Abstract
Background and purpose — Hip dislocation is one of the most common complications following total hip arthroplasty (THA). Several factors that affect dislocation have been identified, including acetabular cup positioning. Optimal values for cup inclination and anteversion are debatable. We performed a systematic review to describe the different methods for measuring cup placement, target zones for cup positioning, and the association between cup positioning and dislocation following primary THA.
Methods — A systematic search of literature in the PubMed database was performed (January and February 2016) to identify articles that compared acetabular cup positioning and the risk of dislocation. Surgical approach and methods for measurement of cup angles were also considered.
Results— 28 articles were determined to be relevant to our research question. Some articles demonstrated that cup positioning influenced postoperative dislocation whereas others did not. The majority of articles could not identify a statistically significant difference between dislocating and non-dislocating THA with regard to mean angles of cup anteversion and inclination. Most of the articles that assessed cup placement within the Lewinnek safe zone did not show a statistically significant reduction in dislocation rate. Alternative target ranges have been proposed by several authors.
Interpretation— The Lewinnek safe zone could not be justified. It is difficult to draw broad conclusions regarding a definitive target zone for cup positioning in THA, due to variability between studies and the likely multifactorial nature of THA dislocation. Future studies comparing cup positioning and dislocation rate should investigate surgical approach separately. Standardized tools for measurement of cup positioning should be implemented to allow comparison between studies.
Hip dislocation is one of the most common complications following THA. A study investigating dislocation within 1 year of primary THA found an overall rate of 1.7% (Khatod et al. 2006) while other studies have found dislocation rates of approximately 3% (Woo and Morrey 1982, Mahomed et al. 2003). Registry-based studies have reported that dislocation is among the leading causes of revision after primary THA (Hailer et al. 2012, Kostensalo et al. 2013, Garellick et al. 2014). Several patient- and surgery-related risk factors for dislocation have been identified, including age (Meek et al. 2006), BMI, ASA score (Jolles et al. 2002), alcohol intake (Paterno et al. 1997), cerebral dysfunction during hospital stay (Woolson and Rahimtoola 1999), rheumatoid arthritis (Khatod et al. 2006), femoral neck length and femoral component fixation (Woolson and Rahimtoola 1999, Nishii et al. 2004), smaller femoral head size (Jolles et al. 2002), soft-tissue factors such as muscular imbalance (Herrlin et al. 1986) and soft-tissue traction (Higa et al. 2011), surgical approach (Woo and Morrey 1982, Masonis and Bourne 2002), and acetabular cup positioning (Lewinnek et al. 1978).
The placement of the cup has historically been guided by the "safe zone", as detailed by Lewinnek et al. (1978). Possible consequences of inappropriate cup positioning include impingement (Higa et al. 2011), wear and edge loading (Callanan et al. 2011), liner fracture leading to osteolysis and aseptic loosening, and reduced range of movement and limb-length discrepancy—subsequently leading to increased revision rates (Kennedy et al. 1998, Nishii et al. 2004, Eilander et al. 2013). On the whole, there is no consensus regarding the optimal placement of the acetabular component in primary THA. We performed a systematic review of available literature (1) to identify different methods for measurement of acetabular component placement, (2) to identify various target zones proposed by investigators, and (3) to investigate whether it is acknowledged in the literature that acetabular malpositioning may be a significant risk factor for dislocation following primary THA.
Methods
In January and February 2016, we conducted a systematic search for literature in the PubMed database that compared angles for cup positioning and dislocation rates in THA. MeSH headings identified for this search included "arthroplasty, replacement, hip", "dislocations", and "outcome and process assessment (health care)".
The search strategy is detailed in Table 1. The results of this search were processed using a 3-step review process of article identification, selection, and inclusion. The investigator was not blind regarding the source of the articles or the authors. Titles of articles listed were screened for relevance to the research question. Abstracts of the articles identified were reviewed and selected for full-text review if there was any mention or indication of a comparison between cup positioning and dislocation rate. Abstracts with no full text unavailable were excluded. Full texts were marked either for inclusion or for exclusion based on predetermined eligibility criteria (as shown in Table 2). Studies that focused on dislocations in hip dysplasia cohorts were excluded as it has been perceived that other factors such as Crowe typing, osteotomy, hip loading, and placement outside the true acetabular region may influence appropriate cup positioning in this group (Pagnano et al. 1996, Bicanic et al. 2009).
Table 1.
PubMed search strategy
| 1. Hip arthroplasty OR hip replacement OR hip prosthesis OR hip implant. |
| 2. Dislocation OR luxation. |
| 3. Orientation OR position OR malposition OR location OR placement OR fitting OR alignment OR anteversion OR inclination OR abduction. |
| 4. Cup OR acetabular component OR socket OR shell. |
| 5. 1 AND 2 AND 3 AND 4. |
Table 2.
Inclusion and exclusion criteria for articles reviewed
| Inclusion criteria |
| Primary THA |
| Cup placement described in terms of anteversion and inclination |
| Mean or target range of anteversion and/or inclination identified |
| Dislocation number/rate identified and compared to cup placement |
| Full text available |
| English-language text |
| Exclusion criteria |
| Revision THA study |
| Hip resurfacing THA |
| Dual mobility THA |
| Hip dysplasia study |
| Animal and cadaver study |
| Non-patient study (e.g. biometric computational simulation(s)) |
Included articles were required to compare the dislocation rate in a patient population and cup abduction and/or inclination angles. Alternatively, a comparison between dislocating/non-dislocating THA and cup abduction and/or inclination was required. Articles lacking this level of quantitative assessment were otherwise included for qualitative purposes. Surgical approach, femoral head size, and the method for measurement of cup positioning were also noted. References within included articles were also included if they were pertinent to our research question. Titles marked for exclusion were reviewed for relevance by a second author before a final decision regarding inclusion or exclusion.
