Abstract
Over the past few decades, significant progress has been made with respect to new concepts about the pathogenesis of osteoarthritis (OA). This article summarises some of the knowledge we have today on the involvement of the subchondral bone in OA. It provides substantial evidence that changes in the metabolism of the subchondral bone are an integral part of the OA disease process and that these alterations are not merely secondary manifestations, but are part of a more active component of the disease. Thus, a strong rationale exists for therapeutic approaches that target subchondral bone resorption and/or formation, and data evaluating the drugs targeting bone remodelling raise the hope that new treatment options for OA may become available.
Keywords: subchondral bone, osteoarthritis, articular tissues
Introduction
Bone remodelling is continuously maintained through a tight equilibrium between osteoblast activity responsible for the bone formation through the synthesis of bone matrix and an osteoclast activity accountable for degrading the bone microenvironment. The equilibrium between the activities of these two cells preserves the mineral component of calcium and phosphorous molecules. Bone remodelling includes several distinct phases, namely the activation, resorption, reversal and formation processes [1–3]. In this cycle, several components, including the specific cells, the osteoblasts, osteocytes and osteoclasts; inorganic non-collagenic substances, such as proteoglycans; and a collagenic component of which collagen type I is the major constituent, are all closely modulated. Mechanical force and stress induce bone alterations, in which osteoclast precursors and mature osteoclasts are recruited from the circulation to the bone-remodelling unit, thereby initiating the mineralised matrix resorption. Following this process, osteoclasts undergo apoptosis, leaving an opening for osteoblasts to invade and build up a new extracellular matrix.
Osteoclasts are derived from the haematopoietic progenitors of the monocyte–macrophage lineage and can be distinguished by their multinucleated giant cell appearance together with specific features such as polarised morphology and an apical differentiation adjoining the calcified matrix in resorption (ruffled border) [1–3]. They are responsible for the acidification of the extracellular matrix followed by the release of proteolytic enzymes, which leads to the breakdown of the bone matrix. The osteoblasts are derived from bone marrow cells and are responsible for the production of new matrix [1–3].
Osteoarthritis
Several tissues of the joint, including the cartilage, the synovial membrane and the subchondral bone, play significant roles in the development/progression of osteoarthritis (OA) pathology [4]. Although articular cartilage breakdown is a major characteristic of OA and synovial membrane inflammation also actively participates in the progression of the joint tissue lesions, the precise mechanism initiating its degradation is still unknown. During the initiation/progression of OA, sub-chondral bone is the site of numerous dynamic morphological transformations due to an altered osteoblast metabolism, which are part of the pathological process. Most importantly, subchondral bone remodelling in OA progresses from increased bone resorption early on to bone accretion, resulting in sclerosis of this tissue. In a primate model of spontaneous OA, increased osteoid volume is often more severe than cartilage changes [5]. Moreover, in this animal model, the severity of cartilage fibrillation and loss generally exceeds bone changes only in advanced OA. Although it has been shown in some induced OA animal models, which allow chronological analysis of the disease progression, that the subchondral bone changes precede cartilage changes [6–9], this has yet to be clarified in humans.
However, in situ structural changes in subchondral bone during the course of OA can now be readily observed using imaging techniques. Indeed, magnetic resonance imaging (MRI) revealed the presence of bone marrow lesions (hypersignal), which increased in size gradually over time [10–12]. Using this technology, the presence of oedema-like lesions in subchondral bone marrow and bone attrition were found to be strong indicators of bone turnover indices as well as structural deterioration in knee OA.
Moreover, a study performed using the anterior cruciate ligament (ACL) transection OA dog model showed that, in general, bone marrow hypersignal as assessed by MRI is topographically associated with cartilage lesions as seen macroscopically [13]. Data also revealed that the loss of cartilage volume/thickness and the deterioration of the subchondral bone structure were interdependent in longitudinal studies in knee OA patients [12,14]. The loss of cartilage, subchondral bone alterations and osteopenia of the underlying trabecular bone were all correlated in some of these patients. Using radiographs in a cross-sectional study, Beuf et al. [15] also demonstrated that the loss of trabecular bone in the femurs of OA patients correlated with the severity of the disease as assessed by the radiography-based Kellgren–Lawrence scale. Interestingly, such hypersignal bone lesions were recently evaluated histologically and appear to correspond mainly to fibrosis, myxoedematous degeneration and/or cellular infiltrate of the bone marrow [16]. Altogether, these findings strengthen the hypothesis that the subchondral bone changes may play a role in the genesis of cartilage lesions.
Subchondral bone remodelling
Early phase of OA: subchondral bone resorption
It is believed that alterations in subchondral bone activity occur quite early in the OA process. Although bone sclerosis is considered a hallmark of OA, subchondral bone indices of resorption were found in patients with progressive knee OA. This suggests that such alterations in the OA subchondral bone have an impact on both the quality and quantity of this tissue. The early bone resorption features observed in OA patients were carefully assessed in a subset of knee OA patients from the Chingford study [17] by measuring markers of bone resorption, such as urinary N-terminal type I collagen telopeptides (NTX) and C-terminal type I collagen telopeptides (CTX), at three different time points. Patients with progressive worsening of the knee showed bone resorption but those with non-progressive OA did not.
Correlation between in vivo findings in animals and human OA patients
Animal models of OA show that the indices of bone resorption are increased early in the disease process and that bone formation is a relatively late phenomenon. In a guinea pig model, bone densitometry evaluation following meniscectomy revealed typical variations in bone metabolism with early resorption of subchondral bone followed by increased bone density [18]. This concurs with findings from other animal models, such as the ACL dog and rat OA models, in which were observed, at an early stage of the disease process, increased subchondral bone resorption with trabecular thickness reduction and an increased number of osteoclasts, as well as increased production of catabolic factors including cathepsin K and matrix metalloproteinase (MMP)-13 [6–9].
Later phase of OA: subchondral bone sclerosis
As mentioned above, studies have also demonstrated that as the disease progresses, or at a later stage of OA, subchondral bone becomes sclerotic. Using quantitative microfocal radiography, Buck-land-Wright et al. [19,20] showed that the changes in OA joints also involve thickening of the sub-chondral cortical plate. In the ACL dog model of OA, Brandt et al. [6] reported that, at a later stage of the disease, 54 months after OA induction, there was a marked increase in the volume of subchondral bone with active bone formation. Studies in OA of the knee and the hand reported that the scintigraphic abnormalities correlated with the osteocalcin concentration in the synovial fluid, which is a marker of bone formation, and serum osteopontin, a bone matrix protein, were also elevated [21–23]. Gevers and Dequeker also showed elevated serum osteocalcin levels in women with hand OA, and elevated osteocalcin in cortical bone explants [24]. Moreover, levels of growth factors such as insulin-like growth factor (IGF)-1 and -2 and transforming growth factor (TGF)-β1 are also higher in samples of iliac crest bone of patients with OA [25]. Considering that this bone is a non-weight-bearing site and at some distance from joints, this would suggest a generalised dysfunction in bone metabolism.
Subchondral bone sclerosis in OA appears to be due to an increase in material density, and not mineral density
Stiffness and bone mineral density (BMD) are not uniform in OA bone [26]. The bone closest to the articular cartilage has the greatest effect on cartilage integrity, with variations in stiffness and BMD probably causing more damage to cartilage than any other parameters under normal conditions [27,28]. Although OA at a later stage demonstrates a thickening of subchondral bone, explants of the femoral heads of OA patients at autopsy revealed a pattern of low mineralisation compared with that of normal [29,30]. Hence, the apparent increase in bone density in OA may be because of an increase in material density, and not mineral density [31–33]. Indications of altered mineralisation and abnormal metabolic subchondral bone can be inferred from the increased osteoid matrix in this OA bone tissue [24,32,34,35]. As the osteoid matrix is primarily composed of an abundant collagen type I matrix, it was therefore of no surprise that this collagen type in the trabecular bone of the femoral heads of OA patients was found to be increased [31,32], along with abnormal collagen type I fibres, as evidenced by an increased ratio of α1 to α2 chains in OA compared to normal trabecular subchondral bone [33]. Data also reported a two- to threefold increase in the expression of COL1A1 chains of type I collagen with no variations in COL1A2 expression in OA subchondral bone osteoblasts, leading to an increase in the production of type I collagen α1 chains [36]. Together with the reduced number of cross-links in OA bone tissue [32], this could explain the reduction in bone mineralisation. Moreover, data also showed an increase in osteocalcin and alkaline phosphatase in human OA subchondral bone both in vivo [24] and in vitro [37,38]. Hence, the early marker (alkaline phosphatase), terminal differentiation marker (osteocalcin) and the mineralisation of OA subchondral bone osteoblasts are altered.
Role of cells/factors in abnormal subchondral bone metabolism in osteoarthritis
Mesenchymal cells
Aspden et al. [39] proposed that the formation and activity of mesenchymal stem cell (MSC) precursor cells in OA skeletal tissues could be modified by systemic and/or local factors. One possibility was that one or more intrinsic cell functions are altered or that abnormal lipid metabolism leads to OA. In agreement with this concept, the same group showed abnormal lipid composition of trabecular bone from OA patients [40]. Moreover, they postulate that, if this is the case, the fate of MSCs in OA should be altered. Further data indeed revealed that the osteogenic potential of bone marrow cells from OA patients was increased compared with that from normal, whereas both the chondrogenic and adipogenic potential of these cells were blunted [41].
In vivo, the altered bone collagen matrix in OA bone tissue may contribute to induce the MSCs to differentiate into osteoblasts. The altered fate of MSCs may also result from an exposition to leptin, because it promotes the differentiation of these cells into osteoblasts while it inhibits adipocyte maturation [42]. This latter effect could also be linked with the collagenous extracellular matrix because leptin also directly stimulates the production of osteoblast markers and collagen [43]. Recent studies have also focussed attention on the potential direct contribution of mature osteoblasts/osteocytes to the recruitment and fate of MSCs via the Wnt signalling pathway. Indeed, the control of adipogenesis, osteogenesis and chondrogenesis in bone marrow may be regulated locally by Wnt agonists and antagonists produced by the mature osteoblast/osteocytes [44,45]. Osteocytes also contribute to local control of bone resorption through the production of the Wnt antagonist, sclerostin (SOST) [46,47]. It is, therefore, also of note that OA osteoblasts produce abnormal levels of Wnt antagonists Dickkopf (DKK)-2 and SOST, which are involved in terminal osteoblast differentiation and bone resorption, respectively [48,49]. Hence, in vivo alterations are likely due to changes in abnormal cellular metabolism and not to changes in systemic regulation.
Moreover, the Wnt/β-catenin signalling pathway is a normal physiological response to mechanical loading in bone [50], and hydrostatic pressure promotes Wnt10b and Wnt4 expression in early-osteoinduced MSCs [51]. Therefore, biomechanical forces in OA may have an impact on the biological response of MSCs and osteoblasts, and in the presence of an abnormal extracellular matrix, these forces would be improperly transmitted within the bone microenvironment.
Wnt
The key role of Wnt in the regulation of bone mass was discovered recently by identifying both activating and loss-of-function mutations in LRP5. Indeed, a single modification of an amino acid in the extracellular domain of LRP5 was linked to high bone mass with resulting weak activation of the β-catenin pathway [52–55]. Conversely, a loss-of-function mutation identified in both humans and mice results in low bone mass [56,57]. A weak association between haplotypes of the LRP5 gene indicates a risk factor for OA [58], and a single nucleotide polymorphism in secreted frizzled-related protein 3 (sFRP3) was identified in a group of females with hip OA [59], but not in knee OA. sFRP3 is an antagonist of the Wnt pathway and the polymorphism reduces the ability of sFRP3 to antagonise Wnt signalling, thereby suggesting that Wnt signalling might be elevated in OA. However, sFRP3 can decrease the proliferation and increase the differentiation of mature osteoblasts via a β-catenin-independent pathway [60].
