Abstract
Objectives
The diagnostic efficacy of sentinel lymph node biopsy(SLNB) in early oral squamous cell carcinoma(OSCC) still remains controversial. This meta-analysis was conducted to assess the diagnostic value of SLNB in clinically neck-negative T1-2 OSCC.
Methods
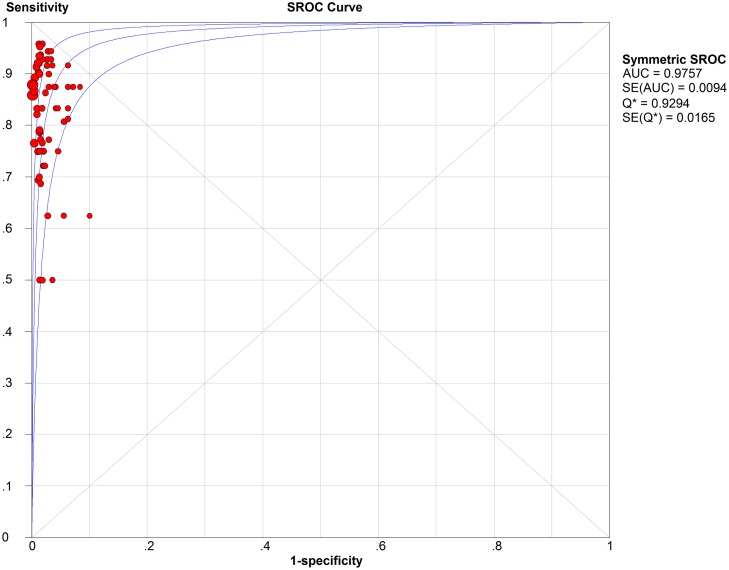
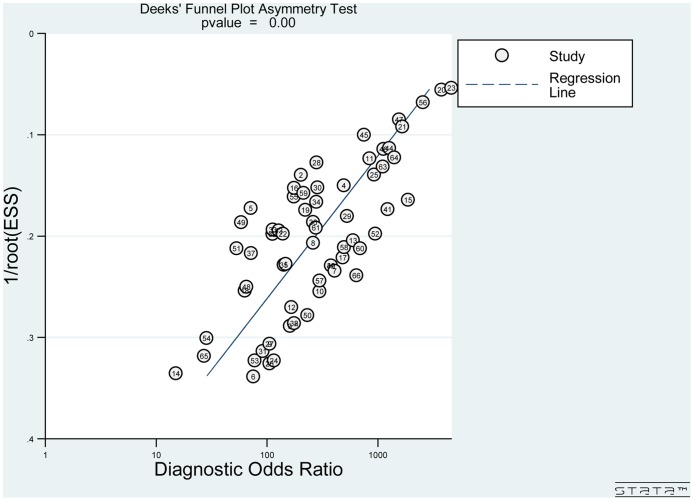
A systematic literature search for relevant literature published up to September 11, 2016 was conducted in PubMed, Embase, Web of Science, Cochrane Library and ClinicalTrials, and the reference lists of eligible studies were examined. Data from different studies were pooled to estimate the summary sentinel lymph node(SLN) identification rate, sensitivity, negative predictive value. Summary receiver operator characteristic curve(SROC) was plotted and area under the SROC curve (AUC) was calculated to evaluate the overall diagnostic efficacy. Threshold effect was assessed with use of the spearman correlation coefficient. Between-study heterogeneity was tested using the Q tests and the I2 statistics. Subgroup analyses were conducted in view of the greater effect of different study characteristics on diagnostic efficacy of SLN. Deeks’ funnel plot asymmetry test was performed to evaluate publication bias. Sensitivity analysis was evaluated through omitting studies one by one and comparing the pooled results of random-effects model and fixed-effects model. All analyses were performed using Review Manager (version 5.3.5), Meta-DiSc (version 1.4), Comprehensive Meta Analysis (version 2.0) and STATA (version 12).
Results
66 studies comprising 3566 patients with cT1-2N0 OSCC were included in this meta-analysis. The pooled SLN identification rate was 96.3%(95% CI: 95.3%-97.0%). The pooled sensitivity was 0.87 (95% CI: 0.85–0.89), pooled negative predictive value was 0.94 (95% CI: 0.93–0.95), and AUC was 0.98 (95% CI: 0.97–0.99). Subgroup analyses indicated that SLN assessment with immunohistochemistry(IHC) achieved a significantly higher sensitivity than without IHC.
Conclusions
This meta-analysis suggests that SLNB has a high diagnostic accuracy in cT1-2N0 oral squamous cell carcinoma, and is an ideal alternative to elective neck dissection. Furthermore, the use of IHC can significantly improve SLNB diagnostic sensitivity for early OSCC.
Introduction
Oral squamous cell carcinoma (OSCC) is one of the most common types of cancer in the world, with a considerable incidence of new cases every year. Approximately 50% of the patients with OSCC present with early stage disease(cT1-2N0) [1]. The main prognostic factor is occult lymph node metastasis in the neck. As it was reported in previous literatures, the overall rate of occult lymph node metastasis is 20%-30% in early stage OSCC patients [2–4]. Therefore, elective neck dissection remains the gold standard treatment in many institutions, resulting in overtreatment in over 70% of early OSCC patients and a considerable morbidity. For this reason, in recent years, sentinel lymph node biopsy(SLNB) has become more important and popular in the cervical treatment of patients with early OSCC. The sentinel lymph node (SLN) procedure is based on the theory that flow from a primary tumor travels sequentially to the sentinel lymph node and subsequently to the remaining lymph node basin [5]. Compared to elective neck dissection, SLNB is less invasive, cost-effective and beneficial to patient quality of life [6–9]. But the diagnostic efficacy of SLNB in early OSCC remains controversial [10–12]. Furthermore, most previous individual studies contained too small of a sample size to yield a valid conclusion. In addition, previous meta-analyses mainly focused on head and neck cancer or oral and oropharyngeal carcinoma [13–16]. However, combining different subset of head and neck cancer with differing clinical characteristics and metastasis patterns, can lead to heterogeneous results for SLNB. Although some previous meta-analyses have conducted subgroup analysis on OSCC, the small included sample size was underpowered to yield credible pooled findings. In recent years, many high quality prospective and some multi-institutional studies on the diagnostic efficacy of SLNB in early OSCC have been published [17–19]. Therefore, we performed a meta-analysis to summarize the diagnostic efficacy of SLNB specially focused exclusively on early OSCC. Additionally, we further stratified results by different clinical and study characteristics in order to explore the potential factors that may affect the diagnostic accuracy and applicability of SLNB.
Materials and Methods
Search strategy
We conducted a search for relevant literatures published up to September 11, 2016 in PubMed, Embase, Web of Science and Cochrane Library. The following medical subject headings(MeSH) and keywords were used: ("oral neoplasm" or "oral cancer" or "oral tumor" or "mouth neoplasm" or "mouth cancer" or "mouth tumor" or "head and neck neoplasm" or "head and neck cancer" or "head and neck tumor") and ("sentinel lymph node biopsy" or "sentinel"). We used no language restrictions. We also manually searched the reference lists of eligible studies and ClinicalTrials.gov to ensure identification of relevant published and unpublished studies.
Inclusion and exclusion criteria
Articles included need to fulfill the following criteria: (1) Human cT1/T2N0 oral cavity squamous cell carcinoma patients (in studies that included T3, T4, N+ or other head and neck tumor cases, only the cT1–T2N0 oral cancer cases were selected); (2) the use of radioactive tracer, blue dye or indocyanine green; (3) presence of "gold standard", which was defined as the use of histological evaluation and follow-up; (4) studies presented sufficient data to allow for the construction of 2×2 tables, including true positive (TP), false positive (FP), false negative (FN) and true negative (TN); (5) Full text available in English. Studies that met the following criteria were excluded: (1) reports of duplicate data published in other studies; (2) letters, editorials, case reports or reviews; (3) studies without qualified data; (4) studies that included T3, T4 or N+ oral cavity cases or other head and neck tumors and not possible to be separated; (5) Full text in English unavailable.
Two reviewers(MY Liu and XH Yang) independently performed first-stage screening of titles and abstracts based on the research question. For the second screening, we retrieved articles in full text according to the initial screening. Any discrepancies were resolved by discussion or referred to a third author.
Data extraction and quality assessment
Two investigators (MY Liu and XH Yang) independently reviewed the full texts of included studies and recorded the following data: first author, year of publication, sample size, description of study population (age), study design (prospective or retrospective), pathology (H&E staining, immunohistochemistry (IHC), serial sectioning (SS)), SLN tracer, SLN identification rate, average of SLNs harvested, data for diagnostic meta-analysis (TP, FP, FN, and TN) and so on. Results were then compared and any disagreements were settled by consensus. Concerning the quality of study design, study quality was assessed with the QUADAS-2 checklist for studies of diagnostic accuracy included in systematic reviews [20].
Analysis
The identification rate, sensitivity and negative predictive value together with their 95% confidence intervals (95% CIs) were summarized in the current meta-analysis. The sensitivity and specificity of each included study were used to plot the summary receiver operator characteristic (SROC) curve and calculate the area under the SROC curve (AUC).