The articles that were included were assessed for quality (Table 3). Criteria assessed were derived from the PRISMA preferred reporting items checklist (Moher et al. 2009) and the Critical Appraisal Skills Programme (CASP) tools (CASP UK 2013), concentrating especially on internal validity, methodological quality, and the presentation of results.
Table 3.
Criteria for appraisal of articles
| Study type | RCT |
|---|---|
| Cohort | |
| Case-control | |
| Case series | |
| Prospective/retrospective | |
| Surgical approach | Anterior, anterolateral, lateral (transgluteal, transtrochanteric), posterolateral, posterior, minimally invasive (Kelmanovich et al. 2003) |
| Diagnoses | A, posttraumatic, AVN, inflammatory, hip dysplasia |
| Patient characteristics | Age |
| Sex | |
| Obesity (weight, height, BMI) | |
| Cup positioning | Anteversion ± inclination |
| Method of measurement | |
| Follow-up | Follow-up period |
Angles for anteversion and inclination presented in the included articles were categorized as follows: (1) angle (mean (SD) (range)) vs. dislocation rate; (2) Lewinnek safe zone: dislocating vs. non-dislocating hips; (3) target range vs. dislocation rate.
We also documented all other statistical tests that had been performed.
Results
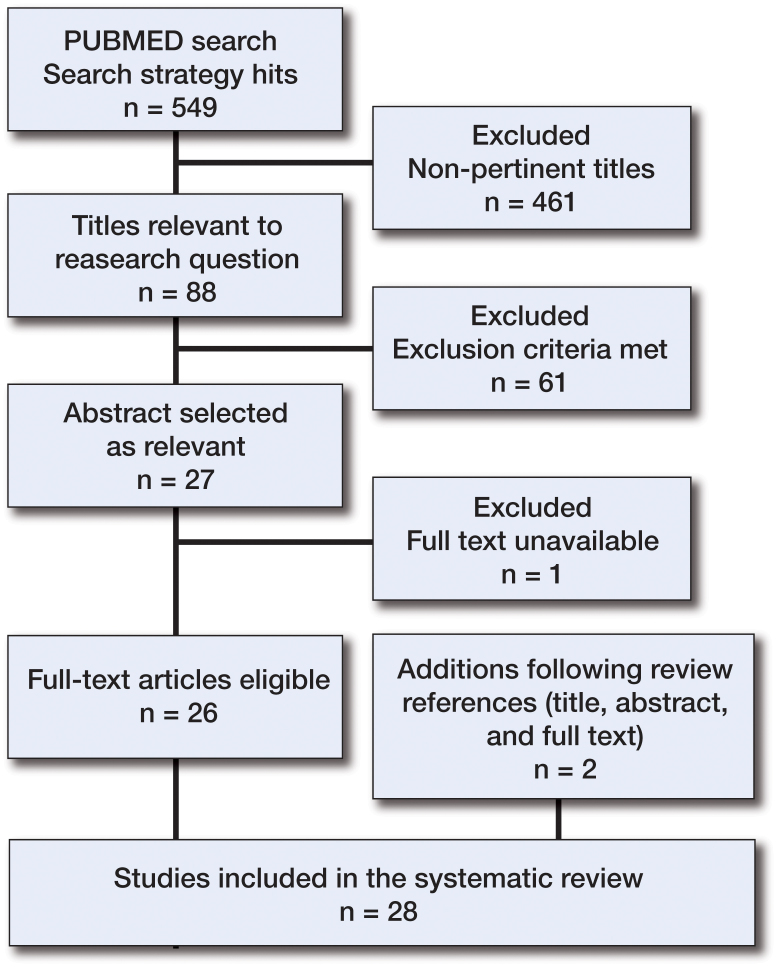
The initial search strategy gave 549 articles. 88 abstracts were reviewed and 27 were selected for further analysis. The full text of 1 article (McCollum and Gray 1990) could not be retrieved and it was excluded, leaving 26 articles. A review of references in these articles revealed that an additional 2 articles were relevant to our research question, and they were included following a review of title, abstract, and full text. In summary, 28 journal articles were included in this systematic review (Figure 1).
Figure 1.
PRISMA flow diagram of search strategy and review of literature (Moher et al. 2009).
Publication dates ranged from 1978 to 2016. 15 of the 28 of articles were published in the period 2006–2016. All but 2 articles had both the age and sex distribution of the patient sample. Preoperative diagnoses were detailed sufficiently in 20 of the 28 articles. The surgical approach was stated in 27 articles, with the majority of THAs being performed via the posterolateral approach (15/28) or the posterior approach (6/28). The follow-up period was described in 19 of the 28 articles; this ranged from no follow-up to at least 5 years. The total number of THAs investigated in each study ranged from 75 (Kennedy et al. 1998) to 9,784 (Abdel et al. 2016). The dislocation rate was not stated in 1 article (Pierchon et al. 1994). Of the remaining 27 articles, dislocation rates ranged from 0.48% (Dudda et al. 2010) to 7.21% (Pollard et al. 1995). This information is summarized in Tables 4 and 5 (see Supplementary data).
Measurement of cup positioning
Angles of anteversion and inclination can be assessed anatomically, radiographically, and intraoperatively as described by Murray (1993). Radiographic anteversion and inclination can be measured on standard anteroposterior (AP) radiographs (Tannast et al. 2005). Cup inclination is formed by the transverse axis (ischial tuberosity line) and the plane of the acetabular opening, as shown in Figure 2. The calculation of cup anteversion is explained in Figure 3 (McLaren 1973, Murray 1993). These calculations were performed either manually or by using computer software such as the Martell Hip Analysis Suite (HAS) (Danoff et al. 2016), Ein Bild Roentgen Analyse (EBRA) (Biedermann et al. 2005, Esposito et al. 2015, Grammatopoulos et al. 2015, McLawhorn et al. 2015), Sectra PACS IDS7 (Opperer et al. 2016), or OrthoView (Timperley et al. 2016).
