Abstract
Background
The number of Medicaid beneficiaries has increased under the Affordable Care Act (ACA), improving access to solid organ transplantation in this disadvantaged patient cohort. It is unclear what impact Medicaid expansion will have on transplant outcomes. We performed a retrospective cohort analysis to measure the frequency and variation in Medicaid transplantation, and post-transplant survival in Medicaid patients.
Study Design
Adult heart, lung, liver, and renal transplant recipients between 2002 and 2011 (n=169,194) reported to the Scientific Registry of Transplant Recipients were identified. Transplant recipients were classified based on insurance status (Private, Medicare or Medicaid). Outcome measures included five-year post-transplant survival, summarized using Kaplan-Meier curves and compared with log-rank tests. Organ-specific Cox proportional hazards models were used to adjust for donor and recipient factors.
Results
Medicaid patients comprised 8.6% of all organ transplant recipients. Fewer transplants were performed than expected among Medicaid beneficiaries for all organs but liver [Observed/Expected ratios (95% CI): liver=1.21 (0.68, 1.90); heart=0.89 (0.44, 1.49); lung=0.57 (0.22, 1.06); renal=0.32 (0.08, 0.72)]. Medicaid transplant recipients were listed with more severe organ failure and experienced shorter transplant wait times. Post-transplant survival was lower in Medicaid patients compared to Private insurance for all organs. Post-transplant survival in Medicaid patients was similar to Medicare patients for heart, liver and renal but lower in lung.
Conclusions
Medicaid organ transplant beneficiaries had significantly lower survival compared to Privately insured beneficiaries. The more severe organ failure among Medicaid beneficiaries at the time of listing suggested a pattern of late referral, which may account for worse outcomes. Implementation of the ACA affords the opportunity to develop the necessary infrastructure to ensure timely transplant referrals and improve long-term outcomes in this vulnerable population.
Precis
Medicaid beneficiaries have a lower survival compared to private insurance and Medicare recipients for all organ transplants. Implementation of the Affordable Care Act provides the opportunity to explore strategies for developing the infrastructure required to ensure timely transplant referrals and improve long-term, post-transplant care in this vulnerable population.
INTRODUCTION
Affordable Care Act (ACA) implementation has significantly increased the number of Medicaid beneficiaries in the US. Current estimates suggest 50% of uninsured Americans have or will gain coverage via Medicaid Expansion. (1–4) For the 31 states adopting Medicaid expansion, financial eligibility requirements decreased to 138% of the federal poverty level resulting in 12.3 million new Medicaid beneficiaries. (1–4) Overall uninsured rates have decreased from 15.7% prior to ACA to now 9.2%. (1–4) Access to solid organ transplantation has thus increased for this previously disadvantaged population. However, it is unclear what impact, if any, implementation of the ACA Medicaid expansion program will have on transplant outcomes.
Non-Private insurance status has been demonstrated to be an adverse marker of transplant outcomes across solid organ transplantation. (5–13) With introduction of the ACA, there will be more Medicaid beneficiaries who can access organ transplantation, and given prior reports of inferior outcomes among this population, (5, 7–9) transplant centers may encounter observed survival rates significantly lower than expected. In the context of the current regulatory environment, understanding the impact of implementation of the ACA on transplant outcomes is of paramount importance.
To this end, we performed a retrospective cohort analysis of solid organ transplant recipients. Our approach was to examine recent historical transplant outcomes data in Medicaid, Medicare and Private insured recipients. Outcome measures include: 1) frequency of Medicaid transplantation across organ groups; 2) variation in Medicaid transplantation in the United States; and 3) post-transplant survival among Medicaid beneficiaries compared to patients with Private insurance or Medicare.
METHODS
Data Source
This study used data from the Scientific Registry of Transplant Recipients (SRTR). The SRTR system includes data, submitted by the members of the Organ Procurement and Transplantation Network, on all donors, waitlisted candidates, and transplant recipients in the United States. The Health Resources and Services Administration of the U.S. Department of Health and Human Services provides the oversight to the activities of the Organ Procurement and Transplantation Network and SRTR contractors. The University of Alabama at Birmingham Institutional Review Board reviewed and approved the study (#E121024003).