Q tests and I2 statistics were used to assess the degree of heterogeneity between studies. A p value less than 0.1 for the Q test and an I2 higher than 50% indicated the existence of significant heterogeneity. Pooled estimates were derived using the fixed-effects model if significant heterogeneity was not present. In case of heterogeneity, the random-effects model was applied.
We assessed diagnostic threshold effect with use of the spearman correlation coefficient. In addition, We further stratified results by the average of SLNs harvested (low: <2, medium: 2≤ and <3 or high: ≥3), SLN pathology methods(IHC or not, SS or not), type of reference test(neck dissection or follow-up), SLN tracer(single tracer or multiple tracers), study design (prospective or retrospective) and publication year(early: 2000–2008 or late: 2009–2016) in view of the greater effect of different study characteristics on diagnostic efficacy of SLN, and to explore the sources of between-study heterogeneity.
In this meta analysis, we performed a sensitivity analysis to evaluate the credibility and consistency of the results through omitting studies one by one and comparing the pooled results of random-effects model and fixed-effects model. Publication bias was assessed by using Deeks' funnel plot.
Two-sided p values were calculated with p<0.05 considered significant for all tests. We did statistical analysis with Review Manager (version 5.3.5), Meta-DiSc (version 1.4), Comprehensive Meta Analysis (version 2.0) and STATA (version 12).
Results
Search results and study selection
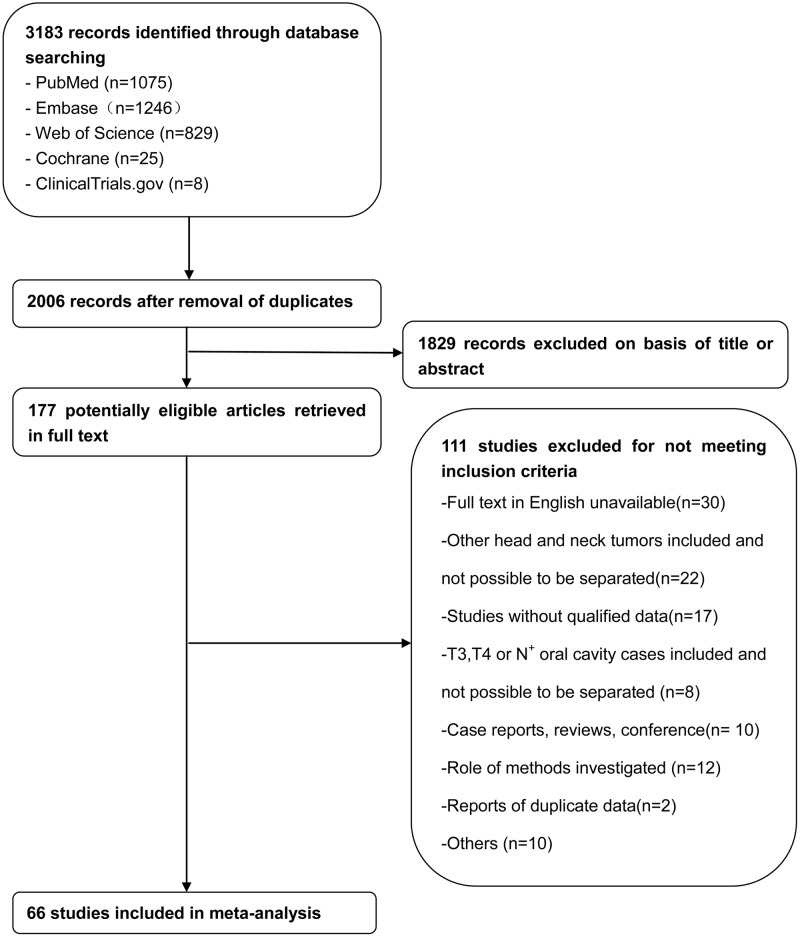
Fig 1 shows the study flowchart. The initial search returned a total of 3183 studies, of which 1177 were excluded as duplications. The remaining 2006 articles were subject to further evaluation. After titles and abstracts were reviewed, 1829 were excluded, leaving 177 articles available for full text review. After full text review, an additional 111 manuscripts were excluded (the reasons were presented on Fig 1). Finally, 66 studies fulfilled the inclusion criteria for the meta analysis, comprising 3566 patients [5, 10–12, 17–19, 21–79] (Fig 1).
Fig 1. Study flow diagram.
Study characteristics
Table 1 summarizes individual studies and their characteristics. Of the 66 studies, the publication years of the included articles ranged from 2000 to2016 (26 articles were published during 2000 and 2008 while 40 articles were published during 2009 and 2016). Among the 66 studies, 56 researches were prospective while 10 studies were retrospective. Additionally, 43 studies detected the SLN by single tracer while 23 studies by multiple tracers. In all included studies, SLN was diagnosed based on histopathology(H&E staining, IHC and/or SS), which is considered the gold standard reference for SLN metastasis diagnosis. Of the total 3566 cases, SLN could be harvested in 3516 cases. The pooled SLN identification rate was 96.3%(95% CI: 95.3%-97.0%). The data of average SLN harvested per person was reported in 38 studies. The TP, FP, FN and TN results for individual studies were shown in Table 1.
Table 1. Basic characteristics of included studies.
| study | year | Design | Population | Index Test | Reference Test ND or FU(mean, range) | Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age, median (range) or mean(SD), y | SLN tracer | SLN localization | Pathology (SLN) | SLN identification rate | No. of SLN, mean | TP | FP | FN | TN | ||||
| Ramamurthy | 2014 | Pros | 32 | 43(26–70) | B | B | H+I+S | ND | 29/32 | 1.56 | 4 | 0 | 1 | 24 |
| Chung | 2015 | Pros | 61 | 49.3(10.3) | R | L+G | H+I+S | FU (70months, 49–111) | 61/61 | NR | 12 | 0 | 5 | 44 |
| Julio | 2007 | Pros | 14 | 65.9(13.7) | R+ICG | L+G | H+I | ND | 14/14 | 3.2 | 3 | 0 | 0 | 11 |
| Heuveling | 2014 | Pros | 66 | NR | R+B | L+G+B+SPECT | Unclear | ND | 66/66 | 2 | 11 | 0 | 2 | 53 |
| Terada | 2011 | Pros | 45 | 62(30–85) | R | L+G+SPECT | H | FU (46months, 9–72) | 45/45 | NR | 5 | 0 | 5 | 35 |
| Barzan | 2002 | Pros | 10 | 64(36–85) | R | G | Unclear | ND | 9/10 | NR | 2 | 0 | 0 | 7 |
| Bluemel | 2014 | Pros | 23 | 58.7(13) | R | L+G+SPECT/CT | H+I+S | ND | 23/23 | 3.1 | 5 | 0 | 0 | 18 |
| Terada | 2008 | Pros | 43 | NR | R | L+G+SPECT/CT | Unclear | ND | 41/43 | NR | 5 | 0 | 1 | 35 |
| Chiesa | 2000 | Pros | 11 | NR | R | L+G | Unclear | ND | 10/11 | NR | 3 | 0 | 0 | 7 |
| Dequanter | 2013 | Pros | 20 | 64(?) | R | L+G | H+I+S | FU (59months, ?-?) | 20/20 | NR | 4 | 0 | 0 | 16 |
| Broglie | 2011 | Pros | 69 | 60(?) | R | L+G+SPECT+PET-CT | Unclear | FU (59.8months, 2.6–120.7) | 69/69 | NR | 23 | 0 | 2 | 44 |
| Vigili | 2007 | Pros | 12 | 57.4(?) | R | L+G | H+I | ND | 12/12 | 2.1 | 5 | 0 | 0 | 7 |
| Aida | 2014 | Pros | 25 | 61.2(42–82) | R | L+G+SPECT/CT | Unclear | FU (?months, 7–88) | 25/25 | NR | 8 | 0 | 0 | 17 |
| Joost | 2013 | Pros | 7 | 59.5(33–73) | ICG | NI | H | ND | 7/7 | 1.7 | 2 | 0 | 1 | 4 |
| Bilde | 2008 | Pros | 51 | 58(29–90) | R | L+G+SPECT/CT | H+I+S | ND | 51/51 | 3 | 11 | 0 | 0 | 40 |
| Chaturvedi | 2015 | Pros | 53 | 44(29–70) | R | L+G+SPECT | H | ND | 51/53 | 3.8 | 10 | 0 | 4 | 37 |
| Yen | 2006 | Pros | 25 | 47.8(30–66) | R | L+G | H+I+S | ND | 24/25 | 2.4 | 6 | 0 | 0 | 18 |
| Minamikawa | 2005 | Retro | 18 | NR | B | B | Unclear | FU (NR) | 15/18 | NR | 4 | 0 | 1 | 10 |
| Ram | 2015 | Retro | 42 | 61.3(40–83) | R | L+G+SPECT/CT | H+I+S | FU (NR) | 42/42 | NR | 8 | 0 | 2 | 32 |
