Abstract
Background
The Air Medical Prehospital Triage (AMPT) score was developed to identify injured patients who may benefit from scene helicopter emergency medical services (HEMS) transport. External validation using a different dataset is essential to ensure reliable performance. The study objective was to validate the effectiveness of the AMPT score to identify patients with a survival benefit from HEMS using the Pennsylvania Trauma Outcomes Study (PTOS) registry.
Methods
Patients age≥16years undergoing scene HEMS or ground EMS (GEMS) transport in the PTOS registry 2000–2013 were included. Patients with ≥2 AMPT score points were triaged to HEMS, while those with <2 points were triaged to GEMS. Multilevel Poisson regression determined the association of survival with actual transport mode across AMPT score triage assignments, adjusting for demographics, mechanism, vital signs, interventions, and injury severity. Successful validation was defined as no survival benefit for actual HEMS transport in patients triaged to GEMS by the AMPT score, with a survival benefit for actual HEMS transport in patients triaged to HEMS by the AMPT score. Subgroup analyses were performed in patients treated by advanced life support providers and patients with transport times>10mins.
Results
There were 222,827 patients included. For patients triaged to GEMS by the AMPT score, actual transport mode was not associated with survival (adjusted relative risk [ARR] 1.004; 95%CI 0.999—1.009, p=0.08). For patients triaged to HEMS by the AMPT score, actual HEMS transport was associated with a 6.7% increase in the relative probability of survival (ARR 1.067; 95%CI 1.040—1.083, p<0.001). Similar results were seen in all subgroups.
Conclusions
This study is the first to externally validate the AMPT score, demonstrating the ability of this tool to reliably identify trauma patients most likely to benefit from HEMS transport. The AMPT score should be considered when protocols for HEMS scene transport are developed and reviewed.
Level of Evidence
Level III, diagnostic criteria
Keywords: Helicopter, Emergency Medical Services, Triage, Prehospital, Validation
INTRODUCTION
Survival of severely injured patients is dependent on timely access to critical interventions and rapid transport to definitive care. Helicopter emergency medical services (HEMS) offers this, as air medical crews provide advanced prehospital care while rapidly delivering patients to a trauma center. These factors have been cited as reasons for the survival benefit seen for HEMS in several studies when compared to ground emergency medical services (GEMS).1–5
However, identifying patients that will benefit from HEMS transport at the scene of injury is challenging, given limited information and resources available in the field. Further, the high cost and aviation risks make patient selection for HEMS transport a critical issue. Despite this, few studies evaluate this problem, leading to significant variation in HEMS triage.6, 7 Many systems extrapolate existing trauma triage criteria for air medical triage. This leads to increasing costs and over-triage while limiting the potential benefits of HEMS transport, as these criteria were developed to determine whether a patient needs to go to a trauma center, not whether they need to fly to a trauma center.
Recently we developed the Air Medical Prehospital Triage (AMPT) score to identify patients most likely to benefit from scene HEMS transport.8 It incorporates seven simple criteria adapted from existing triage guidelines to generate a point total for an individual patient and provides a triage recommendation for HEMS or GEMS transport based on patient-level factors. The AMPT score represents the first attempt at developing standardized HEMS triage criteria based on improved outcome for HEMS transport.
The score was developed using the National Trauma Databank (NTDB); however, this dataset has several limitations. Further, external validation using a different dataset and population is essential to ensure reliable performance and generalizability of the AMPT score.9 The Pennsylvania Trauma Outcomes Study (PTOS) offers the ability to critically evaluate the AMPT score with a different case-mix, time period, and more granular dataset. The objective of this study was to validate the effectiveness of the AMPT score to identify patients with a survival benefit from HEMS compared to GEMS transport using the PTOS registry. We hypothesize that the AMPT score will discriminate between patients that have a survival benefit when transported by HEMS and patients that do not derive a survival benefit from HEMS transport.
METHODS
Study Population
Patients aged ≥16 years transported by either HEMS or GEMS from the scene of injury in the PTOS registry between January 1st, 2000 and June 30th, 2013 were eligible for inclusion. The PTOS dataset represents a state-wide trauma registry collecting detailed clinical data at the patient-level from 36 trauma centers over the study period. Data submission to this registry is mandatory for accreditation as a trauma center in the state of Pennsylvania. Patients were excluded if transferred from another hospital or burn was the primary mechanism of injury. Demographics, comorbidities, prehospital care, injury characteristics, vital signs, International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, procedures, complications, and outcomes were collected for each patient. The PTOS dataset was selected as it has differences in data structure, increased granularity, as well as a different time period from the original development and validation of the AMPT score dataset. This allows evaluation of AMPT score in a different population and access to different variables that may influence performance.
Missing Data
To address missing data, multiple imputation was performed for analysis variables missing between 1% and 35% of observations. Imputed variables included age, sex, race, insurance status, injury severity score (ISS), prehospital systolic blood pressure (SBP), prehospital respiratory rate (RR), prehospital Glasgow Coma Scale (GCS), and prehospital heart rate (HR). Multiple imputation using chained equations with a fully conditional specification model was performed using five imputation steps to develop five imputed datasets. Outcome models were performed using estimation techniques that combine model coefficients and standard errors from each imputed dataset while adjusting for the variability between imputed datasets.10 Missing data for imputed variables ranged from 4% (race) to 34% (prehospital SBP). Sensitivity analyses with complete cases not missing any of the imputed variables were performed to assess the multiple imputation procedures. Patients with missing data compared to complete cases were similar across median ISS (10 [5, 17] versus 10 [5, 17] p=0.22), AMPT points (0 [0, 1] versus 0 [0, 1], p=0.32), and survival (93% versus 94%, p=0.09) suggesting data were missing at random. No significant differences in study results were seen between imputed and complete case data.
