Abstract
Objectives
Whether racial/ethnic differences in prevalence/reporting of sleep disorders exist in pregnant women/women of child-bearing age is unknown. Study objectives were to estimate prevalence of sleep disorders and to examine racial/ethnic differences in sleep disorders, reporting of sleep issues, and amount of sleep among women of child-bearing age (15–44 years) in the US.
Methods
Through a secondary analysis of the National Health and Nutrition Examination Survey 2005–2010 (3175 non-pregnant, 432 pregnant women in main analysis), prevalence of sleep disorders, reporting of sleep disorders to a physician/health professional, and amount of sleep were estimated overall, by pregnancy status, and by race/ethnicity stratified by pregnancy status. Racial/ethnic differences in reporting of trouble sleeping by pregnancy status were examined using univariate and multivariate logistic regression.
Results
Prevalence of diagnosed sleep disorders among women of childbearing age was 4.9% (3.9% pregnant; 5.1% non-pregnant [p<0.01]). Significantly fewer pregnant and non-pregnant minority women reported adequate sleep (7–8 hours) than non-Hispanic white (white) women (p<0.05). Among non-pregnant women, odds of report of trouble sleeping were significantly higher for white compared to black (aOR 0.47 [95% CI 0.36, 0.61]) or Mexican-American women (aOR 0.29 [95% CI 0.21, 0.41]); non-pregnant minority women were also significantly less likely to report trouble sleeping than white women when controlling for amount of sleep. Among pregnant women, these same trends were found.
Discussion
Compared to white women, minority women, despite reporting less adequate sleep, are less likely to report trouble sleeping, providing evidence of an important health disparity.
Keywords: Pregnancy, sleep disorders, National Health and Nutrition Examination Survey (NHANES), health disparities
Introduction
An estimated 50–70 million Americans have chronic sleep or wakefulness disorders (Altevogt & Colten, 2006) and approximately 10% of the general population suffers from a sleep disorder of clinical or public health significance (Partinen & Hublin, 2005); 35.3% of adults report not getting enough sleep (less than seven hours of sleep in 24 hours; Centers for Disease Control and Prevention [CDC], 2011). In a nationally-based sample, estimated prevalence of diagnosed sleep disorders was 7.1%, though the true prevalence is likely higher due to under-diagnosis (Ram, Seirawan, Kumar, & Clark, 2010). Compared to men, women have a higher risk of some sleep issues, including poorer sleep quality and insomnia (Baker, Wolfson, & Lee, 2009), which has important implications due to the association between sleep disorders and adverse pregnancy outcomes, including preeclampsia/pregnancy-induced hypertension, gestational diabetes mellitus, preterm birth, Cesarean section, neonatal intensive-care admission, and post-partum depression (August et al., 2013; Louis et al., 2012; Ursavas & Karadag, 2009; Bourjeily, Ankner, & Mohsenin, 2011).
Further, important racial/ethnic differences have been found, with minorities having poorer sleep quality. A meta-analysis examining the relationship between objective or subjective sleep and ethnicity among adult normal sleepers found that non-Hispanic blacks (hereafter, blacks) had significantly less objective and subjective sleep time, lower sleep efficiency, higher sleep onset latency, higher proportion of Stage 2 sleep, and lower proportion of slow wave sleep compared to non-Hispanic whites (hereafter, whites; p<0.001; Ruiter, Decoster, Jacobs, & Lichstein, 2011). A second meta-analysis focusing on racial/ethnic differences in sleep disordered breathing (SDB) and insomnia found that blacks are both more likely to have and to suffer more severe SDB, though whites experience more symptoms of insomnia (Ruiter, DeCoster, Jacobs, & Lichstein, 2010). However, comparisons of diagnosed sleep disorders by race/ethnicity are complicated by the decreased likelihood among minorities of reporting their sleep issues to a healthcare professional (National Sleep Foundation [NSF], 2010; Grandner et al., 2013), indicating a health disparity in terms of access to quality healthcare and proper diagnosis (Ruiter et al., 2010; Jean-Louis et al., 2007).
Important racial/ethnic disparities also exist in adverse maternal and fetal outcomes (e.g., preeclampsia, gestational diabetes mellitus, low birth weight [LBW], preterm birth, and placental ischemia [Harville, Madkour, & Xie, 2012; Gould, Madan, Qin, & Chavez, 2003; Madkour, Harville, & Xie, 2014; Feinsilver & Hertz, 1992]). Black women have twice the risk of these adverse maternal and neonatal outcomes compared to white women, even after controlling for socio-economic status (SES) and access to care (Gould et al., 2003). Conversely, despite having SES similar to that of blacks, Mexican-American (hereafter, Mexican) women are at decreased risk of LBW compared to blacks, with rates of adverse pregnancy outcomes similar to whites, a phenomenon known as the “Mexican (epidemiological) paradox” (Cervantes, Keith, & Wyshak, 1999; Fuentes-Afflick & Lurie, 1997).