Among the antagonists of Wnt signalling, DKK1 and DKK2 play key roles in osteoblast proliferation, differentiation and mineralisation. DKK1 is a master regulator of osteogenesis [61–63] whereas DKK2 acts as a fine-tuning regulator of osteoblast proliferation, terminal differentiation and mineralisation [49]. Lastly, SOST is an osteocyte-derived negative regulator of bone formation. A loss-of-function mutation of SOST was identified in sclerosteosis patients [64] who show progressive bone thickening and generalised osteosclerosis. SOST was believed to be a bone morphogenic protein (BMP) antagonist because it inhibits BMP-stimulated bone formation, yet it cannot antagonise all BMP responses [47,65]. Moreover, Wnt proteins induce BMPs, a mechanism inhibited by SOST, indicating that SOST may be a canonical Wnt signalling inhibitor, and that BMP activity is required downstream of a Wnt stimulus [65–68]. Of note, our group recently reported [48] that a member of the DKK family, DKK2, a Wnt antagonist, was responsible for the altered phenotype of human primary OA osteoblasts.
IGF and TGF-β1
IGFs are important growth factors that regulate bone formation. OA subchondral bone osteoblasts produce variable total IGF-1 levels and less IGF-binding proteins compared with normal [69]. This results in higher levels of free IGF-1 that could promote bone remodelling and increase bone stiffness, a situation that exacerbates cartilage matrix degradation. TGF-β1 and IGF-1 are also involved in matrix deposition and turnover, with TGF-β1 stimulating matrix synthesis, but, as mentioned above, leading to an abnormal type I collagen α chain ratio and collagenase activity, whereas IGF-1 inhibits matrix degradation in bone cells [70]. It is worth mentioning that a study in mice showed that intra-articular injections of TGF-β into the knee joint induced OA-like changes [71] and that blocking endogenous TGF-β production during experimental OA prevents osteophyte formation [72]. The localised effect of TGF-β and IGF-1 may be linked to an abnormal response to leptin by OA subchondral bone osteoblasts. This may occur as the expression of leptin stimulates TGF-β and IGF-1 in joint tissues [73].
Recent evidence further indicates that abnormal TGF-β1 levels can directly affect subchondral bone tissue quality in OA by altering mineralisation. Indeed, Couchourel et al. [36] recently demonstrated that OA subchondral bone osteoblasts fail to mineralise normally, whereas correcting their endogenous TGF-β1 levels by sustained inhibition enhanced their mineralisation. Moreover, these authors [36] also showed that inhibiting TGF-β1 expression induced a correction of the abnormal ratio of type I collagen α1 to α2 chains observed in OA subchondral bone osteoblasts.
OPG/RANK/RANKL
In the context of bone resorption, a molecular triad composed of osteoprotegerin (OPG), receptor activator of nuclear factor-κB (RANK) and RANK ligand (RANKL), members of the tumour necrosis factor superfamily, has been described as a key cytokine system involved in the differentiation and function of osteoclast cells [74–78].
In the bone remodelling process, the factors of this triad are closely linked to each other. RANKL is expressed in either membranous or soluble form, primarily by the osteoblastic lineage cells, and is essential for mediating bone resorption through osteoclastogenesis and the activation of mature osteoclasts. RANKL stimulates osteoclastogenesis and osteoclast activity by binding to the cell surface receptor RANK, located on precursor and mature osteoclasts. The binding of RANKL to the extracellular RANK domain leads to the activation of specific signalling pathways involved in the formation and survival of osteoclasts, hence bone resorption. The third protagonist, OPG, is secreted by the stromal cells and other cell types, including osteoblasts, and acts as a soluble decoy receptor for RANKL. OPG, by interacting with RANKL, inhibits the binding of RANKL to RANK, thereby blocking RANK activation and subsequent osteoclastogenesis.
Investigation of this molecular triad in human OA subchondral bone osteoblasts revealed that these cells could be discriminated into two subgroups based on their having either a low or a high OPG/ RANKL ratio [79]. Moreover, investigation of the ability of each subgroup to induce osteoclast differentiation demonstrated that the OA subchondral bone osteoblasts with a low OPG/RANKL ratio induced a greater number of mature osteoclasts compared with the high OPG/RANKL ratio OA osteoblast subgroup [79]. Hence, these OA subpopulations could favour bone resorption or bone formation, respectively. Interestingly, in situ histological evaluation of the subchondral bone in each subgroup of OA patients compared with normal individuals suggested that the OA subgroup with a low OPG/RANKL ratio showed reduced subchondral bone thickness, and the OA subgroup with high OPG/RANKL ratio showed increased thickness [79].
Ephrin system
Recently, a system composed of the ephrin ligands and their specific receptors Eph has been described for its ability to control bone remodelling [80]. Two subclasses of Eph receptors have been defined according to their preferred ligand specificity, namely type A receptors (EphA) which bind to ephrins A, and type B receptors (EphB) which bind to ephrins B. However, there are some exceptions in which, for example, an ephrin B binds to an EphA receptor. The two populations of ephrins differ in their anchorage: ephrins A are composed of a GDI anchor, while ephrins B possess a single transmembrane domain.
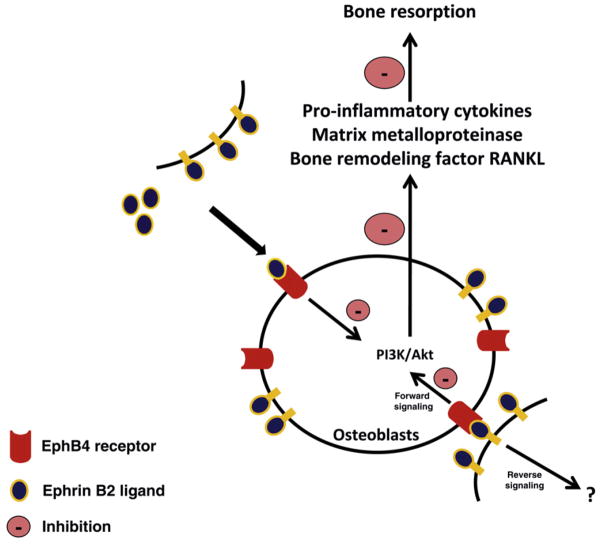
Both ephrins and Eph receptors are cell-membrane-bound proteins and their interaction leads to a bidirectional (osteoblast/osteoclast) Eph/ephrin signalling (Fig. 1). In this particular situation, signalling through EphB receptors is considered forward and, through ephrin B ligands, reverse signalling [80]. Interestingly, it was recently demonstrated that ephrin B2, mainly expressed by osteoclasts, and its specific receptor EphB4, expressed by osteoblasts, are involved in the control of bone homeostasis in which the EphB4 forward signalling favours an osteoblast differentiation process, whereas the reverse signalling through ephrin B2 ligands leads to an inhibitory effect on the osteoclast function. The overall outcome of such an interaction favours bone formation [80].
Fig. 1.
Interaction between the EphB4 receptor and ephrin B2 ligand leads to both a forward and a reverse signaling. The signal through the EphB4 receptor is considered a forward signal whereas the reverse signaling is through the ephrin B2 ligand. In OA subchondral bone osteoblasts, the activation of EphB4 receptor by ephrin B2 results in a decreased activation of PI3K/Akt which, in turn, inhibits some pro-inflammatory cytokines and matrix metalloproteinases as well as RANKL, all of which are involved in the remodeling process of the OA subchondral bone [81].
As mentioned above, OA subchondral bone osteoblasts can be discriminated as pro-resorptive or pro-formative. Interestingly, these two subgroups were also found to differentially express EphB4 receptors and ephrin B2. Those showing pro-resorptive properties showed a higher level of EphB4 receptors and ephrin B2, while those in a pro-formation phase had EphB4 receptor and ephrin B2 ligand expression levels similar to the normal subchondral bone osteoblasts [81]. Although not yet tested, the increased levels of these factors in the pro-resorptive osteoblasts would suggest an attempt by these cells to regulate their resorption activity. In the other OA osteoblast subpopulation, an increase in these factors would not be required, as these cells are in a pro-formation phase. This concurs with further data showing that in pro-resorptive osteoblasts, treatment with ephrin B2 ligands induced a reduction in the bone resorption process as well as in various catabolic mediators, including the inflammatory factors interleukin (IL)-1β and -6; the MMPs -1, -13 and -9; and RANKL [81]. This process appears to occur through an inhibition of the PI3K/Akt signalling pathway.
Other factors
OA subchondral bone osteoblasts were shown to produce less cAMP in response to parathyroid hormone (PTH) stimulation [37], and they have fewer PTH receptors [82]. Since PTH is a negative regulator of collagen synthesis, this could then lead to altered type I collagen production in OA bone tissue [83,84].
An abnormal degradation of the extracellular matrix could also potentially lead to an alteration in OA subchondral bone tissue, as it orchestrates interactions of osteoblasts with neighbouring cells, and changes in matrix composition may alter cell function and communication. In this context, two MMPs, -2 and -9, were found to be elevated in proximal cancellous bone tissue isolated from the femoral heads of OA patients [32], a situation that may be linked to abnormal collagen matrix deposition.
Interaction between subchondral bone and cartilage
It is currently suggested that factors produced locally in subchondral bone can act on chondrocytes in the articular cartilage. However, the question arose as to how these factors could reach the overlying cartilage. The possibility of diffusion of molecules/factors from the subchondral bone to the articular cartilage was evaluated when it was observed that the elastic modulus (stiffness) of the subchondral bone was reduced locally due to an increase in vascularisation and in the remodelling rate [85]. These changes would then lead to reactivation of the secondary ossification centre and a decrease in cartilage thickness [86], suggesting that the altered subchondral bone remodelling or turnover would initiate cartilage degradation. This is possible as clefts and channels in the tidemark were seen early on in OA as well as fatigue microcracks in articular cartilage [87–91].
Nutrients must enter articular cartilage either from the surface, through the synovial fluid, or from the underlying subchondral bone, because healthy cartilage is considered avascular. Although it was initially believed that synovial fluid was the only nutrient route due to the absence of an anatomical barrier and because the cartilage cannot survive when not nourished by the synovial fluid [92], this concept was recently challenged. Indeed, cartilage can degenerate even when in contact with normal synovial fluid; hence, nutrient supply through the subchondral bone may seem obvious. Conversely, it can be argued that the dense calcification in the basal zone of normal articular cartilage constitutes an insurmountable barrier to solute and fluid diffusion. Interestingly, when cartilage was deprived of contact with subchondral bone for a long period in the baboon, the cartilage degenerated as in OA [93]. Therefore, both routes of nutrient entry may co-exist.
In the spontaneous OA guinea pig model, the severity of articular lesions and progression of the disease were also increased in animals with the highest bone turnover rate [94]. Hence, the state of OA subchondral bone at any given time point would be less important than tissue homeostasis and turnover to the appearance and progression of OA, which indicates the dynamic nature of the disease. The response to the biomechanical alterations of the subchondral bone tissue at any time point would then induce local responses that contribute to thinning of the articular cartilage. This would then further contribute to shear stress and lead to complete cartilage loss.
Nonetheless, what triggers the initial cartilage damage is still speculative. As mentioned above, some studies have indicated that subchondral bone changes precede and may be responsible for the evolution of cartilage lesions [29,95,96]. Others have indicated that subchondral bone changes would only be secondary to cartilage degradation [97,98]. Although the pathways involved in cross-talk between subchondral bone and cartilage remain largely unknown, some factors synthesised by sub-chondral bone cells are capable of inducing metabolic changes in the cartilage.
Potential factors in subchondral bone/cartilage cross-talk
Bone produces a number of factors that are involved in both tissue remodelling and the modulation of cartilage catabolism. Hence, subchondral bone tissue may, through the production of cytokines, growth factors and eicosanoids, induce OA cartilage degradation [98–100]. Interestingly, in addition to the subchondral bone cells, the OPG/RANK/RANKL molecular triad has also been observed to be expressed and produced by another articular cell, the chondrocyte. Recent findings showed that human chondrocytes express and produce these factors and that treatment of these cells with OPG results in increased levels of two catabolic factors involved in cartilage pathophysiology, MMP-13 and proteinase-activated receptor (PAR)-2 [101]. However, treatment with RANKL did not show any effect. This could reflect the fact that RANK was shown to be produced by only 29% of OA chondrocytes localised throughout human cartilage [101].
