Abstract
OBJECTIVE
Many individuals with prediabetes have evidence of subclinical myocardial damage and are at an increased risk of cardiovascular disease (CVD). If subclinical myocardial damage is independently associated with incident diabetes, this may contribute to the understanding of the association between diabetes and CVD. This study was conducted to determine whether high-sensitivity cardiac troponin T (hs-cTnT) is associated with incident diabetes.
RESEARCH DESIGN AND METHODS
Using Kaplan-Meier curves and Cox models, we prospectively analyzed 8,153 participants without known diabetes or CVD. We used the Harrell C statistic to investigate whether hs-cTnT added incremental prognostic information for diabetes prediction.
RESULTS
During a median of 13 years of follow-up, there were 1,830 incident cases of diagnosed diabetes. After adjustment for demographics and traditional risk factors, participants with a baseline hs-cTnT of 9–13 ng/L or ≥14 ng/L had a significantly increased risk for diabetes compared to those with an hs-cTnT of ≤5 ng/L, with hazard ratios of 1.14 (95% CI 0.99–1.33) and 1.25 (95% CI 1.03–1.53), respectively (P = 0.018 for trend). Linear spline modeling that included adjustment for baseline fasting glucose suggested an increased risk of incident diabetes for participants with hs-cTnT levels >8 ng/L. Furthermore, the addition of hs-cTnT to fully adjusted models that included glucose significantly improved the prediction of incident diabetes from 0.7636 to 0.7644 (P = 0.023).
CONCLUSIONS
Participants with elevated hs-cTnT levels at baseline had an increased risk of incident diabetes, suggesting that the measurement of hs-cTnT may incorporate an underlying pathophysiologic overlap between diabetes and CVD not captured by other traditional risk factors. Measurement of hs-cTnT may be useful to identify individuals at an increased risk for incident diabetes and CVD in order to provide early and more intensive risk factor modification.
Introduction
The incidence of diabetes has significantly increased during the last three decades, and in 2010, there were an estimated 21 million people with diagnosed diabetes in the U.S. (1,2). People with prediabetes and diabetes have a substantially elevated risk for cardiovascular disease (CVD), and approximately half of individuals aged older than 65 years with diabetes have experienced a CVD event (3,4). Prediabetes is a precursor of diabetes, and blood glucose—whether measured by fasting glucose, glycated hemoglobin, or 2-h postprandial glucose—is one of the most important predictors of subsequent diabetes (4,5). However, only ∼2% of individuals with prediabetes progress to diabetes per year, and exposure to hyperglycemia via its damage to the vasculature may contribute to subclinical myocardial damage along with the damaging effects of traditional CVD risk factors (6,7).
As a result of the strong association between diabetes and CVD, the 2013 atherosclerotic cardiovascular disease (ASCVD) lipid treatment guidelines identify patients with diabetes as one of the four groups to benefit from statin treatment (8). High-sensitivity cardiac troponin T (hs-cTnT) is a marker of subclinical myocardial damage that has been proposed for use in the risk stratification of asymptomatic individuals (9–11). People with diabetes have significantly higher hs-cTnT values than those without diabetes, although an increased risk of incident CVD is observed in individuals with and without diabetes with elevated hs-cTnT (12).
hs-cTnT may incorporate an important overlap between diabetes and CVD because the subclinical cardiac microvascular damage reflected by an elevated hs-cTnT may be at least partially secondary to hyperglycemia, even in the prediabetic range, along with other CVD risk factors (13). A better understanding of which individuals are most likely to progress to overt diabetes may highlight possible pathophysiologic mechanisms for future treatment strategies and help to focus resources on those at highest risk. Therefore, in this analysis, we examined the relationship between hs-cTnT and incident diagnosed diabetes to determine whether the measurement of hs-cTnT may identify individuals who are at high risk for both diagnosed diabetes and the major cardiovascular complications associated with it.
Research Design and Methods
Study Populations
We included Atherosclerosis Risk in Communities (ARIC) study participants who had hs-cTnT measured at the fourth ARIC examination (Visit 4), which took place from 1996 to 1998 (baseline for this analysis). The ARIC study design has been described in detail previously (14). Participants were excluded if they had a history of self-reported diabetes or diabetes medication use (n = 1,365); had a history of coronary heart disease, stroke, or heart failure (n = 1,122); were missing data on incidence of diabetes (n = 135); had fasted for <8 h before the laboratory draw (n = 233); did not have available hs-cTnT values (n = 195); were missing other important covariates (n = 158); or were nonblack or nonwhite (n = 24). A total of 8,153 participants met the inclusion criteria, and follow-up was assessed through April 2012.
Data Collection
Standardized questionnaires were used to collect demographic information and other patient-reported data. Height, weight, and blood pressure were measured using standardized protocols during the ARIC Visit 4 examination. Hypertension was defined as a systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or use of a blood pressure–lowering medication. Hypercholesterolemia was defined as patient-reported hypercholesterolemia. Smoking was categorized into never, former, and current groups. Alcohol consumption was categorized into current and not current. Metabolic syndrome was defined as the presence of three or more of the following risk factors: 1) waist circumference ≥40 inches for men or ≥35 inches for women, 2) fasting triglycerides ≥150 mg/dL, 3) HDL cholesterol (HDL-C) <40 mg/dL for men or <50 mg/dL for women, 4) blood pressure ≥130/85 mmHg or treatment for hypertension, and 5) fasting glucose ≥100 mg/dL. Fasting plasma glucose, plasma total cholesterol, LDL cholesterol (LDL-C), triglycerides, and HDL-C were measured in a centralized laboratory.
Measurement of hs-cTnT
hs-cTnT was measured in plasma samples, which were centrally stored at −80°C, using a novel precommercial highly sensitive assay (Elecsys Troponin T; Roche Diagnostics, Indianapolis, IN) that can detect troponin levels as low as 3 ng/L. The hs-cTnT assay had a reliability coefficient (R) of 0.98, based on 418 blinded replicate samples and a between-assay coefficient of variation of 6.9% for control samples that had a mean hs-cTnT concentration of 29 ng/L (15). Participants with subclinical myocardial damage were categorized as those with detectable hs-cTnT (≥5 ng/L) at baseline.
