Statins reduce CVD and mortality risk in patients with diabetes. (1) Practice-level variation in statin use among diabetic patients in cardiology practices is unknown. Accordingly, we examined practice-level variation in statin therapy among 40-75 year-old patients with diabetes and no CVD between 05/2008 and 10/2013 from the ACC’s PINNACLE registry, a national cardiology outpatient quality improvement registry that directly extracts data from electronic medical records. Statin use was defined as its prescription at any time point during the study period, as documented in the medical records. We calculated practices’ median statin prescription rates, quarterly trends, and median rate ratio (MRR) for statin prescription and MRR for LDL-C <100 mg/dL attainment (which was the performance measure at the time) using hierarchical-modified Poisson regression models. The MRR denotes the median relative difference in treatment rates between practices for patients with similar characteristics. An MRR of 1 suggests no practice-level variation, while an MRR of 2 suggests that patients with similar characteristics, on average, are twice as likely to be treated differently with statin at any two random practices.
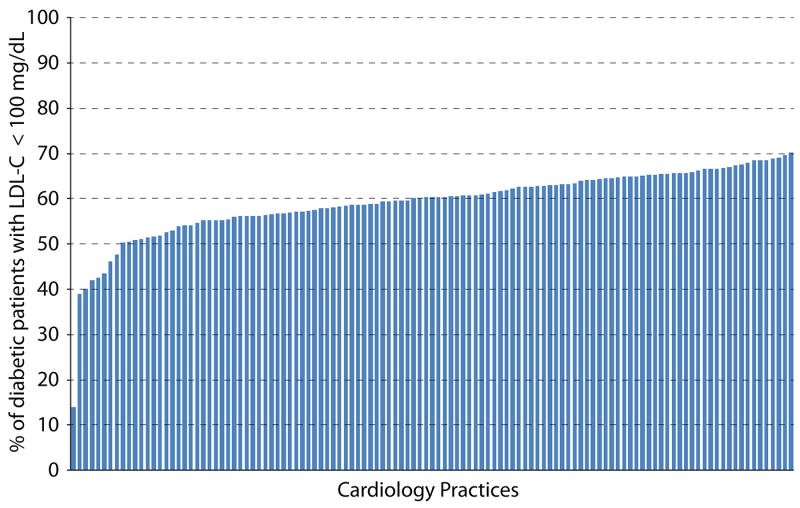
Among 215,193 patients (582,048 encounters) from 204 cardiology practices, statin was prescribed in 61.6% of patients with diabetes. Compared to patients not receiving statin, those on statins had a higher prevalence of cardiovascular risk factors, were also more likely to receive non-statin lipid-lowering therapy (LLT) [28% vs. 13%], and had a lower mean LDL-C level (90 mg/dL vs. 103 mg/dL). Among 182 practices with ≥ 30 diabetic patients, the median practice statin prescription rate was 62.3% (25th – 75th percentile: 55.7%-68.1%, Figure), with no noticeable change over time. Among patients with available LDL-C data (N=62,374), 57.7% had LDL-C<100 mg/dL. For statin use, the unadjusted MRR was 1.56 (95% CI: 1.51-1.60), which was largely unchanged after adjustment for patients’ age, gender, race, hypertension, dyslipidemia, tobacco use, insurance, provider type, and non-statin LLT use (1.57, 1.52-1.61), suggesting 57% practice-level variation in statin use for two similar patients. The corresponding MRR for LDL-C <100 mg/dL attainment were 1.47 (1.42-1.51) and 1.47 (1.42-1.50), respectively (Figure).
Figure.
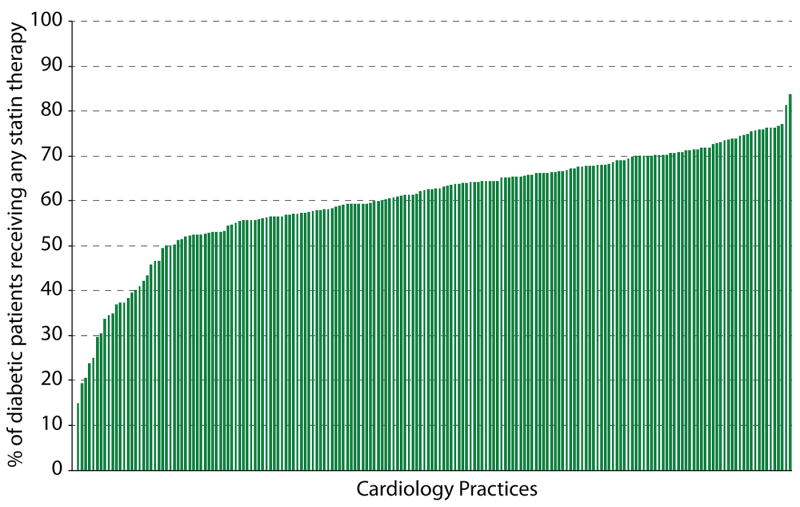
Panel A. Percentage of 40-75 years old patients with diabetes and without CVD receiving statin therapy in cardiology practices participating in the PINNACLE registry
Panel B. Percentage of 40-75 years old patients with diabetes and without CVD in cardiology practices participating in the PINNACLE registry achieving LDL-C <100 mg/Dl
In this national study of diabetic patients without CVD, statin was prescribed in 62% of patients, with wide practice variation. In a subsample, LDL-C <100 mg/dL was attained in 58%, with significant practice variation. In a Veterans Affairs (VA) study from 130 primary-care facilities, statin was prescribed in 61% of diabetic patients without CVD with a MRR of 1.20. (2) Although statin use was similar in the current study, there was larger practice-level variation, suggesting more consistent care in the VA system.