Study Population
Deceased donor, adult heart, lung, liver, and renal transplant recipients reported to the SRTR between January 1, 2002 and December 31, 2011 were identified [heart: 17,239; lung: 13,206; liver: 48,201; renal: 90,548]. This time interval pre-dates implementation of the ACA. (Table 1)
Table 1.
Baseline Characteristics of Heart, Lung, Liver, and Renal transplant Recipients (2002–2011) Stratified by Public Insurance, Medicare, or Medicaid.
| Characteristic | Total | Private | Medicare | Medicaid | p Value |
|---|---|---|---|---|---|
| Sample size, n | 169,194 | 74,800 | 79,803 | 14,591 | |
| Organ type, n (%) |
|||||
| Liver | 48,201 (28.5) | 30,941 (41.4) | 10,158 (12.7) | 7,102 (48.7) | <.001 |
| Renal | 90,548 (53.5) | 25,970 (34.7) | 60,217 (75.5) | 4,361 (29.9) | |
| Heart | 17,239 (10.2) | 9,925 (13.3) | 5,157 (6.5) | 2,157 (14.8) | |
| Lung | 13,206 (7.8) | 7,964 (10.6) | 4,271 (5.4) | 971 (6.7%) | |
| Age, y, mean (SD) |
52.2 (12.3) | 51.9 (11.0) | 53.6 (13.1) | 46.6 (12.9) | <.001 |
| Female sex, n (%) |
61,978 (36.6) | 25,817 (34.5) | 30,179 (37.8) | 5,982 (41.0) | <.001 |
| Race/Ethnicity, n (%) |
|||||
| Caucasian | 101,081 (59.7) | 53,303 (71.3) | 40,689 (51.0) | 7,089 (48.6) | <.001 |
| African American |
37,366 (22.1) | 10,963 (14.6) | 23,260 (29.1) | 3,143 (21.5) | |
| Asian | 7,941 (4.7) | 3,429 (4.6) | 3,630 (4.6) | 882 (6.1) | |
| Hispanic | 20,449 (12.1) | 6,367 (8.5) | 10,870 (13.6) | 3,212 (22.0) | |
| Other | 2,355 (1.4) | 738 (1.0) | 1,353 (1.7) | 264 (1.8) | |
| BMI, units, mean (SD)* |
27.6 (6.6) | 27.5 (7.0) | 27.7 (6.2) | 27.0 (6.1) | <.001 |
| Education† | |||||
| Less than high school |
8,781 (6.3) | 1,839 (3.0) | 5,383 (8.0) | 1,559 (13.4) | <.001 |
| High school | 66,226 (47.3) | 25,292 (41.3) | 34,084 (50.7) | 6,850 (58.9) | |
| Some college | 34,059 (24.3) | 16,157 (26.4) | 15,174 (23.4) | 2,188 (18.8) | |
| ≥ 4yrs college | 30,978 (22.1) | 17,906 (29.3) | 12,033 (17.9) | 1,039 (8.9) | |
| Diabetes* | 49,111 (29.1) | 19,107 (25.6) | 26,484 (33.2) | 3,520 (24.2) | <.001 |
| HTN† | 89,637 (59.1) | 30,810 (46.6) | 53,342 (73.5) | 5,485 (42.2) | <.001 |
| Albumin, g/dL, mean (SD)‡ |
3.8 (0.7) | 3.7 (0.7) | 3.9 (0.6) | 3.6 (0.8) | <.001 |
| Creatinine, mg/dL, mean (SD), excluding renal recipientsc |
1.12 (0.6) | 1.12 (0.6) | 1.15 (0.7) | 1.10 (0.7) | <.001 |
Missing for <10%
Missing for 10% to 20%
Missing for >20%
HTN, hypertension
Transplant recipients were classified by insurance type as Private insurance, Medicare or Medicaid based upon SRTR classifications. Insurance status was assigned based upon the patient’s primary insurance at the time of transplantation.