Figure 2.
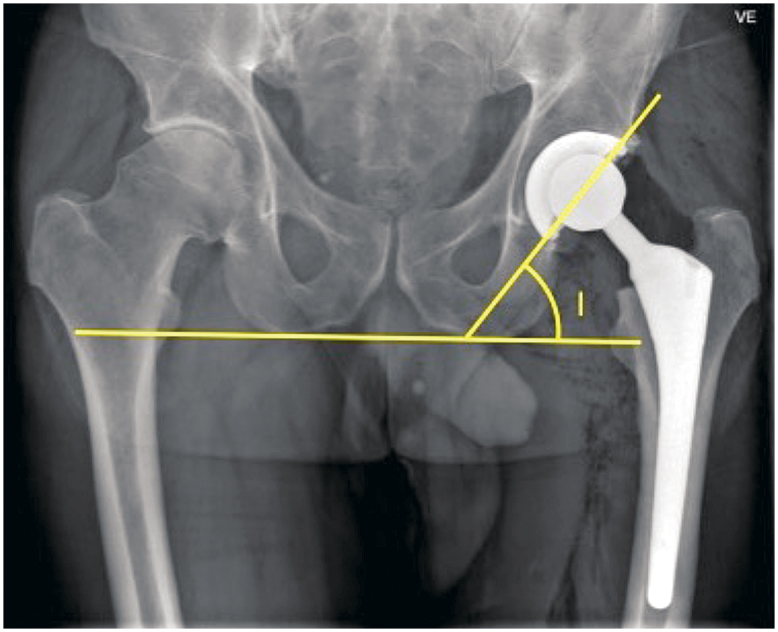
Radiographic cup inclination (I) measured on AP pelvic radiographs (Jolles et al. 2002).
Figure 3.
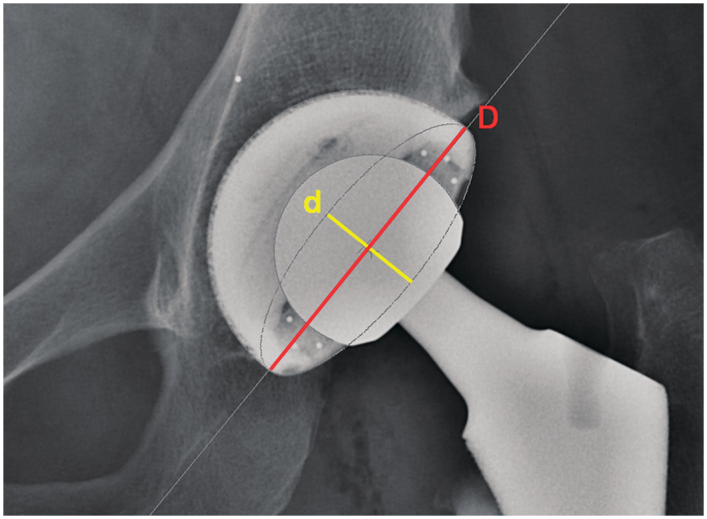
Radiographic cup anteversion as calculated using an AP radiograph (Abdel et al. 2016). d: short axis of the ellipse of the acetabular component; D: long axis of the ellipse of the acetabular component. Anteversion (A) is calculated as: A = sin−1 (d/D).
Lateral radiographs are required to accurately distinguish between cup retroversion and anteversion, as this cannot be determined reliably on an AP radiograph (Woo and Morrey 1982). A shoot-through lateral radiograph may be used to calculate cup anteversion by identification of the angle between the transverse axis and the acetabular opening, as shown in Figure 4. This method has a tendency to overestimate anteversion compared to the AP radiographic calculation (Sculco et al. 2016). 1 study used this method (Jolles et al. 2002). While the standardized AP radiograph is the most common and most logistically accessible method for identifying cup positioning, it does not account for spine deformity or pelvic positioning, and is therefore associated with some inaccuracy compared to anatomical anteversion (Lembeck et al. 2005, Dandachli et al. 2013, Buckland et al. 2015).
Figure 4.
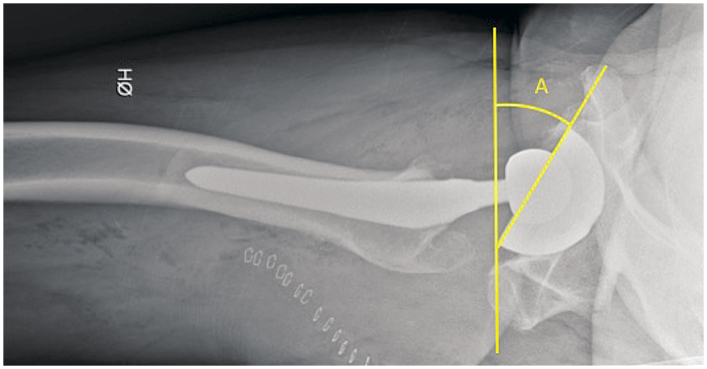
Radiographic cup anteversion (A) from a lateral shoot-through radiograph (Jolles et al. 2002).
3-dimensional analysis of cup positioning may be performed by CT, which will produce angles corresponding to anatomical inclination and anteversion, as shown in Figure 5. Anatomical inclination is defined as the angle between the acetabular axis and the longitudinal axis; anteversion is defined as the angle between the transverse axis and the acetabular axis when projected onto the transverse plane (Murray 1993). These angles are not affected by pelvic positioning, a known confounder in radiological measurements (Wan et al. 2009, Kanawade et al. 2014). 4 studies used CT analysis to determine cup anteversion. To calculate inclination, either AP radiographic reconstructions from CT were generated (Kim et al. 2009) or supplementary AP radiographs were used (Pierchon et al. 1994, Nishii et al. 2004, Fujishiro et al. 2016). 2 studies did not describe the methods by which cup anteversion and inclination were measured (Dudda et al. 2010, Moskal and Capps 2011). 2 studies described the use of intraoperative tools in assisting the placement of the acetabular component: a goniometer (Li et al. 1999) and computer-assisted surgery (CAS) (McLawhorn et al. 2015).