Because sleep disorders are associated with increased risk of adverse pregnancy outcomes, and if sleep disorders contribute to racial/ethnic differences in adverse birth outcomes, one may expect that black women have a higher prevalence of sleep disorders and get less sleep than white and Mexican women. However, the prevalence of sleep disorders or of adequacy of sleep in pregnancy or childbearing-aged women has not been determined. Further, it is unclear if racial/ethnic disparities in sleep disorders or in reporting of sleep issues to a physician exist among pregnant and non-pregnant childbearing-aged women. Therefore, the purpose of this study is to estimate prevalence of sleep disorders among women of childbearing age, to estimate prevalence of diagnosed sleep disorders, reporting of trouble sleeping, and amount of sleep by race/ethnicity, and to examine whether there are racial/ethnic differences in reporting of trouble sleeping in both pregnant and non-pregnant women of child-bearing age in the US.
Methods
This study is a secondary analysis of National Health and Nutrition Examination Survey (NHANES) data collected from 2005–2010 by the National Center for Health Statistics (NCHS). NHANES is a nationally representative cross-sectional survey of the U.S. civilian, non-institutionalized population of all ages and consists of in-depth interviews and physical examinations. This analysis was restricted to women of childbearing age (15–44 years). NHANES methodology, questionnaires, and data are available elsewhere (CDC NCHS, 2015). All NHANES participants provided informed consent. The NHANES protocol was approved by the NCHS Ethical Review Board.
Study Variables
Sleep disorder data for NHANES cycles 2005–6, 2007–8, 2009–10 is available for three sleep outcomes: diagnosed sleep disorders, report of trouble sleeping to a physician, and amount of sleep. Diagnosis of a sleep disorder was derived from the question: “{Have you/Has Sample Person [SP]} ever been told by a doctor or other health professional that {you have/s/he has} a sleep disorder?” In cycles 2005–8, Participants responding yes were then asked “What was the sleep disorder?”, with response options sleep apnea, insomnia, restless legs, and other. Report of trouble sleeping was derived from the question: “{Have you/Has SP} ever told a doctor or other health professional that {you have/s/he has} trouble sleeping?” Self-reported amount of sleep per night (derived from the question: “How much sleep {do you/does SP} usually get at night on weekdays or workdays?”) was categorized as very short (≤5 hours), short (6 hours), adequate (7– 8 hours), or excess (≥9 hours) sleep. Due to potential health disparities related to report of trouble sleeping to a physician, this variable was chosen as the main outcome variable.
In the main analysis, the exposure variable, race/ethnicity, was self-reported (black, white, and Mexican). With exception of overall prevalence estimation, analyses were stratified by pregnancy status (derived from the question: “Are you now pregnant?”). Covariates included age at interview (<20, 20–35, >35), SES (based on poverty income ratio; low income [≤1.85], middle income [>1.85–3.5], high income [>3.5]), body mass index (BMI) category (underweight [<18.5], normal [18.5 - <25], overweight [25 - <30], obese [≥30]), smoking status (current use: yes/no), depression (score ≥10 on Patient Health Questionnaire), education level (<12 years, ≥12 years), marital status (living with partner: yes/no), gravidity (0, 1, ≥2), alcohol use (more than 12 drinks in last year: yes/no), and number of times received healthcare in past year (0–1, 2–3, 4–9, ≥10).
Statistical analysis
Overall prevalence and prevalence by pregnancy status of diagnosed sleep disorders (together and by disorder), report of trouble sleeping, and amount of sleep were calculated, including all women of childbearing age surveyed (regardless of race/ethnicity). Subsequently, in the main analysis examining the association between race/ethnicity and report of trouble sleeping (stratified by pregnancy status), only Mexican, white, and black women with necessary data were included. Women whose self-reported race/ethnicity was “other Hispanic” or “other race-including multi-racial” were excluded due to low sample size for these groups as well as the potentially important heterogeneity between these groups and those included (for example: other Hispanics and Mexicans were not combined; Whinnery, Jackson, Rattanaumpawan, & Grandner, 2014). Prevalence of diagnosed sleep disorders (together and by disorder), report of trouble sleeping, and amount of sleep were calculated by race/ethnicity. The main analysis, the comparison of report of trouble sleeping to a physician by race/ethnicity, was conducted using univariate and multivariate logistic regression. Odds ratios (ORs) and adjusted ORs (aORs; based on confounders chosen a priori and by amount of sleep) and their corresponding 95% confidence intervals (CIs) were calculated to compare risk of the report of trouble sleeping, with whites as the referent group.