Incident Diabetes
Incident cases of diagnosed diabetes were identified during annual follow-up telephone calls to all participants and defined by participant self-report of diagnosed diabetes or new use of a diabetes medication with follow-up until April 2012. Although the participants were not specifically asked whether they were diagnosed with type 1 or type 2 diabetes, all cases were presumed to be type 2 diabetes based on patient demographics.
Statistical Analyses
We used Cox proportional hazards models and the Kaplan-Meier survival analysis method to examine the association between baseline hs-cTnT and risk of incident diagnosed diabetes after adjustment for traditional risk factors. We selected these risk factors because of their strong and well-established relationship with diabetes in the literature. In our Cox models, the proportional hazards assumption was not violated based on Schoenfeld residual testing (16). Model 1 was adjusted for age, race-center, and sex. Model 2 was additionally adjusted for total cholesterol, LDL-C, HDL-C, triglycerides, cholesterol-lowering medication use, BMI, systolic blood pressure, blood pressure–lowering medication use, smoking status, and estimated glomerular filtration rate (eGFR). Model 3 was adjusted for the variables in model 2 plus fasting glucose.
In the Cox proportional hazards models, baseline hs-cTnT was categorized into four groups using cut points consistent with previously reported analyses: ≤5 ng/L, 6–8 ng/L, 9–13 ng/L, and ≥14 ng/L (10,15). Individuals with hs-cTnT values ≤5 ng/L, where there is reduced precision in measurement, were categorized as the lowest group, and individuals with values ≥14 ng/L, which is approximately the 90th percentile of the ARIC cohort and the 99th percentile specified by the manufacturer, were categorized as the highest group. The cut points of 6–8 ng/L and 9–13 mg/L were used for the remaining two middle groups. To further examine the additional information provided by hs-cTnT beyond traditional risk factors (age, race-center, sex, total cholesterol, HDL-C, LDL-C, triglycerides, BMI, eGFR, systolic blood pressure, blood pressure–lowering medication use, smoking status, cholesterol-lowering medication use, family history of coronary heart disease, waist circumference, physical activity, education level, and annual family income level), we used the Harrell C statistic from Cox proportional hazards models and full follow-up data in progressively adjusted models to examine the additive predictive value of hs-cTnT. We also calculated the continuous net reclassification index (NRI) based on the proportion of subjects with movement in the correct direction upward or downward, averaged for event and nonevent subjects (17).
We defined a group at low risk for incident diagnosed diabetes as those without hypertension, hypercholesterolemia, or metabolic syndrome. Participants with undiagnosed diabetes were defined as those without self-reported diabetes but with a fasting blood glucose of ≥126 mg/dL at baseline. We examined associations in subjects with and without undiagnosed diabetes to understand whether the magnitude of the association was similar in these subgroups. This is particularly important, because those individuals with elevated baseline glucose (undiagnosed diabetes) would be more likely to be diagnosed with diabetes during early follow-up compared with people without hyperglycemia at baseline.
In addition, to assess a nonlinear association between hs-cTnT and the incidence of diagnosed diabetes, we used two adjusted Cox models with linear splines: one with a single knot at the mean value of 6 ng/L and one with three knots, at 5, 8, and 14 ng/L, which are the values used to define the hs-cTnT groups in this analysis. Participants with an hs-cTnT ≤5 ng/L were used as the comparison group, and individuals with an hs-cTnT <3 ng/L were assigned a value of 1.5 ng/L, which is halfway between zero and the lower limit of detection (18). In these analyses, we truncated hs-cTnT values >99th percentile (25 ng/L).
We evaluated heterogeneity in the association between hs-cTnT and incidence of diagnosed diabetes across prespecified subgroups: 1) participants with or without traditional risk factors and 2) participants with an overall low risk of incident diabetes, defined as those without hypertension, hypercholesterolemia, or metabolic syndrome. To examine whether reverse causation influenced our results, we performed a sensitivity analysis censoring the first 2 years and first 5 years of follow-up.
Results
Overall, the mean age of participants was 62.5 years (SD 5.6; range 53–75), and 58.9% were female. Participants with higher levels of hs-cTnT were more likely to be male, older, with a higher fasting glucose, BMI, prevalence of hypertension, prevalence of metabolic syndrome, and prevalence of impaired fasting glucose compared with participants with a lower hs-cTnT (Table 1). In addition, they were more likely to have lower HDL-C, eGFR, and LDL-C and more likely to be treated with statin therapy.
Table 1.