Ephrin B2 and its specific receptor EphB4 were also found to be expressed by human chondrocytes and treatment with ephrin B2 also positively impacts on the abnormal metabolism of OA cartilage by inhibiting IL-1β, -6, MMP-1, -9, -13 and PAR-2 levels and increasing collagen type II gene expression [102].
The hepatocyte growth factor (HGF) may also be involved in the cross-talk between the two tissues. Indeed, HGF is expressed and produced in human subchondral bone osteoblasts and at a higher level in OA, whereas only the protein, not the gene, is detected in articular cartilage in OA patients, and only in the lower intermediate and deep layers [103–105], thus suggesting that subchondral bone osteoblasts may be responsible for the HGF found in OA cartilage. Moreover, HGF induces MMP-13, an enzyme involved in OA cartilage degradation [106] and mostly present in the intermediate and deep layers of articular cartilage [107], the same site where HGF is detected.
Bone markers in OA
One of the fundamental problems with OA was the absence of validated markers that could predict the disease or permit follow-up of affected individuals. Indeed, although OA is a prevalent chronic health condition, its diagnosis is based on the clinical assessment and/or conventional radiography that is considered the gold standard, with radiographic changes such as joint-space narrowing and osteophyte formation that appear rather late during the disease process. This radiography approach has inherent limitations, one of which is that it can only detect an advanced stage of the disease in patients and cannot be used to determine early or subtle changes over time. However, imaging methods other than radiography were recently used to detect markers or risk factors for this disease. The literature reveals that MRI is very useful for the assessment of disease activity and the determination not only of disease progression but also of early events [10,11]. In this context, meniscal lesions and bone marrow oedema were demonstrated to be important risk factors for OA progression [12,108].
Individual markers were measured in a number of clinical studies and some indicated correlation with disease activity or progression, but not initiation of OA. These included studies measuring degradation and/or turnover products from cartilage, bone or the synovial membrane [109–114]. Indeed, the focus has been drawn away from the initial determination of individual markers such as hyaluronic acid (HA), C-telopeptide of type II collagen (CTX-II), cartilage oligomeric matrix protein (COMP), sulphate (KS)-5D4, urinary type II collagen-related epitopes, TGF-β1 and type II procollagen carboxy-propeptide (CPII), which are all excellent to determine patients at greatest risk of progression or to discriminate patients with more severe OA from those with less severe OA [109,110,115]. However, these markers could not discriminate either initiation or activity of the disease per se. More sophisticated determination of chondroitin sulphate (CS) epitope WF6 was also done in both OA and rheumatoid arthritis patients. However, as the levels of both HA and WF6 were elevated in patients with these two diseases, a strict correlation with disease activity was not fully validated [116]. As the involvement of bone tissue was also becoming recognised in the initiation and/or progression of OA, biochemical markers of bone turnover were also determined in some clinical studies. More specifically, serum C-terminal cross-linked telopeptide of type I collagen (CTX-I), serum osteocalcin, glucosyl–galactosyl–pyridinoline (Glc-Gal-PYD) and the cartilage marker CTX-II as determined in the MRC Hertfordshire Cohort [117] indicated a strong association with knee OA as assessed by the Kellgren–Lawrence scale. By contrast, no individual association could be found for serum osteocalcin or serum CTX-I.
Whereas these studies were very useful in identifying targets to monitor patient outcomes in clinical studies and progression of the disease in response or not to specific treatments, individual markers, such as those reflecting cartilage degradation, synovial inflammation or bone turnover, were not very informative on their own, and they failed to determine the disease initiation. In recent years, however, the trend has shifted from assessments of individual markers to uncovering clusters of markers that may correlate with disease progression and activity. Indeed, it was recently demonstrated, using an approach based on the association of selected biochemical markers combined into a single factor, that a combined panel of biochemical markers showed a stronger association with OA than any individual markers [118]. Moreover, their analysis also suggested that markers identifying patients with osteophytes overlapped those with a high Kellgren–Lawrence score while markers for BMD of the subchondral bone were uncovering a totally different group, hence raising the possibility that although osteophytes and subchondral BMD are associated with OA, they may have underlying biological differences. Likewise, a study by Meulenbelt et al. [119] also demonstrated that combining biochemical markers was more sensitive at detecting subtle changes in different OA patients, that cartilage and bone turnover markers were more sensitive at detecting OA, particularly hip OA, whereas markers of inflammation correlated with knee OA, and that the changes in cartilage turnover markers correlated with hand and spine OA. Other studies also suggested an imbalance between bone formation and bone resorption indices in OA patients and, more specifically, identified increases in OPG and soluble RANKL (sRANKL). These increases actually led to an increased sRANKL/OPG ratio, which should favour bone resorption in OA patients, and correlated with disease severity [120].
However, these studies still failed to uncover any specific markers that could relate to early events and therefore be predictive of OA initiation. This was recently challenged by a new study that identified biochemical markers that may actually accompany early OA and precede radiographic changes by almost 10 years. Indeed, Ling et al. [121] used a microarray platform that simultaneously tested 169 proteins relevant to inflammation, cell growth, activation and metabolism in a case-control study. They identified 16 proteins that were different between OA patients and control subjects who had not developed OA. Four of these markers associated with cell activation, inflammation and bone collagen degradation were already different 10 years prior to radiographic classification of the individuals as having OA and were still different at the time of diagnosis. Six more proteins were clearly associated with subsequent development of OA. A recent study by Cibere et al. [122] also reported that individual markers could be useful nevertheless, that the usefulness of these markers depended on the stage of OA and that ratios of a combination of markers were more informative.
Therefore, although studies are indicating that individual markers may be suitable for following patients or determining the outcome of specific intervention (Table 1), clusters of biochemical markers appear to be a much more promising avenue for identifying patients at the initiation of the disease (Table 2). These markers alone or in combination with MRI data would then provide a means to identify those patients at risk much earlier, with the possibility of intervention. The prospect of detecting those patients at risk of developing OA may then be useful for testing disease-modifying OA drugs as they become available.
Table 1.
Individual markers of OA progression and initiation.
| Markers of OA progression [109–113,115–117] |
| Hyaluronic acid |
| C-telopeptide of type II collagen (uCTX-II) |
| Cartilage oligomeric matrix protein |
| Keratan sulfate KS-5D4 |
| Urinary type II collagen-related epitopes (uC2C) |
| Transforming growth factor β-1 |
| Type II procollagen carboxy-propeptide |
| Chondroitin sulfate epitopes WF6 |
| Serum C-propeptide of type II procollagen (sCPII) |
| Markers of pre-ROA* [122] |
| uCTX-II:sCPII |
| uC2C:sCPII |
| Miscellaneous markers [109,117,120] |
| Serum C-terminal crosslinked |
| Telopeptide of type I collagen (CTX-I) |
| Serum osteocalcin |
| Glucosyl-galactosyl-pyridinoline |
| OPG;OPG/RANKL ratio |
ROA: radiographic OA.
Table 2.
Clusters of markers used together for the detection of OA.
| Cluster of markers of pre-ROA* [121] |
| Matrix metalloproteinase (MMP)-7 |
| Soluble vascular adhesion protein (sVAP)-1 |
| Interleukin (IL)-15 |
| Plasminogen activator inhibitor (PAI)-1 |
| MMP-2 |
| D-dimers (DD)5 and DD6 |
| Eotaxin-2 (Eot-2) |
| Intracellular adhesion molecule (ICAM-1) |
| P-selectin |
| Cluster of markers of early ROA [121] |
| B-lymphocyte chemokine (BLC) |
| 6-chemokine (6Ckine) |
| Macrophage inhibitory protein (MIP)1α |
| IL-1α |
| IL-2 |
| Fibroblast growth factor (FGF)-7 |
| Insulin-like growth factor (IGF) binding protein-2 |
| Granulocyte macrophage colony stimulating factor (GM-CSF) |
| Neurotrophin-4 (NT-4) |
| ICAM-3 |
| Vascular endothelial (VE)-cadherin |
| Cluster of markers of ROA and other indications [119] |
| uCTX-1;u-CTX-II;OC;Glc-Gal-PYD Bone turnover |
| HsCRP; high BMI Inflammation |
ROA: radiographic OA.
Therapeutics targeting osteoarthritic subchondral bone
The findings demonstrating a remodelling process in the subchondral bone during the OA pathophysiology has raised the question as to whether factors capable of influencing bone metabolism could be used as therapeutic strategies targeting this tissue in OA patients. In this context, a number of studies, most using OA animal models, have explored the effects of drugs/agents that can modulate bone metabolism, but to date only a few have undergone human clinical trials.
Future prospects
OPG and anti-RANKL
As mentioned above, the factors OPG and RANKL are highly involved in the control of bone biology. The pro-resorptive effect of RANKL on the osteoclastogenesis process could therefore be targeted by the use of either OPG or an anti-RANKL antibody. A recent study carried out in an experimental mouse model of OA revealed, upon OPG administration, reduced cartilage degradation through an effect on trabecular bone [123]. In the same line of thought, data from an OPG transgenic mouse model of OA suggested that the in vivo beneficial effect of the administration of OPG could be due to its capacity to bind tumour necrosis factor-related apoptosis-inducing ligand (TRAIL), an inducer of chondrocyte apoptosis [124]. However, data generated from an in vitro study in which treatment of human OA chondrocytes with OPG enhanced two catabolic factors involved in the pathophysiology of the disease [101] suggest that targeting the factor that mediates the effect of OPG, for example, by inhibiting RANKL, could lead to a new therapeutic approach against OA. Such inhibition of RANKL has been proposed as a therapeutic approach in some osteolytic diseases [125,126]. It is thus plausible that therapies interfering with both cartilage and subchondral bone simultaneously could block, or at least attenuate, the progression of OA. The potential of RANKL inhibition as a disease-modifying drug is thus very appealing. However, only appropriate clinical trials will be able to provide the information needed to address this important question.
Ephrin B2/EphB4 receptors
In vitro findings showing that ephrin B2 treatment in human OA subchondral bone and chondrocytes could positively impact on the abnormal metabolism of these diseased cells [81,102] suggest that enhancing this system could lead to a protective effect on the structural changes in these OA tissues.
Drugs/agents that target bone remodelling
Bisphosphonates
Following the line of thought that an active remodelling process occurs in OA subchondral bone and that such phenomenon could contribute to the cartilage degeneration and disease progression, anti-resorptive substances such as bisphosphonates would seem well suited against the progression of OA. Bisphosphonates are among the most commonly used drugs for the treatment of diseases involving excessive resorption of bone, such as osteoporosis.
Studies using different animal models were first conducted with alendronate. In the rat ACL transection model, alendronate demonstrated chondroprotective effects with osteophyte formation inhibition and reduction in cartilage degradation biomarkers [7]. However, different results were obtained with this drug in the spontaneous guinea pig model, in which alendronate increased the bone mineral content and density, which was associated with the acceleration of cartilage degradation [127]. Interestingly, another bisphosphonate, risedronate, when tested in the same model, showed a positive effect on the progression of OA, reducing the size and severity of cartilage lesions and limiting osteophyte formation [128]. In this latter study, a comparison between risedronate and alendronate revealed the former to be more effective. Furthermore, a comparative study among different bisphosphonates revealed that only the compounds containing nitrogen and pyridinyl side chains positively affect cartilage structure [129]. In the ACL dog model of OA, the morphological changes that take place at the subchondral bone level, particularly in the early phase of the disease, are predominantly resorptive in nature. A study in this model using NE-10035, a bisphosphonate administered through subcutaneous injection, showed that over 3 months following surgery, the prophylactic treatment effectively reduced the turnover and resorption of subchondral bone in the OA joint [130]. However, the treatment had no effect on osteophyte formation or the severity of cartilage changes.
In a phase II clinical trial in knee OA patients, oral treatment with risedronate was shown to decrease CTX-II production [131]. However, in a phase III trial, risedronate failed to show any disease-modifying effect in such patients [132]. The reasons for the failure of such trials could be multiple. One reason may be that for treatment to be effective the drug should be administered during the early stages of OA. Moreover, the imaging technology (X-ray) used in these investigations may not have been optimal for assessing a disease-modifying effect. Indeed, data have shown that a few thousand OA patients would be required to demonstrate a statistically significant effect using X-ray technology [132].