Air Medical Prehospital Triage (AMPT) Score
Our group previously developed and internally validated the AMPT score using a large national dataset.8 The AMPT score criteria are shown in Table 1. The score was applied to the current study population. Presence of physiologic criteria in the score were determined using prehospital vital signs. Presence of anatomic criteria in the score were determined using ICD-9 diagnosis codes and Abbreviated Injury Scale (AIS) body regions and scores. AMPT point totals were calculated for each patient. Based on the point totals, each patient was triaged to either HEMS (≥2points) or GEMS (<2points) transport by the AMPT score. This triage assignment was made based solely on the AMPT score and independent of the actual transport mode of the patient.
Table 1.
Air Medical Prehospital Triage (AMPT) Score
| Criterion | Points |
|---|---|
|
| |
| Glasgow Coma Scale <14 | 1 |
| Respiratory Rate <10 or >29 breaths/min | 1 |
| Unstable chest wall fractures* | 1 |
| Suspected hemothorax or pneumothorax† | 1 |
| Paralysis | 1 |
| Multisystem trauma ‡ | 1 |
| PHY+ANA § | 2 |
|
| |
| Consider helicopter transport if AMPT score ≥2 points | |
Any chest wall instability or deformity including flail chest or multiple ribs fractures on physical exam
Absence of breath sounds on affected hemithorax PLUS objective signs of respiratory distress (cyanosis, SpO2<92%, signs of tension physiology)
3 or more anatomic body regions injured
any 1 physiologic criterion plus any 1 anatomic criterion present from American College of Surgeons Committee on Trauma national field triage guidelines
Statistical Analysis
The primary outcome was in-hospital survival. A multilevel random coefficient generalized linear regression model with Poisson family and log link was constructed to determine the independent association of HEMS compared to GEMS transport with survival. The model was adjusted for age, sex, race, insurance status, comorbidities, mechanism of injury, prehospital vital signs, ISS, units of blood transfusion in the emergency department (ED), prehospital time, the level of prehospital care provided (advanced life support [ALS] versus basic life support [BLS]), prehospital intubation, volume of prehospital crystalloid, surgical intervention for hemorrhage or craniotomy within 24hours of admission, and complications. The model included a random effect for centers to account for clustering at the hospital-level and allowed for the possibility that the effect of transport mode on survival may differ between centers. Robust variance estimators were utilized. Model goodness-of-fit was assessed using the Pearson chi-squared goodness-of-fit test.
Patients were divided according to AMPT score triage assignment. Within each of these AMPT score triage assignments (HEMS or GEMS), there were some patients that actually underwent HEMS transport and some that actually underwent GEMS transport. Thus, the above multilevel model was applied to each AMPT score triage assignment group to evaluate whether the actual transport mode the patient arrived at the trauma center by was associated with survival. Additionally, the model was applied to patients on either side of the score cut-off (1 and 2 AMPT points) to evaluate whether the cut-off of 2 points remains optimal. Successful validation performance of the AMPT score was defined as no survival benefit associated with actual HEMS transport among patients assigned to GEMS transport by the AMPT score, with a survival benefit associated with actual HEMS transport in patients assigned to HEMS transport by the AMPT score. To evaluate the 2-point cut-off for triage assignments, we evaluated patients with only 2 AMPT points as well as those with only 1 AMPT point to ensure consistent HEMS survival benefits were seen for patients with only 2 points, but no HEMS benefit for patients with only 1 point.
Our condition of no survival benefit for HEMS in patients assigned to GEMS by the AMPT score could include a finding of no association between survival and transport mode. To ensure this is not due to type II error, we evaluated the treatment effect size detectable with our sample size of patients assigned to GEMS by the AMPT score. The current study sample has 90% power to detect a difference between groups with a relative risk of 1.003 or 0.36% difference in survival. Thus, this study has the power to detect a clinically significant difference in survival between groups. Further, a non-inferiority analysis was performed for patients assigned to GEMS by the AMPT score (Text, SDC 1).
Continuous data are presented as median (interquartile range [IQR]). Continuous variables were compared using Wilcoxon rank-sum tests, and categorical variables were compared using Chi-squared tests. Adjusted relative risk (ARR) with 95% confidence intervals (95%CI) were obtained from regression models. A two-sided p value ≤0.05 was considered significant. Data analysis was conducted using Stata v13MP (StataCorp; College Station, TX).
Subgroup Analyses
To further explore the validity of the AMPT score, several sub-group analyses were performed. One limitation of the dataset used for AMPT score development is the inability to determine the level of care of prehospital providers.8 Bias may result when comparing survival between patients transported by ground BLS providers and ALS air medical providers, as ALS providers may perform advance procedures such as invasive airway placement and intravenous resuscitation that can influence survival. Thus, we repeated the above analysis restricted to patients only treated by ALS prehospital providers. In Pennsylvania, HEMS provides critical care transport services, offering additional capabilities beyond GEMS ALS providers. Thus, this subgroup analysis compares the highest levels of care for GEMS and HEMS.
Further, some patients are injured so close to a trauma center that HEMS transport is impractical. A survival bias may be introduced by including these patients in the GEMS transport group, as some may be severely injured but survive a relatively short transport to a trauma center whereas they would not have survived if transported from farther away by HEMS. Thus, to capture patients with the potential to undergo HEMS transport and avoid this survival bias, a second subgroup analysis was performed restricted to patients with a transport time >10 minutes, which represents the 25th percentile of transport time in the study population. The final subgroup analysis was performed in patients treated by ALS prehospital providers and had a transport time >10 minutes.
Sensitivity Analysis
A sensitivity analysis was also performed excluding patients in prehospital cardiac arrest with cardiopulmonary resuscitation (CPR), as these patients are generally not eligible for HEMS transport and would be taken to the nearest hospital by GEMS. These patients have very low survival and inclusion may bias results against GEMS transport. This analysis was performed in all subgroups.