| Schilling | 2015 | Pros | 415 | 61(28–92) | R+B | L+G+B | H+I+S | FU (>36months) | 415/415 | 3.2 | 94 | 0 | 15 | 306 |
| Civantos | 2010 | Pros | 140 | 58(24–90) | R | L+G | H+I | ND | 140/140 | 3 | 37 | 0 | 4 | 99 |
| Rigual | 2013 | Retro | 38 | 62(14) | R | L+G | H | FU (31months, 3–71) | 38/38 | 2 | 5 | 0 | 2 | 31 |
| Tartaglione | 2016 | Pros | 434 | NR | R+B | L+G+B+SPECT/CT | H+I+S | ND | 434/434 | 3.2 | 105 | 0 | 14 | 315 |
| Harri | 2008 | Pros | 13 | 65(30–84) | R+B | L+G+B | H+I+S | FU (21months, 12–42) | 13/13 | 3.1 | 2 | 0 | 0 | 11 |
| Pezier | 2012 | Pros | 59 | 62.5(38–90) | R+B | L+G+B | H+I | FU (22.5months, 0.26–53) | 57/59 | 2.6 | 17 | 0 | 1 | 39 |
| Hart | 2005 | Pros | 12 | 62.75(35–83) | R | L+G | H+I+S | ND | 12/12 | NR | 2 | 0 | 0 | 10 |
| Keyvan | 2016 | Pros | 10 | 52(21–82) | R | L+G | Unclear | ND | 10/10 | 2.4 | 3 | 0 | 0 | 7 |
| Flach | 2014 | Pros | 62 | 61.2(28.8–82.6) | R+B | L+G+B | H+I+S | FU (52.5months, 5.3–76.7) | 62/62 | NR | 20 | 0 | 5 | 37 |
| Vishno | 2015 | Pros | 65 | 47(20–77) | B | B | H+I | ND | 60/65 | 2.02 | 7 | 0 | 1 | 52 |
| Hasegawa | 2011 | Pros | 61 | NR | R | G | Unclear | FU (NR) | 60/61 | NR | 10 | 0 | 3 | 47 |
| Burns | 2009 | Pros | 9 | 59.2(38–80) | R+B | L+G+B | H+I | FU (?months, 9–24) | 9/9 | 1.3 | 3 | 0 | 0 | 6 |
| Kontio | 2004 | Pros | 15 | 63.8(35–81) | R+B | L+G+B | H+I | ND | 15/15 | 2.8 | 3 | 0 | 0 | 12 |
| Frerich | 2007 | Pros | 26 | NR | R | G | H+I+S | FU (27.5months, 7.2–49.5) | 26/26 | 2.1 | 8 | 0 | 2 | 16 |
| Hiraki | 2016 | Retro | 47 | 65.4(12.6) | R | L+G+SPECT/CT | H+S | FU (38.5months, 12.4–64.6) | 47/47 | 2.1 | 9 | 0 | 2 | 36 |
| Honda | 2015 | Pros | 31 | 64(33–91) | B | B+CT(Iopamidol) | Unclear | FU (>30months) | 28/31 | NR | 4 | 0 | 1 | 23 |
| Fan | 2014 | Retro | 30 | 48(27–75) | R+B | L+G+B | H | FU (>120months) | 30/30 | NR | 9 | 0 | 1 | 20 |
| Rigual | 2005 | Pros | 20 | NR | R+B | L+G+B | H | ND | 20/20 | NR | 10 | 0 | 2 | 8 |
| Stoeckli | 2001 | Pros | 15 | 56(36–81) | R+B | L+G+B | H+I+S | ND | 15/15 | NR | 3 | 0 | 0 | 12 |
| Terada | 2006 | Pros | 20 | NR | R | L+G+SPECT/CT | H | FU(NR) | 20/20 | 3.3 | 6 | 0 | 0 | 14 |
| Jeong | 2006 | Pros | 20 | 53(35–68) | R | L+G | H+I+S | ND | 20/20 | 2.55 | 6 | 0 | 0 | 14 |
| Thomsen | 2007 | Pros | 39 | ?(32–90) | R+B | L+G+B | H+I+S | FU (28months, 4–54) | 37/39 | NR | 11 | 0 | 0 | 26 |
| Hoft | 2004 | Pros | 20 | NR | R | L+G | H+I+S | ND | 20/20 | 3.2 | 6 | 0 | 0 | 14 |
| Samant | 2014 | Pros | 34 | 61(24–82) | R+B | L+G+B | H+I | FU(36months, 2–60) | 32/34 | NR | 6 | 0 | 2 | 24 |
| Toom | 2015 | Retro | 90 | 60(29–86) | R+B | L+G+B+SPECT/CT | H+I+S | FU(18months, 2–62) | 87/90 | 2 | 26 | 0 | 2 | 59 |
| Yoshimoto | 2012 | Retro | 145 | 63(21–92) | R | L+G+SPECT/CT | H+I | FU (NR) | 145/145 | 2.9 | 24 | 0 | 7 | 114 |
| Stoeckli | 2007 | Pros | 79 | 58.5(34–87) | R | L+G | H+I+S | FU (19months, 3–40) | 78/79 | NR | 29 | 0 | 2 | 47 |
| Melkane | 2012 | Pros | 174 | 56(28–86) | R | L+G | H+I+S | FU (>36months) | 166/174 | 2 | 42 | 0 | 6 | 118 |
| Civantos | 2003 | Pros | 14 | 62(34–79) | R | L+G+PET maping | H+I | ND | 14/14 | NR | 6 | 0 | 1 | 7 |
| Alvarez | 2014 | Pros | 28 | 61.2(41–87) | R+B | L+G+B | H+I+S | FU (>60months) | 28/28 | NR | 7 | 0 | 4 | 17 |
| Peng | 2015 | Pros | 19 | 60.5(43–77) | B+ICG | B+NI | H | ND | 19/19 | 3.4 | 3 | 0 | 0 | 16 |
| Hernando | 2016 | Pros | 32 | 66.4(40–90) | R | L+G | H+I+S | FU (48.2months, 7–70) | 32/32 | 2 | 3 | 0 | 3 | 26 |
| Ikram | 2013 | Pros | 42 | 52(31–75) | R | L+G | H+I+S | ND | 38/42 | NR | 7 | 0 | 0 | 31 |
| Taylor | 2001 | Pros | 8 | 61.9(22–80) | R | L+G | Unclear | ND | 8/8 | NR | 3 | 0 | 0 | 5 |
| Yamauchi | 2012 | Pros | 11 | 62.3(36–84) | R | L+G | H+S | FU (37.1months, 20.1–54.1) | 11/11 | NR | 2 | 0 | 1 | 8 |
| Thomsen | 2005 | Pros | 40 | ?(32–90) | R+B | L+G+B | H+I+S | FU (15.8months, 4.3–40.4) | 40/40 | NR | 11 | 0 | 3 | 26 |
| Pedersen | 2016 | Retro | 253 | 63(30–95) | R | L+G+SPECT/CT | H+I+S | FU (32months, 1–92) | 253/253 | 3 | 68 | 0 | 9 | 176 |
| Kaya | 2015 | Pros | 18 | 54.5(28–76) | R | L+G | H+I | ND | 18/18 | NR | 5 | 0 | 0 | 13 |
| Tartaglione | 2008 | Pros | 22 | 62.6(28–80) | R | L+G | H+I | FU (23.2months, 10–35) | 22/22 | 2.2 | 8 | 0 | 0 | 14 |
| Hernandez | 2005 | Pros | 48 | 57(28–83) | R+B | L+G+B | H+S | ND | 48/48 | 2 | 10 | 0 | 3 | 35 |
| Bilde | 2006 | Pros | 34 | 58(47–70) | R | L+G+SPECT/CT | H+I+S | ND | 32/34 | 3 | 6 | 0 | 0 | 26 |
| Bell | 2013 | Pros | 36 | 60.5(20–87) | R | L+G | H+I+S | ND | 35/36 | 1.9 | 7 | 0 | 1 | 27 |
| Matsuzuka | 2014 | Retro | 29 | 66(31–82) | R | L+G | H | FU (91months, 10–165) | 29/29 | 3.1 | 6 | 0 | 2 | 21 |
| Heuveling | 2012 | Retro | 60 | 60(29–81) | R+B | L+G+B | H+I+S | FU (19months, 5–51) | 60/60 | 3 | 21 | 0 | 1 | 38 |
| Agrawal | 2015 | Pros | 66 | 60.8(12.8) | R | L+G+SPECT/CT | H+I | ND | 65/66 | 3.9 | 30 | 0 | 1 | 34 |
| Nakamura | 2015 | Pros | 15 | 63.1(44–84) | R+ICG | L+G+NI | Unclear | FU (38.5months, 10.7–69.9) | 15/15 | 2.2 | 1 | 0 | 1 | 13 |
| Mozzillo | 2001 | Pros | 41 | NR | R+B | L+G+B | Unclear | ND | 39/41 | NR | 4 | 0 | 0 | 35 |
Abbreviations: Pros, Prospective; Retro, Retrospective; NR, Not reported; R, Radionucleotide; B, Blue dye; ICG, Indocyanine green; NI, near-infrared fluorescence camera; H, Hematoxylin and eosin; I, Immunohistochemistry; S, Serial sectioning; ND, Neck dissection; FU, Follow-up; SLN, Sentinel lymph node; TP, Ture positive; FP, False positive; FN, False Negative; TN, Ture negative.