Strontium ranelate
Strontium ranelate is a newly developed drug that induces an increase in bone mass and an amelioration of bone architecture. Strontium ranelate is an approved treatment for osteoporosis, reducing the risk of both vertebral and hip fractures. Strontium ranelate acts on both bone formation indices and bone resorption indicators. Indeed, strontium ranelate prevents trabecular bone loss, decreases bone resorption and increases or maintains bone formation in the ovariectomised rat model or in rats subjected to hindlimb immobilisation [133,134]. Strontium ranelate also reduces bone resorption and enhances bone mass and strength in mice, rats and monkeys [135–137]. In in vitro studies, strontium ranelate also directly reduced osteoclast differentiation and resorption, whereas it increased pre-osteoblast replication and differentiation [138–142]. Preclinical studies in normal and osteopenic animals provided evidence that the dissociation of bone formation and resorption induced by strontium ranelate have beneficial effects on bone mass and bone quality (i.e., microarchitecture, geometry and intrinsic properties), resulting in a positive bone balance.
Although the role of strontium ranelate in related skeletal diseases is yet unknown, the effect of the properties of this drug on bone metabolism supports a potentially important role of promoting sub-chondral bone tissue homeostasis in OA patients. A phase III clinical study is presently underway to test the potential joint-structure-modifying effect of this drug in knee OA patients.
Calcitonin
Additional bone-active agents studied include salmon calcitonin [143]. Calcitonin is a well-known bone anti-resorptive agent that has demonstrated its efficacy in the treatment of osteoporosis and Paget’s disease. Salmon calcitonin was administered daily for 1–8 weeks or from weeks 8 to 16 in the cruciate deficiency rabbit model [143]. The calcitonin-treated groups demonstrated smoother cartilage with minimal or no ulcerations, smaller osteophytes and hypercellularity where mild OA was present, suggesting regeneration. The investigators suggested that calcitonin worked in both prophylactic and therapeutic stages of OA. Studies in the ACL dog model [144,145] also showed that subcutaneous injections of calcitonin under therapeutic conditions reduced the progression of OA cartilage and subchondral bone changes as well as the level of serum markers of bone resorption up to 4 months after the surgery. A small phase II trial assessing the efficacy of oral salmon calcitonin in knee OA was recently published [146]. Results showed an improvement in function scores as well as a reduction in some biomarker levels. While this study was not analysed as an intention to treat and the sample size was not sufficiently powered, its promising results will perhaps lead to further larger trials.
Cathepsin K inhibitors
Cathepsin K is the most abundant cysteine protease expressed in the osteoclast, and it has been shown to play a critical role in the degradation of type I collagen containing bone matrix. This protease has also been demonstrated to be involved in OA cartilage degradation and subchondral bone alterations [8,147]. Transgenic mouse models have provided evidence supporting its important role in arthritis. Interestingly, cathepsin K is one of the few non-collagenase enzymes capable of degrading native fibrillar collagen types I and II [148]. Owing to the lack of adequate cross reactivity between the rat and human isoenzymes, animal models using cathepsin K inhibitors have been developed mostly in monkeys, and data have shown that inhibiting cathepsin K results in the prevention of bone loss. Majority of the clinical trials were phase II and almost all investigated the effect on BMD. To the authors’ knowledge, one clinical phase II study was started in OA patients. Those clinical trials were stopped due to adverse events, which included skin changes. Inhibition of cathepsin K could be an interesting candidate for OA as it could act on both cartilage and subchondral bone remodelling, provided that no safety issues arise in phase II and phase III studies.
Oestrogen
The effects of oestrogen on tissues such as bone have been extensively studied, and the pleiotropic effects of the female sex hormone are well established. Cartilage is not generally viewed as an oestrogen-responsive tissue. However, several epidemiological studies support the hypothesis that oestrogen may play a role in OA. Accordingly, the issue of chondroprotective properties of oestrogen has recently received increased attention. Treatment with oestrogen and a selective oestrogen-receptor modulator (SERM) was tested in ovariectomised rats and in postmenopausal women. A recent review analysing the effect of oestrogen treatment on animal models of OA revealed that the effect was inconclusive in 11 out of 22 studies reporting a beneficial effect on cartilage, whereas six studies in which SERMs were administered after ovariectomy described protective effects [149]. In a recent clinical trial conducted for 2 years in postmenopausal women, Karsdal et al. [150] investigated if the administration of a synthetic steroid with oestrogenic, androgenic and progestogenic properties would have similar dual actions on both bone and cartilage turnover. Data from this trial suggest that bone resorption can be attenuated, however, without the positive effects on cartilage degradation. These findings indicate an uncoupling effect on bone and cartilage from the synthetic steroid, which could be due to the pharmacology and biological activity of the product on these tissues.
It is suggested that currently available hormone replacement therapy and SERMs in clinical practice should not be recommended as therapy for OA [151]. However, there is hope that new treatment options based on compounds acting through the oestrogen receptor could be efficacious.
Vitamin D
It is well known that there is a decline in the circulating level of vitamin D with ageing, which may contribute to a stimulation of bone remodelling. A vitamin D deficiency in adults can result in increased bone turnover, enhanced bone loss and increased risk of fragility fracture. Although vitamin D was also shown to be an important hormonal contributor to cartilage and chondrocyte homeostasis and vitamin D receptors are present in chondrocytes [152], its role in OA is far less understood and still controversial. Indeed, while some clinical studies reported that vitamin D deficiency was associated with an increased risk of progression of knee OA and incidence of hip OA [153,154], others demonstrated no association between serum vitamin D levels and joint space loss or worsening cartilage score in knee OA [155,156]. Most of these studies used radiographic assessment of OA and one also employed MRI. However, in the study using MRI [155], the authors did not assess the whole knee or cartilage volume. Interestingly, in a recent study [157] in which the assessment of knee OA structural changes was performed both radiographically and by quantitative MRI, a change in serum vitamin D level was positively associated with change in cartilage volume. Despite the fact that the mechanisms of the action of vitamin D on cartilage remain unclear, one may speculate that it may have a direct effect on cartilage through vitamin-D-specific receptors. Conversely, but not exclusive of the latter, an effect on the subchondral bone metabolism is also possible as the vitamin D levels in serum were also associated with reduced subchondral bone area [157], a known risk factors for knee OA.
To our knowledge, there is presently no clinical trial addressing the effect of vitamin D on joint structure changes in human OA. However, there is an ongoing phase IV clinical trial, conducted in Europe and the USA, in knee OA patients undergoing unilateral total knee replacement, evaluating the effect of two doses of vitamin D on the pain as well as rehabilitation.
Other therapeutics
Medications commonly prescribed for OA include analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids and viscosupplementation. However, patients are sometimes given complementary therapy. These complementary therapies include diacerein as well as nutraceutical agents such as the avocado/soybean unsaponifiables (ASU), glucosamine and CS. These products are prescribed in many countries worldwide. Some have undergone clinical trials and were shown to be effective on OA symptoms and sometimes also on joint structure changes. Clinical data supportive of diacerein as a modifying agent were shown in human hip OA [158]. On human OA knee subchondral bone osteoblasts, data showed that diacerein reduces osteocalcin, urokinase, IL-6- and IL-1β-induced MMP-13 production, as well as the synthesis of cathepsin K and MMP-13 on osteoclasts and the formation of these cells, factors that would contribute to curbing bone formation/resorption [159,160]. However, these in vitro findings need to be confirmed in vivo.
The disease-modifying effects of ASU were first shown in animal models. In the context of acting on the remodelling of OA subchondral bone, ASU treatment in the ACL dog model was shown to significantly improve the subchondral bone morphometry and calcified cartilage thickness as well as to reduce the severity of macroscopic and histological cartilage lesions, and the level of inducible nitric oxide synthase and MMP-13 [161]. The efficacy of ASU evaluated in the experimentally induced OA horse model showed that it had no effect on signs, pain or lameness, but there was a reduction in severity of articular cartilage erosion and synovial membrane inflammation and an increase in cartilage glycosaminoglycan synthesis [162]. Similarly, a positive effect of ASU was found on articular cartilage and subchondral bone pathophysiology in a sheep meniscectomy model of OA [163]. In humans, ASU showed significant symptomatic efficacy in the treatment of OA [164]. Furthermore, one study evaluating the effect of ASU in hip OA patients over 2 years demonstrated a significant reduction in joint space loss in the most severe cases [165]. With regard to glucosamine, the hydrochloride formula administered to the cruciate transection rabbit OA model reduced the high subchondral trabecular bone turnover [166]. A recent in vitro study carried out on pro-resorptive human OA subchondral bone osteoblasts demonstrated that the combination of glucosamine and CS could modulate the OPG/RANKL ratio in favour of reduced bone resorption [167]. These drugs have also been evaluated in many studies as agents to relieve pain, improve functional ability and slow disease progression, especially in knee OA patients [168,169].
Conclusion regarding bone-targeting drugs
The use of drugs/agents to treat knee OA and prevent the progression of structural changes needs further exploration. There is a good rationale behind the use of such agents since some are already being given to patients with osteolytic diseases and are proven safe for long-term administration. Some results from studies on humans affected with OA, however, have been disappointing. An explanation could be that the patients were in later stages of the disease upon study entry and that the technologies used to determine the disease-modifying effect were not sensitive enough. As data show that sub-chondral bone resorption is involved early during the OA process, further trials, perhaps in patients with less advanced disease, and with the use of more reliable and sensitive imaging technology, such as MRI and biomarkers, are needed.
Conclusion
Findings with regard to the physiological and pathological mechanisms of OA will make it possible to better target therapeutic approaches that could lead to the development of treatments to reduce or stop the progression of the disease. In that regard, this article summarises some of the knowledge we have today on the involvement of the subchondral bone in OA. It was long believed that the focal characteristic pathological feature of OA was the destruction of articular cartilage. Consequently, it is not surprising that investigations have concentrated for the past few decades on the mechanisms involved in cartilage degradation. In this article, substantial evidence is provided of the integral role in the OA process played by the changes in the metabolism of the subchondral bone.
The question that remains is whether subchondral bone alterations are the cause or a consequence of cartilage degeneration. However, as studies have demonstrated that the subchondral bone is the site of a number of active morphological changes at an early stage of the disease and that cross-talk with cartilage could very well occur, it is becoming increasingly evident that subchondral bone changes in OA are not merely secondary manifestations of the disease but are part of a more active component of OA. Not only is subchondral bone matrix altered in OA but also factors produced by OA subchondral bone cells can influence cartilage metabolism. This could possibly explain why increased subchondral bone activity can predict cartilage loss.
The ultimate goal in the treatment of OA is to improve or preserve the patient’s joint structure by preventing its destruction. This changed view of the pathogenesis of OA from the involvement of the cartilage to the entire joint, and the recognition of early changes in the subchondral bone, provides the potential for new approaches to treatment of this disease. Targeting subchondral bone resorption and/ or mineralisation thus represents an interesting approach to therapy for this disease, and data evaluating the drugs targeting bone remodelling raise the hope that new treatment options for OA may become available. Consequently, the field is opening up to a new era in which drugs and agents that can specifically block important mechanisms responsible for the joint tissue structural changes of OA can be brought into clinical trials.
Practice points.
-
Subchondral bone remodelling in OA
Alterations in subchondral bone activity occur early in the OA process
Early subchondral bone activity is resorptive
Although subchondral bone sclerosis is considered a hallmark of OA, it appears to occur at a later stage of the disease
Subchondral bone sclerosis is due to an increase in material density, and not mineral density
-
Cross-talk between subchondral bone and cartilage
There is strong evidence of a diffusion of molecules/factors from the subchondral bone to the articular cartilage
This diffusion possibly occurs through the clefts and channels in the tidemark seen early in OA as well as through microcracks in the articular cartilage
-
Markers of OA
Individual biomarkers are not very informative on their own of the disease process or of early disease
Clusters of markers are suggested to better correlate with disease progression and also could identify early disease
Imaging technology, such as MRI, is useful for assessing not only disease progression but also early events
Research agenda.