RESULTS
Study Population
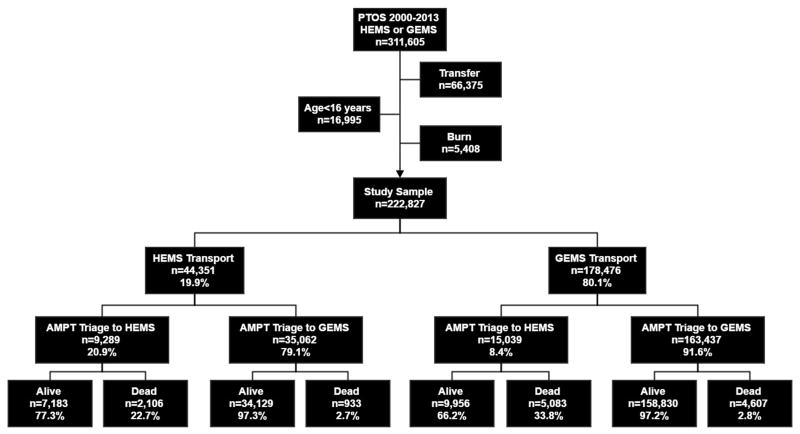
A total of 222,827 patients were included with 44,351 (19.9%) undergoing HEMS transport (Fig. 1). Patients transported by HEMS were younger, less likely to have penetrating injury, had higher injury severity, were more likely to require prehospital procedures or in-hospital surgical intervention (Table 2). Unadjusted survival was lower in the HEMS transport group.
Figure 1.
Study participant selection from the Pennsylvania Trauma Outcomes Study (PTOS) 2000—2013. Distribution of helicopter emergency medical service (HEMS) and ground emergency medical service (GEMS) transports, Air Medical Prehospital Triage (AMPT) score triage assignment, and survival are show. Reported percent represent proportion of the group one level above.
Table 2.
Characteristics of patients transported by HEMS and GEMS
| HEMS n = 44,351 |
GEMS n = 178,476 |
p value | |
|---|---|---|---|
| Age [years; med (IQR)] | 41 (25, 56) | 52 (32, 75) | <0.001 |
| Sex [n (%) male] | 30,965 (70) | 104,890 (59) | <0.001 |
| Insurance Status [n (%)] | <0.001 | ||
| Commercial | 31,168 (71) | 83,016 (47) | |
| Subsidized/None | 12,716 (29) | 93,986 (53) | |
| Race [n (%)] | <0.001 | ||
| White | 39,571 (93) | 134,280 (78) | |
| Non-White | 3,180 (7) | 37,118 (22) | |
| Number of comorbidities [med (IQR)] | 1 (0, 2) | 1 (0, 3) | <0.001 |
| Prehospital response time [mins; med (IQR)] | 15 (11, 20) | 7 (4, 11) | <0.001 |
| Prehospital scene time [mins; med (IQR)] | 15 (11, 22) | 15 (11, 20) | <0.001 |
| Prehospital transport time [mins; med (IQR)] | 17 (13, 22) | 17 (11, 26) | <0.001 |
| Total prehospital time [mins; med (IQR)] | 50 (41, 61) | 40 (31, 53) | <0.001 |
| Prehospital level of care [n (%) ALS] | 42,841 (97) | 119,545 (74) | <0.001 |
| Prehospital intubation [n (%)] | 8058 (18) | 1,999 (1) | <0.001 |
| Prehospital crystalloid volume [n (%)] | <0.001 | ||
| None | 2,001 (5) | 65,128 (43) | |
| <500mL | 18,151 (47) | 39,786 (26) | |
| 500–2000mL | 13,079 (34) | 17,002 (11) | |
| >2000mL | 742 (2) | 302 (0.2) | |
| Unknown volume | 4,801 (12) | 28,711 (19) | |
| Prehospital RR<10 or >29bpm [n (%)] | 5,101 (13) | 7,194 (6) | <0.001 |
| Prehospital GCS≤13 [n (%)] | 11,441 (31) | 23,679 (18) | <0.001 |
| Unstable chest wall fractures [n (%)] | 4,564 (10) | 9,971 (6) | <0.001 |
| Paralysis [n (%)] | 558 (1) | 845 (0.5) | <0.001 |
| Hemothorax or Pneumothorax [n (%)] | 8,740 (20) | 17,266 (10) | <0.001 |
| Multisystem injury [n (%)] | 4,414 (10) | 5,226 (3) | <0.001 |
| PHY + ANA injury [n (%)] | 3,911 (9) | 8,066 (5) | <0.001 |
| Surgery within 24hrs for hemorrhage or craniotomy [n (%)] | 4,219 (10) | 11,934 (7) | <0.001 |
| Number of complications [med (IQR)] | 0 (0, 0) | 0 (0, 0) | <0.001 |
| ISS [med (IQR)] | 14 (9, 25) | 9 (5, 17) | <0.001 |
| Survival [n (%)] | 41,312 (93) | 168,786 (95) | <0.001 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; ALS, advanced life support; RR, respiratory rate; GCS, Glasgow Coma Scale; PHY + ANA, any one physiologic criterion plus any one anatomic criterion
Overall, 24,328 (10.9%) of patients were triaged to HEMS transport by the AMPT score (Table 3). Among patients triaged to HEMS transport by the AMPT score, 38.2% actually underwent HEMS transport, while 17.7% of patients triaged to GEMS transport by the AMPT score actually underwent HEMS transport (p<0.001). The five most common AMPT score criteria combinations with ≥2 point accounted for 50% of patients triaged to HEMS (Table, SDC 2). A total of 865 (3.6%) patients were triaged to HEMS by the physiologic plus anatomic triage criterion alone. Among patients actually transported by HEMS, 18,667 (42.1%) had an AMPT score of zero.
Table 3.
