Abstract
Cytomegalovirus (CMV) infection has been linked to inflammation-related disease processes in the human host, including vascular diseases and chronic transplant rejection. The mechanisms through which CMV affects the pathogenesis of these diseases are for the most part unknown. To study the contributing role of the host immune response to CMV in these chronic inflammatory processes, we examined endothelial cell interactions with peripheral blood mononuclear cells (PBMC). Endothelial cultures were monitored for levels of fractalkine induction as a marker for initiating the host inflammatory response. Our results demonstrate that in the presence of CMV antigen PBMC from normal healthy CMV-seropositive donors produce soluble factors that induce fractalkine in endothelial cells. This was not observed in parallel assays with PBMC from seronegative donors. Examination of subset populations within the PBMC further revealed that CMV antigen-stimulated CD4+ T cells were the source of the factors, gamma interferon and tumor necrosis factor alpha, driving fractalkine induction. Direct contact between CD4+ cells and the endothelial monolayers is required for this fractalkine induction, where the endothelial cells appear to provide antigen presentation functions. These findings indicate that CMV may represent one member of a class of persistent pathogens where the antigen-specific T-cell response can result in the induction of fractalkine, leading to chronic inflammation and endothelial cell injury.
Human cytomegalovirus (CMV) is a member of the beta herpesvirus family. This large double-stranded DNA virus encodes more than 200 gene products with roles in the lytic and latent stages of its life cycle (reviewed in reference 22). Several viral genes encode factors associated with modulating functions of the host immune system, including homologues of host chemokines and chemokine receptors (9, 19, 22, 24, 26). These viral homologues have been reported to interact with their host receptor or ligand counterparts that are known to play a role in the host inflammation response (13, 28, 38). A recent report also demonstrates that the virus can bind to TLR-2 and CD14+ receptors on host cells and activate signaling pathways for inflammatory cytokine responses (5, 30).
CMV is an opportunistic pathogen and causes significant morbidity and mortality in immunocompromised populations, including transplant recipients, the developing fetus, and human immunodeficiency virus-infected individuals. There is also increasing evidence to associate CMV infection with inflammation-related diseases. Significant rates of vascular complications and transplant loss are linked with CMV infection. Moreover, the increasing number of surgeries for vascular diseases and transplants identifies a pressing need for a better understanding of the pathogenesis of these disorders so that new approaches can be developed to prevent and treat these debilitating and often life-threatening diseases (12, 43). Specific examples of disorders in which CMV may play a role include coronary artery disease, restenosis after angioplasty procedures, and transplant vascular sclerosis (TVS) in chronic graft rejection (31, 33, 37, 43). Prior infection with CMV has been shown to be a strong independent risk factor for restenosis (33, 43). In addition, several examples support an association between CMV infection and TVS. In an animal model, rat CMV infection is associated with the acceleration of TVS, leading to graft failure (4, 15, 18, 19, 23). Ganciclovir therapy can eliminate virus-induced TVS and also prolongs graft survival significantly in these animal model systems (14, 16, 17). In addition, ganciclovir has been shown to delay graft rejection after heart transplant (21, 37). The mechanisms through which CMV affects the pathogenesis of these inflammatory diseases are for the most part unknown. Viral chemokine and receptor homologues in the CMV genome highlight the potential for CMV to modulate the host immune response (17, 29, 32, 37), and these may also have a role in the pathogenesis of inflammatory diseases. In addition, the inflammatory response in these disease processes may also be influenced through effects mediated by the host immune response to the virus itself (34).
The vascular endothelium plays a major role during disease processes and responds to inflammatory cytokines and chemokine factors by upregulation of cell surface markers to recruit leukocyte populations to inflammation sites. The expression of the host chemokine, fractalkine, on activated endothelial cells contributes to leukocyte adhesion and can be secreted to form a chemoattractant gradient to induce migration of natural killer (NK) cells, monocytes, and specific CD8+ populations (reviewed in references 1, 7, 34, 35, and 36). There is increasing evidence to support a key role for fractalkine-fractalkine receptor (CX3CR1) interactions in the host inflammatory response leading to vascular injury (reviewed in references 34 and 35). During the rejection process in kidney and cardiac transplants, expression levels of fractalkine are dramatically increased in endothelial cells within the graft tissues (27, 36, 40). Neutralizing antibodies to fractalkine block the transplant rejection process in animal models (6). In fractalkine receptor knockout mice, a significant increase in graft survival time of heart transplants can be observed (10). Fractalkine expression is also upregulated on endothelial cells in cases of human atherosclerosis and TVS (40). Consistent with these models, an association between a polymorphism in CX3CR1 and coronary vascular endothelial dysfunction and atherosclerosis has been reported, suggesting an important role for fractalkine and its receptor in vascular disease (20). Fractalkine can also activate NK cells directly, which can result in an enhanced rate of NK-mediated cytolysis targeting fractalkine-expressing endothelium (41). A recent report demonstrates that cytomegalovirus-mediated upregulation of chemokine expression, including fractalkine correlates with the acceleration of chronic rejection in rat heart transplants (32).
The effects on inflammatory processes involved in CMV-associated vascular disease probably involve both virus infection and the host immune response, but the specific mechanisms in this complex virus-host interaction are unclear. To study the contributing role of the host immune response to CMV in these chronic inflammatory processes, we examined the interactions of endothelial cell monolayers with peripheral blood mononuclear cell (PBMC) populations from CMV-seropositive and -seronegative donors. Our findings indicate that CMV may represent one member of a class of pathogens where the host antigen-specific T-cell activation response can result in the induction of fractalkine leading to chronic inflammation and endothelial cell injury.
MATERIALS AND METHODS
Cells.
Human PBMC were isolated from heparinized blood of healthy donors by using density centrifugation over Ficoll-Hypaque (Pharmacia-Biotech, Piscataway, N.J.). Donors were determined to be either seropositive or seronegative for CMV as determined by latex agglutination (Becton Dickinson, Sparks, Md.). After two washes with phosphate-buffered saline (PBS), PBMC were suspended at a concentration of 1.0 × 106 cells/ml in RPMI 1640 with glutamine, 10% fetal bovine serum, and penicillin-streptomycin (100 U and 100 μg per ml of medium, respectively).
Primary human foreskin fibroblast cultures were maintained in Dulbecco modified Eagle medium (Invitrogen), supplemented with 5% fetal calf serum (Invitrogen; endotoxin and mycoplasma free) and penicillin-streptomycin (100 U and 100 μg per ml of medium, respectively).
Primary human aortic endothelial cells (AEC) and culture medium were purchased from Clonetics (San Diego, Calif.). Each cell lot was from a single donor. Low-passage AEC were used from doubling 5 to doubling 10. All experiments were repeated with at least two different donors of AEC.
ELISA.
Soluble fractalkine (CX3CL1) was detected in culture supernatants with a commercially available enzyme-linked immunosorbent assay (ELISA) detection kit (DY365 DuoSet System for human fractalkine/CX3CL1; R&D Systems, Inc.). The kit contains reagents for developing sandwich-type ELISAs to measure native and recombinant human fractalkine. The linear range of detection is within 3 to 200 ng of fractalkine per ml, when following the manufacturer's instructions. Samples of >200 ng/ml were diluted 1:10 and 1:20 in sample dilution buffer and reassayed. For fractalkine standards, 420 ng of recombinant human fractalkine (provided with kit)/ml was used diluted as twofold serial dilutions in diluent buffer.