Therapeutic agents targeting bone remodelling
The promise of agents targeting bone remodelling in the treatment of OA has created an urgent need for clinical trials in humans
With the recognition of early changes in subchondral bone during the OA process, patients with less advanced disease could be enrolled in standardised clinical trials instead of those at later stages
References
- 1.Ng KW, Romas E, Donnan L, Findlay DM. Bone biology. Baillieres Clin Endocrinol Metab. 1997;11:1–22. doi: 10.1016/s0950-351x(97)80473-9. [DOI] [PubMed] [Google Scholar]
- 2.Hill PA. Bone remodelling. Br J Orthod. 1998;25:101–7. doi: 10.1093/ortho/25.2.101. [DOI] [PubMed] [Google Scholar]
- 3.Troen BR. Molecular mechanisms underlying osteoclast formation and activation. Exp Gerontol. 2003;38:605–14. doi: 10.1016/s0531-5565(03)00069-x. [DOI] [PubMed] [Google Scholar]
- *4.Martel-Pelletier J, Lajeunesse D, Pelletier JP. Etiopathogenesis of osteoarthritis. In: Koopman WJ, Moreland LW, editors. Arthritis & allied conditions. A textbook of rheumatology. 15. Baltimore: Lippincott, Williams & Wilkins; 2005. pp. 2199–226. [Google Scholar]
- 5.Carlson CS, Loeser RF, Jayo MJ, et al. Osteoarthritis in cynomolgus macaques: a primate model of naturally occurring disease. J Orthop Res. 1994;12:331–9. doi: 10.1002/jor.1100120305. [DOI] [PubMed] [Google Scholar]
- 6.Brandt KD, Myers SL, Burr D, Albrecht M. Osteoarthritic changes in canine articular cartilage, subchondral bone, and synovium fifty-four months after transection of the anterior cruciate ligament. Arthritis Rheum. 1991;34:1560–70. doi: 10.1002/art.1780341214. [DOI] [PubMed] [Google Scholar]
- 7.Hayami T, Pickarski M, Wesolowski GA, et al. The role of subchondral bone remodeling in osteoarthritis: reduction of cartilage degeneration and prevention of osteophyte formation by alendronate in the rat anterior cruciate ligament transection model. Arthritis Rheum. 2004;50:1193–206. doi: 10.1002/art.20124. [DOI] [PubMed] [Google Scholar]
- 8.Pelletier JP, Boileau C, Brunet J, et al. The inhibition of subchondral bone resorption in the early phase of experimental dog osteoarthritis by licofelone is associated with a reduction in the synthesis of MMP-13 and cathepsin K. Bone. 2004;34:527–38. doi: 10.1016/j.bone.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Hayami T, Pickarski M, Zhuo Y, et al. Characterization of articular cartilage and subchondral bone changes in the rat anterior cruciate ligament transection and meniscectomized models of osteoarthritis. Bone. 2006;38:234–43. doi: 10.1016/j.bone.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al. Long term evaluation of disease progression through the quantitative magnetic resonance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthritis Res Ther. 2006;8:R21. doi: 10.1186/ar1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pelletier JP, Raynauld JP, Berthiaume MJ, et al. Risk factors associated with the loss of cartilage volume on weight bearing areas in knee osteoarthritis patients assessed by quantitative MRI: a longitudinal study. Arthritis Res Ther. 2007;9:R74. doi: 10.1186/ar2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raynauld J-P, Martel-Pelletier J, Berthiaume M-J, et al. Correlation between bone lesion changes and cartilage volume loss in patients with osteoarthritis of the knee as assessed by quantitative magnetic resonance imaging over a 24-month period. Ann Rheum Dis. 2008;67:683–8. doi: 10.1136/ard.2007.073023. [DOI] [PubMed] [Google Scholar]
- *13.Boileau C, Martel-Pelletier J, Abram F, et al. Magnetic resonance imaging can accurately assess the long-term progression of knee structural changes in experimental dog OA. Ann Rheum Dis. 2008;67:926–32. doi: 10.1136/ard.2007.077297. [DOI] [PubMed] [Google Scholar]
- 14.Blumenkrantz G, Lindsey CT, Dunn TC, et al. A pilot, two-year longitudinal study of the interrelationship between trabecular bone and articular cartilage in the osteoarthritic knee. Osteoarthritis Cartilage. 2004;12:997–1005. doi: 10.1016/j.joca.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Beuf O, Ghosh S, Newitt DC, et al. Magnetic resonance imaging of normal and osteoarthritic trabecular bone structure in the human knee. Arthritis Rheum. 2002;46:385–93. doi: 10.1002/art.10108. [DOI] [PubMed] [Google Scholar]
- 16.Martig S, Boisclair J, Konar M, et al. MRI characteristics and histology of bone marrow lesions in dogs with experimentally induced osteoarthritis. Vet Radiol Ultrasound. 2007;48:105–12. doi: 10.1111/j.1740-8261.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- *17.Bettica P, Cline G, Hart DJ, et al. Evidence for increased bone resorption in patients with progressive knee osteoarthritis: longitudinal results from the Chingford study. Arthritis Rheum. 2002;46:3178–84. doi: 10.1002/art.10630. [DOI] [PubMed] [Google Scholar]
- 18.Pastoureau PC, Chomel AC, Bonnet J. Evidence of early subchondral bone changes in the meniscectomized guinea pig. A densitometric study using dual-energy X-ray absorptiometry subregional analysis. Osteoarthritis Cartilage. 1999;7:466–73. doi: 10.1053/joca.1999.0241. [DOI] [PubMed] [Google Scholar]
- 19.Buckland-Wright JC, Macfarlane DG, Lynch JA, Clark B. Quantitative microfocal radiographic assessment of progression in osteoarthritis of the hand. Arthritis Rheum. 1990;33:57–65. doi: 10.1002/art.1780330107. [DOI] [PubMed] [Google Scholar]
- 20.Buckland-Wright JC, Lynch JA, Macfarlane DG. Fractal signature analysis measures cancellous bone organisation in macroradiographs of patients with knee osteoarthritis. Ann Rheum Dis. 1996;55:749–55. doi: 10.1136/ard.55.10.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharif M, George E, Dieppe PA. Correlation between synovial fluid markers of cartilage and bone turnover and scintigraphic scan abnormalities in osteoarthritis of the knee. Arthritis Rheum. 1995;38:78–81. doi: 10.1002/art.1780380112. [DOI] [PubMed] [Google Scholar]
- 22.Dieppe P, Cushnaghan J, Young P, Kirwan J. Prediction of the progression of joint space narrowing in osteoarthritis of the knee by bone scintigraphy. Ann Rheum Dis. 1993;52:557–63. doi: 10.1136/ard.52.8.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCarthy C, Cushnaghan J, Dieppe P. The predictive role of scintigraphy in radiographic osteoarthritis of the hand. Osteoarthritis Cartilage. 1994;2:25–8. doi: 10.1016/s1063-4584(05)80003-2. [DOI] [PubMed] [Google Scholar]
- 24.Gevers G, Dequeker J. Collagen and non-collagenous protein content (osteocalcin, sialoprotein, proteoglycan) in the iliac crest bone and serum osteocalcin in women with and without hand osteoarthritis. Coll Relat Res. 1987;7:435–42. doi: 10.1016/s0174-173x(87)80041-9. [DOI] [PubMed] [Google Scholar]
- 25.Dequeker J, Mohan R, Finkelman RD, et al. Generalized osteoarthritis associated with increased insulin-like growth factor types I and II and transforming growth factor beta in cortical bone from the iliac crest. Possible mechanism of increased bone density and protection against osteoporosis. Arthritis Rheum. 1993;36:1702–8. doi: 10.1002/art.1780361209. [DOI] [PubMed] [Google Scholar]
- 26.Ferguson VL, Bushby AJ, Boyde A. Nanomechanical properties and mineral concentration in articular calcified cartilage and subchondral bone. J Anat. 2003;203:191–202. doi: 10.1046/j.1469-7580.2003.00193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crane GJ, Fazzalari NL, Parkinson IH, Vernon-Roberts B. Age-related changes in femoral trabecular bone in arthrosis. Acta Orthop Scand. 1990;61:421–6. doi: 10.3109/17453679008993554. [DOI] [PubMed] [Google Scholar]
- 28.Fazzalari NL, Parkinson IH. Femoral trabecular bone of osteoarthritic and normal subjects in an age and sex matched group. Osteoarthritis Cartilage. 1998;6:377–82. doi: 10.1053/joca.1998.0141. [DOI] [PubMed] [Google Scholar]
- 29.Grynpas MD, Alpert B, Katz I, et al. Subchondral bone in osteoarthritis. Calcif Tissue Int. 1991;49:20–6. doi: 10.1007/BF02555898. [DOI] [PubMed] [Google Scholar]
- 30.Li B, Aspden RM. Composition and mechanical properties of cancellous bone from the femoral head of patients with osteoporosis or osteoarthritis. J Bone Miner Res. 1997;12:641–51. doi: 10.1359/jbmr.1997.12.4.641. [DOI] [PubMed] [Google Scholar]
- 31.Mansell JP, Tarlton JF, Bailey AJ. Biochemical evidence for altered subchondral bone collagen metabolism in osteoarthritis of the hip. Br J Rheumatol. 1997;36:16–9. doi: 10.1093/rheumatology/36.1.16. [DOI] [PubMed] [Google Scholar]
- 32.Mansell JP, Bailey AJ. Abnormal cancellous bone collagen metabolism in osteoarthritis. J Clin Invest. 1998;101:1596–603. doi: 10.1172/JCI867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bailey AJ, Sims TJ, Knott L. Phenotypic expression of osteoblast collagen in osteoarthritic bone: production of type I homotrimer. Int J Biochem Cell Biol. 2002;34:176–82. doi: 10.1016/s1357-2725(01)00107-8. [DOI] [PubMed] [Google Scholar]
- 34.Gevers G, Dequeker J, Geusens P, et al. Physical and histomorphological characteristics of iliac crest bone differ according to the grade of osteoarthritis at the hand. Bone. 1989;10:173–7. doi: 10.1016/8756-3282(89)90050-1. [DOI] [PubMed] [Google Scholar]
- 35.Zysset PK, Sonny M, Hayes WC. Morphology-mechanical property relations in trabecular bone of the osteoarthritic proximal tibia. J Arthroplasty. 1994;9:203–16. doi: 10.1016/0883-5403(94)90070-1. [DOI] [PubMed] [Google Scholar]
- *36.Couchourel D, Aubry I, Delalandre A, et al. Altered mineralization of human osteoarthritic osteoblasts is due to abnormal collagen type 1 production. Arthritis Rheum. 2009;60:1438–50. doi: 10.1002/art.24489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *37.Hilal G, Martel-Pelletier J, Pelletier JP, et al. Osteoblast-like cells from human subchondral osteoarthritic bone demonstrate an altered phenotype in vitro: possible role in subchondral bone sclerosis. Arthritis Rheum. 1998;41:891–9. doi: 10.1002/1529-0131(199805)41:5<891::AID-ART17>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 38.Hilal G, Martel-Pelletier J, Pelletier JP, et al. Abnormal regulation of urokinase plasminogen activator by insulin-like growth factor 1 in human osteoarthritic subchondral osteoblasts. Arthritis Rheum. 1999;42:2112–22. doi: 10.1002/1529-0131(199910)42:10<2112::AID-ANR11>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 39.Aspden RM, Scheven BA, Hutchison JD. Osteoarthritis as a systemic disorder including stromal cell differentiation and lipid metabolism. Lancet. 2001;357:1118–20. doi: 10.1016/S0140-6736(00)04264-1. [DOI] [PubMed] [Google Scholar]
- 40.Plumb MS, Aspden RM. High levels of fat and (n − 6) fatty acids in cancellous bone in osteoarthritis. Lipids Health Dis. 2004;3:12. doi: 10.1186/1476-511X-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murphy JM, Dixon K, Beck S, et al. Reduced chondrogenic and adipogenic activity of mesenchymal stem cells from patients with advanced osteoarthritis. Arthritis Rheum. 2002;46:704–13. doi: 10.1002/art.10118. [DOI] [PubMed] [Google Scholar]
