practice (pp. 414–421). New York, NY: The Guilford Press. [Google Scholar]
- Mond, J. M. , Hay, P. J. , Rodgers, B. , & Owen, C. (2006). Eating Disorder Examination Questionnaire (EDE‐Q): Norms for young adult women. Behavior Research and Therapy, 44, 53–62. doi:10.1016/j.brat.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Monteath, S. A. , & McCabe, M. P. (1997). The influence of societal factors on the female body image. Journal of Social Psychology, 137, 708–727. doi:10.1080/00224549709595493 [DOI] [PubMed] [Google Scholar]
- O'Dea, J. (2004). Evidence for a self‐esteem approach in the prevention of body image and eating problems among children and adolescents. Eating Disorders, 12, 225–239. doi:10.1093/heapro/dan004 [DOI] [PubMed] [Google Scholar]
- O'Dea, J. A. , & Yager, Z. (2011). School‐based psychoeducational approaches to prevention In Cash T. F. & Smolak L. (Eds.), Body image: A handbook of science, practice, and prevention (2nd ed., pp. 434–441). New York, NY: Guilford. [Google Scholar]
- Penton‐Voak, I. S. , Bate, H. , Lewis, G. , & Munafò, M. R. (2012). Effects of emotion perception training on mood in undergraduate students: Randomised controlled trial. British Journal of Psychiatry, 201, 71–72. doi:10.1192/bjp.bp.111.107086 [DOI] [PubMed] [Google Scholar]
- Penton‐Voak, I. S. , Thomas, J. , Gage, S. H. , McMurran, M. , McDonald, S. , & Munafò, M. R. (2013). Increasing recognition of happiness in ambiguous facial expressions reduces anger and aggressive behavior. Psychological Science, 24, 688–697. doi:10.1177/0956797612459657 [DOI] [PubMed] [Google Scholar]
- Probst, M. , Vandereycken, W. , Vanderlinden, J. , & Van Coppenolle, H. (1998). The significance of body size estimation in eating disorders: Its relationship with clinical and psychological variables. International Journal of Eating Disorders, 24, 167–174. doi:10.1002/(SICI)1098‐108X(199809)24:2<167::AID‐EAT6>3.0.CO;2‐C [DOI] [PubMed] [Google Scholar]
- Rosenberg, M. (1965). Society and the adolescent self‐image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Tovée, M. J. , Benson, P. J. , Emery, J. L. , Mason, S. M. , & Cohen‐Tovée, E. M. (2003). Measurement of body size and shape perception in eating‐disordered and control observers using body‐shape software. British Journal of Psychology, 94, 501–516. doi:10.1348/000712603322503060 [DOI] [PubMed] [Google Scholar]
- Tovée, M. J. , Edmonds, L. , & Vuong, Q. C. (2012). Categorical perception of human female physical attractiveness and health. Evolution & Human Behavior, 33, 85–93. doi:10.1016/j.evolhumbehav.2011.05.008 [Google Scholar]
- Tovée, M. J. , Emery, J. L. , & Cohen‐Tovée, E. M. (2000). The estimation of body mass index and physical attractiveness is dependent on the observer's own body mass index. Proceedings of the Royal Society B: Biological Sciences, 267, 1987–1997. doi:10.1098/rspb.2000.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treasure, J. , Claudino, A. M. , & Zucker, N. (2010). Eating disorders. Lancet, 375, 583–593. doi:10.1016/S0140‐6736(09)61748‐7 [DOI] [PubMed] [Google Scholar]
- Vocks, S. , Wachter, A. , Wucherer, M. , & Kosfelder, J. (2008). Look at yourself: Can body image therapy affect the cognitive and emotional response to seeing oneself in the mirror in eating disorders? European Eating Disorders Review, 16, 147–154. doi:10.1002/erv.825 [DOI] [PubMed] [Google Scholar]
- Wechsler, D. (1981). Manual for the Wechsler adult intelligence scale—F6revised. New York: Psychological Corporation. [Google Scholar]
- Williamson, D. A. , Cubic, B. A. , & Gleaves, D. H. (1993). Equivalence of body image disturbances in anorexia and bulimia nervosa. Journal of Abnormal Psychology, 102, 177–180. doi:10.1037/0021‐843X.102.1.177 [PubMed] [Google Scholar]