Characteristics of patients by AMPT Score assignment and actual transport mode concordance
| AMPT triage HEMS | AMPT triage GEMS | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| HEMS n = 9,289 |
GEMS n = 15,039 |
p value | HEMS n = 35,062 |
GEMS n = 163,437 |
p value | |
| Age [years; med (IQR)] | 40 (24, 55) | 40 (25, 58) | <0.001 | 41 (25, 56) | 53 (34, 76) | <0.001 |
| Sex [n (%) male] | 30,965 (70) | 104,890 (59) | <0.001 | 24,193 (69) | 94,793 (58) | <0.001 |
| Insurance Status [n (%)] | <0.001 | <0.001 | ||||
| Commercial | 6,557 (72) | 7,283 (49) | 24,894 (71) | 76,815 (47) | ||
| Subsidized/None | 2,604 (28) | 7,571 (51) | 10,168 (29) | 86,622 (53) | ||
| Race [n (%)] | <0.001 | <0.001 | ||||
| White | 8,387 (93) | 9,727 (68) | 32,608 (93) | 130,750 (80) | ||
| Non-White | 606 (7) | 4,583 (32) | 2,454 (7) | 32,687 (20) | ||
| Number of comorbidities [med (IQR)] | 1 (0, 1) | 1 (0, 2) | <0.001 | 1 (0, 2) | 1 (0, 3) | <0.001 |
| Prehospital response time [mins; med (IQR)] | 15 (11, 20) | 7 (4, 9) | <0.001 | 15 (11, 20) | 7 (4, 11) | <0.001 |
| Prehospital scene time [mins; med (IQR)] | 20 (13, 28) | 13 (9, 17) | <0.001 | 15 (11, 20) | 15 (11, 20) | 0.004 |
| Prehospital transport time [mins; med (IQR)] | 17 (13, 22) | 13 (9, 20) | <0.001 | 17 (13, 24) | 17 (11, 26) | <0.001 |
| Total prehospital time [mins; med (IQR)] | 55 (45, 66) | 33 (24, 44) | <0.001 | 50 (41, 61) | (41 (31, 52) | <0.001 |
| Prehospital level of care [n (%) ALS] | 9,156 (99) | 13,932 (92) | <0.001 | 33,660 (96) | 117,675 (72) | <0.001 |
| Prehospital intubation [n (%)] | 4,456 (48) | 1,221 (8) | <0.001 | 1,402 (4) | 161 (0.1) | <0.001 |
| Prehospital crystalloid volume [n (%)] | <0.001 | <0.001 | ||||
| None | 243 (3) | 2,710 (20) | 1,752 (5) | 71,850 (44) | ||
| <500mL | 2,749 (33) | 3,979 (30) | 18,930 (54) | 47,359 (29) | ||
| 500–2000mL | 3,982 (48) | 3,199 (24) | 10,172 (29) | 16,296 (10) | ||
| >2000mL | 379 (5) | 110 (1) | 351 (1) | 151 (0.1) | ||
| Unknown volume | 898 (11) | 3,393 (25) | 3,857 (11) | 27,781 (17) | ||
| Prehospital RR<10 or >29bpm [n (%)] | 4,568 (49) | 5,962 (40) | <0.001 | 344 (1) | 1,634 (1) | <0.001 |
| Prehospital GCS≤13 [n (%)] | 6,458 (70) | 9,760 (65) | <0.001 | 4,558 (13) | 17,978 (11) | <0.001 |
| Unstable chest wall fractures [n (%)] | 2,968 (32) | 4,991 (33) | 0.046 | 1,052 (3) | 3,269 (2) | <0.001 |
| Paralysis [n (%)] | 292 (3) | 408 (3) | 0.051 | 355 (1) | 327 (0.2) | <0.001 |
| Hemothorax or Pneumothorax [n (%)] | 4,757 (51) | 7,248 (48) | <0.001 | 3,156 (9) | 8,171 (5) | <0.001 |
| Multisystem injury [n (%)] | 2,771 (30) | 3,105 (21) | <0.001 | 701 (2) | 1,530 (1) | <0.001 |
| PHY + ANA injury [n (%)] | 3,271 (35) | 7,344 (49) | <0.001 | 0 (0) | 0 (0) | NA |
| Surgery within 24hrs for hemorrhage or craniotomy [n (%)] | 1,819 (20) | 3,236 (22) | <0.001 | 2,104 (6) | 8,027 (5) | <0.001 |
| Number of complications [med (IQR)] | 0 (0, 1) | 0 (0, 1) | <0.001 | 0 (0, 0) | 0 (0, 0) | <0.001 |
| ISS [med (IQR)] | 27 (17, 35) | 24 (14, 34) | <0.001 | 11 (6, 17) | 9 (5, 14) | <0.001 |
| Survival [n (%)] | 7,183 (77) | 9,956 (66) | <0.001 | 34,010 (97) | 158,535 (97) | 0.170 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; ALS, advanced life support; RR, respiratory rate; GCS, Glasgow Coma Scale; PHY + ANA, any one physiologic criterion plus any one anatomic criterion
When evaluating the overall effect of transport mode in the study population, HEMS was independently associated with an 2.4% increase in the relative probability of survival (ARR 1.024; 95%CI 1.013—1.035, p<0.001). The risk-adjustment model fit the data adequately with a non-significant Pearson goodness-of-fit test (p>0.999).
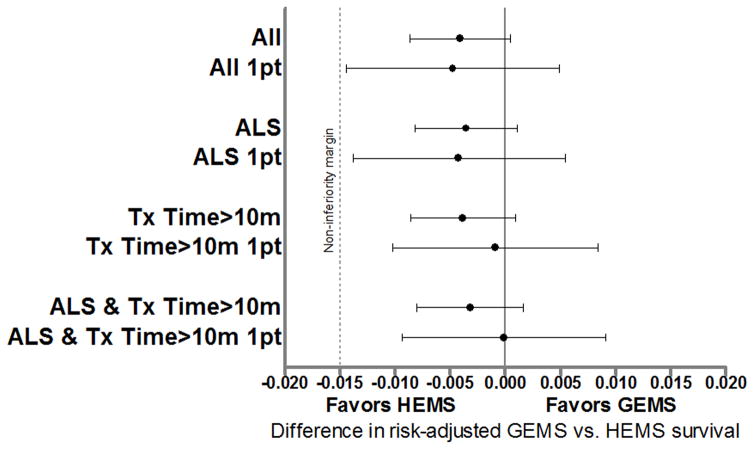
AMPT Score Performance
For patients triaged to GEMS transport by the AMPT score (0 or 1 point), actual transport mode was not associated with survival (ARR 1.004; 95%CI 0.999—1.009, p=0.077) and non-inferiority of GEMS transport was demonstrated (Fig. 2). For patients triaged to HEMS transport by the AMPT score (≥2 points), actual transport by HEMS was independently associated with a 6.7% increase in the relative probability of survival (ARR 1.067; 95%CI 1.040—1.094, p<0.001). This association between HEMS transport and increased relative probability of survival remained in patients with only 2 points from the AMPT score (ARR 1.058; 95%CI 1.033—1.083, p<0.001). There was, however, no association between transport mode and survival in patients with only 1 point from the AMPT score (ARR 1.005; 95%CI 0.995—1.016, p=0.331) and non-inferiority was again shown for GEMS (Fig. 2).