Because of the complex NHANES design and to provide generalizable estimates, analyses incorporated sampling weights, providing unbiased standard error (SE) estimates. In all comparisons of proportions, the Rao-Scott χ2 statistic was used to evaluate statistical significance between groups. Analyses were carried out using SAS 9.3 statistical software. All statistical tests were two-tailed, with p-value ≤0.05 considered significant.
Results
Sleep characteristics overall and by pregnancy status
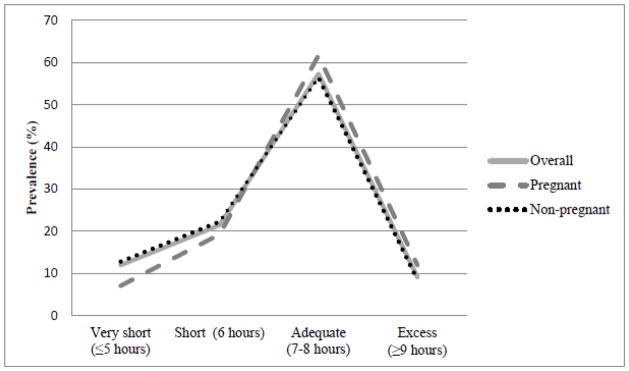
Data was available for 5236 women of all races/ethnicities, including 507 pregnant and 3875 non-pregnant women of child-bearing age. Overall, prevalence of diagnosed sleep disorders among women of childbearing age in the US was 4.9% (SE=0.4) and was higher in non-pregnant than in pregnant women (p<0.01); insomnia was the most commonly diagnosed sleep disorder (1.9%, SE=0.3), followed by sleep apnea (1.6%, SE=0.3), other sleep disorders (1.1%, SE=0.2), and restless leg syndrome (0.3, SE=0.1). The prevalence of report of trouble sleeping among women of childbearing age in the US was 21.4% (SE=0.9), and was higher among non-pregnant compared to pregnant women (p<0.01). Finally, over half of women of childbearing age in the US reported getting adequate sleep, with non-pregnant women being more likely to report either very short or short sleep while pregnant women were more likely to report excess sleep (p<0.01) [Figure 1].
Figure 1.
Adequacy of amount of sleep (hours) in women in childbearing age in the US, NHANES 2005–10 (N=5236)
*Significant Rao-Scott χ2 (p<0) for difference in adequacy of amount of sleep (hours) by pregnancy status
Demographic characteristics by race/ethnicity in pregnant and non-pregnant women of childbearing age
Among both pregnant and non-pregnant Mexican, white, or black women, many demographic characteristics were significantly different by race/ethnicity (SES, smoking status, depression, education, marital status, alcohol use, and number of doctor visits); among non-pregnant women, BMI and gravidity were also significantly different (p<0.05) [Table 1].
Table 1.
Characteristics of pregnant and non-pregnant women of childbearing age by race and ethnicity, NHANES 2005–2010 (N=3607)
| Pregnant | Non-pregnant women | |||||
|---|---|---|---|---|---|---|
| Characteristics N (%) |
Mexican- American (n=160) | Non- Hispanic White (n=190) | Non- Hispanic Black (n=82) | Mexican- American (n=833) | Non- Hispanic White (n=1499) | Non- Hispanic Black (n=843) |
| Age <20 |
17 (4.0) | 12 (4.5) | 11 (5.2) | 150 (4.9) | 131 (4.8) | 170 (5.7) |
| 20–35 | 135 (87.2) | 162 (80.5) | 66 (88.5) | 431 (61.1) | 800 (55.1) | 431 (60.5) |
| >35 | 8 (8.8) | 16 (15.0) | 5 (6.3) | 252 (34.0) | 568 (40.1) | 242 (33.9) |
| SES*a Low Income |
112 (79.1) | 48 (16.0) | 49 (64.5) | 498 (65.3) | 577 (28.4) | 432 (51.9) |
| Middle Income | 18 (15.3) | 49 (30.0) | 19 (19.2) | 145 (19.4) | 326 (25.3) | 210 (27.8) |
| High Income | 7 (5.6) | 89 (54.0) | 9 (16.3) | 109 (15.2) | 544 (46.2) | 152 (20.3) |
| BMI category**
a Underweight |
1 (1.3) | 4 (1.1) | 2 (2.0) | 19 (1.4) | 55 (3.4) | 28 (2.6) |
| Normal weight | 37 (23.0) | 55 (27.8) | 22 (26.6) | 246 (28.1) | 650 (44.5) | 223 (23.3) |
| Overweight | 55 (29.3) | 69 (37.2) | 22 (21.2) | 261 (31.5) | 342 (23.2) | 201 (25.2) |