For fractalkine detection, specific antibodies were provided by R&D Systems (Minneapolis, Minn.). Each well of a 96-well Immulon plate (Fisher, Tustin, Calif.) was coated overnight at room temperature with 100 μl of 0.4 μg of primary antibody in phosphate-buffered saline (PBS; pH 7.2). Plates were washed in 0.05% Tween 20 in PBS and then blocked for 2 h in 1% bovine serum albumin-5% sucrose in PBS. Standards or culture sample supernatants (100 μl) were added, followed by incubation overnight at room temperature. Peroxidase-conjugated detection antibody (also supplied by R&D Systems) at a dilution of 1:200 (100 μl) was added, followed by incubation at room temperature for 30 min. Color was then developed by adding 100 μl a solution of hydrogen peroxide mixed with tetramethylbenzidine (R&D Systems). The optical density was then read at a wavelength of 450 nm, with subtraction of 630 nm in a Bio-Tek Kinetics Reader (Bio-Tek Instruments, Inc., Winooski, Vt.).
For the detection of gamma interferon (IFN-γ), tumor necrosis factor alpha (TNF-α), interleukin-1β (IL-1β), IL-6, and IL-12, human cytokine kits were obtained from BioSource (Camarillo, Calif.), and assays were performed according to the standard protocol. All samples were prepared in duplicate and graphed as the mean or the mean and standard deviation.
Cocultures of PBMC or subset populations with AEC monolayers.
Cocultures were set up with resting confluent primary AEC monolayers, overlaid with either 106 PBMC or CD4+ cells except where specified. Cocultured cells were then stimulated with either heat-inactivated AD169 or PHA-P (10 μg/ml of medium) and incubated in a humidified incubator for 72 h at 37°C in 5% CO2. Cocultures were maintained in a 50:50 mix of RPMI and EGM-2 medium (Clonetics) to support both cell types.
Western blot analysis.
Cell monolayers were rinsed in PBS buffer, lysed according to manufacturer's instructions in sample loading buffer, a component of the NuPage Gel System provided by Invitrogen. Samples were loaded, and proteins were separated on NuPage 10% bisacrylamide gels. A positive control for fractalkine detection was used, consisting of an 85- to 90-kDa form of recombinant human fractalkine lacking the carboxy-terminal 57 amino acids (#365-FR; R&D Systems) (7). Proteins were then transferred onto nitrocellulose membranes (pure nitrocellulose; Schleicher & Schuell) by using NuPage system transfer buffer and following the manufacturer's protocol. Blot membranes were blocked in solution of 10% (wt/vol) nonfat dry milk in 1× PBS, 0.05% Tween 20, 2% normal donkey serum (Jackson Laboratories), and 2% bovine fetal calf serum. Blocking was done overnight. For detection of fractalkine on Western blots, the blocked membranes were incubated with primary antibody (R&D anti-human fractalkine goat polyclonal antibody #AF365) at a dilution of 1:200 in blocking buffer for 2 h at room temperature. Blot membranes were then washed three times at room temperature in wash buffer consisting of 1× PBS with 10% dried milk and 0.1% Tween 20. Membranes were then incubated with secondary antibody, a donkey anti-goat conjugated to horseradish peroxidase (available from Santa Cruz) at a 1:1,000 dilution in 1× PBS in 10% dried milk, 2% bovine fetal calf serum, and 0.05% Tween 20 for 1 h at room temperature. This was followed by washing in three changes of wash buffer as described above. For detection of fractalkine bands, the blot was incubated with chemiluminescence substrate from the Western Lightning ECL detection kit (NEN/Perkin-Elmer) according to the manufacturer's instructions. This step was followed by exposure to X-ray film (Kodak X-Omat Blue XB-1) for detection of the fractalkine band signal.
PBMC subset isolations.
CMV-seropositive and -seronegative donor pairs were compared for fractalkine induction by using PBMC, a CD14+ cell fraction, and a non-CD14+ (T-cell-enriched fraction). CD14+ cells for these assays were prepared by using a positive selection system for CD14+ cells available from Miltenyi Biotech (Auburn, Calif.). A total of 1.5 × 106 cells were overlaid per well of 24-well tissue culture dishes; for PBMC, the cell fractions were loaded per culture well “to scale” relative to this number. For example, the CD14+ fraction represents ca. 10% of the total PBMC. Then, 1.5 × 105 CD14+ cells were loaded per culture well.
CMV-seropositive donors were then used to compare fractalkine induction abilities between CD4+, CD8+, and CD4+ CD8+ cells and PBMC. To prepare the CD4+ and CD8+ groups, a negative selection approach was used with the StemSep system. A total of 4 × 106 cells overlaid per well with the total PBMC population; isolated cells from the other subset groups were then loaded to scale relative to this number.
For preparations of CD4+ cells for other assays, including neutralization assays, the CD4+ cells were enriched from PBMC populations according to the manufacturer's instructions by using a negative selection MidiMACS system and LS+ immunomagnetic columns (Miltenyi Biotech).
Viral antigen preparations.
Primary human foreskin fibroblast cultures were infected at a multiplicity of infection of 0.01 with strain AD169 (originally obtained from the American Type Culture Collection in 1986) and monitored for the point of 100% cytopathic effect. Cell culture supernatants were collected and clarified by centrifugation at 1,200 × g for 5 min. Clarified supernatants were then collected and divided into aliquots among a series of sterile 1.5-ml Eppendorf tubes at 1 ml per tube. Samples were then centrifuged at 14,000 rpm in microfuge at 4°C, and pellets were resuspended in 1 ml of RPMI plus 10% fetal calf serum. Resuspended samples were then placed in a 56°C water bath for 1 h to denature them. Aliquots prior to heat inactivation were also assayed for virus titers, which ranged from 2 × 106 to 5 × 106 PFU/ml. The heat-inactivated preparations were then stored at −70°C until needed. For each assay, 100 μl of thawed antigen preparation was added to each well per 24-well plate in 1 ml of medium.
Neutralization assays.
Neutralization assays with antibodies specific for TNF-α, IFN-γ, and IL-12 were carried out by adding the specific antibodies at the time of the cocultivations of CD4+ lymphocytes or PBMC with AEC. For some samples, antibody combinations were added on each of the 3 days and referred to as “per day” in figure. The various combinations of neutralizing antibodies are indicated on the x axis for each sample. The results are shown for day 3, where effects of neutralization of the different cytokines are associated with decreases in fractalkine levels in comparison to untreated controls, as measured by ELISA. Commercially available antibodies used in the neutralization assays were anti-IL-12 monoclonal antibody C11.5 (BD Pharmingen), anti-IFN-γ monoclonal antibody B27 (BD Pharmingen), anti-TNF-α monoclonal antibody MABTNF-A5 (BD Pharmingen), and purified mouse IgG1 antibody clone 107.3 and mouse IgG2a,K as isotype controls (BD Pharmingen). All antibodies were prepared without azide. Manufacturer's recommended concentrations were used for neutralization assays.
RESULTS
PBMC populations from CMV-seropositive donors can be stimulated by viral antigen, resulting in the induction of fractalkine in endothelial cell cultures.