- 42.Thomas T, Gori F, Khosla S, et al. Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology. 1999;140:1630–8. doi: 10.1210/endo.140.4.6637. [DOI] [PubMed] [Google Scholar]
- 43.Gordeladze JO, Drevon CA, Syversen U, Reseland JE. Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: impact on differentiation markers, apoptosis, and osteoclastic signaling. J Cell Biochem. 2002;85:825–36. doi: 10.1002/jcb.10156. [DOI] [PubMed] [Google Scholar]
- 44.Bennett CN, Ross SE, Longo KA, et al. Regulation of Wnt signaling during a dipogenesis. J Biol Chem. 2002;277:30998–1004. doi: 10.1074/jbc.M204527200. [DOI] [PubMed] [Google Scholar]
- 45.Fox KE, Colton LA, Erickson PF, et al. Regulation of cyclin D1 and Wnt10b gene expression by cAMP-responsive element-binding protein during early adipogenesis involves differential promoter methylation. J Biol Chem. 2008;283:35096–105. doi: 10.1074/jbc.M806423200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Poole KE, van Bezooijen RL, Loveridge N, et al. Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. Fed Am Soc Exp Bio J. 2005;19:1842–4. doi: 10.1096/fj.05-4221fje. [DOI] [PubMed] [Google Scholar]
- 47.van Bezooijen RL, ten Dijke P, Papapoulos SE, Lowik CW. SOST/sclerostin, an osteocyte-derived negative regulator of bone formation. Cytokine Growth Factor Rev. 2005;16:319–27. doi: 10.1016/j.cytogfr.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 48.Couchourel D, Delalandre A, Lajeunesse D. Increased expression of Wnt inhibitory factors in subchondral osteoblasts from osteoarthritic patients could play a role in their abnormal phenotype and mineralization. Ann Rheum Dis. 2008;67(Suppl II):98. abstract. [Google Scholar]
- 49.Li X, Liu P, Liu W, et al. Dkk2 has a role in terminal osteoblast differentiation and mineralized matrix formation. Nat Genet. 2005;37:945–52. doi: 10.1038/ng1614. [DOI] [PubMed] [Google Scholar]
- 50.Robinson JA, Chatterjee-Kishore M, Yaworsky PJ, et al. Wnt/beta-catenin signaling is a normal physiological response to mechanical loading in bone. J Biol Chem. 2006;281:31720–8. doi: 10.1074/jbc.M602308200. [DOI] [PubMed] [Google Scholar]
- 51.Liu J, Zou L, Wang J, et al. Hydrostatic pressure promotes Wnt10b and Wnt4 expression dependent and independent on ERK signaling in early-osteoinduced MSCs. Biochem Biophys Res Commun. 2009;379:505–9. doi: 10.1016/j.bbrc.2008.12.087. [DOI] [PubMed] [Google Scholar]
- 52.Boyden LM, Mao J, Belsky J, et al. High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med. 2002;346:1513–21. doi: 10.1056/NEJMoa013444. [DOI] [PubMed] [Google Scholar]
- 53.Little RD, Carulli JP, Del Mastro RG, et al. A mutation in the LDL receptor-related protein 5 gene results in the autosomal dominant high-bone-mass trait. Am J Hum Genet. 2002;70:11–9. doi: 10.1086/338450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Babij P, Zhao W, Small C, et al. High bone mass in mice expressing a mutant LRP5 gene. J Bone Miner Res. 2003;18:960–74. doi: 10.1359/jbmr.2003.18.6.960. [DOI] [PubMed] [Google Scholar]
- 55.Hartmann C. A Wnt canon orchestrating osteoblastogenesis. Trends Cell Biol. 2006;16:151–8. doi: 10.1016/j.tcb.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 56.Gong Y, Slee RB, Fukai N, et al. LDL receptor-related protein 5 (LRP5) affects bone accrual and eye development. Cell. 2001;107:513–23. doi: 10.1016/s0092-8674(01)00571-2. [DOI] [PubMed] [Google Scholar]
- 57.Kato M, Patel MS, Levasseur R, et al. Cbfa1-independent decrease in osteoblast proliferation, osteopenia, and persistent embryonic eye vascularization in mice deficient in Lrp5, a Wnt coreceptor. J Cell Biol. 2002;157:303–14. doi: 10.1083/jcb.200201089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *58.Smith AJ, Gidley J, Sandy JR, et al. Haplotypes of the low-density lipoprotein receptor-related protein 5 (LRP5) gene: are they a risk factor in osteoarthritis? Osteoarthritis Cartilage. 2005;13:608–13. doi: 10.1016/j.joca.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 59.Loughlin J, Dowling B, Chapman K, et al. Functional variants within the secreted frizzled-related protein 3 gene are associated with hip osteoarthritis in females. Proc Natl Acad Sci USA. 2004;101:9757–62. doi: 10.1073/pnas.0403456101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chung YS, Baylink DJ, Srivastava AK, et al. Effects of secreted frizzled-related protein 3 on osteoblasts in vitro. J Bone Miner Res. 2004;19:1395–402. doi: 10.1359/JBMR.040412. [DOI] [PubMed] [Google Scholar]
- 61.Li J, Sarosi I, Cattley RC, et al. Dkk1-mediated inhibition of Wnt signaling in bone results in osteopenia. Bone. 2006;39:754–66. doi: 10.1016/j.bone.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 62.Morvan F, Boulukos K, Clement-Lacroix P, et al. Deletion of a single allele of the Dkk1 gene leads to an increase in bone formation and bone mass. J Bone Miner Res. 2006;21:934–45. doi: 10.1359/jbmr.060311. [DOI] [PubMed] [Google Scholar]
- 63.Diarra D, Stolina M, Polzer K, et al. Dickkopf-1 is a master regulator of joint remodeling. Nat Med. 2007;13:156–63. doi: 10.1038/nm1538. [DOI] [PubMed] [Google Scholar]
- 64.Gardner JC, van Bezooijen RL, Mervis B, et al. Bone mineral density in sclerosteosis; affected individuals and gene carriers. J Clin Endocrinol Metab. 2005;90:6392–5. doi: 10.1210/jc.2005-1235. [DOI] [PubMed] [Google Scholar]
- 65.Winkler DG, Sutherland MS, Ojala E, et al. Sclerostin inhibition of Wnt-3a-induced C3H10T1/2 cell differentiation is indirect and mediated by bone morphogenetic proteins. J Biol Chem. 2005;280:2498–502. doi: 10.1074/jbc.M400524200. [DOI] [PubMed] [Google Scholar]
- 66.Fischer L, Boland G, Tuan RS. Wnt-3A enhances bone morphogenetic protein-2-mediated chondrogenesis of murine C3H10T1/2 mesenchymal cells. J Biol Chem. 2002;277:30870–8. doi: 10.1074/jbc.M109330200. [DOI] [PubMed] [Google Scholar]
- 67.Bain G, Muller T, Wang X, Papkoff J. Activated beta-catenin induces osteoblast differentiation of C3H10T1/2 cells and participates in BMP2 mediated signal transduction. Biochem Biophys Res Commun. 2003;301:84–91. doi: 10.1016/s0006-291x(02)02951-0. [DOI] [PubMed] [Google Scholar]
- 68.Zamurovic N, Cappellen D, Rohner D, Susa M. Coordinated activation of notch, Wnt, and transforming growth factor-beta signaling pathways in bone morphogenic protein 2-induced osteogenesis. Notch target gene Hey1 inhibits mineralization and Runx2 transcriptional activity. J Biol Chem. 2004;279:37704–15. doi: 10.1074/jbc.M403813200. [DOI] [PubMed] [Google Scholar]
- 69.Massicotte F, Fernandes JC, Martel-Pelletier J, et al. Modulation of insulin-like growth factor 1 levels in human osteo-arthritic subchondral bone osteoblasts. Bone. 2006;38:333–41. doi: 10.1016/j.bone.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 70.Rydziel S, Delany AM, Canalis E. Insulin-like growth factor I inhibits the transcription of collagenase 3 in osteoblast cultures. J Cell Biochem. 1997;67:176–83. [PubMed] [Google Scholar]
- 71.van Beuningen HM, van der Kraan PM, Arntz OJ, van den Berg WB. Transforming growth factor-beta 1 stimulates articular chondrocyte proteoglycan synthesis and induces osteophyte formation in the murine knee joint. Lab Invest. 1994;71:279–90. [PubMed] [Google Scholar]
- 72.Scharstuhl A, Glansbeek HL, van Beuningen HM, et al. Inhibition of endogenous TGF-beta during experimental osteoarthritis prevents osteophyte formation and impairs cartilage repair. J Immunol. 2002;169:507–14. doi: 10.4049/jimmunol.169.1.507. [DOI] [PubMed] [Google Scholar]
- 73.Dumond H, Presle N, Terlain B, et al. Evidence for a key role of leptin in osteoarthritis. Arthritis Rheum. 2003;48:3118–29. doi: 10.1002/art.11303. [DOI] [PubMed] [Google Scholar]
- 74.Darnay BG, Haridas V, Ni J, et al. Characterization of the intracellular domain of receptor activator of NF-kappaB (RANK). Interaction with tumor necrosis factor receptor-associated factors and activation of NF-kappaB and c-Jun N-terminal kinase. J Biol Chem. 1998;273:20551–5. doi: 10.1074/jbc.273.32.20551. [DOI] [PubMed] [Google Scholar]
- 75.Gravallese EM, Goldring SR. Cellular mechanisms and the role of cytokines in bone erosions in rheumatoid arthritis. Arthritis Rheum. 2000;43:2143–51. doi: 10.1002/1529-0131(200010)43:10<2143::AID-ANR1>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 76.Khosla S. Minireview: the OPG/RANKL/RANK system. Endocrinology. 2001;142:5050–5. doi: 10.1210/endo.142.12.8536. [DOI] [PubMed] [Google Scholar]
- 77.Armstrong AP, Tometsko ME, Glaccum M, et al. A RANK/TRAF6-dependent signal transduction pathway is essential for osteoclast cytoskeletal organization and resorptive function. J Biol Chem. 2002;277:44347–56. doi: 10.1074/jbc.M202009200. [DOI] [PubMed] [Google Scholar]
- 78.Kwan Tat S, Padrines M, Theoleyre S, et al. IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 2004;15:49–60. doi: 10.1016/j.cytogfr.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 79.Kwan Tat S, Pelletier JP, Lajeunesse D, et al. The differential expression of osteoprotegerin (OPG) and receptor activator of nuclear factor kappaB ligand (RANKL) in human osteoarthritic subchondral bone osteoblasts is an indicator of the metabolic state of these disease cells. Clin Exp Rheumatol. 2008;26:295–304. [PMC free article] [PubMed] [Google Scholar]
- 80.Zhao C, Irie N, Takada Y, et al. Bidirectional ephrinB2-EphB4 signaling controls bone homeostasis. Cell Metab. 2006;4:111–21. doi: 10.1016/j.cmet.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 81.Kwan Tat S, Pelletier JP, Amiable N, et al. Activation of the receptor EphB4 by its specific ligand ephrin B2 in human osteoarthritic subchondral bone osteoblasts: a new therapeutic approach. Arthritis Rheum. 2008;58:3820–30. doi: 10.1002/art.24029. [DOI] [PubMed] [Google Scholar]
- 82.Hilal G, Massicotte F, Martel-Pelletier J, et al. Endogenous prostaglandin E2 and insulin-like growth factor 1 can modulate the levels of parathyroid hormone receptor in human osteoarthritic osteoblasts. J Bone Miner Res. 2001;16:713–21. doi: 10.1359/jbmr.2001.16.4.713. [DOI] [PubMed] [Google Scholar]
- 83.Dietrich JW, Canalis EM, Maina DM, Raisz LG. Hormonal control of bone collagen synthesis in vitro: effects of parathyroid hormone and calcitonin. Endocrinology. 1976;98:943–9. doi: 10.1210/endo-98-4-943. [DOI] [PubMed] [Google Scholar]
- 84.Beresford JN, Gallagher JA, Poser JW, Russell RG. Production of osteocalcin by human bone cells in vitro Effects of 1,25(OH)2D3, 24,25(OH)2D3, parathyroid hormone, and glucocorticoids. Metab Bone Dis Relat Res. 1984;5:229–34. doi: 10.1016/0221-8747(84)90064-x. [DOI] [PubMed] [Google Scholar]
- 85.Coats AM, Zioupos P, Aspden RM. Material properties of subchondral bone from patients with osteoporosis or osteoarthritis by microindentation testing and electron probe microanalysis. Calcif Tissue Int. 2003;73:66–71. doi: 10.1007/s00223-002-2080-8. [DOI] [PubMed] [Google Scholar]