Quality of included studies
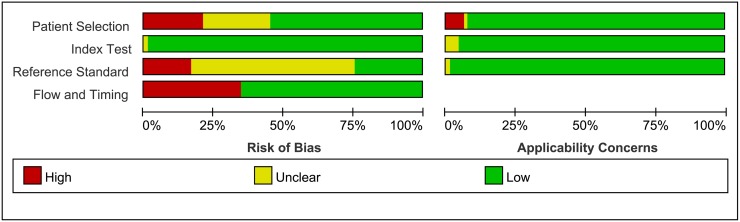
Quality assessments are shown in a bar graph of QUADAS-2 in Fig 2. The graph indicates that all included studies were of moderately high quality. Risk of bias regarding patient selection was high in 14 (21.2%) studies mostly due to their retrospective nature without a consecutive or random sample enrollment of patients. Risk of bias regarding index test was unclear in only 1(1.5%) study while 65 (98.5%) studies were low risk. By contrast, the reference standard was unclear in 39 (59.1%) studies because in most of these studies it was unclear whether the index test and reference test were interpreted independently and blindly from each other. For risk of bias in flow and timing there were 23 (34.8%) studies considered high risk mainly due having a the different reference standard. In these studies, patients with positive SLN would undergo a comprehensive neck dissection and pathology results of cervical lymph nodes were the "gold standard" however SLN-negative patients would not undergo neck dissection and clinical follow-up was the "gold standard". There was less concern about the applicability of the studies. In 5 (7.6%) studies, there were concerns about applicability because of patient selection, in 3 (4.5%) studies because of the index test and in1 (1.5%) study because of the reference test.
Fig 2. Results of QUADAS-2, Risk of bias and concerns regarding applicability.
Diagnostic accuracy
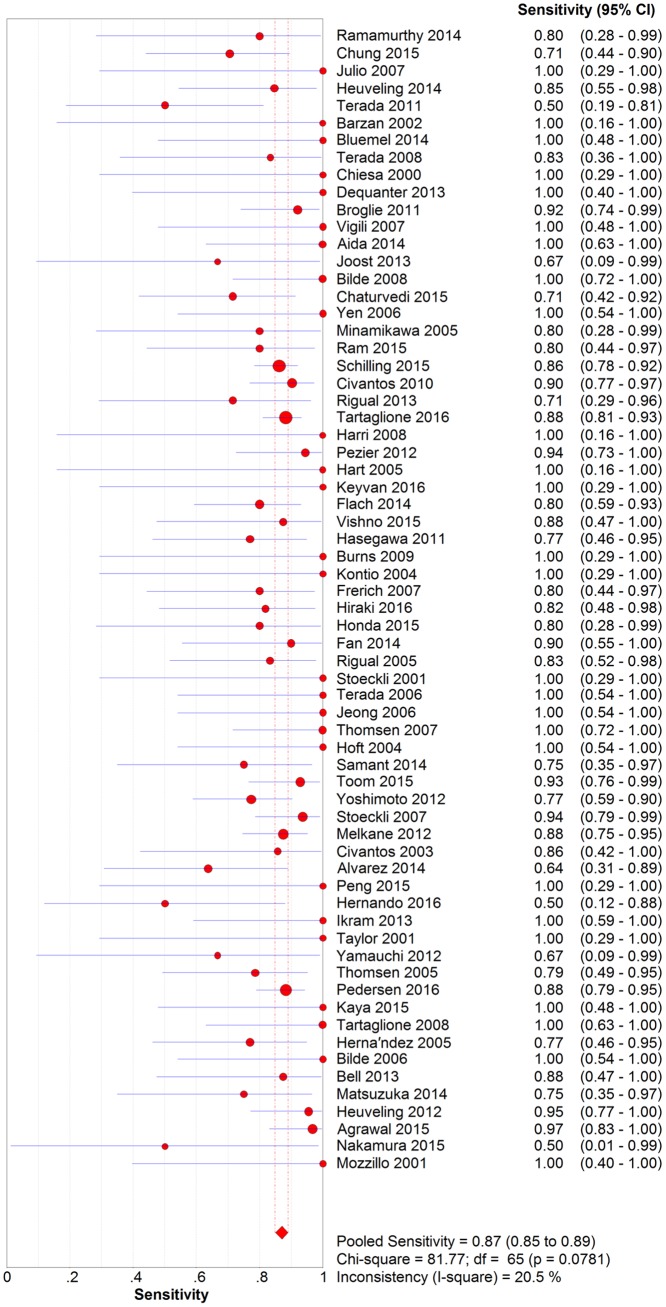
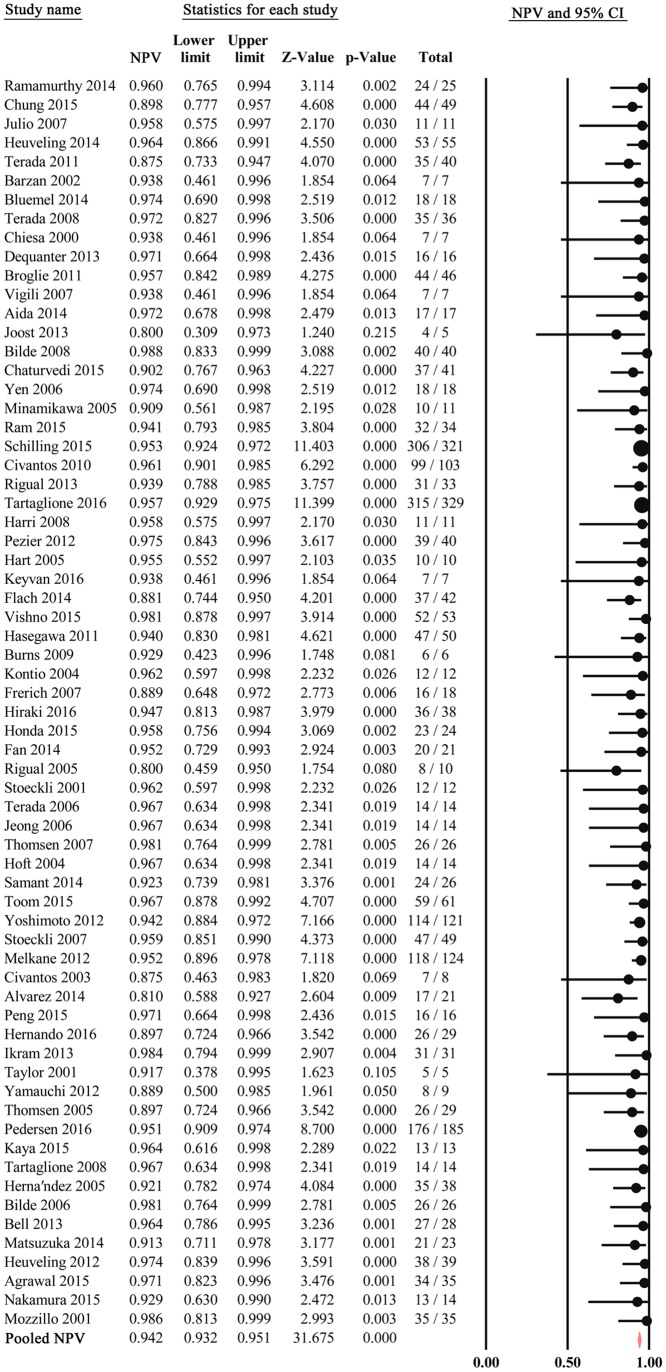
Analysis of diagnostic threshold showed that the spearman correlation coefficient was -0.037 with a p-value of 0.769. Forest plots of data from the 66 studies on the sensitivity and negative predictive value of SLNB are shown in Figs 3 and 4, respectively. Since no significant heterogeneity were found between studies in sensitivity and negative predictive value data (I2 = 20.5% and I2 = 0.0, respectively), the fixed effects model was used to calculate the pool estimates in this study. In the present analysis, the pooled SLN identification rate, pooled sensitivity and negative predictive value were 96.3%(95% CI: 95.3%-97.0%), 0.87 (95% CI: 0.85–0.89) and 0.94 (95% CI: 0.93–0.95), respectively. Fig 5 shows the corresponding overall SROC curve with an AUC of 0.98 (95% CI: 0.97–0.99). In order to view the greater effect of different study characteristics on the diagnostic efficacy of SLN, subgroup analysis was conducted.
Fig 3. Forest plot of pooled sensitivity.
Fig 4. Forest plot of pooled negative predictive value.
Fig 5. SROC curve.
Subgroup analysis
We conducted subgroup analysis by the average of SLNs harvested (low: <2, medium: 2≤ and <3 or high: ≥3), SLN pathology methods(IHC or not, SS or not), type of reference test (neck dissection or follow-up), SLN tracer (single tracer or multiple tracers), study design (prospective or retrospective) and publication year (early: 2000–2008 or late: 2009–2016). The pooled sensitivity, negative predictive value and AUC for each subgroup are listed in Table 2.