Characteristics of participants stratified by hs-cTnT group
| Overall | ≤5 ng/L | 6–8 ng/L | 9–13 ng/L | ≥14 ng/L | ||
|---|---|---|---|---|---|---|
| n = 8,153 | n = 5,101 | n = 1,641 | n = 971 | n = 440 | P trend | |
| hs-cTnT (ng/L)* | 4.0 (1.5–7.0) | 1.5 (1.5–4) | 7.0 (6.0–8.0) | 10.0 (9.0–11.0) | 18.0 (15.0–22.0) | |
| Female | 58.9 | 71.4 | 44.8 | 33.2 | 23.0 | <0.001 |
| Black | 19.2 | 18.5 | 19.6 | 20.4 | 22.5 | 0.019 |
| Age (years) | 62.5 (5.6) | 61.3 (5.3) | 63.6 (5.6) | 65.1 (5.5) | 65.3 (5.6) | <0.001 |
| Current drinker | 34.7 | 34.5 | 35.0 | 36.4 | 33.2 | 0.610 |
| Blood pressure (mmHg) | ||||||
| Systolic | 126.2 (18.4) | 124.5 (17.8) | 127.3 (18.2) | 130.9 (19.8) | 131.4 (19.8) | <0.001 |
| Diastolic | 71.2 (10.0) | 70.8 (9.8) | 71.6 (9.9) | 72.2 (10.7) | 72.3 (11.3) | <0.001 |
| Hypertension medication | 45.1 | 40.2 | 48.4 | 55.7 | 64.5 | <0.001 |
| Cholesterol (mg/dL) | ||||||
| Total | 202.3 (35.7) | 204.8 (35.2) | 199.4 (35.9) | 197.8 (36.4) | 193.7 (36.1) | <0001 |
| LDL-C | 123.9 (33.1) | 124.6 (33.3) | 123.4 (32.5) | 123.3 (33.4) | 120.1 (32.3) | 0.008 |
| HDL-C | 50.3 (15.5) | 54.1 (15.5) | 50.3 (15.5) | 46.4 (15.5) | 46.4 (15.5) | <0.001 |
| Triglycerides (mg/dL) | 133.2 (64.9) | 133.4 (64.2) | 131.7 (65.7) | 134.1 (64.6) | 135.1 (69.2) | 0.846 |
| Hypercholesterolemia | 10.3 | 10.2 | 9.9 | 11.7 | 9.8 | 0.590 |
| Statin use | 7.9 | 7.9 | 7.3 | 8.8 | 8.6 | 0.414 |
| Fasting glucose (mg/dL) | 101.7 (19.1) | 100.3 (17.5) | 103.2 (20.9) | 104.1 (20.3) | 106.5 (24.4) | <0.001 |
| Impaired fasting glucose | 40.5 | 36.9 | 44.9 | 49.6 | 45.2 | <0.001 |
| Undiagnosed diabetes | 5.0 | 4.0 | 5.6 | 6.1 | 11.6 | <0.001 |
| Family history diabetes | 24.0 | 23.6 | 24.3 | 26.4 | 23.4 | 0.236 |
| Metabolic syndrome | 40.8 | 38.2 | 42.7 | 47.5 | 48.9 | <0.001 |
| BMI (kg/m2) | 28.3 (5.3) | 27.9 (5.3) | 28.7 (5.5) | 29.0 (5.3) | 29.4 (5.3) | <0.001 |
| eGFR (mL/min/1.73 m2) | 86.7 (14.8) | 88.6 (14.0) | 85.0 (14.7) | 82.6 (15.2) | 79.7 (18.4) | <0.001 |
Continuous variables are presented as mean (SD); categorical variables are presented as percent.
*Median and interquartile range (25th percentile, 75th percentile).
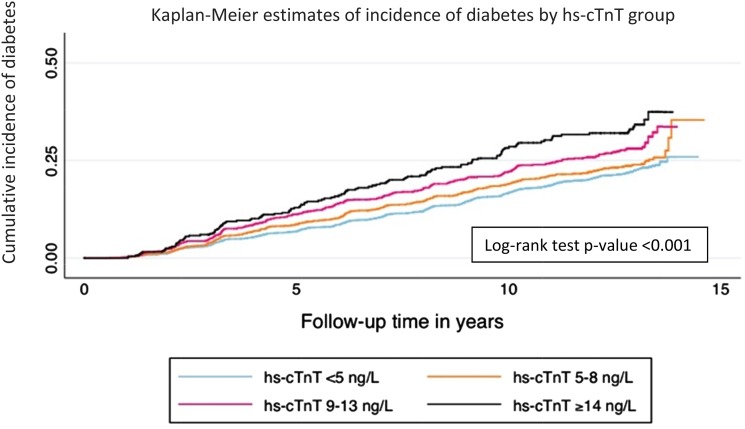
At baseline, 40.5% of participants had impaired fasting glucose, and 5.0% had undiagnosed diabetes. Over a median follow-up of 13 years, 1,830 participants developed diagnosed diabetes. Unadjusted Kaplan-Meier curves showed a higher risk of incident diagnosed diabetes with increasing hs-cTnT categories and a consistent separation in risk among hs-cTnT groups over time (P < 0.001) (Fig. 1). In multivariable adjusted Cox models, participants in the highest hs-cTnT groups were more likely to report a subsequent diagnosis of diabetes than those with hs-cTnT ≤5 ng/L, with a hazard ratio (HR) of 1.14 (95% CI 0.99–1.33) for the hs-cTnT 9–13 ng/L group and an HR of 1.25 (95% CI 1.03–1.53) for the hs-cTnT group ≥14 ng/L (P = 0.018 for trend) (Table 2). After further adjustment for fasting glucose, the association was attenuated and no longer statistically significant for these groups, with an HR of 1.12 (95% CI 0.96–1.30) for 9–13 ng/L and an HR of 1.13 (95% CI 0.93–1.38) for ≥14 ng/L. The association between hs-cTnT groups and incident diagnosed diabetes for participants with undiagnosed diabetes at baseline was not significant. Among participants with hs-cTnT ≥14 ng/L, but without undiagnosed diabetes and/or metabolic syndrome, there was a consistently higher risk for incident diagnosed self-reported diabetes compared with those with hs-cTnT ≤5 ng/L, with HRs of 1.82 (95% CI 1.22–2.71) and 1.47 (95% CI 1.05–2.05), respectively, even after adjustment for fasting glucose. There was no significant association for the groups by BMI except for obese (BMI 25–30 kg/m2) participants in the highest hs-cTnT group, who had an HR of 1.46 (95% CI 1.04–2.05).
Figure 1.
Kaplan-Meier estimates of the incidence of diabetes stratified by hs-cTnT group.
Table 2.