Figure 2.
Non-inferiority evaluation of patients triaged to ground emergency medical services (GEMS) by the Air Medical Prehospital Triage (AMPT) score. The non-inferiority margin was set at 1.5% for the difference between GEMS and helicopter emergency medical services (HEMS) risk-adjusted survival. Non-inferiority is established if the lower 95% confidence interval (95%CI) bound for the difference in risk-adjusted survival for GEMS versus HEMS is not lower than the non-inferiority margin.
1pt, 1 point; ALS, advanced life support; Tx time, transport time
Subgroup Analyses
When evaluating patients treated by prehospital ALS providers only, 16.3% of patients were triaged to HEMS transport by the AMPT score overall. Among patients triaged to HEMS transport by the AMPT score, 39.2% actually underwent HEMS transport, while 21.5% of patients triaged to GEMS transport actually underwent HEMS transport (p<0.001). In this subgroup, there was no association between actual transport mode and survival among patients triaged to GEMS transport by the AMPT score and non-inferiority was demonstrated for GEMS transport (Fig. 2), while actual HEMS transport was associated with an increase in the relative probability of survival among patients triaged to HEMS transport by the AMPT score (Table 4).
Table 4.
Treatment effect estimates for association between actual transport mode (HEMS versus GEMS) and survival in subgroup analyses
| Subgroup | Adjusted Relative Risk for actual transport mode (HEMS vs. GEMS) | 95% Confidence Interval | p value |
|---|---|---|---|
| ALS providers only | |||
| Triaged to GEMS by AMPT | 1.003 | 0.998—1.008 | 0.130 |
| Triaged to HEMS by AMPT | 1.067 | 1.041—1.094 | <0.001 |
| 1 point from AMPT | 1.005 | 0.994—1.015 | 0.389 |
| 2 points from AMPT | 1.058 | 1.033—1.083 | <0.001 |
|
| |||
| >10-minute transport time | |||
| Triaged to GEMS by AMPT | 1.004 | 0.999—1.008 | 0.109 |
| Triaged to HEMS by AMPT | 1.056 | 1.035—1.079 | <0.001 |
| 1 point from AMPT | 1.001 | 0.991—1.011 | 0.837 |
| 2 points from AMPT | 1.046 | 1.023—1.070 | <0.001 |
|
| |||
| ALS providers only and >10-minute transport time | |||
| Triaged to GEMS by AMPT | 1.003 | 0.998—1.008 | 0.193 |
| Triaged to HEMS by AMPT | 1.058 | 1.036—1.080 | <0.001 |
| 1 point from AMPT | 1.000 | 0.990—1.010 | 0.969 |
| 2 points from AMPT | 1.046 | 1.023—1.071 | <0.001 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; ALS, advanced life support; AMPT, Air Medical Prehospital Triage score
When evaluating patients with a transport time >10 minutes, 13.8% of patients were triaged to HEMS transport by the AMPT score overall. Of patients triaged to HEMS transport, 46.2% actually underwent HEMS transport, while 21.5% of patients triaged to GEMS transport by the AMPT score actually underwent HEMS transport (p<0.001). Again, there was no association between transport mode and survival for patients triaged to GEMS by the AMPT score and non-inferiority was shown for GEMS (Fig. 2), while those triaged to HEMS transport by the AMPT score did have a survival benefit when actually transported by HEMS (Table 4).
Finally, when evaluating only patients treated by ALS providers with a transport time >10 minutes, 14.9% of patients were triaged to HEMS transport overall. Among patients triaged to HEMS transport, 47.3% actually underwent HEMS transport, while 24.1% of patients triaged to GEMS transport by the AMPT score actually underwent HEMS transport (p<0.001). The AMPT score again performed well, as patients triaged to GEMS transport by the AMPT score did not have a survival benefit from HEMS transport (Fig. 2), while patients triaged to HEMS by the AMPT score had a 5.8% increase in the relative probability of survival when actually transported by HEMS (Table 4). Among all three subgroups studied, the 2-point cut-off for the AMPT score remained optimal (Table 4).
Sensitivity Analysis
For sensitivity analysis, 2,357 patients were in prehospital cardiac arrest with CPR ongoing. Among this group, 5% survived to hospital discharge. Excluding these patients resulted similar treatment effect estimates in the overall study population and each subgroup when compared to the main results (Table, SDC 3).
DISCUSSION
The current study demonstrates that the AMPT score performs well when applied to an external dataset. The AMPT score was able to discriminate between patients at the scene of injury that had a survival benefit when transported by HEMS and those that did not. The AMPT score maintained its performance when applying the AMPT score to patients treated only by ALS providers, patients with transport times >10 minutes, as well as those treated by ALS providers with transport times >10 minutes. A 2-point cut-off was confirmed to be the optimal threshold for triaging patient to GEMS or HEMS in this dataset.
External validation of any prediction model is critical to support generalizability and clinical utility. The PTOS dataset addresses primarily the temporal and methodological aspects of external validation.11 The PTOS data set was collected over a longer time period, including earlier and later periods and thus evaluates temporal validity of the AMPT score. Methodologic validity refers to evaluation using data with different collection methods or data structure. PTOS data is much more granular, with different data structure than the NTDB. This allows use of additional important variables for risk-adjustment that may impact performance of the AMPT score. Further, there is generally less missing data in the PTOS dataset, increasing reliability. Data submission is mandatory for PTOS while submission to NTDB is voluntary and thus sampling may be different between these datasets. Another advantage of the PTOS dataset is the ability to identify the level of prehospital care. This allows mitigation of the bias that may exist if comparing care from highly trained air medical providers to BLS care in GEMS transport as may have occurred in the NTDB where prehospital level of care is unknown.