| Obese | 67 (46.4) | 61 (33.9) | 36 (50.3) | 303 (38.9) | 441 (28.9) | 387 (48.9) |
| Current smoker* | 4 (26.1) | 30 (30.6) | 9 (60.9) | 75 (56.0) | 447 (61.7) | 153 (81.3) |
| Depression*b | 13 (9.3) | 8 (2.5) | 9 (11.2) | 61 (9.4) | 140 (8.5) | 78 (12.7) |
| Education* <12years |
88 (47.5) | 26 (13.7) | 27 (30.6) | 411 (45.1) | 269 (13.2) | 236 (20.5) |
| 12/+ | 72 (52.5) | 164 (86.3) | 55 (69.4) | 422 (55.0) | 1229 (86.8) | 607 (79.5) |
| Live with partner* | 131 (77.2) | 162 (83.5) | 41 (53.7) | 477 (63.5) | 853 (61.5) | 259 (36.0) |
| Gravidity** 0 |
209 (21.3) | 484 (35.1) | 253 (25.2) | |||
| 1 | 32 (23.3) | 58 (33.6) | 17 (21.2) | 108 (14.5) | 193 (15.7) | 87 (12.6) |
| ≥2 | 119 (76.7) | 126 (66.4) | 53 (78.8) | 405 (64.2) | 677 (49.2) | 387 (62.2) |
| Alcohol use* | 57 (50.4) | 126 (80.8) | 28 (53.7) | 336 (58.3) | 969 (80.1) | 327 (57.2) |
| Number of doctor visits* 0–1 |
44 (26.6) | 13 (5.1) | 16 (19.3) | 420 (51.0) | 454 (29.6) | 279 (33.4) |
| 2–3 | 31 (22.6) | 26 (17.2) | 16 (23.2) | 201 (23.6) | 466 (32.7) | 291 (33.2) |
| 4–9 | 52 (28.5) | 68 (29.0) | 30 (28.9) | 117 (14.4) | 331 (21.7) | 172 (20.9) |
| ≥10 | 33 (22.3) | 83 (48.8) | 20 (28.6) | 95 (11.1) | 247 (15.9) | 101 (12.5) |
Significant Rao-Scott χ2 (p<0.05) for difference between races/ethnicities in both pregnant and non-pregnant women
Significant Rao-Scott χ2 (p<0.05) for difference between races/ethnicities in only non-pregnant women
Based on poverty income ratio (low income [≤1.85], middle income[>1.85–3.5], high income [>3.5])
Based on score ≥10 on Patient Health Questionnaire
Sleep characteristics by race/ethnicity in pregnant women
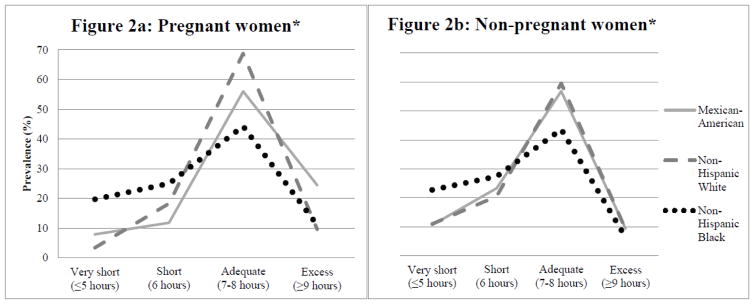
Prevalence of any diagnosed sleep disorder and report of trouble sleeping did not differ by race/ethnicity among pregnant women [Table 2]. Amount of sleep among pregnant women differed by race/ethnicity (p<0.05), with more black women reporting very short or short sleep and more Mexican women reporting excess sleep [Figure 2a].
Table 2.
Prevalence of sleep disorders and reporting of trouble sleeping to doctor in pregnant women in the US, NHANES 2005–2010 (N=507)
| Sleep characteristic % (SE) | Overall | Mexican- American | Non- Hispanic White | Non- Hispanic Black |
|---|---|---|---|---|
| Any diagnosed sleep disorder | 3.9 (1.3) | 1.4 (1.3) | 2.9 (1.9) | 8.2 (3.2) |
| Report of trouble sleeping | 13.8 (2.3) | 9.2 (3.1) | 17.6 (4.2) | 11.4 (4.3) |
Figure 2.
Adequacy of amount of sleep (hours) by race/ethnicity among women of childbearing age in the US, NHANES 2005–2010 (N=3607)
*Significant Rao-Scott χ2 (p<0) for difference in adequacy of amount of sleep (hours) by race/ethnicity
Sleep characteristics by race/ethnicity in non-pregnant women of childbearing age
Prevalence of diagnosed sleep disorders (overall and by disorder) did not differ by race/ethnicity among non-pregnant women [Table 3]. However, non-pregnant white women were more likely to have reported trouble sleeping to a physician, followed by black and lastly Mexican women (p<0.05). Comparing amount of sleep, while non-pregnant Mexican and white women report similar amounts of sleep, non-pregnant black women were more likely to report short or very short sleep compared to white women or Mexican women (p<0.05) [Figure 2b].
Table 3.
