Abstract
Alcohol use is a risk factor for severe injury in pedestrians struck by motor vehicles. Our objective was to investigate alcohol use by bicyclists and its effects on riding behaviors, medical management, injury severity, and mortality within a congested urban setting. A hospital-based, observational study of injured bicyclists presenting to a Level I regional trauma center in New York City was conducted. Data were collected prospectively from 2012 to 2014 by interviewing all bicyclists presenting within 24 h of injury and supplemented with medical record review. Variables included demographic characteristics, scene-related data, Glasgow Coma Scale (GCS), computed tomography (CT) scans, and clinical outcomes. Alcohol use at the time of injury was determined by history or blood alcohol level (BAL) >0.01 g/dL. Of 689 bicyclists, 585 (84.9%) were male with a mean age of 35.2. One hundred four (15.1%) bicyclists had consumed alcohol prior to injury. Alcohol use was inversely associated with helmet use (16.5% [9.9–25.1] vs. 43.2% [39.1–47.3]). Alcohol-consuming bicyclists were more likely to fall from their bicycles (42.0% [32.2–52.3] vs. 24.2% [20.8–27.9]) and less likely to be injured by collision with a motor vehicle (52.0% [41.7–62.1] vs. 67.5% [63.5–71.3]). 80% of alcohol-consuming bicyclists underwent CT imaging at presentation compared with 51.5% of non-users. Mortality was higher among injured bicyclists who had used alcohol (2.9% [0.6–8.2] vs. 0.0% [0.0–0.6]). Adjusted multivariable analysis revealed that alcohol use was independently associated with more severe injury (Adjusted Odds Ratio 2.27, p = 0.001, 95% Confidence Interval 1.40–3.68). Within a dense urban environment, alcohol use by bicyclists was associated with more severe injury, greater hospital resource use, and higher mortality. As bicycling continues to increase in popularity internationally, it is important to heighten awareness about the risks and consequences of bicycling while under the influence of alcohol.
Keywords: bicycle injury, bicycle trauma, traffic safety, alcohol
Introduction
A staggering number of traffic fatalities have been linked to alcohol; of the 858,741 traffic fatalities from 1982–2001 in the United States (US), 43% were associated with alcohol use [1]. Alcohol is a well-recognized risk factor for traffic collisions because it can impair judgment and cognitive function [2]. Driving a motor vehicle while intoxicated leads to a significantly increased risk of severe injury and mortality and legislation has been passed to combat the problem of driving under the influence [2, 3]. Urban pedestrians who use alcohol have also been shown to demonstrate risky behaviors which put them at risk for injury by motor vehicles [3]. The use and sequelae of alcohol by bicyclists in these settings are less clear.
In the last decade, bicycling has increased substantially in popularity in many cities worldwide. With the recent implementation of the largest bicycle sharing program in the US, New York City (NYC) is representative of this trend. In NYC, there are no laws prohibiting bicycling under the influence, even though the proportion of bicycle injuries related to alcohol intoxication has been increasing [4]. Although the body of literature on alcohol-linked bicycle injuries is limited, alcohol consumption among cyclists has been shown to increase the risk of an injury or fatal crash [5–7]. The association between alcohol intoxication and bicycle-related injury has been studied [2, 8–10], yet precise information about mechanisms of injury, injury severity, medical management, and detailed outcomes is sparse. Moreover, the design of previous studies has been inconsistent and the sample size of published reports often small.
The objective of this study was to investigate alcohol use by bicyclists and its role in bicyclist injuries, including its effects on riding behaviors, medical management, injury severity, and mortality within a congested urban setting. Despite the lower speeds inherent in a high population urban center, we hypothesize that alcohol use by urban bicyclists is independently associated with greater injury severity and worse outcomes.
Methods
An observational study of injured bicyclists presenting to Bellevue Hospital Center (BHC) – a Level I regional trauma center – was performed. Data were collected in a prospective fashion between February 1, 2012 and August 31, 2014, excluding a 14-week interruption (between October 29, 2012 and February 7, 2013) when clinical services were disrupted as a result of Superstorm Sandy. BHC’s catchment area includes midtown and lower Manhattan and western Brooklyn and its emergency department (ED) evaluates over 100,000 patients annually.
Bicyclists who presented to the BHC ED within 24 hours of injury were approached for enrollment in the study. Children under 13 years of age were excluded from analysis.
Demographic and incident-related data were elicited primarily from the patients (i.e. self-report) and supplemented by first responders as available. Data collection was performed by a dedicated study coordinator, attending trauma surgeons, emergency medicine physicians, physician assistants, and the trauma program coordinator. Patients were interviewed only when they were able to give informed verbal consent. Pre-hospital care reports were reviewed if available.
Data collection involved over one hundred distinct variables. Alcohol use at the time of injury was determined on a case-by-case basis by history or blood alcohol level (BAL). BALs were obtained as part of a routine work-up in many cases including those where triage criteria warranted a trauma team activation. A BAL of >0.01 g/dL was considered positive and an indication of use prior to the incident. If laboratory data were not available, self-reported history of alcohol use in the moments prior to the incident was assessed for.
Outcomes variables included Glasgow Coma Scale (GCS) score, initial computed tomography (CT) imaging studies, Abbreviated Injury Scale (AIS) score, Injury Severity Score (ISS), admission status, hospital length of stay (LOS), procedures (e.g. surgeries, intubations), disposition, and mortality. AIS and ISS were calculated for each patient after attending radiology evaluations were finalized.
Data were analyzed using STATA version 13.0 statistical software. Means and proportions with 95% Confidence Intervals (CIs) were reported for continuous and categorical data and stratified by alcohol use. Any missing data points were specified for the relevant variables as footnotes in the tables. Hospital-based variables (e.g. AIS score, procedures performed, imaging results) had no missing data. We used multivariable ordinal logistic regression to model the effect of alcohol use on injury severity, as defined by a five-category injury severity score, while controlling for other variables. Results of the multivariable logistic regression are represented by adjusted odds ratios (AOR) and 95% CIs. Additionally, the multivariable model employed multiple imputations to account for missing data using the method of chained equations.