Hazard ratio (95% CI) of incident diabetes by major diabetes risk factor groups stratified by hs-cTnT
| ≤5 ng/L | 6–8 ng/L | 9–13 ng/L | ≥14 ng/L | P for trend | P for interaction* | |
|---|---|---|---|---|---|---|
| Overall | ||||||
| Model 1 | Reference | 1.09 (0.97–1.23) | 1.35 (1.16–1.56) | 1.66 (1.36–2.02) | <0.001 | – |
| Model 2 | Reference | 0.98 (0.86–1.11) | 1.14 (0.99–1.33) | 1.25 (1.03–1.53) | 0.018 | – |
| Model 3 | Reference | 0.93 (0.82–1.05) | 1.12 (0.96–1.30) | 1.13 (0.93–1.38) | 0.154 | – |
| Undiagnosed diabetes | ||||||
| Model 1 | Reference | 0.95 (0.72–1.24) | 1.03 (0.74–1.43) | 0.86 (0.59–1.24) | 0.538 | – |
| Model 2 | Reference | 0.94 (0.71–1.25) | 1.13 (0.79–1.62) | 0.84 (0.57–1.23) | 0.615 | – |
| Model 3 | Reference | 0.87 (0.66–1.16) | 1.09 (0.77–1.55) | 0.81 (0.55–1.19) | 0.485 | – |
| Fasting glucose | ||||||
| Normal | ||||||
| Model 1 | Reference | 0.95 (0.73–1.23) | 1.07 (0.75–1.51) | 2.13 (1.44–3.15) | 0.014 | <0.001 |
| Model 2 | Reference | 0.91 (0.70–1.19) | 1.02 (0.72–1.44) | 1.81 (1.22–2.70) | 0.078 | <0.001 |
| Model 3 | Reference | 0.91 (0.70–1.19) | 1.02 (0.72–1.45) | 1.82 (1.22–2.71) | 0.072 | 0.012 |
| Impaired | ||||||
| Model 1 | Reference | 1.03 (0.88–1.21) | 1.33 (1.10–1.61) | 1.21 (0.90–1.62) | 0.009 | – |
| Model 2 | Reference | 0.93 (0.79–1.10) | 1.15 (0.95–1.39) | 0.96 (0.71–1.29) | 0.578 | – |
| Model 3 | Reference | 0.94 (0.79–1.10) | 1.12 (0.93–1.36) | 0.96 (0.72–1.29) | 0.661 | – |
| Metabolic syndrome | ||||||
| No | ||||||
| Model 1 | Reference | 0.97 (0.79–1.20) | 1.07 (0.82–1.40) | 1.70 (1.23–2.37) | 0.027 | <0.001 |
| Model 2 | Reference | 0.91 (0.74–1.12) | 1.00 (0.76–1.31) | 1.54 (1.10–2.15) | 0.150 | <0.001 |
| Model 3 | Reference | 0.80 (0.65–1.00) | 0.95 (0.72–1.25) | 1.47 (1.05–2.05) | 0.408 | <0.001 |
| Yes | ||||||
| Model 1 | Reference | 1.08 (0.93–1.26) | 1.34 (1.12–1.60) | 1.39 (1.09–1.77) | <0.001 | – |
| Model 2 | Reference | 1.01 (0.87–1.18) | 1.21 (1.01–1.45) | 1.18 (0.92–1.51) | 0.043 | – |
| Model 3 | Reference | 0.96 (0.82–1.12) | 1.18 (0.98–1.41) | 1.03 (0.80–1.32) | 0.280 | – |
Model 1: age, race-center, sex; model 2: model 1 plus total cholesterol, LDL-C, HDL-C, triglycerides, cholesterol-lowering medication use, BMI, systolic blood pressure, blood pressure–lowering medication use, smoking status, eGFR, family history of coronary heart disease, waist circumference, physical activity, education level, and annual family income level; model 3: model 2 plus fasting glucose.
*P value for interaction within the respective subgroup, where applicable.
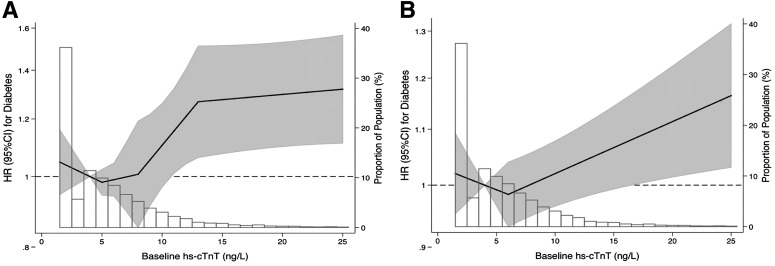
To examine the continuous association, we modeled hs-cTnT as a piece-wise linear spline with knots at 5, 8, and 14 ng/L using a fully adjusted model that included fasting glucose. There was a nonsignificant increase in the risk for incident diagnosed diabetes for participants with hs-cTnT <8 ng/L, but the risk appeared to sharply increase among participants with hs-cTnT between 8 and 14 ng/L. Participants with hs-cTnT ≥14 ng/L had a statistically significant elevation in risk for diagnosed diabetes with an HR >1.2, although the incremental increase in risk with further rise in hs-cTnT beyond 14 ng/L was small (Fig. 2).
Figure 2.
Adjusted HR and 95% CI of incident diabetes by hs-cTnT level with superimposed frequency histograms. A: The linear spline model has three knots at 5, 8, and 14 ng/L. B: The linear spline model has one knot at 6 ng/L. The hs-cTnT level is represented by solid lines and the 95% CI is represented by the shaded area. The data were truncated at the 99th percentiles. The models were adjusted for age, race-center, sex, total cholesterol, HDL-C, LDL-C, triglycerides, BMI, eGFR, systolic blood pressure, blood pressure–lowering medication use, smoking status, cholesterol-lowering medication use, and fasting glucose.
A higher risk for diagnosed diabetes among participants with hs-cTnT ≥14 ng/L was also observed in subgroup analysis for participants not taking statins (HR 1.34; 95% CI 1.09–1.66), those without hypertension (HR 1.71; 95% CI 1.22–2.41), and those without self-reported hypercholesterolemia (HR 1.33; 95% CI 1.07–1.64) (Table 3). After adjustment for glucose, these relationships remained significant only for those without hypertension (HR 1.46; 95% CI 1.03–2.07), and overall, the interaction term among the subgroups was statistically nonsignificant.
Table 3.