Figure 5.
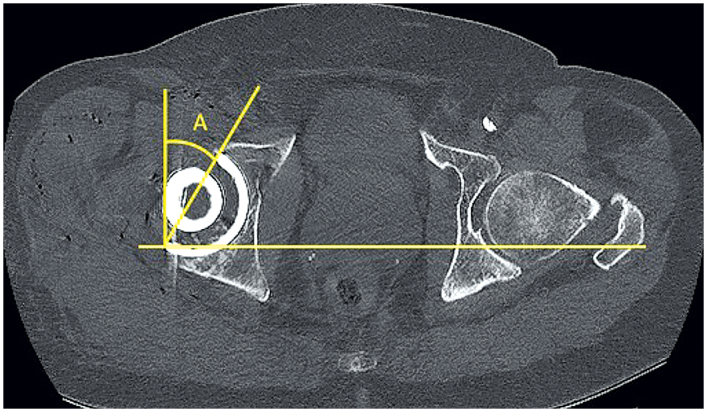
Anatomical cup anteversion using CT imaging (Kim et al. 2009). A: anatomical anteversion with respect to the sagittal plane measured on CT transverse images.
Anteversion and inclination angles
The distribution of cup anteversion and inclination angles was calculated in 19 of the 28 articles and compared between dislocating and non-dislocating hips. Paterno et al. (1997) looked only at inclination. 3 of those 19 studies found a statistically significant difference between mean inclination values when comparing dislocating hips and non-dislocating hips. Biedermann et al. (2005) (anterolateral approach) found that hips that dislocated anteriorly were more abducted, and those that dislocated posteriorly were less abducted than non-dislocating hips. Kim et al. (2009) (posterolateral approach) identified hips with posterior dislocation to have higher inclination angles compared to non-dislocating hips. Garcia-Rey and Garcia-Cimbrelo (2016) (posterolateral) found that dislocating hips in general had greater angles of inclination than non-dislocating hips.
6 of 8 studies found that mean anteversion angles differed statistically significantly between dislocating hips and non-dislocating hips. 4 of these studies used the posterolateral approach (Lewinnek et al. 1978, Nishii et al. 2004, Kim et al. 2009, Fujishiro et al. 2016), 1 the posterior approach (Masaoka et al. 2006), and 1 the anterolateral approach (Biedermann et al. 2005). 4 studies analyzed anterior and posterior dislocations separately; 3 found that anterior dislocations were associated with increased anteversion (Lewinnek et al. 1978, Biedermann et al. 2005, Fujishiro et al. 2016), and 2 found that posterior dislocations were less anteverted compared to non-dislocators (Masaoka et al. 2006, Fujishiro et al. 2016). Nishii et al. (2004) found that anteversion was less in dislocating hips that dislocated posteriorly than in non-dislocating hips. 1 study did not state whether dislocations were anterior or posterior, but the dislocations were found to be less anteverted in this case (Kim et al. 2009).
A significant degree of variability between articles was found when comparing mean angles of anteversion and inclination. As shown in Table 6 (see Supplementary data), most of the articles did not find statistically significant differences in mean inclination values (16/19) and mean anteversion values (12/18) between dislocating and non-dislocating THAs.
Target zone for cup placement
Lewinnek et al. (1978) proposed a safe zone of 30–50 degrees of inclination and 5–25 degrees of anteversion as a means of minimizing postoperative dislocation. Given the association between excessive inclination and an increased rate of wear and edge loading, Callanan et al. (2011) recommended that an inclination range of 30–45 degrees was more ideal.
16 studies identified a range of angles of anteversion and inclination to guide safe placement of the acetabular component; these new target zones differed from the range of values first proposed by Lewinnek et al. (1978), and are summarized in Table 7 (see Supplementary data). Biedermann et al. (2005) (transgluteal approach) found a statistically significant reduction in dislocation risk for 35–55 degrees of inclination and 5–25 degrees of anteversion. Rittmeister and Callitsis (2006) (76% anterolateral THA) found no difference for this target range. For the posterolateral approach, Fujishiro et al. (2016) assessed 10–30 degrees of anteversion and found a statistically significant reduction in dislocation risk.
4 studies found a statistically significant reduction in cup dislocation for differing target ranges of anteversion and inclination. Biedermann et al. (2005) identified 35–55 degrees of inclination and 5–25 degrees of anteversion, Grammatopoulos et al. (2015) 27–57 degrees of inclination and −3 to 27 degrees of anteversion, and Danoff et al. (2016) identified 30–50 degrees of inclination and 10–25 degrees of anteversion Garcia-Rey and Garcia-Cimbrelo (2016) identified 2 "safe windows": (1) 35–50 degrees of inclination and 5–25 degrees of anteversion, and (2) 35–50 degrees of inclination and 15–25 degrees of anteversion. The surgical approaches were as follows: posterolateral (Garcia-Rey and Garcia-Cimbrelo 2016), posterior (Danoff et al. 2016), 74% anterolateral (Grammatopoulos et al. 2015), and anterolateral (Biedermann et al. 2005). While the target range identified by Grammatopoulos et al. (2015) was broader (± 15 degrees) than the other ranges detailed above, it nevertheless identified that extreme outliers of cup positioning from the target zone have a higher risk of dislocation.