- *86.Burr DB. Increased biological activity of subchondral mineralized tissues underlies the progressive deterioration of articular cartilage in osteoarthritis. J Rheumatol. 2005;32:1156–8. discussion 1158–1159. [PubMed] [Google Scholar]
- 87.Mital MA, Millington PF. Osseous pathway of nutrition to articular cartilage of the human femoral head. Lancet. 1970;1:842. doi: 10.1016/s0140-6736(70)92443-8. [DOI] [PubMed] [Google Scholar]
- 88.Mori S, Harruff R, Burr DB. Microcracks in articular calcified cartilage of human femoral heads. Arch Pathol Lab Med. 1993;117:196–8. [PubMed] [Google Scholar]
- 89.Sokoloff L. Microcracks in the calcified layer of articular cartilage. Arch Pathol Lab Med. 1993;117:191–5. [PubMed] [Google Scholar]
- 90.Villanueva AR, Longo JA, 3rd, Weiner G. Staining and histomorphometry of microcracks in the human femoral head. Biotech Histochem. 1994;69:81–8. doi: 10.3109/10520299409106266. [DOI] [PubMed] [Google Scholar]
- *91.Burr DB, Radin EL. Microfractures and microcracks in subchondral bone: are they relevant to osteoarthrosis? Rheum Dis Clin North Am. 2003;29:675–85. doi: 10.1016/s0889-857x(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 92.Laurent UB, Fraser JR, Engstrom-Laurent A, et al. Catabolism of hyaluronan in the knee joint of the rabbit. Matrix. 1992;12:130–6. doi: 10.1016/s0934-8832(11)80054-5. [DOI] [PubMed] [Google Scholar]
- *93.Malinin T, Ouellette EA. Articular cartilage nutrition is mediated by subchondral bone: a long-term autograft study in baboons. Osteoarthritis Cartilage. 2000;8:483–91. doi: 10.1053/joca.1999.0324. [DOI] [PubMed] [Google Scholar]
- 94.Huebner JL, Hanes MA, Beekman B, et al. A comparative analysis of bone and cartilage metabolism in two strains of guinea-pig with varying degrees of naturally occurring osteoarthritis. Osteoarthritis Cartilage. 2002;10:758–67. doi: 10.1053/joca.2002.0821. [DOI] [PubMed] [Google Scholar]
- 95.Radin EL, Rose RM. Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop. 1986;213:34–40. [PubMed] [Google Scholar]
- *96.Carlson CS, Loeser RF, Purser CB, et al. Osteoarthritis in cynomolgus macaques. III: effects of age, gender, and subchondral bone thickness on the severity of disease. J Bone Miner Res. 1996;11:1209–17. doi: 10.1002/jbmr.5650110904. [DOI] [PubMed] [Google Scholar]
- 97.Brandt KD. Insights into the natural history of osteoarthritis provided by the cruciate-deficient dog. An animal model of osteoarthritis. Ann NY Acad Sci. 1994;732:199–205. doi: 10.1111/j.1749-6632.1994.tb24735.x. Review. [DOI] [PubMed] [Google Scholar]
- 98.Burr DB. The importance of subchondral bone in osteoarthrosis. Curr Opin Rheumatol. 1998;10:256–562. doi: 10.1097/00002281-199805000-00017. [DOI] [PubMed] [Google Scholar]
- 99.Burr DB, Schaffler MB. The involvement of subchondral mineralized tissues in osteoarthrosis: quantitative microscopic evidence. Microsc Res Tech. 1997;37:343–57. doi: 10.1002/(SICI)1097-0029(19970515)37:4<343::AID-JEMT9>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 100.Imhof H, Breitenseher M, Kainberger F, et al. Importance of subchondral bone to articular cartilage in health and disease. Top Magn Reson Imaging. 1999;10:180–92. doi: 10.1097/00002142-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 101.Kwan Tat S, Amiable N, Pelletier JP, et al. Modulation of OPG, RANK, and RANKL by human chondrocytes and their implication during osteoarthritis. Rheumatology. doi: 10.1093/rheumatology/kep300. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kwan Tat S, Pelletier JP, Amiable N, et al. Treatment with ephrin B2 positively impacts the abnormal metabolism of human osteoarthritic chondrocytes. Arthritis Res Ther. 2009;11:R119. doi: 10.1186/ar2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pfander D, Cramer T, Weseloh G, et al. Hepatocyte growth factor in human osteoarthritic cartilage. Osteoarthritis Cartilage. 1999;7:548–59. doi: 10.1053/joca.1999.0259. [DOI] [PubMed] [Google Scholar]
- 104.Blanquaert F, Pereira RC, Canalis E. Cortisol inhibits hepatocyte growth factor/scatter factor expression and induces c-met transcripts in osteoblasts. Am J Physiol Endocrinol Metab. 2000;278:E509–15. doi: 10.1152/ajpendo.2000.278.3.E509. [DOI] [PubMed] [Google Scholar]
- 105.Guévremont M, Martel-Pelletier J, Massicotte F, et al. Human adult chondrocytes express hepatocyte growth factor (HGF) isoforms but not HGF: potential implication of osteoblasts on the presence of HGF in cartilage. J Bone Miner Res. 2003;18:1073–81. doi: 10.1359/jbmr.2003.18.6.1073. [DOI] [PubMed] [Google Scholar]
- 106.Reboul P, Pelletier JP, Tardif G, et al. Hepatocyte growth factor induction of collagenase 3 production in human osteoarthritic cartilage: involvement of the stress-activated protein kinase/c-Jun N-terminal kinase pathway and a sensitive p38 mitogen-activated protein kinase inhibitor cascade. Arthritis Rheum. 2001;44:73–84. doi: 10.1002/1529-0131(200101)44:1<73::AID-ANR11>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 107.Moldovan F, Pelletier JP, Hambor J, et al. Collagenase-3 (matrix metalloprotease 13) is preferentially localized in the deep layer of human arthritic cartilage in situ: in vitro mimicking effect by transforming growth factor beta. Arthritis Rheum. 1997;40:1653–61. doi: 10.1002/art.1780400915. [DOI] [PubMed] [Google Scholar]
- 108.Berthiaume MJ, Raynauld JP, Martel-Pelletier J, et al. Meniscal tear and extrusion are strongly associated with the progression of knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–63. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bruyere O, Collette J, Kothari M, et al. Osteoarthritis, magnetic resonance imaging, and biochemical markers: a one year prospective study. Ann Rheum Dis. 2006;65:1050–4. doi: 10.1136/ard.2005.045914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jung YO, Do JH, Kang HJ, et al. Correlation of sonographic severity with biochemical markers of synovium and cartilage in knee osteoarthritis patients. Clin Exp Rheumatol. 2006;24:253–9. [PubMed] [Google Scholar]
- 111.Sharif M, Kirwan J, Charni N, et al. A 5-yr longitudinal study of type IIA collagen synthesis and total type II collagen degradation in patients with knee osteoarthritis–association with disease progression. Rheumatology (Oxford) 2007;46:938–43. doi: 10.1093/rheumatology/kel409. [DOI] [PubMed] [Google Scholar]
- 112.Conrozier T, Poole AR, Ferrand F, et al. Serum concentrations of type II collagen biomarkers (C2C, C1, 2C and CPII) suggest different pathophysiologies in patients with hip osteoarthritis. Clin Exp Rheumatol. 2008;26:430–5. [PubMed] [Google Scholar]
- 113.Chaganti RK, Kelman A, Lui L, et al. Change in serum measurements of cartilage oligomeric matrix protein and association with the development and worsening of radiographic hip osteoarthritis. Osteoarthritis Cartilage. 2008;16:566–71. doi: 10.1016/j.joca.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hunter DJ, Lavalley M, Li J, et al. Biochemical markers of bone turnover and their association with bone marrow lesions. Arthritis Res Ther. 2008;10:R102. doi: 10.1186/ar2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kong SY, Stabler TV, Criscione LG, et al. Diurnal variation of serum and urine biomarkers in patients with radiographic knee osteoarthritis. Arthritis Rheum. 2006;54:2496–504. doi: 10.1002/art.21977. [DOI] [PubMed] [Google Scholar]
- 116.Pothacharoen P, Teekachunhatean S, Louthrenoo W, et al. Raised chondroitin sulfate epitopes and hyaluronan in serum from rheumatoid arthritis and osteoarthritis patients. Osteoarthritis Cartilage. 2006;14:299–301. doi: 10.1016/j.joca.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 117.Jordan KM, Syddall HE, Garnero P, et al. Urinary CTX-II and glucosyl-galactosyl-pyridinoline are associated with the presence and severity of radiographic knee osteoarthritis in men. Ann Rheum Dis. 2006;65:871–7. doi: 10.1136/ard.2005.042895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Davis CR, Karl J, Granell R, et al. Can biochemical markers serve as surrogates for imaging in knee osteoarthritis? Arthritis Rheum. 2007;56:4038–47. doi: 10.1002/art.23129. [DOI] [PubMed] [Google Scholar]
- 119.Meulenbelt I, Kloppenburg M, Kroon HM, et al. Clusters of biochemical markers are associated with radiographic subtypes of osteoarthritis (OA) in subject with familial OA at multiple sites. The GARP study. Osteoarthritis Cartilage. 2007;15:379–85. doi: 10.1016/j.joca.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 120.Pilichou A, Papassotiriou I, Michalakakou K, et al. High levels of synovial fluid osteoprotegerin (OPG) and increased serum ratio of receptor activator of nuclear factor-kappa B ligand (RANKL) to OPG correlate with disease severity in patients with primary knee osteoarthritis. Clin Biochem. 2008;41:746–9. doi: 10.1016/j.clinbiochem.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 121.Ling SM, Patel DD, Garnero P, et al. Serum protein signatures detect early radiographic osteoarthritis. Osteoarthritis Cartilage. 2009;17:43–8. doi: 10.1016/j.joca.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cibere J, Zhang H, Garnero P, et al. Association of biomarkers with pre-radiographically defined and radiographically defined knee osteoarthritis in a population-based study. Arthritis Rheum. 2009;60:1372–80. doi: 10.1002/art.24473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kadri A, Ea HK, Bazille C, et al. Osteoprotegerin inhibits cartilage degradation through an effect on trabecular bone in murine experimental osteoarthritis. Arthritis Rheum. 2008;58:2379–86. doi: 10.1002/art.23638. [DOI] [PubMed] [Google Scholar]
- 124.Shimizu S, Asou Y, Itoh S, et al. Prevention of cartilage destruction with intraarticular osteoclastogenesis inhibitory factor/ osteoprotegerin in a murine model of osteoarthritis. Arthritis Rheum. 2007;56:3358–65. doi: 10.1002/art.22941. [DOI] [PubMed] [Google Scholar]
- 125.Nakashima T, Wada T, Penninger JM. RANKL and RANK as novel therapeutic targets for arthritis. Curr Opin Rheumatol. 2003;15:280–7. doi: 10.1097/00002281-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 126.Bekker PJ, Holloway DL, Rasmussen AS, et al. A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res. 2004;19:1059–66. doi: 10.1359/JBMR.040305. [DOI] [PubMed] [Google Scholar]
- 127.Ding M, Danielsen CC, Hvid I. The effects of bone remodeling inhibition by alendronate on three-dimensional microarchitecture of subchondral bone tissues in guinea pig primary osteoarthrosis. Calcif Tissue Int. 2008;82:77–86. doi: 10.1007/s00223-007-9093-2. [DOI] [PubMed] [Google Scholar]
- 128.Meyer J, Farmer R, Prenger MC. Risedronate but not alendronate slows disease progression in the guinea pig model of primary osteoarthritis. J Bone Miner Res. 2001;5305:SA472. abstract. [Google Scholar]
- 129.Meyer JM, Dansereau SM, Farmer RW, et al. Bisphosphonates structurally similar to risedronate (actonel) slow disease progression in the guinea pig model of primary osteoarthritis. Arthritis Rheum. 2001;44(5307):1527. abstract. [Google Scholar]