Subgroup analysis of the HR (95% CI) for incident diabetes by hs-cTnT group
| ≤5 ng/L | 6–8 ng/L | 9–13 ng/L | ≥14 ng/L | P for trend | P for interaction* | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Men | ||||||
| Model 1 | Reference | 0.94 (0.79–1.13) | 1.03 (0.84–1.27) | 1.30 (1.02–1.65) | 0.088 | 0.148 |
| Model 2 | Reference | 0.91 (0.76–1.09) | 1.06 (0.87–1.30) | 1.20 (0.94–1.54) | 0.156 | 0.172 |
| Women | ||||||
| Model 1 | Reference | 0.99 (0.83–1.18) | 1.27 (1.01–1.59) | 0.88 (0.57–1.35) | 0.367 | – |
| Model 2 | Reference | 0.93 (0.78–1.11) | 1.20 (0.96–1.50) | 0.79 (0.51–1.22) | 0.930 | – |
| Race | ||||||
| White | ||||||
| Model 1 | Reference | 0.94 (0.81–1.08) | 1.14 (0.96–1.36) | 1.20 (0.95–1.51) | 0.096 | 0.393 |
| Model 2 | Reference | 0.90 (0.77–1.04) | 1.05 (0.89–1.26) | 1.12 (0.88–1.42) | 0.458 | 0.364 |
| Black | ||||||
| Model 1 | Reference | 1.05 (0.82–1.33) | 1.08 (0.80–1.46) | 1.25 (0.85–1.83) | 0.289 | – |
| Model 2 | Reference | 0.98 (0.77–1.25) | 1.13 (0.83–1.52) | 1.10 (0.75–1.61) | 0.483 | – |
| Age | ||||||
| <65 years | ||||||
| Model 1 | Reference | 1.00 (0.86–1.18) | 1.32 (1.09–1.62) | 1.21 (0.91–1.62) | 0.018 | 0.202 |
| Model 2 | Reference | 0.94 (0.80–1.10) | 1.34 (1.10–1.64) | 1.22 (0.91–1.62) | 0.025 | 0.132 |
| ≥65 years | ||||||
| Model 1 | Reference | 0.96 (0.78–1.17) | 0.99 (0.79–1.23) | 1.26 (0.95–1.67) | 0.311 | – |
| Model 2 | Reference | 0.92 (0.76–1.13) | 0.92 (0.73–1.15) | 0.99 (0.74–1.32) | 0.645 | – |
| Statin use | ||||||
| Yes | ||||||
| Model 1 | Reference | 0.64 (0.42–0.97) | 1.15 (0.76–1.72) | 0.63 (0.31–1.25) | 0.495 | 0.174 |
| Model 2 | Reference | 0.73 (0.48–1.11) | 1.13 (0.76–1.70) | 0.78 (0.39–1.55) | 0.817 | 0.228 |
| No | ||||||
| Model 1 | Reference | 1.03 (0.91–1.17) | 1.14 (0.97–1.34) | 1.34 (1.09–1.66) | 0.006 | – |
| Model 2 | Reference | 0.97 (0.85–1.11) | 1.13 (0.96–1.32) | 1.20 (0.97–1.48) | 0.069 | – |
| Hypercholesterolemia | ||||||
| Yes | ||||||
| Model 1 | Reference | 0.64 (0.44–0.92) | 1.10 (0.77–1.57) | 0.81 (0.44–1.47) | 0.656 | 0.046 |
| Model 2 | Reference | 0.71 (0.50–1.03) | 0.98 (0.69–1.40) | 0.97 (0.53–1.76) | 0.689 | 0.104 |
| No | ||||||
| Model 1 | Reference | 1.05 (0.92–1.20) | 1.14 (0.97–1.34) | 1.33 (1.07–1.64) | 0.008 | – |
| Model 2 | Reference | 0.99 (0.86–1.13) | 1.13 (0.95–1.33) | 1.18 (0.95–1.46) | 0.085 | – |
| Hypertension | ||||||
| Yes | ||||||
| Model 1 | Reference | 1.01 (0.86–1.19) | 1.17 (0.97–1.41) | 1.08 (0.85–1.38) | 0.190 | 0.116 |
| Model 2 | Reference | 0.95 (0.81–1.12) | 1.13 (0.94–1.36) | 1.00 (0.78–1.29) | 0.523 | 0.387 |
| No | ||||||
| Model 1 | Reference | 0.92 (0.75–1.12) | 1.05 (0.81–1.36) | 1.71 (1.22–2.41) | 0.071 | – |
| Model 2 | Reference | 0.88 (0.72–1.07) | 1.08 (0.83–1.39) | 1.46 (1.03–2.07) | 0.199 | – |
| BMI | ||||||
| <25 kg/m2 | ||||||
| Model 1 | Reference | 0.87 (0.61–1.22) | 0.89 (0.55–1.45) | 0.97 (0.48–1.99) | 0.579 | <0.001 |
| Model 2 | Reference | 0.83 (0.59–1.18) | 0.89 (0.54–1.45) | 0.89 (0.43–1.84) | 0.449 | <0.001 |
| 25–30 kg/m2 | ||||||
| Model 1 | Reference | 1.14 (0.93–1.40) | 1.15 (0.89–1.48) | 1.46 (1.04–2.05) | 0.032 | – |
| Model 2 | Reference | 1.08 (0.88–1.33) | 1.07 (0.83–1.39) | 1.41 (1.00–1.98) | 0.097 | – |
| ≥30 kg/m2 | ||||||
| Model 1 | Reference | 0.94 (0.79–1.12) | 1.21 (0.99–1.48) | 1.19 (0.91–1.55) | 0.082 | – |
| Model 2 | Reference | 0.89 (0.74–1.06) | 1.21 (0.99–1.48) | 1.03 (0.78–1.34) | 0.337 | – |
Model 1: age, race-center, sex, total cholesterol, HDL-C, LDL-C, triglycerides, BMI, eGFR, systolic blood pressure, blood pressure–lowering medication use, smoking status, cholesterol-lowering medication use, family history of coronary heart disease, waist circumference, physical activity, education level, and annual family income level; model 2: model 1 plus fasting glucose.
*P value for interaction within the respective subgroup, where applicable.