11 studies compared the combined values of anteversion/inclination to their placement inside or outside the safe zone as described by Lewinnek et al. (1978). These findings are summarized in Table 8. Only 2 of these studies (Biedermann et al. 2005, Danoff et al. 2016) found a statistically significant reduction in postoperative dislocation by placing cups in the Lewinnek safe zone. This was compared to the 4 articles that determined that there was no significant difference between dislocating and non-dislocating hips (Leichtle et al. 2013, Grammatopoulos et al. 2015, McLawhorn et al. 2015, Opperer et al. 2016). The other articles listed in Table 8 did not verify the differences between dislocators and non-dislocators in the Lewinnek safe zone with statistical analysis. 4 studies found that there were more dislocating hips outside the Lewinnek safe zone than inside (Lewinnek et al. 1978, Masaoka et al. 2006, Grammatopoulos et al. 2015, Danoff et al. 2016). This can be compared to 7 studies that identified more dislocating THAs in the Lewinnek safe zone than there were outside it (Biedermann et al. 2005, Minoda et al. 2006, Leichtle et al. 2013, Esposito et al. 2015, McLawhorn et al. 2015, Opperer et al. 2016, Abdel et al. 2016). 1 study (McLawhorn et al. 2015) identified that a greater proportion of dislocating hips were in the safe zone (83%) compared to the non-dislocating group (53%).
Table 8.
Lewinnek safe zone analysis
| THA in safe zone (%) |
|||
|---|---|---|---|
| Article | Non-dislocating | Dislocating | p-value |
| Lewinnek et al. (1978) | 64 | 33 | NA |
| Biedermann et al. (2005) | 79 | 60 | < 0.01 |
| Masaoka et al. (2006) | NA | 40 | NA |
| Minoda et al. (2006) | 72 | 68 | NA |
| Leichtle et al. (2013) | 61 | 56 | > 0.05 |
| Esposito et al. (2015) | 60 | 54 | NA |
| Grammatopoulos et al. (2015) | 50 | 45 | 0.7 |
| McLawhorn et al. (2015) | 53 | 83 | 0.2 |
| Danoff et al. (2015) | 63.50 | 47.60 | 0.04 |
| Opperer et al. (2015) | 94.60 | 91.90 | 0.7 |
| Abdel et al. (2016) | NA | 58 | NA |
THA: total hip arthroplasty; NA: not assessed.
Moskal and Capps (2011) compared navigated and non-navigated placement of the acetabular component with regard to positioning and dislocation rate. 81% of cups placed with the navigated method landed in the Lewinnek safe zone, as compared to 63% in the non-navigated group (p < 0.001). The navigated group also had less dislocations (8/779) than the non-navigated group (17/684) (p = 0.03). Mean angles of anteversion and inclination were similar between the 2 groups (Moskal and Capps 2011).
Discussion
In this systematic review we analyzed 28 articles to identify methods for measurement of cup positioning, to determine the significance of cup malpositioning influencing dislocation rates following primary THA, and to identify proposed target zones for cup anteversion and inclination to reduce the risk of dislocation.
Issues with article appraisal and comparison were mostly limited to study design and methodology. 1 study simply identified cup version as either retro-, normo-, or anteverted, precluding statistical comparison with the other articles (Paterno et al. 1997). 10 studies that analyzed cup positioning radiographically (excluding CT measurements) did not acknowledge the use of lateral pelvic radiographs to distinguish anteversion from retroversion. Anteversion was stated to be assumed in 1 article (Garcia-Rey and Garcia-Cimbrelo 2016). Other articles stated that anteversion calculations were not performed on hips without a lateral radiograph being available (Woolson and Rahimtoola 1999, Jolles et al. 2002, Grammatopoulos et al. 2015). Future studies should follow STROBE guidelines (Von Elm et al. 2007).
5 studies included hip dysplasia cases in the sample analyzed for cup positioning vs. dislocation. This may have affected the appropriateness of angle ranges identified in the setting of non-dysplastic hip arthroplasty (Woolson and Rahimtoola 1999, Minoda et al. 2006, Rittmeister and Callitsis 2006, Jørgensen et al. 2014, Garcia-Rey and Garcia-Cimbrelo 2016), as hip dysplasia has recently been shown to affect cup positioning (Gromov et al. 2016). Of these studies, only 1 (Garcia-Rey and Garcia-Cimbrelo 2016) had greater than 5% dysplastic hip THA. A similar issue was encountered in 3 studies that did not differentiate between primary and revision arthroplasty cases in their analysis (Lewinnek et al. 1978, Pierchon et al. 1994, Timperley et al. 2016). Note that in the Lewinnek et al. (1978) study, 6 out of 9 dislocations were revision cases. While Timperley et al. (2016) identified the proportion of total cases that were primary THA, this was not specified for the dislocation or comparison groups. As primary THAs could not be differentiated from the sample provided, dislocation rate and cup positioning angles for Timperley et al. (2016) are listed in this study as a combination of primary and revision THAs. 1 study was not compared to the other articles, as the data presented indirectly compared cup positioning and dislocation rate (Moskal and Capps 2011). While that study introduced a possible confounder (navigated vs. non-navigated placement), we still found the findings to be relevant to our research question and we included them for qualitative purposes.
The issue of sufficient statistical power was also identified as a possible limitation in comparing and validating article findings. Study group size varied considerably between articles; authors with studies that have limited statistical power may have difficulty in reproducing their results with larger sample sizes. The paper by Pierchon et al. (1994) did not state the size of the patient sample from which the study groups were chosen, and so could not be assessed in this regard.
Regarding the measurement of anteversion/inclination angles, plain radiographs provide different definitions of anteversion and inclination from the anatomical definitions provided by CT. Some studies used computer processing to calculate angles of anteversion and inclination. The method for manual calculation of angles varied between articles; this was considered a possible confounder when comparing cup positioning angles and target zones between studies. For this reason, we recommend the use of standardized methodology for measurement of angles of anteversion and inclination. The use of CT is advantageous as measurements are not affected by pelvic positioning, angles can be identified more accurately (particularly anteversion) (Kalteis et al. 2006b, Ghelman et al. 2009), and additional measurements such as femoral version can be calculated. However, computational analysis of plain AP and lateral radiographs appears to be the simplest and most cost-effective method currently available. Further on, acetabular cup positioning evaluated on standardized standing AP radiographs represents functional cup positioning in the standing position and should be recommended. This is in contrast to anatomical position measured using CT and possibly altered positioning measured on supine AP and shoot-through images (Au et al. 2014, Tiberi et al. 2015).