Prevalence of sleep disorders and reporting of trouble sleeping to doctor in non-pregnant women of childbearing age in the US, NHANES 2005–2010 (N=3875)
| Sleep characteristic % (SE) | Overall | Mexican- American | Non-Hispanic White | Non-Hispanic Black |
|---|---|---|---|---|
| Any diagnosed sleep disorder | 5.1 (0.4) | 3.5 (0.7) | 5.6 (0.6) | 4.7 (0.9) |
| Sleep apneaa | 1.9 (0.3) | 1.5 (0.8) | 1.9 (0.5) | 2.3 (0.6) |
| Insomniaa | 2.0 (0.4) | 0.7 (0.4) | 2.1 (0.4) | 1.3 (0.5) |
| Restless leg syndromea | 0.3 (0.1) | 0 | 0.3 (0.1) | 0.2 (0.2) |
| Othera | 1.0 (0.2) | 1.1 (0.4) | 1.2 (0.3) | 0.2 (0.2) |
| Report of trouble sleeping* | 23.2 (1.0) | 10.0 (1.2) | 27.2 (1.4) | 19.6 (1.7) |
Sig nific ant Rao-Scott χ2 (p<0.05) for difference by race/ethnicity
based on data from NHANES 2005–8
Analysis of report of trouble sleeping by race/ethnicity
In separate unadjusted logistic regression analyses, both pregnant and non-pregnant minorities were less likely to have reported trouble sleeping to a physician compared to white women, though the result was only significant among non-pregnant women. This result was not changed in analyses adjusted for both confounders chosen a priori or adjusted for amount of sleep reported, with a significant difference persisting among non-pregnant women [Table 4].
Table 4.
Association between report of trouble sleeping and race/ethnicity in pregnant and non-pregnant women of childbearing age, NHANES 2005–2010
| Pregnant Women (n=432) | Non-Pregnant Women (n=3175) | |||
|---|---|---|---|---|
| Crude Analysis | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Mexican American | 0.47 | 0.20, 1.15 | 0.30 | 0.22, 0.41 |
| Non-Hispanic White | 1.0 | 1.0 | ||
| Non-Hispanic Black | 0.60 | 0.21,1.75 | 0.65 | 0.52, 0.81 |
| Adjusted Analysisa | ||||
| Mexican American | 0.21 | 0.03, 1.50 | 0.29 | 0.21, 0.41 |
| Non-Hispanic White | 1.0 | 1.0 | ||
| Non-Hispanic Black | 0.45 | 0.09, 2.24 | 0.47 | 0.36, 0.61 |
| Adjusted Analysisb | ||||
| Mexican American | 0.49 | 0.18, 1.34 | 0.31 | 0.22, 0.42 |
| Non-Hispanic White | 1.0 | 1.0 | ||
| Non-Hispanic Black | 0.44 | 0.13, 1.55 | 0.51 | 0.40, 0.66 |
a priori adjustment for alcohol, number of doctors visits in the past year, SES, BMI, gravidity, and marital status
adjusted adequacy of sleep
Discussion
To our knowledge, this is the first study to estimate national prevalence of diagnosed sleep disorders, report of trouble sleeping, and adequacy/amount of sleep and their prevalence by pregnancy status, as well as by race/ethnicity (stratified by pregnancy status) and to examine the association between report of trouble sleeping and race/ethnicity in pregnant and non-pregnant women of childbearing age in the US. Prevalence of any diagnosed sleep disorder, reporting of trouble sleeping, and adequacy of amount of sleep all differed significantly by pregnancy status, with non-pregnant women reporting more diagnosed sleep disorders, reporting of trouble sleeping to a physician, and inadequate sleep. Additionally, minority women, regardless of pregnancy status, were less likely to have reported trouble sleeping to a physician.
This analysis builds upon previous studies examining sleep characteristics in the US adult population. Based on NHANES data from 2005–6, overall prevalence of diagnosed sleep disorders in the general adult population was 7.1% nd 6.6% in adult women (Ram et al., 2010), higher than in our sample; their estimate of prevalence by disorder varied as well, with 2.8% sleep apnea, 1.7% insomnia, 0.6% restless leg syndrome, and 1.5% other. A separate study of employed middle-aged women (30–60) found that 9% had undiagnosed SDB, again higher than our sample, though the estimated 2% prevalence of diagnosable sleep apnea is similar to our findings (Young et al., 1993). Finally, our estimate is lower than the 10% of the population believed to have a sleep or wakefulness disorder (Partinen & Hublin, 2005). However, as sleeping disorders are often undiagnosed (Ram et al., 2010), our finding of a lower prevalence is not surprising and is likely an underestimation of the true prevalence of sleep disorders in this population.