Table 2. Summary of subgroup analysis by different clinical characteristics.
| Subgroup | Study (n) | Sensitivity [95% CIs] | NPV [95% CIs] | AUC [95% CIs] |
|---|---|---|---|---|
| IHC | ||||
| No | 12 | 0.77 [0.68–0.85] | 0.91[0.87–0.94] | 0.97[0.95–0.99] |
| Yes | 41 | 0.88 [0.86–0.90] | 0.95[0.94–0.96] | 0.98[0.97–0.99] |
| SS | ||||
| No | 21 | 0.88[0.84–0.91] | 0.93[0.91–0.95] | 0.96[0.93–0.99] |
| Yes | 32 | 0.87[0.84–0.90] | 0.94[0.93–0.95] | 0.98[0.97–0.99] |
| Average SLNs | ||||
| Low (N<2) | 4 | 0.84 [0.60–0.97] | 0.94[0.83–0.98] | 0.90[0.75–1.00] |
| Medium(2≤N<3) | 18 | 0.86 [0.81–0.90] | 0.95[0.93–0.96] | 0.98[0.97–1.00] |
| High(N≥3) | 16 | 0.88 [0.86–0.92] | 0.95[0.94–0.97] | 0.98[0.97–0.99] |
| Publication Year | ||||
| Early(2000–2008) | 26 | 0.92 [0.87–0.95] | 0.94[0.91–0.96] | 0.98[0.97–0.99] |
| Late(2009–2016) | 40 | 0.86 [0.83–0.88] | 0.94[0.93–0.95] | 0.98[0.96–0.99] |
| SLN Tracer | ||||
| Single | 43 | 0.87 [0.84–0.90] | 0.94[0.93–0.95] | 0.98[0.97–0.99] |
| Multiple | 23 | 0.87 [0.84–0.90] | 0.94[0.93–0.96] | 0.96[0.93–0.99] |
| Study Design | ||||
| Prospective | 56 | 0.87 [0.85–0.90] | 0.94[0.93–0.95] | 0.98[0.97–0.99] |
| Retrospective | 10 | 0.86 [0.81–0.91] | 0.95[0.93–0.96] | 0.97[0.92–1.00] |
| Reference Test | ||||
| ND | 32 | 0.90 [0.87–0.93] | 0.95[0.94–0.96] | 0.97[0.95–0.98] |
| FU | 34 | 0.85 [0.82–0.88] | 0.94[0.92–0.95] | 0.98[0.97–0.99] |
ND: neck dissection; FU: follow-up; IHC: immunohistochemistry; SS: Serial sectioning; NPV: negative predictive value.
For subgroup analyses conducted by the average of SLNs harvested, SLN tracer, study design and serial sectioning, no significant difference could be found among these groups. However, subgroup analysis based on immunohistochemistry(IHC) indicated that H&E combined with IHC was significantly more sensitive than single H&E staining with a sensitivity of 0.88(95%CI: 0.86–0.90) versus 0.77(95%CI: 0.68–0.85). Moreover, early publication subgroup and neck dissection subgroup yielded a better pooled sensitivity than late publication subgroup and clinical follow-up subgroup(0.92[0.87–0.95] vs. 0.86[0.83–0.88] and 0.90[0.87–0.93] vs. 0.85[0.82–0.88], respectively).
Sensitivity analysis and publication bias
We performed sensitivity analyses to assess the credibility and consistency of the results through: (1)Omitting studies one by one. In the current meta analysis, with removal of any single study the pooled findings were essentially unchanged. (2) When switched the fixed-effects model to random-effects model, the pooled findings didn't change significantly. The sensitivity analyses supported the result was robustness.
In order to evaluate potential publication bias, the Deeks' funnel plot asymmetry test was used. The slope coefficient was associated with a P value of 0.00 (Fig 6), revealed a likelihood of publication bias.
Fig 6. Deeks' funnel plot with regression line.
Discussion
To our knowledge, this is the largest meta-analysis focused on the diagnostic efficacy of sentinel lymph node biopsy in early oral squamous cell carcinoma. In this meta-analysis of 66 studies comprising more than 3500 patients, SLNB yielded a pooled identification rate of 96.3%(95% CI: 95.3%-97.0%), a pooled sensitivity of 0.87(95%CI: 0.85–0.89), a pooled negative predictive value of 0.94 (95% CI: 0.93–0.95) and an AUC of 0.98 (95% CI: 0.97–0.99). The high pooled negative predictive value implied that only 6% of SLN-negative early oral cavity cancer patients would result in a false-negative regional recurrence during follow-up. This is similar to the regional recurrence rate after elective neck dissection in clinically neck-negative early OSCC reported by previous literature [80], and is far lower than the acceptable threshold of 20% cervical lymph node metastasis rate for prophylactic neck dissection. Therefore, elective neck dissection could be omitted in SLN-negative early OSCC patients. Moreover, the pooled sensitivity implies that 87% of occult cervical lymph node metastases could be diagnosed by SLNB and the false-negative rate is 13%. The occult lymph node metastasis rate has been reported to be 20%-30% for cT1-2N0 OSCC [2–4]. Therefore, we can estimate that SLNB applied to all early OSCC patients would result in a 2.6%-3.9% regional recurrence rate. This regional recurrence rate is acceptable when considering the serious complications and 70% overtreatment rate in traditional prophylactic neck dissection procedure. Overall, these pooled findings indicated that SLNB had an ideal diagnostic accuracy for predicting occult cervical lymph node metastases in early oral cancer patients and was an ideal alternative to neck dissection. In the previous meta-analyses focusing on the diagnostic efficacy of SLNB in head and neck cancer or oral/oropharyngeal cancer, Tim reported a pooled sensitivity of 0.92 (95%CI: 0.86–0.95) in oral cancer subgroup(n = 508), while Thompson reported a pooled sensitivity and negative predictive value of 0.94 (95%CI: 0.89–0.98) and 0.96 (95%CI: 0.93–0.99) respectively in the subset of oral cavity tumors(n = 631) [14, 15]. Compared to these previous meta-analyses, our research found a lower sensitivity of 0.87(95%CI: 0.85–0.89)(n = 3506). Since those two meta-analyses were published many years ago, we further stratified our results by publication year and found that the pooled sensitivity of early publications(2000–2008) in current meta-analysis was 0.92(95%CI: 0.87–0.95), more similar to the results reported by previous meta-analyses, and better than late publications(2009–2016). A possible reason for this difference may be that SLNB researches in early publications were still during the validation stage, and elective neck dissection of levels I-III was the gold standard for SLN-negative cases in most of these publications(69.2%, 18/26). But in more recent publications, most SLNB research studies use clinical follow-up as their gold standard for SLN-negative cases and only 35%(14/40) of studies were still using elective neck dissection(levels I-III) as their gold standard. Thus, we speculate that: (1) there may have occult lymph node metastases in level IV, level V or even contralateral neck that would be missed by the elective neck dissections in most of the earlier publications, resulting in an overestimated sensitivity; (2) SLNB with neck dissection is definitely easier than SLNB without neck dissection and this may also lead to a higher pooled sensitivity in the validation stage.
Based on our subgroup analyses, we found that SLNB with IHC yielded significantly better sensitivity than the no IHC subgroup. The pooled sensitivity was 0.88(95%CI: 0.86–0.90) in IHC subgroup but only 0.77(95%CI: 0.68–0.85) in the no IHC subgroup. These results indicated that application of IHC associated with a 11% relative increase in sensitivity. Based on this result, we strongly recommend that IHC should be performed for SLN pathologic analysis. By contrast, no significant difference could be found between serial sectioning subgroup and no serial sectioning subgroup. The pooled sensitivity was 0.88(95%CI: 0.84–0.91) and 0.87(95%CI: 0.84–0.90), respectively. A prospective study conducted by Bell demonstrated that SLNB performed with the use of routine H&E staining and IHC could accurately predict neck stage in early oral squamous cell carcinoma with a negative predictive value of 96% and that serial sectioning might not be necessary [75]. Meanwhile, routine serial sectioning was also deemed not feasible or practical to make a quick diagnosis for SLN during frozen section. In the current meta-analysis, our results confirmed Bell's conclusion.
Several limitations should be considered while interpreting our results. First, although we tried to incorporate all relevant studies, the Deeks' funnel plot still revealed a likelihood of publication bias. It is possible that we may have missed some eligible studies in our screening process. There may also have been small trials with opposite results that were never published. Second, quality assessment showed that there was high risk of bias in flow and timing because not all patients received the same reference standard. This bias might restrict interpretation of the true diagnostic efficacy of SLNB. Third, in almost all of the included studies, the SLNs were assessed by postoperative pathological procedure but not by frozen section. This might result in overestimating the practical clinical applicability of SLNB. Nevertheless, this didn't affect the validity of our pooled findings. Finally, similar to other meta-analyses, we included studies with different characteristics and designs. Nevertheless, the heterogeneity test and sensitivity analyses proved our pooled findings to be credible and consistent. Notwithstanding the limitations listed above, our meta-analysis also has its strengths: (1) this is the largest meta-analysis of the diagnostic efficacy of SLNB specifically focused on early oral squamous cell carcinoma; (2) by dividing studies into two subgroups based on the use of IHC, we confirmed that SLN assessment with IHC achieved a significantly higher sensitivity than without IHC; (3) Moreover, serial sectioning does not seem necessary for SLN assessment.