Both the New York University School of Medicine and the BHC institutional review boards approved the studies. Funding was provided by a Highway Safety Grant from the State of New York Governor’s Traffic Safety Committee.
Results
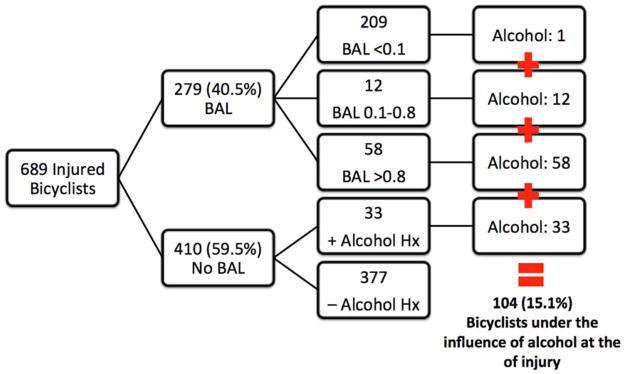
689 bicyclists met inclusion criteria. 585 (84.9%) were male with a mean age of 35.2 years [range:13–82]. Of the 689 patients in this study, BALs were drawn on 279 patients (40.5%.) BAL was positive (>0.1) in seventy patients, who were marked as having used alcohol at the time of injury. Four hundred ten patients (59.5%) did not have BALs drawn; based on a recent history of alcohol use provided by the patient, 33 additional bicyclists were included in the alcohol group [figure 1]. One patient who had a normal BAL on arrival to BHC had been transferred from another hospital with documented alcohol use prior to the crash. In total, 104 (15.1%) bicyclists were under the influence of alcohol at the time of injury, while 585 (84.9%) bicyclists were not.
Figure 1.
Alcohol use by NYC bicyclists based on blood alcohol levels and history of recent consumption
BAL, blood alcohol level; Hx, history
Demographic Characteristics
Bicyclists’ demographic characteristics stratified by alcohol use are listed in Table 1. There were no statistically significant differences in gender or ethnicity between the alcohol use and no alcohol use groups.
TABLE 1.
Demographic characteristics of injured bicyclists based on alcohol use
| No Alcohol Use n=585 |
Alcohol Use n=104 |
|||
|---|---|---|---|---|
|
| ||||
| % (n) | 95% CI | % (n) | 95% CI | |
|
| ||||
| Gender | ||||
| Male | 79.7 (466) | 76.2,82.9 | 81.7 (85) | 73.0,88.6 |
| Female | 20.3 (119) | 17.2,23.8 | 18.3 (19) | 11.4,27.1 |
|
| ||||
| Age | ||||
| 13–17 years | 3.9 (23) | 2.5,5.8 | 0.0 (0) | 0.0,3.5 |
| 18–54 years | 85.0 (497) | 81.8,87.8 | 94.2 (98) | 87.9,97.9 |
| ≥55 years | 11.1 (65) | 8.7,13.9 | 5.8 (6) | 2.2,12.1 |
|
| ||||
| Ethnicitya | ||||
| White (non-Latino) | 45.6 (267) | 41.6,49.8 | 50.0 (52) | 40.0,60.0 |
| Black | 7.7 (45) | 5.7,10.2 | 8.7 (9) | 4.0,15.8 |
| Latino | 29.1 (170) | 25.4,32.9 | 32.7 (34) | 23.8, 42.6 |
| East Asian | 11.5 (67) | 9.0,14.3 | 5.8 (6) | 2.2,12.1 |
| South Asian | 2.2 (13) | 1.2, 3.8 | 0.0 (0) | 0.0,3.5 |
| Other | 3.4 (20) | 2.1, 5.2 | 2.9 (3) | 0.6,8.2 |
CI calculated using exact binomial method.
Three unknowns excluded
CI (confidence interval)
Riding Behaviors and Mechanisms of Injury
Bicyclists’ behaviors and mechanisms of injury are detailed in table 2. Bicyclists who used alcohol were more likely to be riding for leisure (65.6% [55.0,75.1] vs. 42.0% [37.9–46.3]), and less likely to be working (4.1% [1.1–10.2] vs. 23.9% [20.5–27.6]). Alcohol use was inversely associated with wearing a helmet (16.5% [9.9–25.1] vs. 43.2% [39.1–47.3]). Alcohol-consuming bicyclists were more likely to fall from their bicycles (42.0% [32.2–52.3] vs. 24.2% [20.8–27.9]) and less likely to be injured from collisions with motor vehicles (52.0% [41.7–62.1] vs. 67.5% [63.5–71.3]). Alcohol-consuming bicyclists were also less likely to be hit by a car door (2.1% [0.2–7.5] vs. 13.2% [10.5–16.3]). There were no significant differences in other riding behaviors, including riding with or against traffic, riding in a bike lane or path, or crossing against the signal or stop sign.
TABLE 2.