Because both adverse birth outcomes and sleep disorders may differ by race/ethnicity, and if sleep disorders contribute to these racial/ethnic differences in adverse birth outcomes, we expected that black women would have a higher prevalence of sleep disorders than whites. Our results in pregnant women, though non-significant, support this hypothesis. However, in non-pregnant women, white women had the highest prevalence of sleep disorders. These discrepancies are likely due to health disparities related to differences in report of trouble sleeping and under-diagnosis in minorities, as discussed more in-depth below.
Our finding that pregnant women were more likely to get adequate sleep than non-pregnant was surprising, as pregnant women are hypothesized to experience more sleep disturbance due to physical changes to the body, general discomfort, and changing hormone levels (Bourjeily et al., 2011; Ursavas & Karadag, 2009; Venkata & Venkateshiah, 2009). However, research has shown that self-reported number of hours slept per night may be a poor predictor of actual sleep time, particularly in pregnant women (Herring et al., 2013) and some pregnancy conditions, such as sleeping in the lateral position in the third trimester and decreased rapid eye movement sleep, are protective against sleep disorders (Bourjeily et al., 2011).
Our findings that minority women were less likely to get adequate amounts of sleep than white women are in line with previous findings in distinct populations (CDC, 2011; Ram et al., 2010; Lauderdale et al., 2006; Jean-Louis, Kripke, Ancoli-Israel, Klauber, & Sepulveda, 2000; Chen et al., 2015; Ruiter et al., 2011; Whinnery et al., 2014). For example, a study of self-reported amount of sleep in older women found that 27.6% of white women compared to 16.7% of black women got 7–8 hours of sleep, though far fewer women in this sample reported adequate sleep. Further, in their sample, black women were more likely to report getting excess amounts of sleep, in contrast to our finding that blacks got less sleep than white women (Grandner et al., 2013). A separate study of all adults participating in NHANES 2007–8 found that blacks were more likely to report sleeping <5 hours (aOR 2.34, P < 0.001) and 5–6 hours (aOR 1.85, P < 0.001); however, in contrast to our results, Mexicans were less likely to report excess sleep (aOR 0.36, P = 0.032) (Whinnery et al., 2014). Finally, a study using Behavioral Risk Factor Surveillance System data found that almost half of blacks sleep <7 hours, compared to 34.9% of whites and 33.0% of Hispanics (CDC, 2011); these results were similar to our findings, with the exception of in pregnant white and Mexican women, where we found fewer women reporting sleeping <7 hours. The discrepancies between studies are likely due to differences in the populations studied (by age and sex), but could also be influenced by differences in how race/ethnicity was categorized for groups other than black and white women and differences in how amount of sleep was categorized.
Finally, we found that minority women were less likely to report trouble sleeping to a physician than were white women, in agreement with a number of previous studies. For example, the NSF found that 38% of whites, 26% of blacks, 14% of Asians, and 30% of Hispanics had discussed sleep issues with a healthcare professional, while 61% of whites, 40% of blacks, 30% of Asians, and 55% of Hispanic women had been asked about or discussed sleep issues with a healthcare professional (NSF, 2010). However, these proportions are much higher than those found in our sample. Additionally, in a study of older women, 24.1% of white versus 13.9% of black women either agreed or strongly agreed that they had “Seen or talked about sleep problems with [her] doctor (Grandner et al., 2013), proportions more in line with our findings.
Comparing the proportion of women not getting adequate sleep to the number of women discussing trouble sleeping with a physician and diagnosed with a sleeping disorder, our results support previous findings that sleep issues often occur in the absence of reporting (Ohayon, Caulet, & Guilleminault, 1997; Grandner, Petrov et al., 2013) and diagnosis (Ram et al., 2010). Further, given minority women were more likely to get inadequate sleep yet are less likely to report trouble sleeping to a healthcare provider, important differences in reporting and potential health disparities may exist. This finding supports previous research showing that blacks may not report their symptoms outright due to differential prioritization of sleep (Grandner, Petrov et al., 2013) or social desirability (Adenekan et al., 2013; Jean-Louis et al., 2007; Grandner et al., 2013). Other theories explaining differences in the reporting of health problems to healthcare professionals between race/ethnic groups include repressive coping (Jean-Louis et al., 2007), reporting bias, differential experience of sleep in terms of perception of amount of sleep needed (NSF, 2010; Grandner et al., 2013), societal structure (Patel, Grandner, Xie, Branas, & Gooneratne, 2010), perceived racial discrimination when seeking healthcare (Grandner et al., 2012), and cultural attitudes/behavior regarding healthcare (Boss, Smith, & Ishman, 2011).