The target zone that reduces the risk of dislocation may not necessarily reflect the best positioning for reducing other complications such as wear, impingement, and revision rates (Callanan et al. 2011). Other factors such as component sizing and pelvic tilt have been shown to influence appropriate positioning and risk of dislocation (Eilander et al. 2013, Kostensalo et al. 2013, Shon et al. 2014). Femoral version (Fujishiro et al. 2016) and combined acetabular-femoral version (Jolles et al. 2002) have also been investigated as a potential contributor to hip stability. However, these factors were beyond the scope of this review, and were therefore not investigated. Surgical approach may influence the risk of anterior and posterior dislocation; depending on the surgical approach, an alternative target zone may be recommended (Callanan et al. 2011). For example, a posterior approach would lead to soft tissue and muscular weakness at the surgical site, predisposing to posterior dislocation. Increasing anteversion in this case would theoretically reduce the chance of posterior dislocation based on the mechanics of the hip joint (Mihalko and Whiteside 2004, Biedermann et al. 2005). Several studies in this review reported lower anteversion angles in dislocating THAs performed with the posterolateral approach (Nishii et al. 2004, Kim et al. 2009, Fujishiro et al. 2016). This might suggest the need for target zones that are specific to surgical approach in THA.
Narrow target ranges or aiming for mean angles of anteversion and inclination were generally not supported statistically for reducing dislocation rate; instead, dislocations tend to increase in number at deviations further from the mean (outliers from a target range). The Lewinnek safe zone could not be justified—based on the assessments performed by 11 articles (Table 8). 4 of these articles found no statistically significant reduction in hip dislocation for cups placed in this zone, as compared to 2 articles that did find a statistically significant difference (Lewinnek et al. 1978).
5 studies were able to identify target zones for anteversion and inclination that reduced the risk of dislocation (Lewinnek et al. 1978, Biedermann et al. 2005, Grammatopoulos et al. 2015, Danoff et al. 2016, Garcia-Rey and Garcia-Cimbrelo 2016). In comparison, 4 articles identified target zones with no difference in dislocation rate. 2 of these studies identified a relatively narrow range of 10–15 degrees for cup anteversion (Dudda et al. 2010, Jørgensen et al. 2014). The other 2, while testing a broader target range, may have been limited by small sample sizes (Rittmeister and Callitsis 2006, McLawhorn et al. 2015). Given the variability in the articles, we could not identify a target zone that was in agreement across all the articles assessed. It is also important to note that a large proportion of acetabular components investigated were found to lie outside the proposed target zones. In some cases, this suggests that these target zones should be redefined—or that proposed target zones are unrealistic targets and should be expanded. Alternatively, narrow target ranges could be reproduced clinically through the advent of technologies aimed at assisting accurate cup placement. The use of CT-based or imageless navigation techniques has been associated with reduced variability in cup placement and improved placement in a predefined target zone as compared to freehand methods (Kalteis et al. 2006a, Parratte and Argenson 2007, Beckmann et al. 2009). These techniques can use patient-anatomical landmarks such as the anterior superior iliac spines and pubic tubercle to better evaluate appropriate cup positioning in the individual patient (McLawhorn et al. 2015).
In summary, our systematic review of relevant articles found that some articles showed that cup positioning had an influence on postoperative dislocation, whereas others were unable to identify such a correlation. When mean angles of anteversion and inclination were compared between dislocating and non-dislocating THAs, most of the articles did not find a statistically significant difference between these groups. Due to the variety of study designs, surgical approaches, and patient populations identified, it is difficult to draw broad conclusions regarding a definitive target zone for cup positioning in THA. The target zone for cup placement is probably influenced by several other factors, so the ideal target zone for each patient may vary depending on these factors. Placing the cup in a target zone may not eliminate the risk of dislocation, but it could possibly minimize this risk. We recommend that future studies investigating acetabular cup positioning and risk of dislocation should assess different surgical approaches separately, as surgical approach may have an influence on the optimal positioning of the acetabular component.
Supplementary data
Tables 4–7 are available as supplementary data with the online version of this article at http://dx.doi.org/10.1080/17453674.2016.1251255.
AT, KG, HM, and HH conceived the idea of this study. KS performed the literature search and collated data under the guidance of AT and KG. All the authors contributed to the interpretation of data. KS wrote the initial draft of the paper, which was subsequently revised by AT, HM, HH, and KG. All the authors approved the final manuscript.
No competing interests declared.