Fractalkine induction in endothelial cells is a known marker for initiation of the inflammatory response (reviewed in reference 1). A series of CMV-seropositive and -seronegative donors were compared for differences in ability to influence the host fractalkine induction response in the setting of the vascular endothelium. In these experiments, PBMC were compared for ability to induce fractalkine in endothelial cell cultures, in response to phytohemagglutinin (PHA) or antigen-specific (CMV antigen) stimulation. PBMC were maintained as cocultures with endothelial cell monolayers, followed by stimulation with either PHA (10 μg/ml of medium) or heat-inactivated human CMV strain AD169. The cocultures were maintained for 3 days, and supernatants and monolayers were collected separately at 72 h. Fractalkine levels in endothelial monolayers were detected by Western blotting. In addition, endothelial culture supernatants were screened for the soluble, secreted form of fractalkine by ELISA.
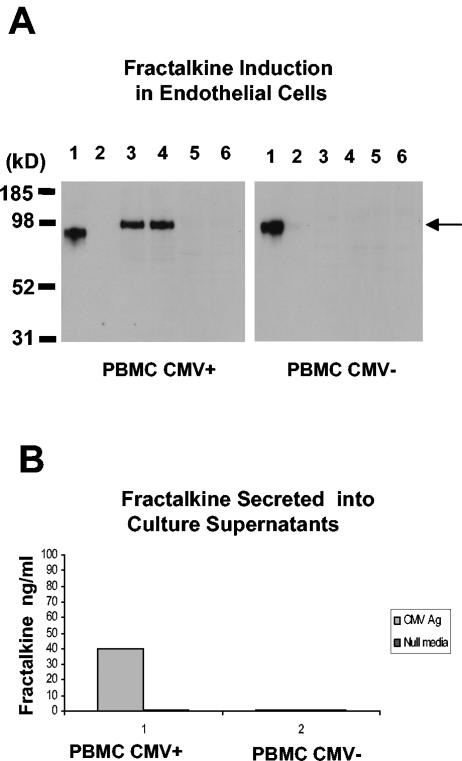
When AEC monolayers were cocultured with CMV antigen-stimulated PBMC from normal healthy CMV-seropositive donors, a single fractalkine-specific protein band was detected (Fig. 1A). The protein migrated with a slightly slower Mr of ∼100 kD compared to that of the positive control fractalkine of ∼85 kDa, a form of fractalkine lacking the carboxy-terminal region of 57 amino acids and similar in size and structure to the secreted form of the protein (7, 8). In the presence of appropriate cytokines such as TNF-α, a host cell protease (ADAM-17) can specifically cleave the cell-associated ∼100-kDa form to the ∼85-kDa secreted form (8). The larger form is consistent with reports of the cell-associated precursor form of fractalkine prior to cleavage and release from the cell surface (7, 8). In contrast, fractalkine induction was not observed when PBMC from CMV-seronegative donors were challenged with CMV antigen. All PBMC populations from each donor responded consistently to the general stimulatory effect of PHA treatment and resulted in fractalkine induction in the endothelial cells (data not shown). As a negative control, PBMC were cocultured with AEC monolayers and maintained for 3 days. Under these conditions, the cells consistently demonstrated a lack of fractalkine induction (Fig. 1A).
FIG. 1.
Fractalkine induction in endothelial cell cultures associated with CMV antigen-stimulated PBMC from CMV-seropositive donors. The data are representative of three separate experiments with different blood donors. (A) Detection of fractalkine induction in endothelial cell monolayers cocultured with CMV-seropositive PBMC by Western blot analysis with fractalkine-specific antibody. Lanes in left gel panel: 1, positive control for fractalkine, with ∼85-kDa form of fractalkine (note that the fractalkine form [R&D] lacks 57 carboxy-terminal amino acids and migrates at ∼85 kDa, whereas the endothelial-cell-associated form [also from R&D] is full length and migrates at ∼100 kDa); 2, negative control for fractalkine with endothelial cells in a resting state; 3 and 4, replicate samples of CMV antigen-treated PBMC from a CMV-seropositive donor; 5 and 6, replicate samples of media alone-treated PBMC from a CMV-seropositive donor. Lanes in right gel panel: 1, positive control for fractalkine, with ∼85-kDa form of fractalkine (commercially available from R&D); 2, negative control for fractalkine with endothelial cells in a resting state; 3 and 4, replicate samples of CMV antigen-treated PBMC from a CMV-seronegative donor; 5 and 6, replicate samples of medium-alone-treated PBMC from a CMV-seronegative donor. The arrow at the right of the gel indicates the Mr of fractalkine. (B) Detection of secreted fractalkine levels in coculture supernatants. ELISA results from coculture supernatants, comparing CMV-seropositive PBMC to CMV-seronegative PBMC.
Fractalkine levels were also measured as cumulative levels of soluble fractalkine released into the culture supernatants by day 3 (Fig. 1B). Levels of soluble fractalkine paralleled those in Western blot analyses, where again the antigen-specific response to CMV was able to induce soluble fractalkine in the AEC cultures. These results were consistently reproducible with all CMV-seropositive donor PBMC able to induce fractalkine in AECs when exposed to CMV antigen (data not shown). In contrast, all seronegative donor PBMC were unable to induce fractalkine under the same conditions (data not shown).
Viral antigen-stimulated host CD4+ cells are the subpopulation that can induce fractalkine in endothelial cells.
Because previous results indicated that soluble factors were driving the fractalkine induction, the next set of experiments was designed to identify the specific cell type(s) producing the factors. The two major cell populations that could contribute important factors impacting on this process, myeloid and lymphoid lineage cells, were examined for these studies.
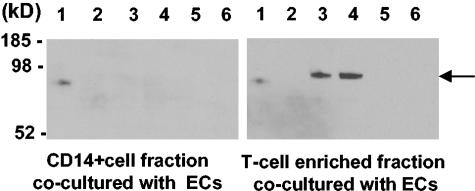
Studies of CD14+ versus CD14− (lymphoid) populations demonstrate that fractalkine induction ability partitions with the lymphoid population.
CD14+ and CD14− cells were separated by positive selection for CD14+ cells (myeloid enriched) and the CD14− group (containing remaining lymphoid cells after CD14+ depletion) (Miltenyi Biotech). A CMV-seropositive and CMV-seronegative donor pair were compared for fractalkine induction with PBMC, the CD14+ cell fraction, and the non-CD14+ fraction (lymphoid enriched) (Fig. 2, left blot panel). Using AEC monolayers cocultured with the CD14+ cell population, no induction of fractalkine was observed. In contrast, the CD14− (lymphoid cells) fraction maintained as cocultures with AEC resulted in fractalkine induction when exposed to CMV antigen by day 3 (Fig. 2, right blot panel).
FIG. 2.
Western blot analysis showing fractalkine induction is associated with CMV-seropositive lymphoid populations. The data are representative of two separate experiments with different blood donors. A CD14+ sample analysis is shown in the left panel, with lanes loaded as follows: lane 1, positive control for fractalkine with ∼85-kDa form of protein; lane 2, negative control for fractalkine with endothelial cells in a resting state; lanes 3 and 4, replicate samples of CMV antigen-treated cocultures with CD14+ and AEC; lanes 5 and 6, replicate cocultures of CD14+ cells and AEC in medium alone. A lymphoid-enriched fraction was used in a parallel analysis (right panel): lane 1, positive control for fractalkine with ∼85-kDa form of the protein (R&D); lane 2, negative control for fractalkine with endothelial cells in a resting state; lanes 3 and 4, replicate samples of CMV antigen-treated cocultures with lymphoid-enriched cells and AEC; lanes 5 and 6, replicate cocultures of lymphoid-enriched cells and AEC in medium alone.