The present study had several limitations. First, small sample size, particularly in the pregnant cohort, resulted in small cell sizes for several analyses (limiting power) and prevented the estimate of the prevalence of individual sleep disorders (not available for NHANES 2009–10) by race/ethnicity in this group. Reporting bias may exist since data was self-reported, and there may have been some misclassification of pregnancy status, as some women very early in their pregnancies may have not realized that they were pregnant. Further, because sleep disorders are underdiagnosed, reported rates do not reflect the true rates of sleep disorders in this population, but rather the prevalence of diagnosed sleep disorders (a much lower prevalence). Additionally, because NHANES data is cross-sectional, causality and temporality of when a sleep disorder was diagnosed or when report of trouble sleeping to a doctor was made is unclear. Finally, comparisons across studies are difficult due to the variety of ways in which sleep/sleep disorders/trouble sleeping are assessed and in how race/ethnicity is categorized/which races/ethnicities are included, particularly for races/ethnicities other than white and black.
The study also had a number of strengths. Foremost, the study population was a representative sample of women of child-bearing age and thus can be generalized to the US. The large sample of women in the non-pregnant group provided sufficient power for analysis and a large number of variables, collected in a standardized and validated manner, were available. Finally, report of trouble sleeping to a doctor as outcome of interest is useful because of its public health significance--only sleep complaints reported will lead to correct diagnosis and treatment.
In summary, sleep disorders are under-diagnosed in pregnant women and women of child-bearing age. Further, minorities, despite getting less adequate sleep, were less likely to have reported trouble sleeping to a doctor than were white women, pointing to potential health disparities. Due to the reported association between sleep disorders and adverse maternal and neonatal outcomes, these findings highlight the importance of discussing sleep issues with pregnant women and women of child-bearing age in a culturally appropriate manner during routine healthcare visits in order to provide proper diagnosis and treatment/intervention, if necessary. Future studies should include a larger sample of pregnant women for sufficient power for more in-depth analysis and should include specific questions to determine why this difference exists, as well as to further examine possible differences in patterns of sleep disorders by race/ethnicity in women of childbearing age. Additionally, future studies should account for timing of diagnosis in relation to pregnancy status.
Significance.
What is already known on this subject?
The relationship between diagnosis of sleep disorders and race/ethnicity is complex, as race/ethnicity is an important predictor of sleep (minorities having poorer sleep) and of likelihood of reporting sleep issues to a healthcare professional (minorities may be less likely to report). However, the relationship has not been fully evaluated among pregnant women/women of child-bearing age.
What this study adds?
Regardless of pregnancy status and despite less adequate amounts of sleep reported by minorities, likelihood of report of trouble sleeping was highest among white women, although the result was only significant among non-pregnant women.
Acknowledgments
The study was supported by the National Institutes of Health Training in Global Reproductive Epidemiology grant (5T32HD057780) and by the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Heart, Blood, and Lung Institute, and the National Institutes of Health Office of Research for Women’s Health through the Fogarty Global Health Fellows Program Consortium comprised of the University of North Carolina, John Hopkins, Morehouse and Tulane (R25TW009340).
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: Role of racial/ethnic differences. Sleep Medicine Reviews. 2013;17(4):255–262. doi: 10.1016/j.smrv.2012.07.002. http://dx.doi.org/10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altevogt BM, Colten HR. Sleep disorders and sleep deprivation: An unmet public health problem. National Academies Press; 2006. [PubMed] [Google Scholar]
- August EM, Salihu HM, Biroscak BJ, Rahman S, Bruder K, Whiteman VE. Systematic review on sleep disorders and obstetric outcomes: Scope of current knowledge. American Journal of Perinatology. 2013;30(4):323–334. doi: 10.1055/s-0032-1324703. [DOI] [PubMed] [Google Scholar]
- Baker FC, Wolfson AR, Lee KA. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: Findings from the 2007 National Sleep Foundation "Sleep in America Poll". Journal of Women's Health (2002) 2009;18(6):841–849. doi: 10.1089/jwh.2008.0986. [DOI] [PubMed] [Google Scholar]
- Boss EF, Smith DF, Ishman SL. Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. International Journal of Pediatric Otorhinolaryngology. 2011;75(3):299–307. doi: 10.1016/j.ijporl.2010.11.006. [DOI] [PubMed] [Google Scholar]
- Bourjeily G, Ankner G, Mohsenin V. Sleep-disordered breathing in pregnancy. Clinics in Chest Medicine. 2011;32(1):175–189. doi: 10.1016/j.ccm.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey. 2005–10 data file and protocols Retrieved from www.cdc.gov/nchs/nhanes.htm.