Adding hs-cTnT to a model that contained age, race, and sex improved the C statistic for the prediction of diabetes by +0.0089 (P < 0.001) (Table 4). In the fully adjusted model with fasting glucose, there was a C statistic of 0.7636, indicating good prediction. The addition of hs-cTnT to this fully adjusted model that already included fasting glucose also demonstrated a statistically significant increase in the C statistic (+0.0008, P = 0.023). The addition of hs-cTnT provided a similar improvement in the C statistic of 0.0006 (P = 0.04) among individuals at low risk for diagnosed diabetes and CVD (those without hypertension, hypercholesterolemia, or impaired fasting glucose) and an improvement of 0.005 (P = 0.005) for those with normal fasting glucose (Table 4 and Supplementary Table 1). The NRI and integrated discrimination improvement index analyses were largely consistent with the C-statistic results, demonstrating that hs-cTnT was associated with the largest improvement in risk discrimination for participants in the “low-risk” group or those with normal fasting glucose, although these improvements were not statistically significant for the continuous NRI (Supplementary Table 2).
Table 4.
Risk prediction for incident diabetes
| C statistic | Change in C statistic** | P value** | |
|---|---|---|---|
| Overall | |||
| Age, sex, race | 0.5749 | Reference | Reference |
| +Risk factors* | 0.6983 | 0.1235 | <0.001 |
| +Fasting glucose | 0.7438 | 0.1690 | <0.001 |
| +hs-cTnT | 0.5838 | 0.0089 | <0.001 |
| Fully adjusted without hs-cTnT | 0.7636 | 0.1888 | <0.001 |
| Fully adjusted with hs-cTnT | 0.7644 | 0.1896 | 0.023† |
| Low-risk groupa | |||
| Age, sex, race | 0.5690 | Reference | Reference |
| +Risk factors* | 0.6961 | 0.1271 | <0.001 |
| +Fasting glucose | 0.7463 | 0.1774 | <0.001 |
| +hs-cTnT | 0.5772 | 0.0083 | <0.001 |
| Fully adjusted without hs-cTnT | 0.7658 | 0.1968 | <0.001 |
| Fully adjusted with hs-cTnT | 0.7664 | 0.1975 | 0.040† |
| Normal fasting glucose | |||
| Age, sex, race | 0.5615 | Reference | Reference |
| +Risk factors* | 0.6871 | 0.1256 | <0.001 |
| +Fasting glucose | 0.7435 | 0.1820 | <0.001 |
| +hs-cTnT | 0.5766 | 0.0151 | <0.001 |
| Fully adjusted without hs-cTnT | 0.7258 | 0.1642 | <0.001 |
| Fully adjusted with hs-cTnT | 0.7308 | 0.1693 | <0.001† |
*Models adjusted for: age, race-center, sex, total cholesterol, HDL-C, LDL-C, triglycerides, BMI, eGFR, systolic blood pressure, blood pressure–lowering medication use, smoking status, cholesterol-lowering medication use, family history of coronary heart disease, waist circumference, physical activity, education level, and annual family income level.
**Compared with age, sex, and race, except where noted.
†Compared with the fully adjusted model without hs-cTnT.
aDefined as no hypertension, hypercholesterolemia, or metabolic syndrome.
Censoring of the first 2 years and first 5 years of follow-up showed similar results to our analysis for complete follow-up, although the overall results were more attenuated with censoring of the first 5 years of follow-up (Supplementary Tables 3 and 4). Additional adjustment for alcohol consumption, parental history of diabetes, and insulin levels did not appreciably alter our results (Supplementary Table 5).
Conclusions
Our results show that among participants without clinically diagnosed CVD, the presence of subclinical myocardial damage—determined by an elevation in hs-cTnT—was associated with a modest but statistically significantly increased risk of incident diagnosed diabetes. This association was strongest among participants without a traditional risk factor and among those at low risk for incident diagnosed diabetes and CVD. Detectable levels of hs-cTnT may potentially be a result of an individual or a combination of myocardial insults because it is associated with submyocardial infarction, underlying structural myocardial disease such as left ventricular hypertrophy, heart failure, and microvascular disease (19–22). These findings suggest that hs-cTnT may incorporate overlapping pathophysiology for the development of both diabetes and CVD, which could help to prioritize prevention strategies for these individuals. Hyperglycemia is strongly associated with microvascular dysfunction and, along with lipotoxicity, has been suggested as a possible mechanism to explain elevated hs-cTnT levels and microvascular myocardial infarctions among individuals with diabetes (23). Other possible mechanisms include shared risk factors between diabetes and CVD that are not directly evaluated here, such as inflammation, endothelial dysfunction, and platelet activation. It may be that a certain amount of subclinical cardiovascular damage from early hyperglycemia (below the threshold for a diagnosis of diabetes) and/or coexisting CVD risk factors may accrue before the onset of diabetes (24). Therefore, an elevated hs-cTnT may at least partially serve as a marker of the cumulative long-term exposure to pathophysiologic changes that occur before diabetes is typically diagnosed. The statistically significant improvement in the C statistic beyond fasting glucose and other risk factors, although clinically small, demonstrates that hs-cTnT provides an additional description of the risk of diabetes not captured by traditional risk factors.
We found that even after adjustment for traditional diabetes risk factors, there was an increased risk of diagnosed diabetes among participants with elevated levels of hs-cTnT. Further adjustment for fasting glucose attenuated this relationship to null, which became statistically nonsignificant. However, the inclusion of fasting glucose as a covariable in our models may represent overadjustment, because fasting glucose also reflects underlying hyperglycemia and those individuals with the highest glucose levels are more likely to cross the threshold to incident diagnosed diabetes. Despite this, we found that the addition of hs-cTnT resulted in a statistically significant, although clinically modest, increase in the risk prediction of incident diagnosed diabetes when added to fully adjusted models that included fasting glucose. Moreover, we found that nearly two-thirds of participants who were subsequently diagnosed with diabetes had evidence of subclinical myocardial damage at baseline and that this percentage remained virtually unchanged after those with undiagnosed diabetes at baseline (20.1%) were excluded. Possible mechanisms for the shared development of diabetes and CVD include increased oxidative stress and advanced glycation end products, both of which have been suggested as pathways for β-cell damage and elevations in hs-cTnT (25–29).