Behaviors, mechanisms of injury, and scene-related variables of injured bicyclists based on alcohol use
| No Alcohol Use n=585 |
Alcohol Use n=104 |
|||
|---|---|---|---|---|
|
| ||||
| % (n) | 95% CI | % (n) | 95% CI | |
|
| ||||
| Bicyclist Behaviors | ||||
|
| ||||
| Commutinga | 33.6 (188) | 29.7,37.7 | 30.1 (28) | 21.0,40.5 |
|
| ||||
| Leisurea | 42.0 (235) | 37.9,46.3 | 65.6 (61) | 55.0,75.1 |
|
| ||||
| Commercialb | 23.9 (136) | 20.5,27.6 | 4.1 (4) | 1.1,10.2 |
|
| ||||
| Bicycle sharec | 8.8 (28) | 5.9,12.5 | 7.8 (5) | 2.9,17.3 |
|
| ||||
| Helmet used | 43.2 (250) | 39.1,47.3 | 16.5 (17) | 9.9,25.1 |
|
| ||||
| Use of distracting devicee | 11.3 (64) | 8.8,14.2 | 12.1 (11) | 6.2,20.6 |
|
| ||||
| Mechanism of Injury | ||||
|
| ||||
| Mechanismf | ||||
| Versus pedestrian or bicyclist | 8.3 (48) | 6.2,10.9 | 6.0 (6) | 2.2,12.6 |
| Versus motor vehicle | 67.5 (390) | 63.5,71.3 | 52.0 (52) | 41.8,62.1 |
| Fall from bicycle | 24.2 (140) | 20.8,27.9 | 42.0 (42) | 32.2,52.3 |
|
| ||||
| Riding against trafficg | 7.7 (41) | 5.6,10.4 | 10.5 (7) | 4.3,20.4 |
|
| ||||
| Riding in bike lane or pathh | 42.2 (219) | 37.9,46.6 | 44.2 (34) | 32.8,55.9 |
|
| ||||
| Cyclist crossed against signali | 8.2 (44) | 6.0,10.8 | 11.0 (9) | 5.1,19.8 |
|
| ||||
| Cyclist crossed against stop signj | 0.9 (5) | 0.3,2.1 | 0.0 (0) | 0.0,4.0 |
|
| ||||
| Striking vehicle doork | 13.2 (74) | 10.5,16.3 | 2.1 (2) | 0.2,7.5 |
|
| ||||
| Cyclists speedl | ||||
| <5mph | 18.8 (95) | 15.5,22.5 | 18.8 (13) | 10.4,30.1 |
| 5–15mph | 68.3 (345) | 64.1,72.4 | 68.1 (47) | 55.8,78.8 |
| >15mph | 12.9 (65) | 10.1,16.1 | 13.0 (9) | 6.1,23.3 |
|
| ||||
| Scene Data | ||||
|
| ||||
| Boroughm | ||||
| Manhattan | 85.3 (494) | 82.2,88.1 | 69.1 (67) | 58.9,78.1 |
| Queens | 1.2 (7) | 0.5,2.5 | 1.0 (1) | 0.0,5.6 |
| Brooklyn | 13.1 (76) | 10.5,16.2 | 28.9 (28) | 20.1,39.0 |
| Bronx | 0.4 (2) | 0.0,1.2 | 0.0 (0) | 0.0, 3.7 |
| Other | 0.0 (0) | 0.0,0.6 | 1.0 (1) | 0.0,5.6 |
|
| ||||
| Road surfacen | ||||
| Normal | 90.0 (513) | 87.2,92.3 | 92.8 (90) | 85.7,97.1 |
| Icy or wet | 10.0 (57) | 7.7,12.8 | 7.2 (7) | 3.0,14.3 |
|
| ||||
| Time of dayo | ||||
| 12am to 2:59am | 2.4 (13) | 1.3,4.0 | 19.0 (18) | 11.6,28.3 |
| 3am to 5:59am | 2.6 (14) | 1.4,4.3 | 14.7 (14) | 8.3,23.5 |
| 6am to 8:59am | 10.1 (55) | 7.7,12.9 | 3.2 (3) | 0.6,9.0 |
| 9am to 11:59am | 21.3 (116) | 17.9,24.9 | 6.3 (6) | 2.4,13.2 |
| 12pm to 2:59pm | 20.0 (109) | 16.7,23.6 | 4.2 (4) | 1.2,10.4 |
| 3pm to 5:59pm | 16.3 (89) | 13.3,19.7 | 12.6 (12) | 6.7,21.0 |
| 6pm to 8:59pm | 17.8 (97) | 14.7,21.2 | 21.1 (20) | 13.4,30.6 |
| 9pm to 11:59pm | 9.7 (53) | 7.4,12.5 | 19.0 (18) | 11.6,28.3 |
|
| ||||
| Day of week | ||||
| Sunday | 8.9 (52) | 6.7,11.5 | 13.5 (14) | 7.6,21.6 |
| Monday | 17.1 (100) | 14.1,20.4 | 10.6 (11) | 5.4,18.1 |
| Tuesday | 11.5 (67) | 9.0,14.3 | 8.7 (9) | 4.0,15.8 |
| Wednesday | 16.8 (98) | 13.8,20.0 | 14.4 (15) | 8.3,22.7 |
| Thursday | 18.6 (109) | 15.6,22.0 | 11.5 (12) | 6.1,19.3 |
| Friday | 15.2 (89) | 12.4,18.4 | 21.2 (22) | 13.8,30.3 |
| Saturday | 12.0 (70) | 9.5,14.9 | 20.2 (21) | 13.0,29.2 |
CI calculated using exact binomial method.
‘Commuting’ cyclists include those going to or returning from work. ‘Leisure’ cyclists are those bicycling for pleasure, sport, or navigating the city.
Thirty-seven unknowns excluded
Twenty-three unknowns excluded
Denominator n=382, representing bicyclists after the initiation of Citibike in May, 2015
Seven unknowns excluded
Twelve unknowns excluded
Eleven unknowns excluded
Eighty-three unknowns excluded
Eighty-one unknowns excluded
Seventy unknowns excluded
Forty-nine unknowns excluded
Thirty-three unknowns excluded
One-hundred fifteen unknowns excluded
Thirteen unknowns excluded
Twenty-two unknowns excluded
Forty-eight unknowns excluded
A higher proportion of alcohol-consuming cyclists were injured in the borough of Brooklyn (28.9% [20.1–39.0] vs. 13.1% [10.5–16.2] and a lower proportion injured in Manhattan (69.1% [58.9–78.1] vs. 85.3% [82.2–88.1]). Intoxicated bicyclists were more likely to be injured from the hours of 12am to 6am, and less likely to be injured during the daylight hours of 9am to 3pm (Table 2). Injuries sustained during morning or evening rush hours did not differ between groups. There were no differences between groups with respect to day of the week or road surface conditions.