Outcome Ascertainment
Post-transplant survival was defined as time from transplantation to death or last follow-up, and was censored at five years post-transplant. Death dates were supplemented by information from the Centers for Medicare and Medicaid Services and the Limited Access Death Master File available from the National Technical Information Service through 2013.
Other outcomes included measures of access to transplant as a function of insurance status including observed to expected transplant ratios (O/E), waitlist time, and measures of end-stage organ disease at the time of transplant (heart status, (14) lung allocation score (LAS), (15, 16) Model for End-Stage Liver Disease (MELD), (17) and cumulative years of dialysis (18)). Expected insurance distribution for the O/E ratios were calculated using health coverage status provided by the Kaiser Family Foundation State Health Facts from 2011 at both the national and state levels, (19) and was calculated as the proportion of Medicaid patients transplanted in each organ group divided by the proportion of the population insured with Medicaid between 2010 and 2011. Other patient covariates, measured at the time of transplant, included recipient age, gender, race/ethnicity, BMI, education, select comorbidities (diabetes and hypertension), albumin, and renal function (creatinine). Additional outcome measures included post-transplant length of stay.
Statistical Analysis
Baseline characteristics among Private, Medicare and Medicaid solid organ recipients (heart, lung, liver and renal) were compared. Continuous variables were analyzed using analysis of variance (ANOVA) or Kruskal Wallis tests, and categorical variables using chi-square tests. O/E ratios, stratified by organ-specific transplant, were calculated for Private, Medicare and Medicaid insurance transplant recipients. Number of Medicaid transplants and O/E ratios were compared for all 50 States and the District of Columbia.
Survival Analysis
Patient survival was summarized using Kaplan-Meier survival curves stratified by insurance group and compared using log-rank tests. Organ-specific Cox proportional hazards models were built using a backwards step-wise selection, with p-value < 0.05 on bivariate analysis and were used to adjust for donor and recipient factors as described above, with the most parsimonious model chosen through minimization of Akaike’s Information Criteria. Although education is reported, age, race, and gender were the only sociodemographic factors considered in adjusted analyses. Recipient age, transplant year (2002–2011), BMI, albumin, and creatinine were treated as continuous covariates. Gender and race (coded as white, black, Hispanic, and other) were categorical variables. Heart status was a categorical variable while MELD and years of dialysis were continuous variables. Adjusted survival curves were generated from the fitted Cox models using the direct adjusted survivor function, (20) and proportional hazards assumptions were tested in the fitted Cox models with Schoenfeld residuals and time dependent covariates. Spline regression was used to generate time-dependent hazard ratios when the assumptions were violated for insurance status. Patients missing data for variables included in the models were excluded from adjusted analyses.
Sensitivity Analyses
Sensitivity analyses were performed for pre-emptive renal transplants (transplant prior to initiation of dialysis). This analysis was done to account for renal recipients who had no dialysis-associated morbidity. Additional models were run with the variables with significant missingness excluded, and inferences were consistent with those reported in this manuscript. Correlation between Medicaid transplant center volume and 1-year post-transplant survival was determined for all organ types using Spearman’s correlation coefficient. All of the tests were two-sided with statistical significance set at α = 0.05. Analyses were performed using SAS 9.3 (Cary, NC). Additional Supporting Information may be found in the online version of this article.