Although our results demonstrate an overall association between hs-cTnT and incident diagnosed diabetes, they suggest that the relationship is stronger in certain groups of individuals. First, the relationship with incident diabetes was not significant at hs-cTnT levels <8 ng/L and was relatively weak for levels <14 ng/L. These levels of hs-cTnT are representative of subclinical myocardial damage, but other nonglucose risk factors may be responsible for most of the increase in hs-cTnT at these lower levels, which is suggested by the smaller attenuation in risk for diabetes after adjustment for glucose in these groups. Accordingly, these relatively low elevations of hs-cTnT may also reflect a lower cumulative exposure to hyperglycemia in which fewer individuals would be expected to progress to incident diagnosed diabetes.
Second, we found that the relative relationship between hs-cTnT and incident diagnosed diabetes was stronger for participants who would traditionally be considered at lower risk for diabetes and CVD such as those with normal fasting glucose, those without metabolic syndrome, those without cardiovascular risk factors, such as hypertension or hypercholesterolemia, those not treated with statin therapy, and those <65 years old. Furthermore, the association between hs-cTnT and incident diagnosed diabetes remained significant even after adjusting for fasting glucose, with the exception of participants without hypertension, in which it became nonsignificant (P = 0.085). This stronger relationship in low-risk individuals with less attenuation from adjustment for fasting glucose suggests that there may be a treatment effect. Participants without these risk factors would not be identified as at increased risk for diabetes and/or CVD and, therefore, would be unlikely to be treated. However, individuals with risk factors would presumably be identified as at higher risk for diabetes and CVD and thus more likely to be prescribed treatment. Therefore, the treatment of risk factors may modify the relationship between hs-cTnT and incident diabetes, possibly resulting in a lower hs-cTnT for individuals at higher risk for incident diabetes. This is supported by evidence demonstrating that obesity, diabetes, and persistent elevations in hypertension are associated with increases in hs-cTnT during 6 years of follow-up, although further work is needed to confirm whether a reduction in risk factors is associated with a reduction in hs-cTnT (30).
These results demonstrate that individuals without traditional diabetes and CVD risk factors, such as impaired fasting glucose, hypercholesterolemia, or hypertension, who have a highly elevated hs-cTnT of ≥14 ng/L, are at an increased risk for incident diagnosed diabetes. Furthermore, despite the absence of these traditional diabetes and CVD risk factors, they are also at an increased risk for CVD and all-cause mortality by virtue of an elevated hs-cTnT (Supplementary Table 6) (15,31,32). This is especially relevant, because it has been suggested that one reason glucose-lowering trials have largely failed to show reductions in CVD is that the treatment is too late in the disease process after irreversible atherosclerotic damage has already occurred (33). Therefore, individuals with a low risk profile but a highly elevated hs-cTnT may benefit from closer monitoring with an increased emphasis on dietary and lifestyle modification. Furthermore, the addition of primary prevention medications, such as aspirin and statins, could be considered for patients with a highly elevated hs-cTnT who have a borderline ASCVD risk (5–7.5%) based on the Pooled Cohort equation. Identifying individuals with a highly elevated hs-cTnT who have an increased risk for both diabetes and CVD would also enable resources to be focused on those at highest risk for diabetes and the associated CVD complications.
Certain limitations of this study should be considered in the interpretation of our results, including the lack of follow-up blood glucose measurements and reliance on reports of diagnosed diabetes and glucose-lowering medication use during annual telephone calls to define incident diagnosed diabetes cases. This likely resulted in missing many undiagnosed cases during follow-up, especially early in follow-up. Indeed, the definition of incident diagnosed diabetes used in the current study (identified by self-report or use of a diabetes medication) has been shown to be specific (87%) but has a low sensitivity (59%) compared with a definition incorporating HbA1c ≥6.5% (34). We used this definition of incident diabetes because there is no biochemical information after Visit 4 (the baseline for this analysis) in ARIC to define incident diabetes. We used only a single measurement of hs-cTnT and the other risk factors examined here, as understanding the prognostic relevance of single measurements is most applicable to clinical care.
We cannot rule out the possibility that reverse causation may explain our results. After adjustment, however, we found that the strongest association between hs-cTnT and incident diabetes was among individuals with normal fasting glucose. Indeed, among individuals with undiagnosed diabetes, no association was found between hs-cTnT and incident diabetes, even in models adjusted only for demographics. The results of subgroup analyses should be interpreted keeping in mind the multiple tests and relatively small sample size of certain subgroups. In addition, as with any observational study, residual confounding remains a concern.
Strengths of this study include the prospective long-term follow-up of more than a decade in participants from a community-based study. This study also benefited from the annual follow-up with participants, rigorous measurement of known diabetes and CVD risk factors, and the use of a centralized laboratory to standardize the analysis of the biomarkers.
Overall, these results demonstrate that individuals without CVD who have subclinical myocardial damage, as represented by an elevated hs-cTnT level, are more likely to develop diagnosed diabetes. Surprisingly, this relationship was strongest in participants who lacked a traditional risk factor or group of risk factors, which suggests that the treatment of traditional risk factors may modify the relationship between hs-cTnT and risk of incident diagnosed diabetes. Regardless, an elevated hs-cTnT is associated with both an increased risk of incident diagnosed diabetes and CVD. This may reflect a pathophysiologic overlap between CVD and diabetes incorporated by hs-cTnT, which is beyond that encompassed by fasting glucose and traditional risk factors. Accordingly, our results demonstrate that the measurement of hs-cTnT can identify individuals who are at an increased risk of both diagnosed diabetes and CVD, which may facilitate the use of resources for those at an increased risk for the associated complications of diabetes and CVD.
Supplementary Material
Article Information
Acknowledgments. The authors thank the staff and participants of the ARIC study for their important contributions. The authors also thank the late Dr. Frederick Brancati (Welch Center for Prevention, Epidemiology and Clinical Research, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; Division of General Internal Medicine, Johns Hopkins Department of Medicine, Baltimore, MD) for his invaluable assistance with the manuscript.
Funding. The ARIC study is performed as a collaborative study supported by National Heart, Lung, and Blood Institute contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C. S.P.W. was partly supported by National Institutes of Health/National Heart, Lung, and Blood Institute Cardiovascular Epidemiology training grant T32-HL-007024 and the Pollin Cardiovascular Prevention Fellowship. This work was also supported by National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases grants R01-DK-089174 and K24-DK-106414 to E.S.