Injuries and outcomes and radiologic imaging
Table 3 details the overall outcomes of injured bicyclists stratified by alcohol use. Bicyclists who used alcohol prior to injury had higher rates of LOC (66.3% [55.3–76.1] vs. 30.4% [26.5–34.4]). Initial GCS scores indicative of coma and concerning for severe traumatic brain injury (i.e. GCS <9) were more common among intoxicated bicyclists (7.0% [2.9–13.9] vs. 1.1% [0.4–2.3]). Bicyclists who used alcohol prior to the crash were less likely to sustain no injury (1.9% [0.2–6.8] vs. 9.1% [6.9–11.7]) and more likely to sustain critical injuries (i.e. ISS≥25) (8.7% [4.0–15.8] vs. 2.1% [1.1–3.6]). Alcohol use was associated with more severe head and cervical spine (20.2% [13.0–29.2] vs. 7.7% [5.7–10.2]), face (32.7% [23.8–42.6] vs. 11.5% [9.0–14.3]), abdomen (2.1% [1.1–3.6] vs. 8.7% [4.0–15.8]), and external injuries (95.2% [89.1–98.4] vs. 86.0% [82.9–88.7]). There was no difference in extremity injures between the groups (26.0% [17.9–35.5] vs. 26.7% [23.1–30.5]).
TABLE 3.
Injuries, diagnostic and therapeutic interventions, and outcomes of injured bicyclists based on alcohol use
| No Alcohol Use n=585 |
Alcohol Use n=104 |
|||
|---|---|---|---|---|
|
| ||||
| % (n) | 95% CI | % (n) | 95% CI | |
|
| ||||
| Injuries | ||||
|
| ||||
| LOC1 | 30.4 (165) | 26.5,34.4 | 66.3 (57) | 55.3,76.1 |
|
| ||||
| GCS2 | ||||
| GCS=15 | 93.3 (532) | 91.0,95.2 | 74.0 (74) | 64.3,82.3 |
| GCS=13–14 | 5.4 (31) | 3.7,7.6 | 17.0 (17) | 10.2,25.8 |
| GCS=9–12 | 0.2 (1) | 0.0,1.0 | 2.0 (2) | 0.2,7.0 |
| GCS=<9 | 1.1 (6) | 0.4,2.3 | 7.0 (7) | 2.9,13.9 |
|
| ||||
| ISS | ||||
| No Injury, ISS=0 | 9.1 (53) | 6.9,11.7 | 1.9 (2) | 0.2,6.8 |
| Mild, ISS=1–8 | 71.5 (418) | 67.6,75.1 | 67.3 (70) | 57.4,76.2 |
| Moderate, ISS=9–15 | 14.7 (86) | 11.9,17.8 | 15.4 (16) | 9.1,23.8 |
| Severe, ISS=16–24 | 2.7 (16) | 1.6,4.4 | 6.7 (7) | 2.8,13.4 |
| Critical, ISS≥25 | 2.1 (12) | 1.1,3.6 | 8.7 (9) | 4.0,15.8 |
|
| ||||
| Head and Neck AIS≥1 | 7.7 (45) | 5.7,10.2 | 20.2 (21) | 13.0,29.2 |
|
| ||||
| Face AIS≥1 | 11.5 (67) | 9.0,14.3 | 32.7 (34) | 23.8,42.6 |
|
| ||||
| Chest AIS≥1 | 2.9 (17) | 1.7,4.6 | 6.7 (7) | 2.8,13.4 |
|
| ||||
| Abdomen AIS≥1 | 2.1 (12) | 1.1,3.6 | 8.7 (9) | 4.0,15.8 |
|
| ||||
| Extremity AIS≥1 | 26.7 (156) | 23.1,30.5 | 26.0 (27) | 17.9,35.5 |
|
| ||||
| External AIS≥1 | 86.0 (503) | 82.9,88.7 | 95.2 (99) | 89.1,98.4 |
|
| ||||
| Initial CT Imaging | ||||
|
| ||||
| Any CT Scan Performed | 51.5 (301) | 47.3,55.6 | 79.8 (83) | 70.8,87.0 |
|
| ||||
| CT Head Performed | 44.1 (258) | 40.0,48.2 | 76.9 (80) | 67.6,84.6 |
|
| ||||
| CT Cervical Spine Performed | 40.0 (234) | 36.0,44.1 | 68.3 (71) | 58.4,77.1 |
|
| ||||
| CT Chest Performed | 11.8 (69) | 9.3,14.7 | 33.7 (35) | 24.7,43.6 |
|
| ||||
| CT Abdomen/Pelvis Performed | 14.2 (83) | 11.5,17.3 | 38.5 (40) | 29.1,48.5 |
|
| ||||
| Injury on Head CT | 13.5 (35) | 9.6,18.2 | 20.5 (16) | 12.2,31.2 |
|
| ||||
| Interventions | ||||
|
| ||||
| Required intubation | 1.7 (10) | 0.8,3.1 | 7.7 (8) | 3.4,14.6 |
|
| ||||
| Required Surgery | 8.7 (51) | 6.6,11.3 | 17.3 (18) | 10.6,26.0 |
|
| ||||
| Required Tracheostomy | 0.9 (5) | 0.3,2.0 | 2.9 (3) | 0.6,8.2 |
|
| ||||
| Required ICP Monitor | 1.5 (4) | 0.4,3.9 | 6.4 (5) | 2.1,14.3 |
|
| ||||
| Required Craniotomy | 1.2 (3) | 0.2,3.3 | 1.3 (1) | 0.0,7.0 |
|
| ||||
| Hospital Course | ||||
|
| ||||
| Hospital Admission3 | 23.3 (136) | 19.9,26.9 | 50.0 (52) | 40.0,60.0 |
|
| ||||
| Required ICU Admission | 13.3 (78) | 10.7,16.4 | 30.1 (32) | 22.1,40.6 |
|
| ||||
| LOS of Admission (days) | ||||
| Mean (SD) | 1.2 (4.7) | 0.8,1.5 | 2.6 (6.8) | 1.3,3.9 |
|
| ||||
| Disposition | ||||
| Home | 96.2 (563) | 94.4,97.6 | 90.4 (94) | 83.0,95.3 |
| Rehab Facility | 3.3 (19) | 2.0,5.0 | 4.8 (5) | 1.6,10.9 |
| Other | 0.5 (3) | 0.1,1.5 | 4.8 (5) | 1.6,10.9 |
|
| ||||
| Mortality | 0.0 (0) | 0.0,0.6 | 2.9 (3) | 0.6,8.2 |
CI calculated using exact binomial method.