Patients may benefit from HEMS for several reasons. First, it is widely accepted that HEMS is faster than GEMS. Prehospital care from HEMS may also benefit patients, either due to advanced capabilities or “regionalized” prehospital trauma care as HEMS providers more frequently care for severely injured patients.2, 12 Many AMPT score criteria identify patients with significant chest trauma and high likelihood of airway problems. As there is evidence to suggest airway management in the hands of HEMS crews leads to improved outcomes,13–17 this may explain some success of the AMPT score. Finally, HEMS may expand access to trauma care for patients that otherwise would be taken to a non-trauma center.18
However, the benefit of HEMS transport in trauma patients has been widely debated. Several studies have found no increase in survival for HEMS transport,19–23 while others report benefits.3–5, 24–26 Additionally, some authors have only found a benefit of HEMS in particular subgroups of patients based on specific injuries or injury severity.19, 21, 27, 28 Even studies that demonstrate a survival benefit suggest high over-triage among HEMS transports.3, 26, 29 Thus, it is clear that not every HEMS patient under current utilization practices is benefiting from this resource.
This issue becomes more striking when considering the costs and risks of HEMS. Hourly operating costs for HEMS are 5 to 7-fold higher than those of GEMS agencies when factoring in aircraft maintenance, fuel, and personnel.30 Although prehospital providers are at higher risk of injury due to crash than the general population, HEMS accidents are more frequently fatal with a nearly 6-fold higher number of fatalities per 100,000 transports.31–33
It becomes clear then that patient selection becomes a paramount consideration in HEMS. Despite this, there has been little evidence addressing this issue. One review reported only five studies published up to 2009 to evaluate HEMS triage in trauma.6 The low quality of evidence has hampered efforts to develop evidence based guidelines for HEMS transport in trauma,34 and the American College of Surgeons called for research to develop evidence in this area.35 Subsequently, many systems extrapolate existing trauma triage criteria for air medical triage; however, these are fundamentally different questions. Trauma triage criteria seek to identify patients that benefit from transport to a trauma center. Air medical triage seeks to identify patients requiring a trauma center that would benefit from HEMS transport. In other words, needing to go to a trauma center is not the same as needing to fly to a trauma center. Our group initially evaluated the National Field Triage Guidelines criteria, demonstrating only a subset of five physiologic and anatomic criteria identified patients with a survival benefit from HEMS transport.36
Based on this, we undertook development of the AMPT score with the goal of a simple score that would be feasible for field use.8 We utilized the NTDB and stratified patients by presence of published trauma and air medical triage criteria in a training cohort. We then determined which criteria identify patients that have a risk-adjusted survival benefit when transported by HEMS compared to GEMS. These criteria were combined into the AMPT score and applied to a separate validation cohort to determine the optimal score cut-off to identify patients benefiting from HEMS transport. The current study confirms the AMPT score performed well in an external dataset.
It is imperative to note the AMPT score cannot be used in isolation. The AMPT score does not account for logistical factors such as distance, traffic patterns, weather, and availability of transport resources, all of which play a crucial role in the decision to use HEMS transport in individual circumstances.6, 37, 38 A significant proportion of actual HEMS transports had an AMPT score of zero; however, it is unclear how many of these may have been due to extreme distances to a trauma center which can be a valid reason for HEMS transport. Additionally, the scope of care among GEMS providers, availability of GEMS transport resources, and remaining EMS coverage influence the role of HEMS among individual trauma systems. These factors cannot be evaluated using traditional outcome measures such as survival, but require innovative methods of assessment and integration into air medical transport protocols. The AMPT score only represents one aspect of air medical triage considerations. It can, however, serve as a starting point for tailored approaches to air medical transport, representing the first evidence based patient-level criteria for HEMS triage in trauma.
Finally, it is worth noting based on the distribution of triage assignments and actual transport mode that the AMPT score is not simply a restrictive triage approach to reduce the number of patients transported by HEMS, but an attempt to identify the set of patients most likely to benefit and make HEMS triage more effective. Implementation of the AMPT score in conjunction with logistical and individual system factors may not necessarily reduce the number of HEMS transports significantly, rather just transport patients that require HEMS.
This study has several limitations. First is its retrospective design. Second as this is a registry based study, data were not collected specifically for the current study. However, the PTOS dataset contains more granular patient-level data for risk-adjustment than the NTDB originally used to develop the AMPT score. As the NTDB is a national sample and our original development study was conducted for admission years 2007–2012, it is possible some of the patients included in this study from PTOS over those years were also included in the original derivation study; however, the more granular data elements still allows methodological validation. Missing data were present, particularly in prehospital variables including substantial SBP data. Multiple imputation was used to mitigate this and has been validated in trauma registry data previously.39, 40 No substantial differences were seen in the results of sensitivity analysis using complete cases only, engendering confidence in the imputed results presented here to maintain statistical power.
As the PTOS dataset collects data from only trauma centers, we cannot evaluate injured patients transported to non-trauma centers. Anatomic criteria were derived from hospital ICD-9 codes and it is unclear whether these criteria were recognized by providers in the field. Prospective study is necessary to ensure these criteria are identified in the field reliably. There is inevitable selection bias and it is impossible to fully evaluate all factors resulting in individual transport decisions in a dataset such as this.
We accounted for prehospital times; however, although related, we did not have transport distances which plays an important role in HEMS triage.41 Prehospital times showed that the median time for HEMS was longer than GEMS, primarily due to longer response times. When looking at long transports (prehospital times >60 minutes) HEMS continues to have longer response times, but does have shorter transport times (24 minutes versus 37 minutes). Again, however, these HEMS transports are coming from much farther away and it is difficult to directly compare transport modes based on time alone.