Reagents for the hs-cTnT were donated by Roche Diagnostics.
Duality of Interest. C.M.B. and E.S. have served on an advisory board for Roche Diagnostics. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. S.P.W., J.W.M., and E.S. analyzed the data. J.W.M., M.L., J.C., and C.M.B. contributed to the discussion and reviewed and edited the manuscript. E.S. coordinated the study, interpreted the data, contributed to the discussion, and reviewed and edited the manuscript. S.P.W. and E.S. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1541/-/DC1.
References
- 1.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB Sr. Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation 2006;113:2914–2918 [DOI] [PubMed] [Google Scholar]
- 2.Selvin E, Rawlings AM, Grams M, et al. Fructosamine and glycated albumin for risk stratification and prediction of incident diabetes and microvascular complications: a prospective cohort analysis of the Atherosclerosis Risk in Communities (ARIC) study. Lancet Diabetes Endocrinol 2014;2:279–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. JAMA 2004;292:2495–2499 [DOI] [PubMed] [Google Scholar]
- 4.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W, Lee ET, Howard BV, Fabsitz RR, Devereux RB, Welty TK. Fasting plasma glucose and hemoglobin A1c in identifying and predicting diabetes: the strong heart study. Diabetes Care 2011;34:363–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeboah J, Bertoni AG, Herrington DM, Post WS, Burke GL. Impaired fasting glucose and the risk of incident diabetes mellitus and cardiovascular events in an adult population: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2011;58:140–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nichols GA, Hillier TA, Brown JB. Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care 2007;30:228–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stone NJ, Robinson JG, Lichtenstein AH, et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(Suppl. 2):S1–S45 [DOI] [PubMed] [Google Scholar]
- 9.Laufer EM, Mingels AM, Winkens MH, et al. The extent of coronary atherosclerosis is associated with increasing circulating levels of high sensitive cardiac troponin T. Arterioscler Thromb Vasc Biol 2010;30:1269–1275 [DOI] [PubMed] [Google Scholar]
- 10.McEvoy JW, Chen Y, Nambi V, et al. High-sensitivity cardiac troponin T and risk of hypertension. Circulation 2015;132:825–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherwood MW, Kristin Newby L. High-sensitivity troponin assays: evidence, indications, and reasonable use. J Am Heart Assoc 2014;3:e000403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selvin E, Lazo M, Chen Y, et al. Diabetes mellitus, prediabetes, and incidence of subclinical myocardial damage. Circulation 2014;130:1374–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster MC, Rawlings AM, Marrett E, et al. Potential effects of reclassifying CKD as a coronary heart disease risk equivalent in the US population. Am J Kidney Dis 2014;63:753–760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The ARIC Investigators The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol 1989;129:687–702 [PubMed] [Google Scholar]
- 15.Saunders JT, Nambi V, de Lemos JA, et al. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the Atherosclerosis Risk in Communities Study. Circulation 2011;123:1367–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515–526 [Google Scholar]
- 17.Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 2008;27:157–172; discussion 207–212 [DOI] [PubMed]
- 18.Hlatky MA, Greenland P, Arnett DK, et al.; American Heart Association Expert Panel on Subclinical Atherosclerotic Diseases and Emerging Risk Factors and the Stroke Council . Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation 2009;119:2408–2416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndumele CE, Coresh J, Lazo M, et al. Obesity, subclinical myocardial injury, and incident heart failure. JACC Heart Fail 2014;2:600–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol 2011;58:1332–1339 [DOI] [PubMed] [Google Scholar]
- 21.Yokoyama I, Momomura S, Ohtake T, et al. Reduced myocardial flow reserve in non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 1997;30:1472–1477 [DOI] [PubMed] [Google Scholar]
- 22.Pons-Lladó G, Ballester M, Borrás X, et al. Myocardial cell damage in human hypertension. J Am Coll Cardiol 2000;36:2198–2203 [DOI] [PubMed] [Google Scholar]
- 23.Wallace TW, Abdullah SM, Drazner MH, et al. Prevalence and determinants of troponin T elevation in the general population. Circulation 2006;113:1958–1965 [DOI] [PubMed] [Google Scholar]
- 24.Folsom AR, Alonso A, Misialek JR, et al. Parathyroid hormone concentration and risk of cardiovascular diseases: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J 2014;168:296–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin N, Zhang H, Su Q. Advanced glycation end-products induce injury to pancreatic beta cells through oxidative stress. Diabetes Metab 2012;38:250–257 [DOI] [PubMed] [Google Scholar]
- 26.Coughlan MT, Yap FY, Tong DC, et al. Advanced glycation end products are direct modulators of β-cell function. Diabetes 2011;60:2523–2532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol 2003;41:1387–1393 [DOI] [PubMed] [Google Scholar]
- 28.Huebschmann AG, Regensteiner JG, Vlassara H, Reusch JE. Diabetes and advanced glycoxidation end products. Diabetes Care 2006;29:1420–1432 [DOI] [PubMed] [Google Scholar]
- 29.Monnier VM, Sell DR, Genuth S. Glycation products as markers and predictors of the progression of diabetic complications. Ann N Y Acad Sci 2005;1043:567–581 [DOI] [PubMed] [Google Scholar]
- 30.McEvoy JW, Lazo M, Chen Y, et al. Patterns and determinants of temporal change in high-sensitivity cardiac troponin-T: the Atherosclerosis Risk in Communities Cohort Study. Int J Cardiol 2015;187:651–657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 2010;304:2503–2512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.deFilippi CR, de Lemos JA, Christenson RH, et al. Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA 2010;304:2494–2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Skyler JS, Bergenstal R, Bonow RO, et al.; American Diabetes Association; American College of Cardiology Foundation; American Heart Association . Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a Scientific Statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol 2009;53:298–304 [DOI] [PubMed] [Google Scholar]
- 34.Schneider AL, Pankow JS, Heiss G, Selvin E. Validity and reliability of self-reported diabetes in the Atherosclerosis Risk in Communities Study. Am J Epidemiol 2012;176:738–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.