Importantly, adjustment for patient-related variables did not change the MRR, suggesting that practice/provider-related factors primarily determined variation in statin use. Identifying such barriers for optimal statin use and leveraging interventions, such as audit/feedback or decision support tools, should be tested to improve guideline-concordant practice. Increasing awareness among providers that diabetic patients may benefit from statin therapy, even with relatively lower LDL-C levels, (1) could also be helpful. The new cholesterol guideline recommends statin therapy in diabetic patients 40-75 years with LDL-C 70-189 mg/dL without atherosclerotic CVD. The current gap in care identified in this study supports national efforts to improve the use of statins in patients with diabetes.
Another reason for lower statin use could be related to documentation, including sub-optimal statin intolerance documentation. Among 5722 excluded patient encounters with documented reasons for not prescribing statin therapy (1.0 % of the sample), 89.4% were not prescribed statins for patient reasons. Although this may partly reflect patients who were intolerant of statin therapy, we did not have data describing statin intolerance. Non-statin LLT was used more often in statin users than non-users, suggesting that statin treated patients were more aggressively treated and statin intolerance may not completely explain sub-optimal statin use. Additionally, despite periodic assessments, data collection in the PINNACLE registry may not be complete.
In conclusion, 38% of patients with diabetes without CVD in cardiology practices from the PINNACLE registry had no documentation of statin prescription with significant practice-level variation. Identifying characteristics of high-performing practices, and barriers at low-performing practices, may help improve statin use in this high-risk population.
Acknowledgments
This study was supported by the 2015-2016 American Medical Association Foundation Seed Grant Award (Dr. Pokharel).
Conflict(s) of Interest/Disclosure(s):
Pokharel: Supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL110837.
Nambi: Research Grant Merck. Consultant/Advisory Board Sanofi Regeneron. Provisional patent (# 61721475) entitled “Biomarkers to Improve Prediction of Heart Failure Risk” filed by Baylor College of Medicine, Roche.
Chan: Supported by a R01 grant from the National Heart, Lung, and Blood Institute (1R01HL123980).
Kosiborod: Research Grant American Heart Association, Gilead Sciences, Genentech, SanofiAventis, Eisai. Consultant/Advisory Board Eli Lilly, Regeneron, Takeda, Edwards Lifesciences, Gilead Sciences, Roche, AstraZeneca, Amgen.
Oetgen: Employee of the American College of Cardiology
Spertus: Has a contract to analyze data from the National Cardiovascular Data Registry
Ballantyne: Grant/Research Support- All significant. (All paid to institution, not individual): Abbott Diagnostic, Amarin, Amgen, Eli Lilly, Esperion, Novartis, Pfizer, Otsuka, Regeneron, Roche Diagnostic, Sanofi-Synthelabo, Takeda, NIH, AHA, ADA. Consultant- Abbott Diagnostics, Amarin, Amgen*, Astra Zeneca*, Eli Lilly, Esperion, Genzyme, Isis, Matinas BioPharma Inc, Merck*, Novartis, Pfizer*, Regeneron, Roche, Sanofi-Synthelabo (*Significant where noted [>$10,000]; remainder modest [<$10,000])
Virani: Supported by the American Heart Association Beginning Grant-in-Aid (14BGIA20460366) and the American Diabetes Association Clinical Science and Epidemiology award (1-14-CE-44); serves on the steering committee (no financial remuneration) for the Patient and Provider Assessment of Lipid Management (PALM) Registry at the Duke Clinical Research Institute.
Others: None
Abbreviations
- ACC
American College of Cardiology
- CVD
cardiovascular disease
- LDL-C
low-density lipoprotein cholesterol
- LLT
lipid lowering therapy
- MRR
median rate ratio
- PINNACLE
Practice Innovation and Clinical Excellence registry
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 2.Pokharel YHR, Nambi V, Shah T, Woodard L, Akeroyd J, Winchester D, Ramsey D, Ballantyne C, Petersen L, Virani S. Statin Use and its Facility-Level Variation in a National Sample of Diabetic Patients. Diabetes. 64(Supplement 1):691–P. [Google Scholar]