Conclusions
Our results confirmed that SLNB had a high diagnostic accuracy in cT1-2N0 oral squamous cell carcinoma, and was an ideal alternative to elective neck dissection. We also found that H&E with IHC yielded much better diagnostic sensitivity than H&E alone. However, further clinical trials are required to verify the clinical utility and application of SLNB by frozen section but not by postoperative pathological assessment. In particular, further studies on the diagnostic accuracy of automated quantitative real-time PCR (qRT-PCR) assay for intra-operative SLN frozen section are required [81, 82].
Supporting Information
(DOCX)
(TIF)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.De Zinis LO, Bolzoni A, Piazza C, Nicolai P. Prevalence and localization of nodal metastases in squamous cell carcinoma of the oral cavity: role and extension of neck dissection. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology—Head and Neck Surgery. 2006;263(12):1131–5. Epub 2006/09/28. [DOI] [PubMed] [Google Scholar]
- 2.Pillsbury HC 3rd, Clark M. A rationale for therapy of the N0 neck. The Laryngoscope. 1997;107(10):1294–315. [DOI] [PubMed] [Google Scholar]
- 3.Braams JW, Pruim J, Freling NJ, Nikkels PG, Roodenburg JL, Boering G, et al. Detection of lymph node metastases of squamous-cell cancer of the head and neck with FDG-PET and MRI. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 1995;36(2):211–6. [PubMed] [Google Scholar]
- 4.Ross GL, Soutar DS, MacDonald DG, Shoaib T, Camilleri IG, Robertson AG. Improved staging of cervical Metastases in clinically node-negative patients with head and neck squamous cell carcinoma. Annals of surgical oncology. 2004;11(2):213–8. [DOI] [PubMed] [Google Scholar]
- 5.van der Vorst JR, Schaafsma BE, Verbeek FPR, Keereweer S, Jansen JC, van der Velden LA, et al. Near-infrared fluorescence sentinel lymph node mapping of the oral cavity in head and neck cancer patients. Oral oncology. 2013;49(1):15–9. 10.1016/j.oraloncology.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernando J, Villarreal P, Alvarez-Marcos F, Gallego L, Garcia-Consuegra L, Junquera L. Comparison of related complications: sentinel node biopsy versus elective neck dissection. International journal of oral and maxillofacial surgery. 2014;43(11):1307–12. 10.1016/j.ijom.2014.07.016 [DOI] [PubMed] [Google Scholar]
- 7.Schiefke F, Akdemir M, Weber A, Akdemir D, Singer S, Frerich B. Function, Postoperative Morbidity, and Quality of Life after Cervical Sentinel Node Biopsy and after Selective Neck Dissection. Head Neck-J Sci Spec Head Neck. 2009;31(4):503–12. [DOI] [PubMed] [Google Scholar]
- 8.Govers TM, Schreuder WH, Klop WMC, Grutters JPC, Rovers MM, Merkx MAW, et al. Quality of life after different procedures for regional control in oral cancer patients: cross-sectional survey. Clin Otolaryngol. 2016;41(3):228–33. 10.1111/coa.12502 [DOI] [PubMed] [Google Scholar]
- 9.Govers TM, Takes RP, Baris Karakullukcu M, Hannink G, Merkx MA, Grutters JP, et al. Management of the N0 neck in early stage oral squamous cell cancer: a modeling study of the cost-effectiveness. Oral oncology. 2013;49(8):771–7. Epub 2013/06/06. 10.1016/j.oraloncology.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 10.Dequanter D, Shahla M, Paulus P, Lothaire P. Long term results of sentinel lymph node biopsy in early oral squamous cell carcinoma. OncoTargets and therapy. 2013;6:799–802. 10.2147/OTT.S43446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pedersen NJ, Jensen DH, Hedback N, Frendo M, Kiss K, Lelkaitis G, et al. Staging of early lymph node metastases with the sentinel lymph node technique and predictive factors in T1/T2 oral cavity cancer: A retrospective single-center study. Head Neck-J Sci Spec Head Neck. 2016;38:E1033–E40. [DOI] [PubMed] [Google Scholar]
- 12.Chiesa F, Mauri S, Grana C, Tradati N, Calabrese L, Ansarin M, et al. Is there a role for sentinel node biopsy in early N0 tongue tumors? Surgery. 2000;128(1):16–21. 10.1067/msy.2000.106809 [DOI] [PubMed] [Google Scholar]
- 13.Yamauchi K, Kogashiwa Y, Nakamura T, Moro Y, Nagafuji H, Kohno N. Diagnostic evaluation of sentinel lymph node biopsy in early head and neck squamous cell carcinoma: A meta-analysis. Head Neck-J Sci Spec Head Neck. 2015;37(1):127–33. [DOI] [PubMed] [Google Scholar]
- 14.Thompson CF, St John MA, Lawson G, Grogan T, Elashoff D, Mendelsohn AH. Diagnostic value of sentinel lymph node biopsy in head and neck cancer: a meta-analysis. Eur Arch Oto-Rhino-Laryn. 2013;270(7):2115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Govers TM, Hannink G, Merkx MAW, Takes RP, Rovers MM. Sentinel node biopsy for squamous cell carcinoma of the oral cavity and oropharynx: A diagnostic meta-analysis. Oral oncology. 2013;49(8):726–32. 10.1016/j.oraloncology.2013.04.006 [DOI] [PubMed] [Google Scholar]
- 16.Paleri V, Rees G, Arullendran P, Shoalb T, Krishman S. Sentinel node biopsy in squamous cell cancer of the oral cavity and oral pharynx: A diagnostic meta-analysis. Head Neck-J Sci Spec Head Neck. 2005;27(9):739–47. [DOI] [PubMed] [Google Scholar]
- 17.Schilling C, Stoeckli SJ, Haerle SK, Broglie MA, Huber GF, Sorensen JA, et al. Sentinel European Node Trial (SENT): 3-year results of sentinel node biopsy in oral cancer. Eur J Cancer. 2015;51(18):2777–84. 10.1016/j.ejca.2015.08.023 [DOI] [PubMed] [Google Scholar]
- 18.Den Toom IJ, Heuveling DA, Flach GB, van Weert S, Karagozoglu KH, van Schie A, et al. Sentinel node biopsy for early-stage oral cavity cancer: the VU University Medical Center experience. Head Neck-J Sci Spec Head Neck. 2015;37(4):573–8. [DOI] [PubMed] [Google Scholar]
- 19.Agrawal A, Civantos FJ, Brumund KT, Chepeha DB, Hall NC, Carroll WR, et al. [Tc-99m]Tilmanocept Accurately Detects Sentinel Lymph Nodes and Predicts Node Pathology Status in Patients with Oral Squamous Cell Carcinoma of the Head and Neck: Results of a Phase III Multi-institutional Trial. Annals of surgical oncology. 2015;22(11):3708–15. 10.1245/s10434-015-4382-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of internal medicine. 2011;155(8):529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 21.Ramamurthy R, Kottayasamy Seenivasagam R, Shanmugam S, Palanivelu K. A prospective study on sentinel lymph node biopsy in early oral cancers using methylene blue dye alone. Indian journal of surgical oncology. 2014;5(3):178–83. Epub 2014/11/25. 10.1007/s13193-014-0337-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung MK, Lee GJ, Choi N, Cho JK, Jeong HS, Baek CH. Comparative study of sentinel lymph node biopsy in clinically N0 oral tongue squamous cell carcinoma: Long-term oncologic outcomes between validation and application phases. Oral oncology. 2015;51(10):914–20 10.1016/j.oraloncology.2015.07.007 [DOI] [PubMed] [Google Scholar]
- 23.Alvarez Amezaga J, Barbier Herrero L, Pijoan del Barrio JI, Martin Rodriguez JC, Romo Simon L, Genolla Subirats J, et al. Diagnostic efficacy of sentinel node biopsy in oral squamous cell carcinoma. Cohort study and meta-analysis. Medicina oral, patologia oral y cirugia bucal. 2007;12(3):E235–43. Epub 2007/05/01. [PubMed] [Google Scholar]
- 24.Heuveling DA, van Weert S, Karagozoglu KH, de Bree R. Evaluation of the use of freehand SPECT for sentinel node biopsy in early stage oral carcinoma. Oral oncology. 2015;51(3):287–90. 10.1016/j.oraloncology.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 25.Terada A, Hasegawa Y, Yatabe Y, Hanai N, Ozawa T, Hirakawa H, et al. Follow-up after intraoperative sentinel node biopsy of N0 neck oral cancer patients. Eur Arch Oto-Rhino-Laryn. 2011;268(3):429–35. [DOI] [PubMed] [Google Scholar]