CD4+ T lymphocytes are associated with fractalkine induction.
To further define the cell type(s) involved in fractalkine induction, CD4+- and CD8+-T-cell populations were tested for the ability to induce fractalkine in AEC during coculture conditions. CD4+, CD8+, and CD4+ CD8+ cells and PBMC populations were isolated from CMV-seropositive donors. Cell numbers were standardized for all experiments. For each of the subpopulations for coculture with AEC, the numbers were set to ∼25% of the total PBMC number. When set up for coculture, 4 × 106 PBMC were overlaid into each culture well of 50,000 AEC; 106 CD4+ cells were set up (∼25% of 4 × 106 PBMC). CD8+ populations were also set up to scale by using the same approach.
Induction of fractalkine in AEC monolayers was determined on day 3 during coculture with either CD4+ or pooled CD4+ and CD8+ populations isolated from a CMV-seropositive donor (Fig. 3). CD4+ alone and CD4+ pooled with CD8+ cocultures induced fractalkine, especially in the viral antigen-treated samples (see lanes 2 and 3 for CD4+ samples in the left gel panel of Fig. 3A; CD4+ and CD8+ pooled data, see lanes 2 and 3, right gel panel); PBMC samples were consistently positive for fractalkine in PHA- and viral-antigen-treated cocultures (data not shown). In contrast, the CD8+ samples were consistently negative for fractalkine induction (Fig. 3A, right gel panel, lanes 6 and 7; Fig. 3B, ELISA results). There was no change in the apparent quantity of fractalkine induction by CD8+ cells since neither an increase or decrease in fractalkine was observed when CD8+ cells were combined with CD4+ cells. Overall, the results show that CD4+ lymphocytes demonstrate fractalkine induction in AEC monolayers, when stimulated with CMV antigen. In contrast, this was not observed in the CD8+ viral-antigen-stimulated populations.
FIG. 3.
Fractalkine induction associated with CD4+ T-cell population. The data are representative of three experiments with different donors. (A) Western blots showing fractalkine induction in AEC cocultured with CD4+ cells, CD4+ CD8+ cells, and CD8+ cells, each stimulated with HCMV antigen and as nonstimulated resting state controls. The left panel shows results for CD4+ T cells with lanes loaded as follows: lane 1, positive control for fractalkine (R&D); lanes 2 and 3, replicate samples of CMV antigen-treated CD4+ T cells from a CMV-seropositive donor; lanes 4 and 5, replicate samples of medium-alone-treated same CD4+ T cells from a CMV-seropositive donor. The arrow between panels indicates the relative mobility of fractalkine. The right panel shows the results for CD4+ CD8+ samples, with lanes loaded as follows: lane 1, positive control for fractalkine; lanes 2 and 3, replicate samples of CMV antigen-treated CD4+ CD8+ T cells from a CMV-seropositive donor; lanes 4 and 5, replicate samples of medium-alone-treated CD4+ CD8+ cells; lanes 6 and 7, replicate samples of CMV antigen-treated CD8+ T cells; lanes 8 and 9, replicate samples of medium-alone-treated samples of CD8+ T cells from a CMV-seropositive donor. (B) ELISA demonstrating presence of secreted fractalkine in coculture medium with CD4+ cells in presence of CMV antigen and AEC. In contrast to this, CD8+ cells from CMV-seropositive donors show a clear absence of fractalkine production with CD8+ cells cocultured with AEC, even in the presence of CMV antigen.
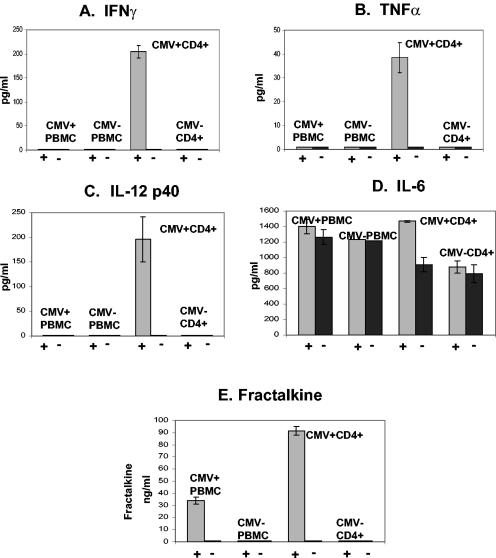
TNF-α and IFN-γ are the dominant soluble factors that drive fractalkine induction in endothelial cells.
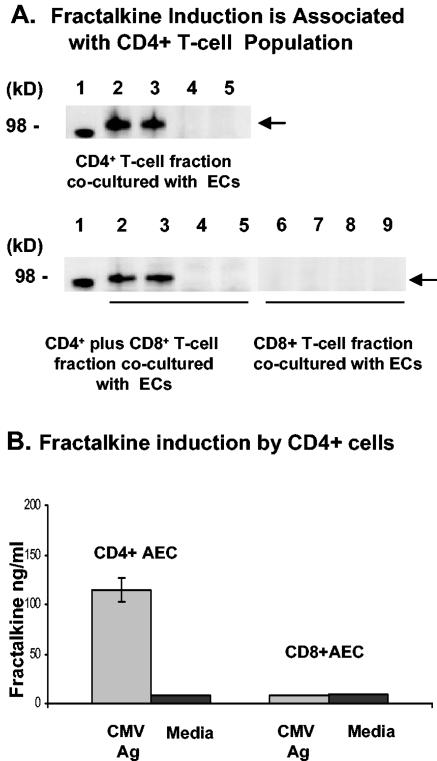
The identification of the CD4+-T-cell subset within the PBMC population producing the soluble factor(s) that induce fractalkine in endothelial cells provided the opportunity to examine candidate factors that could be released by CD4+ cells during CMV antigenic stimulation. To determine potential candidate factors, CD4+ cells from CMV-seropositive and -seronegative donors were prepared for coculture with AEC monolayers and replicate cultures were treated with PHA stimulation, viral antigen stimulation, or medium-only controls. Culture supernatants were collected at day 3 and screened for the following cytokines known to be produced by antigen-stimulated T cells that can also induce fractalkine (30): IL-6, IFN-γ, TNF-α, and IL-12. The results are shown in Fig. 4.
FIG. 4.
Screening for candidate factors (IFN-γ, TNF-α, IL-12, and IL-6) by ELISA to determine which factors are associated consistently with fractalkine induction by CMV antigen stimulation. A “+” or “−” symbol below the bar graphs refers to samples with or without CMV antigen stimulation, respectively. Supernatant samples were screened from day 3 cocultures of AEC monolayers with PBMC or CD4+ cells from a CMV-seropositive and CMV-seronegative pair of donors. (A) IFN-γ; (B) TNF-α; (C) IL-12; (D) IL-6; (E) fractalkine.