Seventy unknowns excluded;
Nineteen unknowns excluded;
One patient who died in Emergency Department excluded
CI (confidence interval); LOC (loss of consciousness); GCS (Glasgow Coma Scale); SD (standard deviation); ISS (Injury Severity Score); AIS (Abbreviated Injury Scale); ICP (intracranial pressure); ICU (intensive care unit); LOS (length of stay)
Alcohol use was associated with increased use of imaging resources (Table 3). Nearly eighty percent of the alcohol-consuming bicyclists underwent CT imaging at the time of presentation, compared with 51.5% of the non-consuming group. Alcohol-consuming bicyclists underwent significantly more CT head (76.9% [67.8–84.6] vs. 44.1% [40.0–48.2]), CT cervical spine, (68.3% [58.4–77.1] vs. 40.0% [36.0–44.1]), CT chest (33.7% [24.7–43.6] vs. 11.8% [9.3–14.7], and CT abdomen/pelvis (38.5% [29.1–48.5] vs. 14.2% [11.5–17.3]).
Alcohol-consuming bicyclists more frequently required endotracheal intubation (7.7% [3.4–14.6] vs. 1.7% [0.8–3.1]) and trended towards requiring more surgical procedures (17.3% [10.6–26.0], 8.7% [6.6–11.3]). Alcohol use was also associated with higher rates of hospital admission (50.0% [40.0–60.0] vs. 23.3% [19.9 vs. 26.9]) and ICU admission (30.1% [22.1–40.6] vs. 13.3% [10.7–16.4]) and trended towards longer inpatient length of stay (2.6 days [1.3–3.9] vs. 1.2 days [0.8–1.5]). Mortality was higher among injured bicyclists who had used alcohol (2.9% [0.6–8.2] vs. 0.0% [0.0–0.6]).
A multivariable logistic regression model was run on multiply imputed data to further define the relationship between alcohol use and injury severity (Table 4). In this model, alcohol use was found to be independently associated with more severe injury after adjusting for possible confounders, including helmet use, mechanism of injury, electronic device use, and age (AOR 2.27, p=0.002, 95% CI= [1.40–3.68]). Striking a motor vehicle door was found to be protective against severe injury (AOR 0.54, p=0.032 95% CI= [0.31–0.95]). Additionally, bicyclists who were involved in collisions with other bicyclists or pedestrians were more likely to sustain severe injury (AOR 1.91, p=0.036, 95% CI= [1.04–3.49]).
Table 4.
Multivariable Logistic Regression
| Outcome: Five Category ISS1 | Odds Ratio | Standard Error | p-value | 95 Confidence Interval |
|---|---|---|---|---|
| Alcohol Use | 2.27 | 0.56 | 0.001 | 1.40–3.68 |
| Helmet | 1.03 | 0.19 | 0.871 | 0.72–1.47 |
| Mechanism: | ||||
| Versus Pedestrian or Bicyclist | 1.91 | 0.59 | 0.036 | 1.04–3.49 |
| Versus Motor Vehicle | Reference | N/A | N/A | N/A |
| Fall from bicycle | 1.21 | 0.25 | 0.340 | 0.81–1.81 |
| Striking vehicle door | 0.54 | 0.16 | 0.032 | 0.31–0.95 |
| Use of distracting device | 1.40 | 0.38 | 0.217 | 0.82–2.40 |
| Age 18–54 years | 0.58 | 0.15 | 0.030 | 0.36–0.95 |
ISS categories defined as: No Injury, Mild: ISS 1–8, Moderate: ISS 9–15, Severe: ISS 16–24, Critical: ISS ≥ 25
ISS: Injury Severity Score
Discussion
Our study identified differences in behaviors and injury mechanisms between bicyclists who used alcohol prior to injury and those who did not. Alcohol-consuming bicyclists were more likely to be unhelmeted and to sustain LOC. They underwent more CT imaging studies, which were warranted as they were more likely to sustain any injury and critical injury. Alcohol-consuming bicyclists also had higher rates of hospitalization, endotracheal intubation, ICU admission, and death, while alcohol was independently associated with more severe injury age (AOR 2.27, p=0.002, 95% CI= [1.40–3.68]).
The rate of alcohol use among injured bicyclists in our study was 15.1%, which is consistent with other studies. A recent study by Asbridge et al. [11] also found 15% of injured bicyclists to be under the influence of alcohol or other intoxicating substances at the time of injury. Their results showed that alcohol caused a four-fold increased risk of a bicycling crash. In a 2003 study by Rosenkranz et al. [12] that reviewed injuries from a Massachusetts hospital, 16% of injured bicyclists were intoxicated at the time of injury as defined by positive BAL although not all patients had BALs drawn. Other studies which analyzed severely injured or fatal bicycle crashes quote higher rates of alcohol intoxication on the order of 19–21% [13, 14]. The identification of patients with alcohol intoxication varies based on the definition used and the study design. Additionally, objectivity is frequently lacking in determining alcohol intoxication as trauma centers do not consistently or routinely screen for alcohol use for all injured patients [2]. Standardization of screening practices and of alcohol-use definitions would be beneficial to better interpret and compare results.