- 26.Barzan L, Sulfaro S, Alberti F, Politi D, Marus W, Pin M, et al. Gamma probe accuracy in detecting the sentinel lymph node in clinically no squamous cell carcinoma of the head and neck. Ann Otol Rhinol Laryngol. 2002;111(9):794–8. [DOI] [PubMed] [Google Scholar]
- 27.Bluemel C, Herrmann K, Kubler A, Buck AK, Geissinger E, Wild V, et al. Intraoperative 3-D imaging improves sentinel lymph node biopsy in oral cancer. European journal of nuclear medicine and molecular imaging. 2014;41(12):2257–64. 10.1007/s00259-014-2870-z [DOI] [PubMed] [Google Scholar]
- 28.Terada A, Hasegawa Y, Yatabe Y, Hyodo I, Ogawa T, Hanai N, et al. Intraoperative diagnosis of cancer metastasis in sentinel lymph node of oral cancer patients. Oral oncology. 2008;44(9):838–43. 10.1016/j.oraloncology.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 29.Pattani KM, Califano J. Long-Term Experience in Sentinel Node Biopsy for Early Oral and Oropharyngeal Squamous Cell Carcinoma. Annals of surgical oncology. 2011;18(10):2709–10. 10.1245/s10434-011-1785-1 [DOI] [PubMed] [Google Scholar]
- 30.Vigili MG, Tartaglione G, Rahimi S, Mafera B, Pagan M. Lymphoscintigraphy and radioguided sentinel node biopsy in oral cavity squamous cell carcinoma: same day protocol. Eur Arch Oto-Rhino-Laryn. 2007;264(2):163–7. [DOI] [PubMed] [Google Scholar]
- 31.Sabate-Llobera A, Benitez-Segura A, Mari A, Arranz C, Bajen MT, Maymo-Garrido S, et al. Lymphoscintigraphy in Oral Squamous Cell Carcinoma Sentinel Node Biopsy and Its Role in the Surgical Planning. Clinical nuclear medicine. 2014;39(2):E142–E5. [DOI] [PubMed] [Google Scholar]
- 32.Bilde A, von Buchwald C, Therkildsen MH. Need for Intensive Histopathologic Analysis to Determine Lymph Node Metastases When Using Sentinel Node Biopsy in Oral Cancer (vol 118, pg 408, 2008). The Laryngoscope. 2008;118(4):760-. [DOI] [PubMed] [Google Scholar]
- 33.Chaturvedi P, Datta S, Arya S, Rangarajan V, Kane SV, Nair D, et al. Prospective study of ultrasound-guided fine-needle aspiration cytology and sentinel node biopsy in the staging of clinically negative T1 and T2 oral cancer. Head Neck-J Sci Spec Head Neck. 2015;37(10):1504–8. [DOI] [PubMed] [Google Scholar]
- 34.Yen CY, Lee SY, Hsieh JF, Wang DZ, Lin GN, Tsai CM, et al. Radiolocalized sentinel lymph node biopsy in squamous cell carcinoma of the oral cavity and analysis of various parameters. Annals of surgical oncology. 2006;13(8):1130–5. 10.1245/ASO.2006.09.023 [DOI] [PubMed] [Google Scholar]
- 35.Minamikawa T, Umeda M, Komori T. Reliability of sentinel lymph node biopsy with squamous cell carcinoma of the oral cavity. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics. 2005;99(5):532–8. [DOI] [PubMed] [Google Scholar]
- 36.Sieira-Gil R, Paredes P, Marti-Pages C, Ferrer-Fuertes A, Garcia-Diez E, Cho-Lee GY, et al. SPECT-CT and intraoperative portable gamma-camera detection protocol for sentinel lymph node biopsy in oral cavity squamous cell carcinoma. J Cranio-MaxilloFac Surg. 2015;43(10):2205–13. [DOI] [PubMed] [Google Scholar]
- 37.Civantos FJ, Zitsch RP, Schuller DE, Agrawal A, Smith RB, Nason R, et al. Sentinel Lymph Node Biopsy Accurately Stages the Regional Lymph Nodes for T1-T2 Oral Squamous Cell Carcinomas: Results of a Prospective Multi-Institutional Trial. J Clin Oncol. 2010;28(8):1395–400. 10.1200/JCO.2008.20.8777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rigual N, Loree T, Frustino J, Jayaprakash V, Cohan D, Sullivan M, et al. Sentinel Node Biopsy in Lieu of Neck Dissection for Staging Oral Cancer. JAMA Otolaryngol-Head Neck Surg. 2013;139(8):779–82 10.1001/jamaoto.2013.3863 [DOI] [PubMed] [Google Scholar]
- 39.Tartaglione G, Stoeckli SJ, de Bree R, Schilling C, Flach GB, Bakholdt V, et al. Sentinel Node in Oral Cancer The Nuclear Medicine Aspects. A Survey from the Sentinel European Node Trial. Clinical nuclear medicine. 2016;41(7):534–42. [DOI] [PubMed] [Google Scholar]
- 40.Keski-Santti H, Kontio R, Leivo I, Tornwall J, Matzke S, Makitie AA, et al. Sentinel lymph node biopsy as an alternative to wait and see policy in patients with small T1 oral cavity squamous cell carcinoma. Acta oto-laryngologica. 2008;128(1):98–102. 10.1080/00016480701362002 [DOI] [PubMed] [Google Scholar]
- 41.Pezier T, Nixon IJ, Gurney B, Schilling C, Hussain K, Lyons AJ, et al. Sentinel Lymph Node Biopsy for T1/T2 Oral Cavity Squamous Cell Carcinoma-A Prospective Case Series. Annals of surgical oncology. 2012;19(11):3528–33. 10.1245/s10434-011-2207-0 [DOI] [PubMed] [Google Scholar]
- 42.Hart RD, Nasser JG, Trites JR, Taylor SM, Bullock MT, Barnes D. Sentinel lymph node biopsy in N0 squamous cell carcinoma of the oral cavity and oropharynx. Arch Otolaryngol Head Neck Surg. 2005;131(1):34–8. 10.1001/archotol.131.1.34 [DOI] [PubMed] [Google Scholar]
- 43.Sagheb K, Sagheb K, Rahimi-Nedjat R, Taylor K, Al-Nawas B, Walter C. Sentinel lymph node biopsy in T1/T2 squamous cell carcinomas of the tongue: A prospective study. Oncology letters. 2016;11(1):600–4. 10.3892/ol.2015.3933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Flach GB, Bloemena E, Klop WMC, van Es RJJ, Schepman KP, Hoekstra OS, et al. Sentinel lymph node biopsy in clinically N0 T1-T2 staged oral cancer: The Dutch multicenter trial. Oral oncology. 2014;50(10):1020–4. 10.1016/j.oraloncology.2014.07.020 [DOI] [PubMed] [Google Scholar]
- 45.Vishnoi JR, Kumar V, Gupta S, Agrawal P, Jamal N, Misra S, et al. Sentinel lymph node biopsy in early oral cancer using methylene blue dye alone: A tertiary care cancer centre experience from india. Eur J Cancer. 2015;51:S573–S4. [Google Scholar]
- 46.Hasegawa Y, Terada A, Yatabe Y, Hanai N, Ozawa T, Hirakawa H. Sentinel lymph node biopsy in early tongue cancer patients. Oral oncology. 2011;47:S16–S. [DOI] [PubMed] [Google Scholar]
- 47.Burns P, Foster A, Walshe P, O'Dwyer T. Sentinel lymph node biopsy in node-negative squamous cell carcinoma of the oral cavity and oropharynx. J Laryngol Otol. 2009;123(4):439–43. 10.1017/S0022215108003514 [DOI] [PubMed] [Google Scholar]
- 48.Kontio R, Leivo I, Leppanen E, Atula T. Sentinel lymph node biopsy in oral cavity squamous cell carcinoma without clinically evident metastasis. Head Neck-J Sci Spec Head Neck. 2004;26(1):16–21. [DOI] [PubMed] [Google Scholar]
- 49.Frerich B, Foerster M, Schiefke F, Wittekind C, Hemprich A, Sabri O. Sentinel lymph node biopsy in squamous cell carcinomas of the lips and the oral cavity—A single center experience. Journal of surgical oncology. 2007;95(2):97–105. 10.1002/jso.20664 [DOI] [PubMed] [Google Scholar]
- 50.Hiraki A, Fukuma D, Nagata M, Shiraishi S, Kawahara K, Matsuoka Y, et al. Sentinel lymph node biopsy reduces the incidence of secondary neck metastasis in patients with oral squamous cell carcinoma. Molecular and clinical oncology. 2016;5(1):57–60. Epub 2016/06/23. 10.3892/mco.2016.882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Honda K, Ishiyama K, Suzuki S, Oumi E, Sato T, Kawasaki Y, et al. Sentinel lymph node biopsy using computed tomographic lymphography in patients with early tongue cancer. Acta oto-laryngologica. 2015;135(5):507–12. 10.3109/00016489.2015.1010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fan SF, Zeng ZY, Peng HW, Guo ZM, Wang SL, Zhang Q. Sentinel lymph node biopsy versus elective neck dissection in patients with cT1-2N0 oral tongue squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(2):186–90. 10.1016/j.oooo.2013.09.012 [DOI] [PubMed] [Google Scholar]
- 53.Rigual N, Douglas W, Lamonica D, Wiseman S, Cheney R, Hicks W, et al. Sentinel lymph node biopsy: A rational approach for staging T2N0 oral cancer. The Laryngoscope. 2005;115(12):2217–20. 10.1097/01.mlg.0000187870.82699.ed [DOI] [PubMed] [Google Scholar]