Initial screening for cytokines potentially involved in fractalkine induction eliminated IL-6 and IL-1β as important factors because only minor differences were observed between stimulated and nonstimulated cultures (IL-1β; data not shown). Likewise, there were similar IL-6 and IL-1β levels between CMV-seropositive and -seronegative donors upon exposure to CMV antigen. The results for other cytokine levels are shown in Fig. 4. Three cytokines—IL-12, TNF-α, and IFN-γ—were consistently found to be elevated in AEC cocultured with CD4+ cells from CMV-seropositive donors exposed to CMV antigen. Therefore, these cytokines were selected as the candidate factors to focus on further testing by reconstruction approaches and neutralization assays. Figure 4E demonstrates that the samples used to screen for candidate factors involved in the induction process are associated with the production of fractalkine.
The ability of each candidate factor was tested for fractalkine induction in AEC by using levels of each factor as measured on day 3 in supernatants from cocultivations. Briefly, AEC cultures were treated for 24 h with the observed concentrations of each candidate factor and measured for levels of induced fractalkine by Western blotting and ELISA. Levels of fractalkine induced in the reconstruction assays are similar to those detected in the actual viral antigen stimulated cocultures of CMV-seropositive CD4+ cells with AEC (Fig. 5). The induced fractalkine levels are consistent between the Western blot analyses and ELISA results (blot data not shown). The results indicate that IFN-γ and TNF-α have the most important impact on fractalkine induction (Fig. 5). A synergistic effect of these two cytokines for fractalkine induction can also be seen in the ELISA results of Fig. 5, where dual treatment with these factors results in increased fractalkine levels relative to treatment with each factor alone (35). The levels of IFN-γ and TNF-α produced by CMV-seropositive CD4+ cells during treatment with viral antigen can induce significant levels of fractalkine in AEC during coculture (Fig. 6).
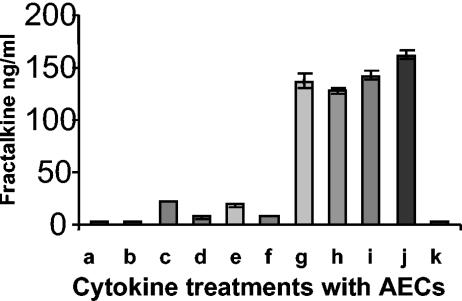
FIG. 5.
Reconstruction assays in which the candidate factors IFN-γ, TNF-α, and IL-12 were tested for their ability to directly induce fractalkine in endothelial cultures, with the levels of each factor as measured on day 3 in supernatants from cocultivations. The graph shows the levels of induced fractalkine resulting from each cytokine or combination as detected by ELISA screen for fractalkine secreted into supernatants. Specific cytokines and concentrations are represented on the x axis as follows: a, 200 pg of IL-12/ml; b, 400 pg of IL-12/ml; c, 500 pg of IFN-γ/ml; d, 50 pg of TNF-α/ml; e, 200 pg of IL-12/ml + 50 pg of TNF-α/ml; f, 200 pg of IL-12/ml + 50 pg of TNF-α/ml; g, 50 pg of TNF-α/ml + 500 pg of IFN-γ/ml; h, 200 pg of IL-12/ml + 500 pg of IFN-γ/ml + 50 pg of TNF-α/ml; i, CMV + CD4+ cells + CMV antigen-stimulated AEC coculture supernatants day 3; j, 50 ng of TNF-α/ml + 1,000 pg of IFN-γ/ml; k, medium alone.
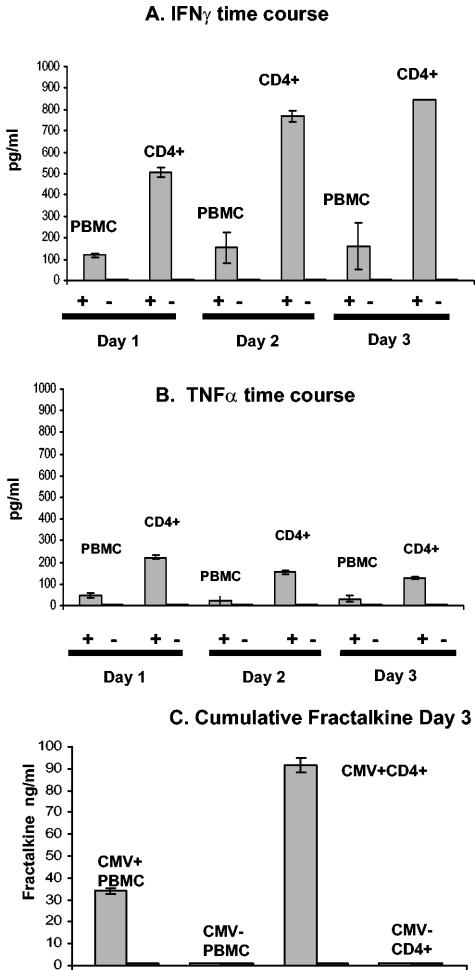
FIG. 6.
Time course in CMV antigen-stimulated CD4+ lymphocytes and PBMC cocultured with endothelial cells, showing cumulative levels of TNF-α (A) and IFN-γ (B) in culture supernatants over the course of 3 days. The results are shown with a CMV-seropositive donor, since the CMV-seronegative donor was completely negative for fractalkine induction. (C) Cumulative fractalkine levels by day 3 from same cocultures, showing results from a CMV-seropositive donor and a CMV-seronegative donor as a control. The data are representative of three separate experiments with different donors. The “+” or “−” symbol below graphs refer to samples with or without CMV antigen stimulation, respectively.
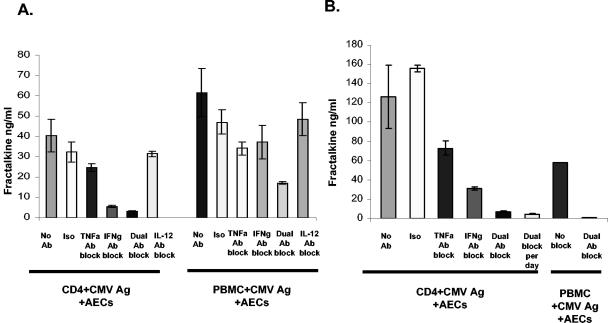
Neutralization assays with specific antibody were set up to identify the factors driving fractalkine induction in the AEC. Neutralizing antibodies were added directly to cocultivations of CD4+ lymphocytes and AEC. A marked reduction in fractalkine levels was observed in supernatants with neutralizing antibodies to TNF-α and IFN-γ (Fig. 7).
FIG. 7.
Neutralization assays confirm TNF-α and IFN-γ drive fractalkine induction in AEC. Neutralization carried out directly in cocultivations of CD4+ lymphocytes or PBMC with AEC. (A) Demonstration by ELISA screens of culture supernatants, showing loss of fractalkine in supernatants with neutralizing antibodies to target TNF-α and IFN-γ. In this sample, CD4+ cells were set up to scale with PBMC. Specific antibody blocks and controls are identified on the x axis as follows: No Ab, positive control with no antibody block; Iso, isotype control antibody; TNFa Ab block, antibody-treated sample to specifically neutralize TNF-α; IFNg Ab block, specific neutralization with IFN-γ antibody; Dual Ab block, combined anti-IFNγ and TNF-α antibodies; IL-12 Ab block, antibody to specifically neutralize IL-12. (B) In this sample, CD4+ cells are not set to scale but were loaded at ∼106 cells per well, ∼4-fold above scale to the level of CD4+ cells in PBMC. Antibody blocks and controls are as described for panel A on the x axis; “Dual Ab block per day” refers to combined anti-IFN-γ and TNF-α antibodies added on each of the 3 days during cocultivation. The data are representative of three separate experiments with different donor samples.