Orsi et al.[10] studied German bicyclists injured in collisions and demonstrated a male predominance among the intoxicated subjects: women were 80% less likely to be intoxicated than men. This finding was consistent with several others. Stubig et al. [2] found higher rates of intoxicated road traffic incidents among males and those between 25 and 34 years of age. Plurad et al. [15] studied all bicyclist traumas presenting to thirteen hospitals and found young males, particularly Hispanics, to have high alcohol levels. In our study, age, gender and ethnicity distribution were not significantly different between those bicyclists who had used alcohol and those who had not; patients aged 13–17 and over 65 years were infrequently intoxicated. Likely, cultural, socioeconomic and geographic factors play a role in these discrepancies.
There are a several ways in which alcohol leads to traffic-related injury [5]. First, alcohol alters psychomotor skills, cognitive functions, and endurance performance, thereby reducing a rider’s ability to maintain balance, negotiate traffic, and perceive and respond to situational hazards [5, 16]. Additionally, a host of risk-taking behaviors correlating with alcohol use expose subjects to more dangerous circumstances and increase the risk of injury [5]. These behaviors include riding at higher speeds or riding at night or under adverse roadway or weather conditions. Our study found that intoxicated bicyclists were more likely to be riding at night and for leisure. These findings correspond with the Orsi et al.[10] and Twisk et al.[4], who speculated that riding at night in the setting of poor visibility may synergistically contribute to bicycling crashes among intoxicated bicyclists.
Juhra et al.[17] noted that bicyclists often disregard traffic laws (such as crossing a street on red, driving on the wrong side, etc.), which was one of the main causes of bicycle collisions with motor vehicles; they did not report on alcohol intoxication. Our study found no association between intoxicated bicycling and traffic law violations, including riding against traffic or crossing against the signal.
The mechanism of injury can also vary for intoxicated bicyclists, with prior studies demonstrating an association of alcohol-intoxication with increased risk of bicyclists being injured at a higher speed of impact [2]. Our study found that intoxicated bicycling was associated with falls from bicycles, but involved a lower proportion of collisions with motor-vehicles or with stationary vehicle open doors. We also found no differences in self-reported speeds. These results likely represent the congested, low-velocity, motor vehicle-dominated traffic environment of NYC.
Lack of helmet use is a risk-taking behaviour, which significantly impacts risk of injury among intoxicated bicyclists. Intoxicated bicyclists in our study used helmets less often as compared to sober bicyclists. Other studies have similarly noted a negative correlation between helmet use and alcohol intoxication [5, 6, 10, 18]. Orsi et al. [10] reported that cyclists who did not wear a helmet were more than twice as likely to be intoxicated as those who did (OR 2.41, 95% CI 1.08–5.38). Li et al. [5] found that patients with a BAL less than 0.02g/dL were seven times as likely as those with a BAL greater than 0.02g/dL to be wearing a helmet (35% vs. 5%, p=0.007). As a result of infrequent helmet use, intoxicated bicyclists are also at higher risk for head and brain injury, with our results demonstrating a three-fold increase in percentage of head and neck AIS among intoxicated bicyclists (20.2% vs. 7.7%). Anderson et al. [18] found that 57% of intoxicated bicyclists sustained head injuries versus 30% of sober riders. Similar findings were reported by a 2010 study by Crocker et al, which demonstrated a strong correlation between alcohol use and head injury (OR 3.23, 95% CI 1.57–6.63) [19]. In 2012, the same group focused their regression analysis on whether increased risks of head and brain injury among intoxicated bicyclists were caused by their lower rates of helmet use and concluded that alcohol use is independently associated with head and brain injury regardless of helmet use [20].
Intoxicated bicyclists in our study were more likely to present with a GCS under nine consistent with coma and severe traumatic brain injury. This finding has been echoed in other studies, including one by Plurad et al. [15] who found high BALs to be positively associated with low GCS. Low GCS on presentation among intoxicated trauma patients may be secondary to brain injury or may represent depressed levels of consciousness from intoxication alone [3].
In addition to head injury, other injuries may be impacted by alcohol intoxication among bicyclists. Alcohol-consuming bicyclists in our study sustained more head and neck, face, abdomen, and skin and soft tissue injuries, contributing to an overall greater injury severity. An association between alcohol and injury severity has been noted in other studies [2, 21]. In our study, alcohol use was found to be independently associated with more severe injury after controlling for other factors such as helmet use, mechanism of injury, and age. This implies that alcohol use makes it more likely that cyclists will suffer severe injury in the event of a crash. This contrasts with certain studies that have suggested a potential protective effect on injury severity and even a reduced trauma mortality in intoxicated patients [22, 23]; these studies did not stratify for bicyclists but instead focused on overall victims of trauma.
Our study found that hospital resource use, hospital and ICU admission rates and durations, and interventions such as endotracheal intubations were significantly more common among alcohol-consuming bicyclists. Regarding hospital admissions, although a majority of our patients were discharged from the ED, a much greater proportion of intoxicated bicyclists were admitted versus sober bicyclists. The reasons for this may be similar to those discussed in a study on intoxicated pedestrians by Dultz et al. [3]. Like intoxicated pedestrians, intoxicated bicyclists present with more injuries overall and more severe injuries. Additionally, intoxication even without injury often requires admission for repeating of an unreliable physical exam in a sober patient to assess for unrecognized injuries or for social reasons. In the same vein, the higher rates of CT scans obtained for intoxicated bicyclists are likely a result of these unreliable exams. The increased rates of hospital and ICU admission and the longer LOS lead to higher costs for hospitals irrespective of the cause [3]. Spaite et al.[21] found a similar association with ICU stay and intoxication (13.3 vs. 2.8 mean ICU days), as well as an increase in mean hospital charges ($7206 vs. $1170) among admitted intoxicated bicyclists compared with sober ones.
Several studies have demonstrated that the mortality rate is higher among intoxicated individuals involved in a traffic crash [2]. Li et al. [9]found that alcohol use among bicyclists dying in crashes may be as high as one in three. Nicaj et al. [14] analyzed NYC bicycle fatalities from 1996–2005 and found that 21% of fatally injured bicyclists had detectable levels of blood alcohol. Another study by Li et al. [24] found that bicyclists who died at the scene were four times as likely as those who died in hospitals to be legally intoxicated (35% vs. 9%, p<0.02). Our results confirm the association of intoxication with higher rates of mortality and indicate that alcohol pays an important role in fatal and serious bicycling injuries.