- 130.Myers SL, Brandt KD, Burr DB, et al. Effects of a bisphosphonate on bone histomorphometry and dynamics in the canine cruciate deficiency model of osteoarthritis. J Rheumatol. 1999;26:2645–53. [PubMed] [Google Scholar]
- 131.Spector TD, Conaghan PG, Buckland-Wright JC, et al. Effect of risedronate on joint structure and symptoms of knee osteoarthritis: results of the BRISK randomized, controlled trial. Arthritis Res Ther. 2005;7:R625–33. doi: 10.1186/ar1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bingham CO, 3rd, Buckland-Wright JC, Garnero P, et al. Risedronate decreases biochemical markers of cartilage degradation but does not decrease symptoms or slow radiographic progression in patients with medial compartment osteoarthritis of the knee: results of the two-year multinational knee osteoarthritis structural arthritis study. Arthritis Rheum. 2006;54:3494–507. doi: 10.1002/art.22160. [DOI] [PubMed] [Google Scholar]
- 133.Hott M, Deloffre P, Tsouderos Y, Marie PJ. S12911-2 reduces bone loss induced by short-term immobilization in rats. Bone. 2003;33:115–23. doi: 10.1016/s8756-3282(03)00115-7. [DOI] [PubMed] [Google Scholar]
- 134.Marie PJ, Hott M, Modrowski D, et al. An uncoupling agent containing strontium prevents bone loss by depressing bone resorption and maintaining bone formation in estrogen-deficient rats. J Bone Miner Res. 1993;8:607–15. doi: 10.1002/jbmr.5650080512. [DOI] [PubMed] [Google Scholar]
- 135.Ammann P, Shen V, Robin B, et al. Strontium ranelate improves bone resistance by increasing bone mass and improving architecture in intact female rats. J Bone Miner Res. 2004;19:2012–20. doi: 10.1359/JBMR.040906. [DOI] [PubMed] [Google Scholar]
- 136.Buehler J, Chappuis P, Saffar JL, et al. Strontium ranelate inhibits bone resorption while maintaining bone formation in alveolar bone in monkeys (Macaca fascicularis) Bone. 2001;29:176–9. doi: 10.1016/s8756-3282(01)00484-7. [DOI] [PubMed] [Google Scholar]
- 137.Delannoy P, Bazot D, Marie PJ. Long-term treatment with strontium ranelate increases vertebral bone mass without deleterious effect in mice. Metabolism. 2002;51:906–11. doi: 10.1053/meta.2002.33360. [DOI] [PubMed] [Google Scholar]
- 138.Barbara A, Delannoy P, Denis BG, Marie PJ. Normal matrix mineralization induced by strontium ranelate in MC3T3-E1 osteogenic cells. Metabolism. 2004;53:532–7. doi: 10.1016/j.metabol.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 139.Baron R, Tsouderos Y. In vitro effects of S12911-2 on osteoclast function and bone marrow macrophage differentiation. Eur J Pharmacol. 2002;450:11–7. doi: 10.1016/s0014-2999(02)02040-x. [DOI] [PubMed] [Google Scholar]
- 140.Canalis E, Hott M, Deloffre P, et al. The divalent strontium salt S12911 enhances bone cell replication and bone formation in vitro. Bone. 1996;18:517–23. doi: 10.1016/8756-3282(96)00080-4. [DOI] [PubMed] [Google Scholar]
- 141.Fromigue O, Hay E, Barbara A, et al. Calcium sensing receptor-dependent and -independent activation of osteoblast replication and survival by strontium ranelate. J Cell Mol Med. 2009 doi: 10.1111/j.1582-4934.2008.00673.x. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Takahashi N, Sasaki T, Tsouderos Y, Suda TS. 12911-2 inhibits osteoclastic bone resorption in vitro. J Bone Miner Res. 2003;18:1082–7. doi: 10.1359/jbmr.2003.18.6.1082. [DOI] [PubMed] [Google Scholar]
- 143.Papaioannou NA, Triantafillopoulos IK, Khaldi L, et al. Effect of calcitonin in early and late stages of experimentally induced osteoarthritis. A histomorphometric study. Osteoarthritis Cartilage. 2007;15:386–95. doi: 10.1016/j.joca.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 144.Manicourt DH, Altman RD, Williams JM, et al. Treatment with calcitonin suppresses the responses of bone, cartilage, and synovium in the early stages of canine experimental osteoarthritis and significantly reduces the severity of the cartilage lesions. Arthritis Rheum. 1999;42:1159–67. doi: 10.1002/1529-0131(199906)42:6<1159::AID-ANR12>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 145.El Hajjaji H, Williams JM, Devogelaer JP, et al. Treatment with calcitonin prevents the net loss of collagen, hyaluronan and proteoglycan aggregates from cartilage in the early stages of canine experimental osteoarthritis. Osteoarthritis Cartilage. 2004;12:904–11. doi: 10.1016/j.joca.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 146.Manicourt DH, Azria M, Mindeholm L, et al. Oral salmon calcitonin reduces Lequesne’s algofunctional index scores and decreasesurinaryand serum levels ofbiomarkers ofjointmetabolism inkneeosteoarthritis. Arthritis Rheum. 2006;54:3205–11. doi: 10.1002/art.22075. [DOI] [PubMed] [Google Scholar]
- 147.Konttinen YT, Mandelin J, Li TF, et al. Acidic cysteine endoproteinase cathepsin K in the degeneration of the superficial articular hyaline cartilage in osteoarthritis. Arthritis Rheum. 2002;46:953–60. doi: 10.1002/art.10185. [DOI] [PubMed] [Google Scholar]
- 148.Kafienah W, Bromme D, Buttle DJ, et al. Human cathepsin K cleaves native type I and II collagens at the N- terminal end of the triple helix. Biochem J. 1998;331(Pt 3):727–32. doi: 10.1042/bj3310727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sniekers YH, Weinans H, Bierma-Zeinstra SM, et al. Animal models for osteoarthritis: the effect of ovariectomy and estrogen treatment - a systematic approach. Osteoarthritis Cartilage. 2008;16:533–41. doi: 10.1016/j.joca.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 150.Karsdal MA, Byrjalsen I, Leeming DJ, Christiansen C. Tibolone inhibits bone resorption without secondary positive effects on cartilage degradation. BMC Musculoskelet Disord. 2008;9:153. doi: 10.1186/1471-2474-9-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Christgau S, Cloos PA. Sex hormones in the regulation of bone and cartilage metabolism: an old paradigm and a new challenge. Minerva Ginecol. 2005;57:611–7. [PubMed] [Google Scholar]
- 152.Tetlow LC, Woolley DE. Expression of vitamin D receptors and matrix metalloproteinases in osteoarthritic cartilage and human articular chondrocytes in vitro. Osteoarthritis Cartilage. 2001;9:423–31. doi: 10.1053/joca.2000.0408. [DOI] [PubMed] [Google Scholar]
- 153.McAlindon TE, Felson DT, Zhang Y, et al. Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125:353–9. doi: 10.7326/0003-4819-125-5-199609010-00001. [DOI] [PubMed] [Google Scholar]
- 154.Lane NE, Gore LR, Cummings SR, et al. Serum vitamin D levels and incident changes of radiographic hip osteoarthritis: a longitudinal study. Study of Osteoporotic Fractures Research Group. Arthritis Rheum. 1999;42:854–60. doi: 10.1002/1529-0131(199905)42:5<854::AID-ANR3>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 155.Felson DT, Niu J, Clancy M, et al. Low levels of vitamin D and worsening of knee osteoarthritis: results of two longitudinal studies. Arthritis Rheum. 2007;56:129–36. doi: 10.1002/art.22292. [DOI] [PubMed] [Google Scholar]
- 156.Hunter DJ, Hart D, Snieder H, et al. Evidence of altered bone turnover, vitamin D and calcium regulation with knee osteoarthritis in female twins. Rheumatology (Oxford) 2003;42:1311–6. doi: 10.1093/rheumatology/keg373. [DOI] [PubMed] [Google Scholar]
- 157.Ding C, Cicuttini F, Parameswaran V, et al. Serum levels of vitamin D, sunlight exposure, and knee cartilage loss in older adults: the Tasmanian older adult cohort study. Arthritis Rheum. 2009;60:1381–9. doi: 10.1002/art.24486. [DOI] [PubMed] [Google Scholar]
- 158.Dougados M, Nguyen M, Berdah L, et al. Evaluation of the structure-modifying effects of diacerein in hip osteoarthritis: ECHODIAH, a three-year, placebo-controlled trial. Evaluation of the Chondromodulating Effect of Diacerein in OA of the Hip. Arthritis Rheum. 2001;44:2539–47. doi: 10.1002/1529-0131(200111)44:11<2539::aid-art434>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 159.Pelletier JP, Lajeunesse D, Reboul P, et al. Diacerein reduces the excess synthesis of bone remodeling factors by human osteoblast cells from osteoarthritic subchondral bone. J Rheumatol. 2001;28:814–24. [PubMed] [Google Scholar]
- 160.Boileau C, Tat SK, Pelletier JP, et al. Diacerein inhibits the synthesis of resorptive enzymes and reduces osteoclastic differentiation/survival in osteoarthritic subchondral bone: a possible mechanism for a protective effect against sub-chondral bone remodelling. Arthritis Res Ther. 2008;10:R71. doi: 10.1186/ar2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Boileau C, Martel-Pelletier J, Caron C, et al. Protective effects of total fraction of avocado/soybean unsaponifiables (ASU) on the structural changes in experimental dog osteoarthritis: inhibition of nitric oxide synthase and MMP-13. Arthritis Res Ther. 2009;11:R41. doi: 10.1186/ar2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kawcak CE, Frisbie DD, McIlwraith CW, et al. Evaluation of avocado and soybean unsaponifiable extracts for treatment of horses with experimentally induced osteoarthritis. Am J Vet Res. 2007;68:598–604. doi: 10.2460/ajvr.68.6.598. [DOI] [PubMed] [Google Scholar]
- 163.Cake MA, Read RA, Guillou B, Ghosh P. Modification of articular cartilage and subchondral bone pathology in an ovine meniscectomy model of osteoarthritis by avocado and soya unsaponifiables (ASU) Osteoarthritis Cartilage. 2000;8:404–11. doi: 10.1053/joca.1999.0315. [DOI] [PubMed] [Google Scholar]
- 164.Maheu E, Mazieres B, Valat JP, et al. Symptomatic efficacy of avocado/soybean unsaponifiables in the treatment of osteoarthritis of the knee and hip: a prospective, randomized, double-blind, placebo-controlled, multicenter clinical trial with a six-month treatment period and a two-month followup demonstrating a persistent effect. Arthritis Rheum. 1998;41:81–91. doi: 10.1002/1529-0131(199801)41:1<81::AID-ART11>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 165.Lequesne M, Maheu E, Cadet C, Dreiser RL. Structural effect of avocado/soybean unsaponifiables on joint space loss in osteoarthritis of the hip. Arthritis Rheum. 2002;47:50–8. doi: 10.1002/art1.10239. [DOI] [PubMed] [Google Scholar]
- 166.Wang SX, Laverty S, Dumitriu M, et al. The effects of glucosamine hydrochloride on subchondral bone changes in an animal model of osteoarthritis. Arthritis Rheum. 2007;56:1537–48. doi: 10.1002/art.22574. [DOI] [PubMed] [Google Scholar]
- 167.Tat SK, Pelletier JP, Vergés J, et al. Chondroitin and glucosamine sulfate in combination decrease the pro-resorptive properties of human osteoarthritis subchondral bone osteoblasts. Arthritis Res Ther. 2007;9:R117. doi: 10.1186/ar2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.McAlindon TE, LaValley MP, Gulin JP, Felson DT. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. J Am Med Assoc. 2000;283:1469–75. doi: 10.1001/jama.283.11.1469. [DOI] [PubMed] [Google Scholar]
- 169.Richy F, Bruyere O, Ethgen O, et al. Structural and symptomatic efficacy of glucosamine and chondroitin in knee osteoarthritis: a comprehensive meta-analysis. Arch Intern Med. 2003;163:1514–22. doi: 10.1001/archinte.163.13.1514. [DOI] [PubMed] [Google Scholar]