DISCUSSION
CMV infection is associated with vascular diseases such as restenosis and transplant vascular sclerosis, diseases that are also characterized by abnormal inflammatory processes. Much research has examined the effects of virus-encoded factors on the host immune system and has provided important insights on how the virus circumvents the host's defense mechanisms. However, limited research has examined the contributing effects of the host immune responses to the pathogenesis of these CMV-associated vascular diseases that is the focus of the present study. PBMC populations or subsets were stimulated with CMV antigen and cocultured with endothelial monolayers. The overall results of this research demonstrate that, in the presence of CMV antigen, PBMC populations from normal healthy seropositive donors produce soluble factors that induce fractalkine in endothelial cells. Examination of subset populations within the PBMC further revealed that CMV antigen-stimulated CD4+ cells were the source of the factors, IFN-γ and TNF-α, driving this fractalkine induction process. To our knowledge, this is the first report to show that the host antigen-specific T-cell activation response directed against CMV can produce the appropriate cytokines at levels high enough to induce fractalkine in local adjacent endothelial cells.
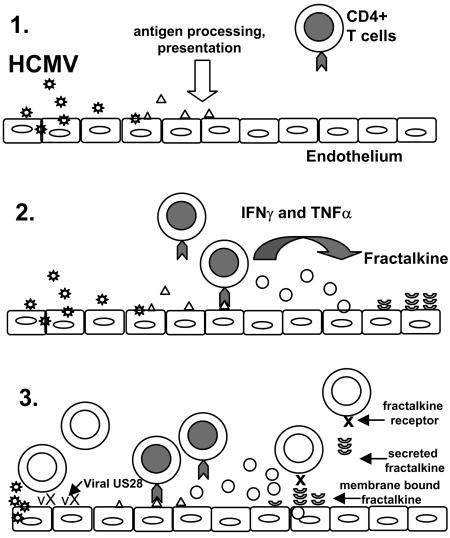
These results provide support for a model on the role of fractalkine induction by the host's CMV antigen-specific CD4+-T-cell response and how this may contribute to endothelial damage (Fig. 8). In the first step, CMV infection of endothelial cells leads to the release of infectious virus, defective virion particles, and viral proteins. The latter two have the clear potential to be processed and presented as antigen by other adjacent endothelial cells. In the second step, viral antigen is presented to CMV antigen-specific CD4+ T cells by the endothelial cells. IFN-γ and TNF-α are then released by the antigen-stimulated CD4+ cell. These cytokine factors interact with the endothelium, resulting in fractalkine induction and secretion (8, 35). In the third step, the localized concentration of fractalkine on the apical surface of endothelial cells, together with the release of soluble fractalkine, results in a fractalkine gradient. This gradient can attract additional inflammatory cells to the site and can include NK cells, monocytes, and certain types of CD8+ T cells. These incoming inflammatory infiltrate cells can bind to membrane-bound fractalkine on the endothelial cell surface via their fractalkine receptor, CX3CR1. NK cells are especially known to cause endothelial damage in this setting, since they can be activated by fractalkine and destroy cells through cytolytic activity (6, 41).
FIG. 8.
Proposed model for role of fractalkine induction by CMV antigen-specific CD4+ response leading to endothelial damage. CMV infection in endothelial cells releases viral proteins as shown in panel 1. These are processed and presented as antigen by other adjacent endothelial cells as shown in panel 2. CMV viral antigen is presented to CMV antigen-specific CD4+ cells by the endothelial cells. IFN-γ and TNF-α are released by the antigen-stimulated CD4+ cells (represented by cells with gray-shaded nuclei); these released factors interact with the endothelial cells, resulting in fractalkine induction (panel 3). Localized concentrations of fractalkine on the surface of endothelial cells, together with the release of soluble fractalkine, results in a fractalkine gradient. This can attract additional inflammatory cells to the site (these cells are represented by nonshaded nuclei), including monocyte/macrophage cells, NK cells, and CD8+ populations. Also, the presence of CMV US28, a CX3CR1 mimic, on the surface of endothelial cells during infection and on the envelope of virion particles released in the localized area could bind fractalkine and influence the inflammation processes dependent on fractalkine signals. This illustration is expanded from the fractalkine and vascular injury model of H. Umehara (30).
In the setting of the infected host, the expression of CMV US28, a viral CX3CR1 mimic, has the potential to bind fractalkine and influence the inflammation process. CMV US28 is expressed on the surface of infected endothelial cells and has also recently been shown to be a physical component of the virion particle where it is expressed on the viral surface (1, 6, 13, 25). The localized presence of high concentrations of virion particles expressing US28 could potentially bind secreted fractalkine and affect levels of this chemokine to the point of altering gradients to attract various inflammatory or effector cell populations. Viral US28 expressed on infected endothelial cells may also bind fractalkine, again either interfering with gradient levels or perhaps creating localized high levels of fractalkine by altering or reversing the gradient. These events may shift the normal inflammatory response of the host to an outcome resulting in damage to the endothelium.
Another contributing factor to endothelial damage could be the actual frequency of CMV-specific CD4+ T-lymphocytes in a specific host, which can be relatively high. In some individuals, as many as 20% of all CD4+ T cells are specific for CMV (2, 3, 11). This high frequency also contributes to a greater probability of direct contact between viral-antigen-presenting endothelial cells and CMV-specific CD4+ T cells, especially in the setting of slow blood flow, as occurs in arteries with a smaller cross-sectional area, such as coronary arteries or arterioles. Again, this could lead to a higher risk of damage to the endothelial cells within the immediate vascular endothelium. The high investment in the T-cell response on the part of the host may only occur with certain types of pathogens, such as CMV. The predicted outcome would be that the higher the cell frequency, the stronger the CD4+ response to initiate higher levels of fractalkine. This relationship has been found in men in at least one study suggesting a relationship of CMV with coronary artery disease and potentially other vascular diseases (42).
The degree of exposure between virus and host may also provide another contributing factor toward endothelial damage associated with vascular disease. CMV is a herpesvirus, with the characteristic ability to establish a latent infection in the human host. Recurrent reactivation episodes could create a setting for repeated exposure over time of viral antigen to the CD4+ antigen-specific populations. This would also be consistent with the chronic nature of vascular disease, particularly in the setting of long-term or chronic transplant rejection and vascular disease. With recurrent episodes, the accumulated damage to the endothelium may become severe enough to develop into permanent vascular damage. In this situation, the frequency of reactivation and the latent viral load level in the host may affect the degree of endothelial damage.
Another aspect of the host immune response may also influence the degree of endothelial damage. In TVS, there is an allogeneic component to the inflammatory disease process. Although the PBMC and endothelial sources in the coculture system are each from different donors, the reported results cannot be explained entirely on the basis of an allogeneic response due to donor mismatch. Despite these nonautologous conditions between the endothelial cells and blood populations, fractalkine induction was never detected when PBMC from seronegative donors were exposed to CMV antigen. Thus, the fractalkine induction that we observed is not due to a background allogeneic response. CMV antigen presentation by the endothelial cells to CD4+ cells also still occurs in this nonautologous setting, an observation consistent with previous reports (39). The advantage of this nonautologous coculture system is that it may actually model processes occurring in TVS in the setting of graft rejection. In CMV-associated transplant rejection, the early stages may be characterized by CMV-specific CD4+ T cells recognizing CMV antigen and producing IFN-γ and TNF-α. These cytokines not only induce fractalkine expression on the endothelial cells but will also induce major histocompatibility complex (MHC) class II expression on local endothelial cells. The resulting activated endothelium, therefore, would express fractalkine and significant levels of MHC class II. These levels of MHC class II could contribute to later stages of the transplant rejection process, where an allogeneic response plays a dominant role. An improved understanding of how these host-virus interactions affect inflammation-related disease processes has the potential to identify novel strategies to prevent vascular damage due to endothelial cell injury.