- Centers for Disease Control and Prevention CDC. Unhealthy sleep-related behaviors--12 states, 2009. Morbidity and Mortality Weekly Report. 2011;60(8):233–238. mm6008a2 [pii] [PubMed] [Google Scholar]
- Cervantes A, Keith L, Wyshak G. Adverse birth outcomes among native-born and immigrant women: Replicating national evidence regarding Mexicans at the local level. Maternal and Child Health Journal. 1999;3(2):99–109. doi: 10.1023/a:1021805427469. [DOI] [PubMed] [Google Scholar]
- Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcantara C, Redline S. Racial/Ethnic differences in sleep disturbances: The multi-ethnic study of atherosclerosis (MESA) Sleep. 2015;38(6):877–888. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinsilver SH, Hertz G. Respiration during sleep in pregnancy. Clinics in Chest Medicine. 1992;13(4):637–644. [PubMed] [Google Scholar]
- Fuentes-Afflick E, Lurie P. Low birth weight and Latino ethnicity: Examining the epidemiologic paradox. Archives of Pediatrics & Adolescent Medicine. 1997;151(7):665–674. doi: 10.1001/archpedi.1997.02170440027005. [DOI] [PubMed] [Google Scholar]
- Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: A dual epidemiologic paradox. Pediatrics. 2003;111(6 Pt 1):e676–82. doi: 10.1542/peds.111.6.e676. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behavioral Sleep Medicine. 2012;10(4):235–249. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Jean-Louis G, Jackson N, Gehrman PR, Perlis ML, Gooneratne NS. Sleep-related behaviors and beliefs associated with race/ethnicity in women. Journal of the National Medical Association. 2013;105(1):4–15. doi: 10.1016/s0027-9684(15)30080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. 2013;9(9):897–905. 905A–905D. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harville EW, Madkour AS, Xie Y. Predictors of birth weight and gestational age among adolescents. American Journal of Epidemiology. 2012;176(Suppl 7):S150–63. doi: 10.1093/aje/kws231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herring SJ, Foster GD, Pien GW, Massa K, Nelson DB, Gehrman PR, Davey A. Do pregnant women accurately report sleep time? A comparison between self-reported and objective measures of sleep duration in pregnancy among a sample of urban mothers. Sleep & Breathing. 2013;17(4):1323–1327. doi: 10.1007/s11325-013-0835-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, Magai C, Consedine NS, Pierre-Louis J, Zizi F, Casimir GJ, Belzie L. Insomnia symptoms and repressive coping in a sample of older black and white women. BMC Women's Health. 2007;7:1. doi: 10.1186/1472-6874-7-1. 1472-6874-7-1 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, Kripke DF, Ancoli-Israel S, Klauber MR, Sepulveda RS. Sleep duration, illumination, and activity patterns in a population sample: Effects of gender and ethnicity. Biological Psychiatry. 2000;47(10):921–927. doi: 10.1016/S0006-3223(99)00169-9. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, Liu K. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. American Journal of Epidemiology. 2006;164(1):5–16. doi: 10.1093/aje/kwj199. kwj199 [pii] [DOI] [PubMed] [Google Scholar]
- Louis J, Auckley D, Miladinovic B, Shepherd A, Mencin P, Kumar D, … Redline S. Perinatal outcomes associated with obstructive sleep apnea in obese pregnant women. Obstetrics and Gynecology. 2012;120(5):1085–1092. doi: 10.1097/AOG.0b013e31826eb9d8. http://10.1097/AOG.0b013e31826eb9d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madkour AS, Harville EW, Xie Y. Neighborhood disadvantage, racial concentration and the birthweight of infants born to adolescent mothers. Maternal and Child Health Journal. 2014;18(3):663–671. doi: 10.1007/s10995-013-1291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation. 2010 Sleep in America Poll: Summary of findings. 2010 PDF Document Retrieved from http://sleepfoundation.org/sites/default/files/nsaw/NSF%20Sleep%20in%20%20America%20Poll%20-%20Summary%20of%20Findings%20.pdf.
- Ohayon MM, Caulet M, Guilleminault C. How a general population perceives its sleep and how this relates to the complaint of insomnia. Sleep. 1997;20(9):715–723. doi: 10.1093/sleep/20.9.715. [DOI] [PubMed] [Google Scholar]
- Partinen M, Hublin C. Epidemiology of Sleep Disorders. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4. Philadelphia: W. B. Saunders Company; 2005. pp. 626–647. [Google Scholar]
- Patel N, Grandner M, Xie D, Branas C, Gooneratne N. "Sleep disparity" in the population: Poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10(1):475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep and Breathing. 2010;14(1):63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Sleep disorders in African Americans and Caucasian Americans: A meta-analysis. Behavioral Sleep Medicine. 2010;8(4):246–259. doi: 10.1080/15402002.2010.509251. [DOI] [PubMed] [Google Scholar]
- Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: A meta-analysis. Sleep Medicine. 2011;12(3):209–214. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- Ursavas A, Karadag M. Sleep breathing disorders in pregnancy. Tuberkuloz Ve Toraks. 2009;57(2):237–243. [PubMed] [Google Scholar]
- Venkata C, Venkateshiah SB. Sleep-disordered breathing during pregnancy. Journal of the American Board of Family Medicine. 2009;22(2):158–168. doi: 10.3122/jabfm.2009.02.080057. [DOI] [PubMed] [Google Scholar]
- Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. The New England Journal of Medicine. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]