Supplementary Material
References
- Abdel M P, von Roth P, Jennings M T, Hanssen A D, Pagnano M W.. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 2016; 474 (2): 386–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au J, Perriman D M, Neeman T M, Smith P N.. Standing or supine x-rays after total hip replacement-when is the safe zone not safe? Hip Int 2014; 24 (6). [DOI] [PubMed] [Google Scholar]
- Beckmann J, Stengel D, Tingart M, Götz J, Grifka J, Lüring C.. Navigated cup implantation in hip arthroplasty: a meta-analysis. Acta Orthop 2009; 80 (5): 538–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bicanic G, Delimar D, Delimar M, Pecina M.. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop 2009; 33 (2): 397–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B.. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br 2005; 87 (6): 762–9. [DOI] [PubMed] [Google Scholar]
- Buckland A J, Vigdorchik J, Schwab F J, Errico T J, Lafage R, Ames C, Bess S, Smith J, Mundis G M, Lafage V.. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am 2015; 97 (23): 1913–20. [DOI] [PubMed] [Google Scholar]
- Callanan M C, Jarrett B, Bragdon C R, Zurakowski D, Rubash H E, Freiberg A A, Malchau H.. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res 2011; 469 (2): 319–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASP UK CASP Checklists. Middle Way, Oxford: Better Value Healthcare Ltd, 2013. [Google Scholar]
- Dandachli W, Ul Islam S, Richards R, Hall-Craggs M, Witt J.. The influence of pelvic tilt on acetabular orientation and cover: a three-dimensional computerised tomography analysis. Hip Int 2013; 23 (1): 87–92. [DOI] [PubMed] [Google Scholar]
- Danoff J R, Bobman J T, Cunn G, Murtaugh T, Gorroochurn P, Geller J A, Macaulay W.. Redefining the acetabular component safe zone for posterior approach total hip arthroplasty. J Arthroplasty 2016; 31(2): 506–11. [DOI] [PubMed] [Google Scholar]
- Dudda M, Gueleryuez A, Gautier E, Busato A, Roeder C.. Risk factors for early dislocation after total hip arthroplasty: a matched case-control study. J Orthop Surg (Hong Kong). 2010; 18 (2): 179–83. [DOI] [PubMed] [Google Scholar]
- Eilander W, Harris SJ, Henkus H E, Cobb J P, Hogervorst T.. Functional acetabular component position with supine total hip replacement. Bone Joint J 2013; 95-B (10): 1326–31. [DOI] [PubMed] [Google Scholar]
- Esposito C I, Gladnick B P, Lee Y Y, Lyman S, Wright T M, Mayman D J, Padgett D E.. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty 2015; 30 (1): 109–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujishiro T, Hiranaka T, Hashimoto S, Hayashi S, Kurosaka M, Kanno T, Masuda T.. The effect of acetabular and femoral component version on dislocation in primary total hip arthroplasty. Int Orthop 2016; 40(4): 697–702. [DOI] [PubMed] [Google Scholar]
- Garcia-Rey E, Garcia-Cimbrelo E.. Abductor biomechanics clinically impact the total hip arthroplasty dislocation rate: a prospective long-term study. J Arthroplasty 2016; 31 (2): 484–90. [DOI] [PubMed] [Google Scholar]
- Garellick G, Karrholm J, Lindahl H, Malchau H, Rogmark C, Rolfson O. Swedish Hip Arthroplasty Register: Annual Report 2013. Goothenburg: Swedish Hip Arthroplasty Register, 2014.
- Ghelman B, Kepler C K, Lyman S, Della Valle A G.. CT outperforms radiography for determination of acetabular cup version after THA. Clin Orthop Relat Res 2009; 467 (9): 2362–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grammatopoulos G, Thomas G E, Pandit H, Beard D J, Gill H S, Murray D W.. The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Joint J 2015; 97-B(2): 164–72. [DOI] [PubMed] [Google Scholar]
- Gromov K, Greene M E, Huddleston J I, Emerson R, Gebuhr P, Malchau H, Troelsen A.. Acetabular dysplasia and surgical approaches other than direct anterior increases risk for malpositioning of the acetabular component in total hip arthroplasty. J Arthroplasty 2016; 31(4): 835–41. [DOI] [PubMed] [Google Scholar]
- Hailer N P, Weiss R J, Stark A, Kärrholm J.. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis: an analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop 2012; 83 (5): 442–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrlin K, Selvik G, Pettersson H.. Space orientation of total hip prosthesis. A method for three-dimensional determination. Acta Radiol Diagn (Stockh) 1986; 27 (6): 619–27. [DOI] [PubMed] [Google Scholar]
- Higa M, Tanino H, Abo M, Kakunai S, Banks S A.. Effect of acetabular component anteversion on dislocation mechanisms in total hip arthroplasty. J Biomech 2011; 44 (9): 1810–3. [DOI] [PubMed] [Google Scholar]
- Jolles B M, Zangger P, Leyvraz P F.. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 2002; 17 (3): 282–8. [DOI] [PubMed] [Google Scholar]
- Jørgensen C C, Kjaersgaard-Andersen P, Solgaard S, Kehlet H.. Hip dislocations after 2,734 elective unilateral fast-track total hip arthroplasties: incidence, circumstances and predisposing factors. Arch Orthop Trauma Surg 2014; 134 (11): 1615–22. [DOI] [PubMed] [Google Scholar]
- Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J.. Imageless navigation for insertion of the acetabular component in total hip arthroplasty. Bone Joint J 2006a; 88 (2): 163–7. [DOI] [PubMed] [Google Scholar]
- Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J.. Position of the acetabular cup—accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006b; 58 (2): 294–300. [DOI] [PubMed] [Google Scholar]
- Kanawade V, Dorr L D, Wan Z.. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am 2014; 96 (12): 978–86. [DOI] [PubMed] [Google Scholar]
- Kelmanovich D, Parks M L, Sinha R, Macaulay W.. Surgical approaches to total hip arthroplasty. J South Orthop Assoc. 2003; 12 (2): 90–4. [PubMed] [Google Scholar]
- Kennedy J G, Rogers W B, Soffe K E, Sullivan R J, Griffen D G, Sheehan L J.. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty 1998; 13 (5): 530–4. [DOI] [PubMed] [Google Scholar]
- Khatod M, Barber T, Paxton E, Namba R, Fithian D.. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res 2006; 447: 19–23. [DOI] [PubMed] [Google Scholar]
- Kim Y H, Choi Y, Kim J S.. Influence of patient-, design-, and surgery-related factors on rate of dislocation after primary cementless total hip arthroplasty. J Arthroplasty 2009; 24 (8): 1258–63. [DOI] [PubMed] [Google Scholar]