Acknowledgments
This study was supported in part by grants from the National Institute of Allergy and Infectious Diseases (AI39004, AI27563, AI33835, and AI36214) to the Virology Core, University of California, San Diego, Center for AIDS Research.
REFERENCES
- 1.Ancuta, P., R. Rao, A. Moses, A. Mehle, S. K. Shaw, F. W. Luscinskas, and D. Gabuzd. 2003. Fractalkine preferentially mediates arrest and migration of CD16+ monocytes. J. Exp. Med. 197:1701-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bettinotti, M. P., S. Solomon, M. Battiwala, N. Hensel, K. Ghazarian, D. Stroncek, and J. Barrett. 2003. T-cell response against the cytomegalovirus proteins pp65 and IE1. Hum. Immunol. 64:S73. [Google Scholar]
- 3.Bitmanseur, A. D., S. L. Waldrop, C. J. Pitcher, E. Khatamzah, F. Kern, V. C. Maino, and L. J. Picker. 2001. Clonotypic structure of the human CD4+ memory T-cell response to CMV. J. Immunol. 167:1151-1163. [DOI] [PubMed] [Google Scholar]
- 4.Bruning, J. H., M. C. Persoons, K. B. Lemstrom, F. S. Stals, E. De Clercq, and C. A. Bruggeman. 1994. Enhancement of transplantation-associated atherosclerosis by CMV, which can be prevented by antiviral therapy in the form of HPMPC. Transplant. Int. 7(Suppl. 1):S365-S370. [DOI] [PubMed] [Google Scholar]
- 5.Compton, T., E. A. Kurt-Jones, K. W. Boehme, J. Belko, E. Latz, D. T. Golenbock, and R. W. Finberg. 2003. Human cytomegalovirus activates inflammatory cytokine responses via CD14and Toll-like receptor 2. J. Virol. 77:4588-4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng, L., S. Chen, G. E. Garcia, Y. Xia, M. A. Siani, P. Botti, C. B. Wilson, J. K. Harrison, and K. B. Bacon. 1999. Prevention of crescentic glomerulonephritis by immunoneutralization of the fractalkine receptor CX3CR1 rapid communication. Kidney Int. 56:612-620. [DOI] [PubMed] [Google Scholar]
- 7.Fraticelli, P., M. Sironi, G. Bianchi, D. D'Ambrosio, C. Albanesi, A. Stoppacciaro, M. Chieppa, P. Allavena, L. Ruco, G. Girolomoni, F. Sinigaglia, A. Vecchi, and A. Mantovani. 2001. Fractalkine (CX3CL1) as an amplification circuit of polarized Th1 responses. J. Clin. Investig. 107:1173-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garton, K. J., P. J. Gough, C. P. Blobel, G. Murphy, D. R. Greaves, P. J. Dempsey, and E. W. Raines. 2001. Tumor necrosis factor-converting enzyme (ADAM17) mediates cleavage and shedding of fractalkine (CX3CL1). J. Biol. Chem. 276:37993-38001. [DOI] [PubMed] [Google Scholar]
- 9.Gruhler, A., and K. Fruh. 2000. Control of MHC I traffic from the ER by cellular chaperones and viral anti-chaperones. Traffic 1:306-311. [DOI] [PubMed] [Google Scholar]
- 10.Haskell, C. A., W. W. Hancock, D. J. Salant, W. Gao, V. Csizmadia, W. Peters, K. Faia, O. Fituri, J. B. Rottman, and I. F. Charo. 2001. Targeted deletion of CX3CR1 reveals a role for fractalkine in cardiac allograft rejection. J. Clin. Investig. 108:679-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hensel, N., J. J. Melenhorst, K. Bradstock, A. P. Schwarer, R. Eniale, R. Nakamura, and A. J. Barrett. 2002. Flow cytometric quantitation and characterization of the T-lymphocyte memory response to CMV in healthy donors. Cytotherapy 4:29-40. [DOI] [PubMed] [Google Scholar]
- 12.Hosenpud, J. D., G. D. Shipley, and C. R. Wagner. 1992. Cardiac allograft vasculopathy: current concepts, recent developments, and future directions. J. Heart Lung Transplant. 11:9-23. [PubMed] [Google Scholar]
- 13.Kledal, T. N., M. M. Rosenkilde, and T. W. Schwartz. 1998. Selective recognition of the membrane-bound CX3C chemokine, fractalkine, by the human cytomegalovirus-encoded broad-spectrum receptor US28. FEBS Lett. 441:209-214. [DOI] [PubMed] [Google Scholar]
- 14.Lemstrom, K., R. Sihvola, C. Bruggeman, P. Hayry, and P. Koskinen. 1997. Cytomegalovirus-infection enhanced cardiac allograft vasculopathy is abolished by DHPG prophylaxis in the rat. Circulation 95:2614-2616. [DOI] [PubMed] [Google Scholar]
- 15.Lemstrom, K., P. Koskinen, L. Krogerus, M. Daemen, C. A. Bruggeman, and P. J. Hayry. 1995. Cytomegalovirus antigen expression, endotheliaocell proliferation, and intimal thickening in rat cardiac allografts. Circulation 92:2594-2604. [DOI] [PubMed] [Google Scholar]
- 16.Lemstrom, K. B., J. H. Bruning, C. A. Bruggeman, P. Koskinen, P. T. Aho, S. Yilmaz, I. T. Lautenschlager, and P. J. Hayry. 1994. Cytomegalovirus infection-enhanced allograft arteriosclerosis is prevented by DHPG prophylaxis in the rat. Circulation 90:1969-1978. [DOI] [PubMed] [Google Scholar]
- 17.Lemstrom, K., J. Bruning, P. Koskinen, C. A. Bruggeman, I. Lautenschlager, and P. Hayry. 1994. Triple-drug immunosuppression significantly reduces chronic rejection in noninfected and RCMV-infected rats. Transplant. Proc. 26:1727-1728. [PubMed] [Google Scholar]
- 18.Lemstrom, K. B., J. H. Bruning, C. A. Bruggeman, I. T. Lautenschlager, and P. J. Hayry. 1993. Cytomegalovirus infection enhances smooth muscle cell proliferation and intimal thickening of rat aortic allografts. J. Clin. Investig. 92:549-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Margulies, B. J., H. Browne, and W. Gibson. 1996. Identification of the human cytomegalovirus G protein coupled receptor homologue encoded by UL33 in infected cells and enveloped virus particles. Virology 225:111-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDermott, D. H., J. P. Halcox, W. H. Schenke, M. A. Waclawiw, M. N. Merrell, N. Epstein, A. A. Quyyumi, and P. M. Murphy. 2001. Association between polymorphism in the chemokine receptor CX3CR1 and coronary vascular endothelial dysfunction and atherosclerosis. Circ. Res. 89:401-407. [DOI] [PubMed] [Google Scholar]
- 21.Merigan, T. C., D. G. Renlund, S. Keay, et al. 1992. A controlled trial of ganciclovir to prevent cytomegalovirus disease after heart transplantation. N. Engl. J. Med. 326:1182-1186. [DOI] [PubMed] [Google Scholar]
- 22.Mocarski, E. S., Jr., and C. T. Courcelle. 2001. Cytomegaloviruses and their replication, p. 2629-2674. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott/The Williams & Wilkins Co., Philadelphia, Pa.