Our study used a BAL level below the legal limit in NYC as the lower limit of the laboratory definition for alcohol consumption given that certain individuals may be affected by low levels of alcohol [15, 25]. Because a large portion of our alcohol use group did not have BAL drawn at the time of injury, we did not perform sub-analyses based on variable levels of BAL. Other studies have shown that higher BAL may be associated with greater risk of injury; Twisk et al. [4] demonstrated that a BAL of 0.02g/dl has 5.6 times higher risk of bicycling injury relative to sober bicyclists. When the BAL increases to 0.08, the risk of bicycling injury rose to 20 times that of sober bicyclists. Additionally, the results of several European experimental studies suggested that bicycle riding requires a higher level of psychomotor skills than driving a car, implying that a low BAL may impair a bicyclist more than a motorist [24].
Several studies have shown an association between intoxicated bicycling collisions and repeated bicycling under the influence as well as a history of chronic alcohol use [8, 11, 26]. In a study of 120 bicyclists injured between 1990 and 1997, Li et al. found that bicyclists with positive BALs at the time of admission to a trauma center were significantly more likely than those with negative BALs to have a record of licence suspension/revocation (52% vs. 14%, p<0.01) and to have ‘driving while intoxicated’ or ‘driving under the influence of alcohol’ convictions (30% vs. 3%, p<0.01) [8]. It may be beneficial to expand public policy and prevention programs that target drunk drivers to include drunk cyclists as well.
Bicycling under the influence of alcohol is associated with significant risk of collision, injury, critical injury, and mortality. Yet few people seem to be aware of this risk [18], as there is a dearth of research on alcohol intoxication in the context of bicycling injuries limiting the ability of legislators and those involved in health policy to direct public health initiatives. Although arguments against legislation have been made so as not to limit bicycling or worse promote intoxicated driving [27], a negative impact may be less likely in NYC in light of its vast public transportation system. For their part, trauma centers must continue to implement and strengthen screening, brief intervention, and referral to treatment programs [28, 29] to ideally include all injured patients including those treated and released.
The authors acknowledge several limitations in this study. First, this is a single hospital center study, so results may not be generalizable to experiences of other hospitals and geographical locations. Second, not all subjects had BALs drawn at the time of injury, thus some level of subjectivity may be involved in determining intoxication. Given that it is unlikely that a patient would report alcohol use when it was not used, this study likely underreports the nature of the problem. To be clear, we found that 15% of injured cyclists used alcohol; this study was not designed to identify the percentage of all riders who consume alcohol prior to riding. More liberal or standardized BAL draws may have prevented this problem. Nonetheless, it is rare and not value-based for trauma centers to routinely obtain BAL on all patients as reflected in past studies. Another limitation is recall bias of circumstances of the crash incident, which can be an issue especially with intoxicated subjects. We attempted to reduce this by speaking with corroborating sources including first responders. A fourth limitation is selection bias; this study does not include patients who refused to be brought to the hospital or were declared dead at the scene within our catchment area. Lastly, the use of other illicit substances was not systematically assessed for in our study and may have played a role in a similar fashion as alcohol.
Conclusion
Within a dense urban environment, alcohol consumption by bicyclists is associated with more severe injury, greater hospital resource use, and higher mortality. As bicycling continues to increase in popularity across many cities internationally, it is important to heighten awareness about the risks and consequences of bicycling while under the influence of alcohol.
References
- 1.Cummings P, Rivara FP, Olson CM, Smith KM. Changes in traffic crash mortality rates attributed to use of alcohol, or lack of a seat belt, air bag, motorcycle helmet, or bicycle helmet, United States, 1982–2001. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2006;12:148–154. doi: 10.1136/ip.2005.010975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stubig T, Petri M, Zeckey C, Brand S, Muller C, Otte D, Krettek C, Haasper C. Alcohol intoxication in road traffic accidents leads to higher impact speed difference, higher ISS and MAIS, and higher preclinical mortality. Alcohol (Fayetteville, NY) 2012;46:681–686. doi: 10.1016/j.alcohol.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Dultz LA, Frangos S, Foltin G, Marr M, Simon R, Bholat O, Levine DA, Slaughter-Larkem D, Jacko S, Ayoung-Chee P, Pachter HL. Alcohol use by pedestrians who are struck by motor vehicles: how drinking influences behaviors, medical management, and outcomes. The Journal of trauma. 2011;71:1252–1257. doi: 10.1097/TA.0b013e3182327c94. [DOI] [PubMed] [Google Scholar]
- 4.Twisk DA, Reurings M. An epidemiological study of the risk of cycling in the dark: the role of visual perception, conspicuity and alcohol use. Accident; analysis and prevention. 2013;60:134–140. doi: 10.1016/j.aap.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 5.Li G, Baker SP, Smialek JE, Soderstrom CA. Use of alcohol as a risk factor for bicycling injury. JAMA : the journal of the American Medical Association. 2001;285:893–896. doi: 10.1001/jama.285.7.893. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Ruiz V, Lardelli-Claret P, Jimenez-Mejias E, Amezcua-Prieto C, Jimenez-Moleon JJ, de Luna del Castillo JD. Risk factors for causing road crashes involving cyclists: An application of a quasi-induced exposure method. Accident; analysis and prevention. 2013;51:228–237. doi: 10.1016/j.aap.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 7.Olkkonen S, Honkanen R. The role of alcohol in nonfatal bicycle injuries. Accident; analysis and prevention. 1990;22:89–96. doi: 10.1016/0001-4575(90)90010-i. [DOI] [PubMed] [Google Scholar]