- Kostensalo I, Junnila M, Virolainen P, Remes V, Matilainen M, Vahlberg T, Pulkkinen P, Eskelinen A, Mäkelä KT.. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop 2013; 84 (4): 342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leichtle U G, Leichtle C I, Taslaci F, Reize P, Wunschel M.. Dislocation after total hip arthroplasty: risk factors and treatment options. Acta Orthop Traumatol Turc 2013; 47 (2): 96–103. [DOI] [PubMed] [Google Scholar]
- Lembeck B, Mueller O, Reize P, Wuelker N.. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop 2005; 76 (4): 517–23. [DOI] [PubMed] [Google Scholar]
- Lewinnek G E, Lewis J L, Tarr R, Compere C L, Zimmerman J R.. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978; 60 (2): 217–20. [PubMed] [Google Scholar]
- Li E, Meding J B, Ritter M A, Keating E M, Faris P M.. The natural history of a posteriorly dislocated total hip replacement. J Arthroplasty 1999; 14 (8): 964–8. [DOI] [PubMed] [Google Scholar]
- Lindberg H O, Carlsson A S, Gentz C F, Pettersson H.. Recurrent and non-recurrent dislocation following total hip arthroplasty. Acta Orthop Scand 1982; 53 (6): 947–52. [DOI] [PubMed] [Google Scholar]
- Mahomed N N, Barrett J A, Katz J N, Phillips C B, Losina E, Lew R A, Guadagnoli E, Harris WH, Poss R, Baron JA.. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 2003; 85-A (1): 27–32. [DOI] [PubMed] [Google Scholar]
- Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D.. Study of hip joint dislocation after total hip arthroplasty. Int Orthop 2006; 30 (1): 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masonis J L, Bourne R B.. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res 2002; 405: 46–53. [DOI] [PubMed] [Google Scholar]
- McCollum D E, Gray W J.. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res 1990; (261): 159–70. [PubMed] [Google Scholar]
- McLaren R H. Prosthetic hip angulation. Radiology 1973; 107 (3): 705–6. [DOI] [PubMed] [Google Scholar]
- McLawhorn A S, Sculco P K, Weeks K D, Nam D, Mayman D J.. Targeting a new safe zone: a step in the development of patient-specific component positioning for total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2015; 44 (6): 270–6. [PubMed] [Google Scholar]
- Meek R M, Allan D B, McPhillips G, Kerr L, Howie C R.. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res 2006; 447: 9–18. [DOI] [PubMed] [Google Scholar]
- Mihalko W M, Whiteside L A.. Hip mechanics after posterior structure repair in total hip arthroplasty. Clin Orthop Relat Res 2004; (420): 194–8. [DOI] [PubMed] [Google Scholar]
- Minoda Y, Kadowaki T, Kim M.. Acetabular component orientation in 834 total hip arthroplasties using a manual technique. Clin Orthop Relat Res 2006; 445: 186–91. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG.. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151 (4): 264–9. [DOI] [PubMed] [Google Scholar]
- Moskal J T, Capps S G.. Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty 2011; 26 (8): 1432–7. [DOI] [PubMed] [Google Scholar]
- Murray D, Murray W. The definition and measurement of acetabular orientation. J Bone Joint Surg Br 1993; 75 (2): 228–32. [DOI] [PubMed] [Google Scholar]
- Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H.. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty 2004; 19 (2): 162–6. [DOI] [PubMed] [Google Scholar]
- Opperer M, Lee YY, Nally F, Blanes Perez A, Goudarz-Mehdikhani K, Gonzalez Della Valle A.. A critical analysis of radiographic factors in patients who develop dislocation after elective primary total hip arthroplasty. Int Orthop 2016; 40(4): 703–8. [DOI] [PubMed] [Google Scholar]
- Pagnano W, Hanssen A D, Lewallen D G, Shaughnessy W J.. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am 1996; 78 (7): 1004–14. [DOI] [PubMed] [Google Scholar]
- Parratte S, Argenson J-NA.. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. J Bone Joint Surg Am 2007; 89 (3): 494–9. [DOI] [PubMed] [Google Scholar]
- Paterno S A, Lachiewicz PF, Kelley S S.. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am 1997; 79 (8): 1202–10. [DOI] [PubMed] [Google Scholar]
- Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A.. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br 1994; 76 (1): 45–8. [PubMed] [Google Scholar]
- Pollard J A, Daum W J, Uchida T.. Can simple radiographs be predictive of total hip dislocation? J Arthroplasty 1995; 10 (6): 800–4. [DOI] [PubMed] [Google Scholar]
- Rittmeister M, Callitsis C.. Factors influencing cup orientation in 500 consecutive total hip replacements. Clin Orthop Relat Res 2006; 445: 192–6. [DOI] [PubMed] [Google Scholar]
- Sculco P K, McLawhorn A S, Carroll K M, McArthur B A, Mayman D J.. Anteroposterior radiographs are more accurate than cross-table lateral radiographs for acetabular anteversion assessment: a retrospective cohort study. HSS J 2016; 12 (1): 32–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shon W Y, Sharma V, Keon O J, Moon J G, Suh D H.. Can pelvic tilting be ignored in total hip arthroplasty? Int J Surg Case Rep 2014; 5 (9): 633–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock K A.. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res 2005; 438: 182–90. [DOI] [PubMed] [Google Scholar]
- Tiberi J V, Antoci V, Malchau H, Rubash H E, Freiberg A A, Kwon Y-M.. What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? J Arthroplasty 2015; 30 (9): 1555–60. [DOI] [PubMed] [Google Scholar]
- Timperley A J, Biau D, Chew D, Whitehouse S L.. Dislocation after total hip replacement: there is no such thing as a safe zone for socket placement with the posterior approach. Hip Int 2016; 26(2): 121–7. [DOI] [PubMed] [Google Scholar]
- Von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche PC, Vandenbroucke J P, Initiative S.. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med. 2007; 45 (4): 247–51. [DOI] [PubMed] [Google Scholar]
- Wan Z, Malik A, Jaramaz B, Chao L, Dorr L D.. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res 2009; 467 (1): 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo R Y, Morrey B F.. Dislocations after total hip arthroplasty. J Bone Joint Surg Am 1982; 64 (9): 1295–306. [PubMed] [Google Scholar]
- Woolson S T, Rahimtoola Z O.. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty 1999; 14 (6): 662–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.