- 23.Orloff, S. L. 1999. Elimination of donor-specific alloreactivity by bone marrow chimerism prevents cytomegalovirus accelerated transplant vascular sclerosis in rat small bowel transplants. J. Clin. Virol. 12:G23-G25. [Google Scholar]
- 24.Penfold, M. E., D. J. Dairaghi, G. M. Duke, N. Saederup, E. S. Mocarski, G. W. Kemble, and T. J. Schall. 1999. Cytomegalovirus encodes a potent alpha chemokine. Proc. Natl. Acad. Sci. USA 96:9839-9844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penfold, M. E. T., T. L. Schmidt, D. J. Dairaghi, P. A. Barry, and T. J. Schall. 2003. Characterization of the rhesus cytomegalovirus US28 locus. J. Virol. 77:10404-10413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prichard, M. N., M. E. Penfold, G. M. Duke, R. R. Spaete, and G. W. Kemble. 2001. A review of genetic differences between limited and extensively passaged human cytomegalovirus strains. Rev. Med. Virol. 11:191-200. [DOI] [PubMed] [Google Scholar]
- 27.Robinson, L. A., C. Nataraj, D. W. Thomas, D. N. Howell, R. Griffiths, V. Bautch, D. D. Patel, L. Feng, and T. M. Coffman. 2000. A role for fractalkine and its receptor (CX3CR1) in cardiac allograft rejection. J. Immunol. 165:6067-6072. [DOI] [PubMed] [Google Scholar]
- 28.Saederup, N., S. A. Aguirre, T. E. Sparer, D. M. Bouley, and E. S. Mocarski. 2001. Murine CMV CC chemokine homolog MCK-2 (m131-129) is a determinant of dissemination that increases inflammation at initial sites of infection. J. Virol. 75:9966-9976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saederup, N., Y. C. Lin, D. J. Dairaghi, T. J. Schall, and E. S. Mocarski. 1999. Cytomegalovirus-encoded beta chemokine promotes monocyte-associated viremia in the host. Proc. Natl. Acad. Sci. USA 96:10881-10886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simmen, K. A., J. Singh, B. G. Luukkonen, M. Lopper, A. Bittner, N. E. Miller, M. R. Jackson, T. Compton, and K. Fruh. 2001. Global modulation of cellular transcription by human cytomegalovirus is initiated by viral glycoprotein B. Proc. Natl. Acad. Sci. USA 98:7140-7145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Speir, E., Modali, R., Huang, E-S, Leon, M. B., Shawl, F., Finkel, T., and S. E. Epstein. 1994. Potential role of human cytomegalovirus and p53 interaction in coronary restenosis. Science 265:391-394. [DOI] [PubMed] [Google Scholar]
- 32.Streblow, D. N., C. Kreklywich, Q. Yin, V.T. dela Melena, C. L. Corless, P. A. Smith, C. Brakebill, J. W. Cook, C. Vink, C. A. Bruggeman, J. A. Nelson, and S. L. Orloff. 2003. Cytomegalovirus-mediated upregulation of chemokine expression correlates with the acceleration of chronic rejection in rat heart transplants. J. Virol. 77:2182-2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Streblow, D. N., C. Soderberg-Naucler, J. Vieira, P. Smith, E. Wakabayashi, F. Ruchti, K. Mattison, Y. Altschuler, and J. A. Nelson. 1999. The human cytomegalovirus chemokine receptor US28 mediates vascular smooth muscle cell migration. Cell 99:511-520. [DOI] [PubMed] [Google Scholar]
- 34.Umehara, H., E. T. Bloom, T. Okazaki, N. Domae, and T. Imai. 2001. Fractalkine and vascular injury. Trends Immunol. 22:602-607. [DOI] [PubMed] [Google Scholar]
- 35.Umehara, H., and T. Imai. 2001. Role of fractalkine in leukocyte adhesion and migration and in vascular injury. Drug News Perspect. 14:460-464. [DOI] [PubMed] [Google Scholar]
- 36.Umehara, H., E. T. Bloom, T. Okazaki, Y. Nagano, O. Yoshie, and T. Imai. 2003. Fractalkine in vascular biology. Arterioscler. Thromb. Vasc. Biol. 23:1-8. [DOI] [PubMed] [Google Scholar]
- 37.Valantine, H. A., S.-Z. Gao, S. G. Menon, D. G. Renlund, S. A. Hunt, M. D., P. Oyer, E. B. Stinson, B. W. Brown, T. C. Merigan, and J. S. Schroeder. 1999. Impact of prophylactic immediate posttransplant ganciclovir on development of transplant atherosclerosis: a post hoc analysis of a randomized, placebo-controlled study. Circulation 100:61-66. [DOI] [PubMed] [Google Scholar]
- 38.Vieira, J., T. J. Schall, L. Corey, and A. P. Geballe. 1998. Functional analysis of the human cytomegalovirus US28 gene by insertion mutagenesis with the green fluorescent protein gene. J. Virol. 72:8158-8165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Waldman, W. J., J. D. LeClaire, and D. A. Knight. 2002. T-cell activation response to allogenic CMV-infected endothelial cells is not prevented by ganciclovir or foscarnet: implications for transplant vascular sclerosis. Transplantation 73:314-318. [DOI] [PubMed] [Google Scholar]
- 40.Wong, B, W., D. Wong, and B. M. McManus. 2002. Characterization of fractalkine (CX3CL1) and CX3R1 in human coronary arteries with native atherosclerosis, diabetes mellitus, and transplant vascular diseases. Cardiovasc. Pathol. 11:332-338. [DOI] [PubMed] [Google Scholar]
- 41.Yoneda, O., T. Imai, S. Goda, H. Inoue, A. Yamauchi, T. Okazaki, H. Imai, O. Yoshie, E. T. Bloom, N. Domae, and H. Umehara. 2000. Fractalkine-mediated endothelial cell injury by NK cells. J. Immunol. 164:4055-4062. [DOI] [PubMed] [Google Scholar]
- 42.Zhu, J., G. M. Shearer, J. E. Norman, L. A. Pinto, F. M. Marincola, A. Prasad, M. A. Waclawiw, G. Csako, A. A. Quyyumi, and S. E. Epstein. 2000. Host response to cytomegalovirus infection as a determinant of susceptibility to coronary artery disease: sex-based differences in inflammation and type of immune response. Circulation 102:2491-2496. [DOI] [PubMed] [Google Scholar]
- 43.Zhou, Y. F., M. B. Leon, M. W. Waclawiw, J. J. Popma, Z. X. Yu, T. Finkel, and S. E. Epstein. 1996. Association between prior cytomegalovirus infection and the risk of restenosis after coronary atherectomy. N. Engl. J. Med. 335:624-630. [DOI] [PubMed] [Google Scholar]