Other important outcomes such as health related quality of life are not available, but remain important to evaluate in severely injured patients. Further, we cannot determine the underlying mechanisms that result in a survival benefit for HEMS in this dataset. Finally, it should be noted that the AMPT score was developed to help guide trauma triage decisions made in the field by providers after patient contact. It was not meant to influence locally developed dispatch or launch criteria that incorporate other factors such as mechanism, distance, and terrain into the HEMS triage process.
CONCLUSION
This study is the first to externally validate the AMPT score, demonstrating the ability of this tool to correctly and reliably identify trauma patients most likely to benefit from HEMS transport. The AMPT score directly addresses the need for standardized HEMS triage criteria and can help guide future study in this area. These findings warrant prospective study of the AMPT score in further investigation of HEMS triage. The AMPT score should be considered with individual system factors when protocols for HEMS scene transport are developed and reviewed.
Supplementary Material
Ten most-common AMPT score patterns among patients triaged to HEMS (N=24,328)
Treatment effect estimates for association between actual transport mode (HEMS versus GEMS) and survival when excluding patients in prehospital cardiac arrest.
Supplemental methods.
Acknowledgments
No funding or support was directly received to perform the current study. Dr. Brown receives support from an institutional T32 Ruth L. Kischstein National Research Service Award training grant (5T32GM008516-20) from the National Institutes of Health.
Footnotes
There are no conflicts of interest for the current study
This paper was presented at the 75th annual meeting of the American Association for the Surgery of Trauma, September 14–17, 2016, in Waikoloa, Hawaii.
AUTHOR CONTRIBUTIONS: J.B.B. and M.L.G designed the study and performed the literature search. J.B.B. and J.L.S. performed the data collection. J.B.B performed the data analysis. J.B.B., M.L.G., M.R.R and J.L.S participated in initial manuscript preparation. All authors contributed to data interpretation and critical revision of the manuscript.
References
- 1.Galvagno SM., Jr Comparative effectiveness of helicopter emergency medical services compared to ground emergency medical services. Crit Care. 2013;17:169. doi: 10.1186/cc12779. Epub ahead of print 2013/07/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Helicopter transport improves survival following injury in the absence of a time-saving advantage. Surgery. 2016;159:947–959. doi: 10.1016/j.surg.2015.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034. doi: 10.1097/TA.0b013e3181f6f450. discussion 1034–1036. [DOI] [PubMed] [Google Scholar]
- 4.Galvagno SM, Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, Jr, Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307:1602–1610. doi: 10.1001/jama.2012.467. Epub ahead of print 2012/04/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care. 2011;15:295–302. doi: 10.3109/10903127.2011.569849. [DOI] [PubMed] [Google Scholar]
- 6.Ringburg AN, de Ronde G, Thomas SH, van Lieshout EM, Patka P, Schipper IB. Validity of helicopter emergency medical services dispatch criteria for traumatic injuries: a systematic review. Prehosp Emerg Care. 2009;13:28–36. doi: 10.1080/10903120802472012. [DOI] [PubMed] [Google Scholar]
- 7.Tiamfook-Morgan TO, Kociszewski C, Browne C, Barclay D, Wedel SK, Thomas SH. Helicopter scene response: regional variation in compliance with air medical triage guidelines. Prehosp Emerg Care. 2008;12:443–450. doi: 10.1080/10903120802290794. [DOI] [PubMed] [Google Scholar]
- 8.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Development and validation of the Air Medical Prehospital Triage score for helicopter transport of trauma patients. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001496. Epub ahead of print Oct 1, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altman DG, Royston P. What do we mean by validating a prognostic model? Statist Med. 2000;19:453–473. doi: 10.1002/(sici)1097-0258(20000229)19:4<453::aid-sim350>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 10.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 1987. [Google Scholar]
- 11.Steyerberg EW. Clinical Predication Models. New York: Springer; 2009. Validation of Prediction Models; pp. 299–311. [Google Scholar]
- 12.Brown JB, Sperry JL, Fombona A, Billiar T, Peitzman AB, Guyette FX. Pre-Trauma Center Red Blood Cell Transfusion is Associated with Improved Early Outcomes in Air Medical Trauma Patients. J Am Coll Surg. 2015;220:797–808. doi: 10.1016/j.jamcollsurg.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cudnik MT, Newgard CD, Wang H, Bangs C, Herrington Rt. Distance impacts mortality in trauma patients with an intubation attempt. Prehosp Emerg Care. 2008;12:459–466. doi: 10.1080/10903120802290745. [DOI] [PubMed] [Google Scholar]
- 14.Davis DP, Peay J, Sise MJ, Kennedy F, Simon F, Tominaga G, Steele J, Coimbra R. Prehospital airway and ventilation management: a trauma score and injury severity score-based analysis. J Trauma. 2010;69:294–301. doi: 10.1097/TA.0b013e3181dc6c7f. [DOI] [PubMed] [Google Scholar]
- 15.Fakhry SM, Scanlon JM, Robinson L, Askari R, Watenpaugh RL, Fata P, Hauda WE, Trask A. Prehospital rapid sequence intubation for head trauma: conditions for a successful program. J Trauma. 2006;60:997–1001. doi: 10.1097/01.ta.0000217285.94057.5e. [DOI] [PubMed] [Google Scholar]
- 16.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Annals of Emergency Medicine. 2004;44:439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Brown JB, Rosengart MR, Forsythe RM, Reynolds BR, Gestring ML, Hallinan WM, Peitzman AB, Billiar TR, Sperry JL. Not all prehospital time is equal: Influence of scene time on mortality. J Trauma Acute Care Surg. 2016;81:93–100. doi: 10.1097/TA.0000000000000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 19.Brathwaite CE, Rosko M, McDowell R, Gallagher J, Proenca J, Spott MA. A critical analysis of on-scene helicopter transport on survival in a statewide trauma system. J Trauma. 1998;45:140–144. doi: 10.1097/00005373-199807000-00029. discussion 144–146. Epub ahead of print 1998/07/29. [DOI] [PubMed] [Google Scholar]