- 54.Stoeckli SJ, Steinert H, Pfaltz M, Schmid S. Sentinel lymph node evaluation in squamous cell carcinoma of the head and neck. Otolaryngology—head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2001;125(3):221–6. Epub 2001/09/14. [DOI] [PubMed] [Google Scholar]
- 55.Terada A, Hasegawa Y, Goto M, Sato E, Hyodo I, Ogawa T, et al. Sentinel lymph node radiolocalization in clinically negative neck oral cancer. Head & neck. 2006;28(2):114–20. Epub 2005/09/13. [DOI] [PubMed] [Google Scholar]
- 56.Jeong HS, Baek CH, Son YL, Cho DY, Chung MK, Min JY, et al. Sentinel lymph node radiolocalization with Tc-99m filtered tin colloid in clinically node-negative squamous cell carcinomas of the oral cavity. Journal of Korean medical science. 2006;21(5):865–70. 10.3346/jkms.2006.21.5.865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomsen JB, Christensen RK, Sorensen JA, Krogdahl A. Sentinel lymph nodes in cancer of the oral cavity: is central step-sectioning enough? J Oral Pathol Med. 2007;36(7):425–9. 10.1111/j.1600-0714.2007.00538.x [DOI] [PubMed] [Google Scholar]
- 58.Hoft S, Maune S, Muhle C, Brenner W, Czech N, Kampen WU, et al. Sentinel lymph-node biopsy in head and neck cancer. British journal of cancer. 2004;91(1):124–8. 10.1038/sj.bjc.6601877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Samant S. Sentinel node biopsy as an alternative to elective neck dissection for staging of early oral carcinoma. Head Neck-J Sci Spec Head Neck. 2014;36(2):241–6. [DOI] [PubMed] [Google Scholar]
- 60.Yoshimoto S, Hasegawa Y, Matsuzuka T, Shiotani A, Takahashi K, Kohno N, et al. Sentinel node biopsy for oral and laryngopharyngeal squamous cell carcinoma: A retrospective study of 177 patients in Japan. Auris, nasus, larynx. 2012;39(1):65–70. 10.1016/j.anl.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 61.Stoeckh SJ. Sentinel node biopsy for oral and oropharyngeal squamous cell carcinoma of the head and neck. The Laryngoscope. 2007;117(9):1539–51. 10.1097/MLG.0b013e318093ee67 [DOI] [PubMed] [Google Scholar]
- 62.Melkane AE, Mamelle G, Wycisk G, Temam S, Janot F, Casiraghi O, et al. Sentinel node biopsy in early oral squamous cell carcinomas: A 10-year experience. The Laryngoscope. 2012;122(8):1782–8. 10.1002/lary.23383 [DOI] [PubMed] [Google Scholar]
- 63.Civantos FJ, Gomez C, Duque C, Pedroso F, Goodwin WJ, Weed DT, et al. Sentinel node biopsy in oral cavity cancer: Correlation with PET scan and immunohistochemistry. Head Neck-J Sci Spec Head Neck. 2003;25(1):1–9. [DOI] [PubMed] [Google Scholar]
- 64.Alvarez J, Bidaguren A, McGurk M, Diaz-Basterra G, Brunso J, Andikoetxea B, et al. Sentinel node biopsy in relation to survival in floor of the mouth carcinoma. International journal of oral and maxillofacial surgery. 2014;43(3):269–73. 10.1016/j.ijom.2013.10.022 [DOI] [PubMed] [Google Scholar]
- 65.Peng HW, Wang SJ, Niu XH, Yang XH, Chi CW, Zhang GJ. Sentinel node biopsy using indocyanine green in oral/oropharyngeal cancer. World journal of surgical oncology. 2015;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hernando J, Villarreal P, Alvarez-Marcos F, Garcia-Consuegra L, Gallego L, Junquera L. Sentinel node biopsy versus elective neck dissection. Which is more cost-effective? A prospective observational study. J Cranio-MaxilloFac Surg. 2016;44(5):550–6. [DOI] [PubMed] [Google Scholar]
- 67.Ikram M, Akhtar S, Maseeh uz Z, Junaid M, Dhari T, Ahmad Z, et al. Sentinel node localisation using pre-operative lymphoscintigraphy and intraoperative gamma probe in early oral cavity cancer. J Pak Med Assoc. 2013;63(8):976–9. [Google Scholar]
- 68.Taylor RJ, Wahl RL, Sharma PK, Bradford CR, Terrell JE, Teknos TN, et al. Sentinel node localization in oral cavity and oropharynx squamous cell cancer. Arch Otolaryngol Head Neck Surg. 2001;127(8):970–4. [DOI] [PubMed] [Google Scholar]
- 69.Yamauchi K, Fujioka Y, Kohno N. Sentinel node navigation surgery versus observation as a management strategy for early tongue carcinoma. Head Neck-J Sci Spec Head Neck. 2012;34(4):568–72. [DOI] [PubMed] [Google Scholar]
- 70.Thomsen JB, Sorensen JA, Grupe P, Karstoft J, Krogdahl A. Staging N0 oral cancer: Lymphoscintigraphy and conventional imaging. Acta Radiol. 2005;46(5):492–6. [DOI] [PubMed] [Google Scholar]
- 71.Kaya I, Gode S, Ozturk K, Turhal G, Aliyev A, Akyildiz S, et al. The Value of Sentinel Lymph Node Biopsy in Oral Cavity Cancers. Turk Arch Otorhinolaryn. 2015;53(2):62–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tartaglione G, Vigili MG, Rahimi S, Celebrini A, Pagan M, Lauro L, et al. The impact of superficial injections of radiocolloids and dynamic lymphoscintigraphy on sentinel node identification in oral cavity cancer: a same-day protocol. Nuclear medicine communications. 2008;29(4):318–22. [DOI] [PubMed] [Google Scholar]
- 73.Gallegos-Hernandez JF, Hernandez-Hernandez DM, Flores-Diaz R, Sierra-Santiesteban I, Pichardo-Romero P, Arias-Ceballos H, et al. The number of sentinel nodes identified as prognostic factor in oral epidermoid cancer. Oral oncology. 2005;41(9):947–52. 10.1016/j.oraloncology.2005.05.010 [DOI] [PubMed] [Google Scholar]
- 74.Bilde A, Von Buchwald C, Mortensen J, Marving J, Therkildsen MH, Kirkegaard J, et al. The role of SPECT-CT in the lymphoscintigraphic identification of sentinel nodes in patients with oral cancer. Acta oto-laryngologica. 2006;126(10):1096–103. 10.1080/00016480600794453 [DOI] [PubMed] [Google Scholar]
- 75.Bell RB, Markiewicz MR, Dierks EJ, Gregoire CE, Rader A. Thin Serial Step Sectioning of Sentinel Lymph Node Biopsy Specimen May Not Be Necessary to Accurately Stage the Neck in Oral Squamous Cell Carcinoma. J Oral Maxillofac Surg. 2013;71(7):1268–77. 10.1016/j.joms.2012.12.019 [DOI] [PubMed] [Google Scholar]
- 76.Matsuzuka T, Suzuki M, Saijo S, Matsui T, Nomoto Y, Ikeda M, et al. Usefulness of sentinel node navigation surgery in the management of early tongue cancer. Auris, nasus, larynx. 2014;41(5):475–8. 10.1016/j.anl.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 77.Heuveling DA, Flach GB, van Schie A, van Weert S, Karagozoglu KH, Bloemena E, et al. Visualization of the sentinel node in early-stage oral cancer: limited value of late static lymphoscintigraphy. Nuclear medicine communications. 2012;33(10):1065–9. [DOI] [PubMed] [Google Scholar]
- 78.Nakamura T, Kogashiwa Y, Nagafuji H, Yamauchi K, Kohno N. Validity of Sentinel Lymph Node Biopsy by ICG Fluorescence for Early Head and Neck Cancer. Anticancer research. 2015;35(3):1669–74. [PubMed] [Google Scholar]
- 79.Mozzillo N, Chiesa F, Botti G, Caraco C, Lastoria S, Giugliano G, et al. Sentinel node biopsy in head and neck cancer. Annals of surgical oncology. 2001;8(9 Suppl):103s–5s. Epub 2001/10/16. [PubMed] [Google Scholar]
- 80.Yeh CF, Li WY, Yang MH, Chu PY, Lu YT, Wang YF, et al. Neck observation is appropriate in T1-2, cN0 oral squamous cell carcinoma without perineural invasion or lymphovascular invasion. Oral oncology. 2014;50(9):857–62. Epub 2014/07/08. 10.1016/j.oraloncology.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 81.Ferris RL, Stefanika P, Xi LQ, Gooding W, Seethala RR, Godfrey TE. Rapid molecular detection of metastatic head and neck squamous cell carcinoma as an intraoperative adjunct to sentinel lymph node biopsy. The Laryngoscope. 2012;122(5):1020–30. 10.1002/lary.22467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marcinow AM, Hall N, Byrum E, Teknos TN, Old MO, Agrawal A. Use of a Novel Receptor-Targeted (CD206) Radiotracer, Tc-99m-Tilmanocept, and SPECT/CT for Sentinel Lymph Node Detection in Oral Cavity Squamous Cell Carcinoma Initial Institutional Report in an Ongoing Phase 3 Study. JAMA Otolaryngol-Head Neck Surg. 2013;139(9):895–902. 10.1001/jamaoto.2013.4239 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(TIF)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.