- 8.Li G, Shahpar C, Soderstrom CA, Baker SP. Alcohol use in relation to driving records among injured bicyclists. Accident; analysis and prevention. 2000;32:583–587. doi: 10.1016/s0001-4575(99)00089-5. [DOI] [PubMed] [Google Scholar]
- 9.Li G, Baker SP. Alcohol in fatally injured bicyclists. Accident; analysis and prevention. 1994;26:543–548. doi: 10.1016/0001-4575(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 10.Orsi C, Ferraro OE, Montomoli C, Otte D, Morandi A. Alcohol consumption, helmet use and head trauma in cycling collisions in Germany. Accident; analysis and prevention. 2014;65:97–104. doi: 10.1016/j.aap.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 11.Asbridge M, Mann R, Cusimano MD, Tallon JM, Pauley C, Rehm J. Cycling-related crash risk and the role of cannabis and alcohol: a case-crossover study. Preventive medicine. 2014;66:80–86. doi: 10.1016/j.ypmed.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Rosenkranz KM, Sheridan RL. Trauma to adult bicyclists: a growing problem in the urban environment. Injury. 2003;34:825–829. doi: 10.1016/s0020-1383(02)00389-3. [DOI] [PubMed] [Google Scholar]
- 13.Rowe BH, Rowe AM, Bota GW. Bicyclist and environmental factors associated with fatal bicycle-related trauma in Ontario. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 1995;152:45–53. [PMC free article] [PubMed] [Google Scholar]
- 14.Nicaj L, Stayton C, Mandel-Ricci J, McCarthy P, Grasso K, Woloch D, Kerker B. Bicyclist fatalities in New York City: 1996–2005. Traffic injury prevention. 2009;10:157–161. doi: 10.1080/15389580802641761. [DOI] [PubMed] [Google Scholar]
- 15.Plurad D, Demetriades D, Gruzinski G, Preston C, Chan L, Gaspard D, Margulies D, Cryer HG. Pedestrian injuries: the association of alcohol consumption with the type and severity of injuries and outcomes. Journal of the American College of Surgeons. 2006;202:919–927. doi: 10.1016/j.jamcollsurg.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 16.Lecoultre V, Schutz Y. Effect of a small dose of alcohol on the endurance performance of trained cyclists. Alcohol and alcoholism (Oxford, Oxfordshire) 2009;44:278–283. doi: 10.1093/alcalc/agn108. [DOI] [PubMed] [Google Scholar]
- 17.Juhra C, Wieskotter B, Chu K, Trost L, Weiss U, Messerschmidt M, Malczyk A, Heckwolf M, Raschke M. Bicycle accidents - do we only see the tip of the iceberg? A prospective multi-centre study in a large German city combining medical and police data. Injury. 2012;43:2026–2034. doi: 10.1016/j.injury.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 18.Andersson AL, Bunketorp O. Cycling and alcohol. Injury. 2002;33:467–471. doi: 10.1016/s0020-1383(02)00028-1. [DOI] [PubMed] [Google Scholar]
- 19.Crocker P, Zad O, Milling T, Lawson KA. Alcohol, bicycling, and head and brain injury: a study of impaired cyclists’ riding patterns R1. The American journal of emergency medicine. 2010;28:68–72. doi: 10.1016/j.ajem.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Crocker P, King B, Cooper H, Milling TJ. Self-reported alcohol use is an independent risk factor for head and brain injury among cyclists but does not confound helmets’ protective effect. The Journal of emergency medicine. 2012;43:244–250. doi: 10.1016/j.jemermed.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 21.Spaite DW, Criss EA, Weist DJ, Valenzuela TD, Judkins D, Meislin HW. A prospective investigation of the impact of alcohol consumption on helmet use, injury severity, medical resource utilization, and health care costs in bicycle-related trauma. The Journal of trauma. 1995;38:287–290. doi: 10.1097/00005373-199502000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Blondell RD, Looney SW, Krieg CL, Spain DA. A comparison of alcohol-positive and alcohol-negative trauma patients. Journal of studies on alcohol. 2002;63:380–383. doi: 10.15288/jsa.2002.63.380. [DOI] [PubMed] [Google Scholar]
- 23.Yaghoubian A, Kaji A, Putnam B, De Virgilio N, De Virgilio C. Elevated blood alcohol level may be protective of trauma patient mortality. The American surgeon. 2009;75:950–953. [PubMed] [Google Scholar]
- 24.Li G, Baker SP, Sterling S, Smialek JE, Dischinger PC, Soderstrom CA. A comparative analysis of alcohol in fatal and nonfatal bicycling injuries. Alcoholism, clinical and experimental research. 1996;20:1553–1559. doi: 10.1111/j.1530-0277.1996.tb01698.x. [DOI] [PubMed] [Google Scholar]
- 25.Kerr WC, Greenfield TK. Racial/Ethnic Disparities in the Self-Reported Number of Drinks in 2 Hours Before Driving Becomes Impaired. American journal of public health. 2015;105:1409–1414. doi: 10.2105/AJPH.2014.302276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weber JE, Maio RF, Blow FC, Hill EM, Barry KL, Waller PF. Alcohol and/or other drug use among adult non-occupant motor vehicle crash victims. Alcohol and alcoholism (Oxford, Oxfordshire) 2002;37:468–471. doi: 10.1093/alcalc/37.5.468. [DOI] [PubMed] [Google Scholar]
- 27.Komanoff C. Elevated blood alcohol and risk of injury among bicyclists. JAMA : the journal of the American Medical Association. 2001;285:2445–2446. doi: 10.1001/jama.285.19.2445. [DOI] [PubMed] [Google Scholar]
- 28.Gentilello LM. Alcohol interventions in trauma centers: the opportunity and the challenge. The Journal of trauma. 2005;59:S18–20. doi: 10.1097/01.ta.0000174703.52284.f3. [DOI] [PubMed] [Google Scholar]
- 29.Gentilello LM. Confronting the obstacles to screening and interventions for alcohol problems in trauma centers. The Journal of trauma. 2005;59:S137–143. doi: 10.1097/01.ta.0000174877.66875.f3. discussion S146–166. [DOI] [PubMed] [Google Scholar]