- 20.Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, Minei JP, Warden C, Rizoli S, Morrison LJ, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2012;72:567–573. doi: 10.1097/TA.0b013e31824baddf. discussion 573–565; quiz 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cunningham P, Rutledge R, Baker CC, Clancy TV. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma. 1997;43:940–946. doi: 10.1097/00005373-199712000-00013. Epub ahead of print 1998/01/07. [DOI] [PubMed] [Google Scholar]
- 22.Schiller WR, Knox R, Zinnecker H, Jeevanandam M, Sayre M, Burke J, Young DH. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma. 1988;28:1127–1134. doi: 10.1097/00005373-198808000-00004. Epub ahead of print 1988/08/01. [DOI] [PubMed] [Google Scholar]
- 23.Shatney CH, Homan SJ, Sherck JP, Ho CC. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma system. J Trauma. 2002;53:817–822. doi: 10.1097/00005373-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Helicopter transport improves survival following injury in the absence of a time-saving advantage. Surgery. 2015 doi: 10.1016/j.surg.2015.09.015. Epub ahead of print Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ryb GE, Dischinger P, Cooper C, Kufera JA. Does helicopter transport improve outcomes independently of emergency medical system time? J Trauma Acute Care Surg. 2013;74:149–154. doi: 10.1097/TA.0b013e31827890cc. discussion 154–146. [DOI] [PubMed] [Google Scholar]
- 26.Stewart KE, Cowan LD, Thompson DM, Sacra JC, Albrecht R. Association of direct helicopter versus ground transport and in-hospital mortality in trauma patients: a propensity score analysis. Acad Emerg Med. 2011;18:1208–1216. doi: 10.1111/j.1553-2712.2011.01207.x. [DOI] [PubMed] [Google Scholar]
- 27.Bekelis K, Missios S, Mackenzie TA. Prehospital Helicopter Transport and Survival of Patients With Traumatic Brain Injury. Ann Surg. 2014 doi: 10.1097/SLA.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters improve survival in seriously injured patients requiring interfacility transfer for definitive care. J Trauma. 2011;70:310–314. doi: 10.1097/TA.0b013e3182032b4f. [DOI] [PubMed] [Google Scholar]
- 29.Brown JB, Leeper CM, Sperry JL, Peitzman AB, Billiar TR, Gaines BA, Gestring ML. Helicopters and injured kids: Improved survival with scene air medical transport in the pediatric trauma population. J Trauma Acute Care Surg. 2016;80:702–710. doi: 10.1097/TA.0000000000000971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Delgado MK, Staudenmayer KL, Wang NE, Spain DA, Weir S, Owens DK, Goldhaber-Fiebert JD. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62:351–364. e319. doi: 10.1016/j.annemergmed.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bledsoe BE, Smith MG. Medical Helicopter Accidents in the United States: A 10-Year Review. The Journal of Trauma: Injury, Infection, and Critical Care. 2004;56:1325–1329. doi: 10.1097/01.ta.0000109001.35996.af. [DOI] [PubMed] [Google Scholar]
- 32.Blumen IJ, Lees D. Air Medical Safety: Your First Priority. In: Blumen IJ, Lemkin DL, editors. Principles and Direction of Air Medical Transport. Salt Lake City, UT: Air Medical Physician Association; 2006. pp. 519–532. [Google Scholar]
- 33.National Highway Traffic Safety Administration. [Accessed: April 4th, 2015];NHTSA and Ground Ambulance Crashes. 2014 Available at: http://www.ems.gov/pdf/GroundAmbulanceCrashesPresentation.pdf.
- 34.Thomas SH, Brown KM, Oliver ZJ, Spaite DW, Lawner BJ, Sahni R, Weik TS, Falck-Ytter Y, Wright JL, Lang ES. An Evidence-based Guideline for the air medical transportation of prehospital trauma patients. Prehosp Emerg Care. 2014;18(Suppl 1):35–44. doi: 10.3109/10903127.2013.844872. [DOI] [PubMed] [Google Scholar]
- 35.Doucet J, Bulger E, Sanddal N, Fallat M, Bromberg W, Gestring M Emergency Medical System Subcommittee CoTACoS. Appropriate use of helicopter emergency medical services for transport of trauma patients: guidelines from the Emergency Medical System Subcommittee, Committee on Trauma, American College of Surgeons. J Trauma Acute Care Surg. 2013;75:734–741. doi: 10.1097/TA.0b013e3182a5389e. [DOI] [PubMed] [Google Scholar]
- 36.Brown JB, Forsythe RM, Stassen NA, Gestring ML. The National Trauma Triage Protocol: can this tool predict which patients with trauma will benefit from helicopter transport? J Trauma Acute Care Surg. 2012;73:319–325. doi: 10.1097/TA.0b013e3182572bee. [DOI] [PubMed] [Google Scholar]
- 37.Air Medical Physicians Association. [Accessed: Jan 13, 2015];Appropriate and Safe Utilization of Helicopter Emergency Medical Services. Available at: https://ampa.org/node/64.
- 38.Thomson DP, Thomas SH. Guidelines for air medical dispatch. Prehosp Emerg Care. 2003;7:265–271. doi: 10.1080/10903120390936923. Epub ahead of print 2003/04/25. [DOI] [PubMed] [Google Scholar]
- 39.Haider AH, Saleem T, Leow JJ, Villegas CV, Kisat M, Schneider EB, Haut ER, Stevens KA, Cornwell EE, 3rd, MacKenzie EJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214:756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore L, Hanley JA, Lavoie A, Turgeon A. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. J Emerg Trauma Shock. 2009;2:73–79. doi: 10.4103/0974-2700.44774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw JJ, Psoinos CM, Santry HP. It’s All About Location, Location, Location: A New Perspective on Trauma Transport. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Ten most-common AMPT score patterns among patients triaged to HEMS (N=24,328)
Treatment effect estimates for association between actual transport mode (HEMS versus GEMS) and survival when excluding patients in prehospital cardiac arrest.
Supplemental methods.