RESULTS
Study Population
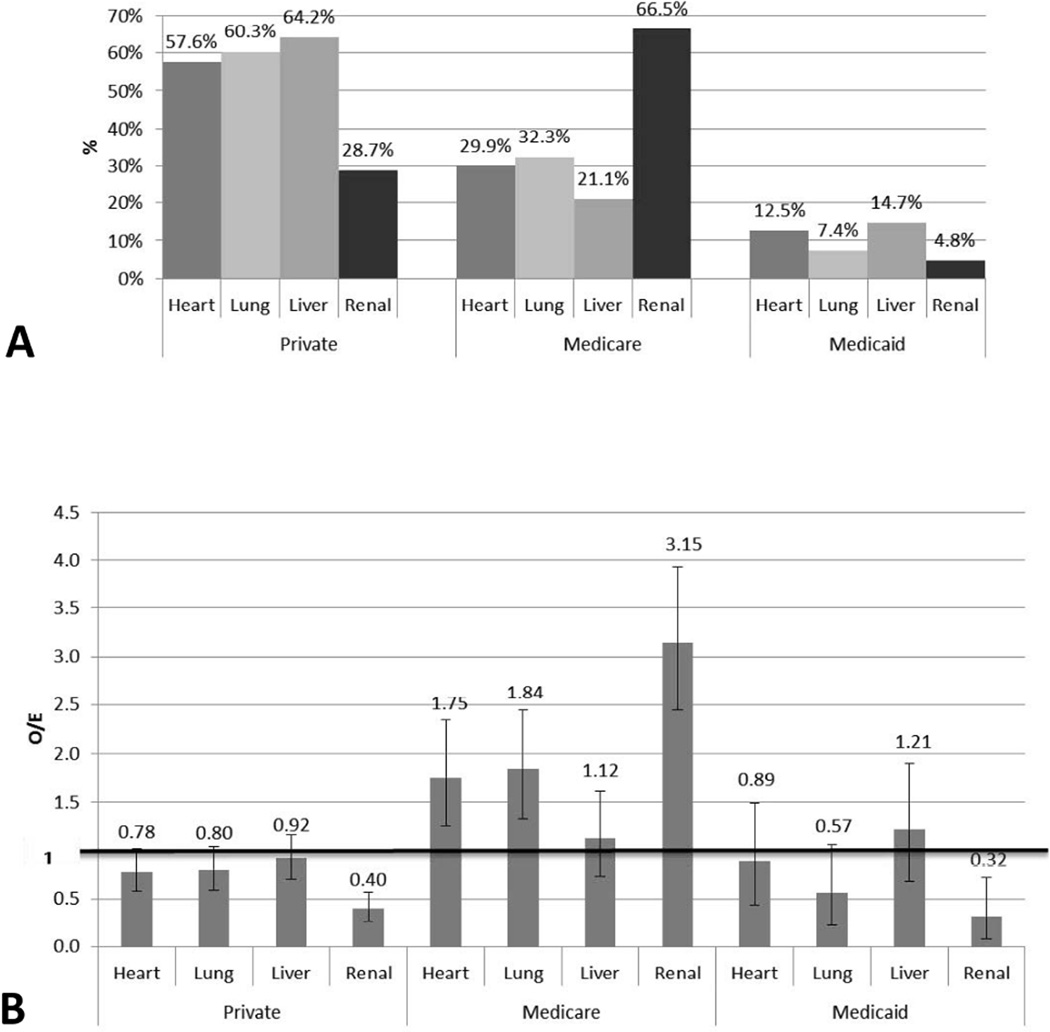
Only 8.6% of solid organ transplants were performed for patients with Medicaid insurance (Table 1). Medicaid transplant recipients were younger and more often female. Medicaid patients were more frequently non-Caucasian than Medicare and Private. Medicaid transplant recipients were less likely to have a college or beyond education than Private or Medicare recipients. The highest frequency of Medicaid transplants was performed for liver (14.7%) and heart (12.5%) with the lowest frequency performed for lung (7.4%) and renal (4.8%) (Figure 1a and Supplemental Digital Content Tables 1–4).
Figure 1.
A) Percentage of heart, lung, liver and renal transplantation stratified by organ type. The percentages were corresponds to the number of transplants performed in Medicaid patients divided by the total number of transplants performed for each organ as seen in Table 1 (ie liver transplant: 7,102/48,201× 100%). B) Observed to expected ratios for heart, lung, liver and renal transplantation stratified by insurance group.
Access to Transplant
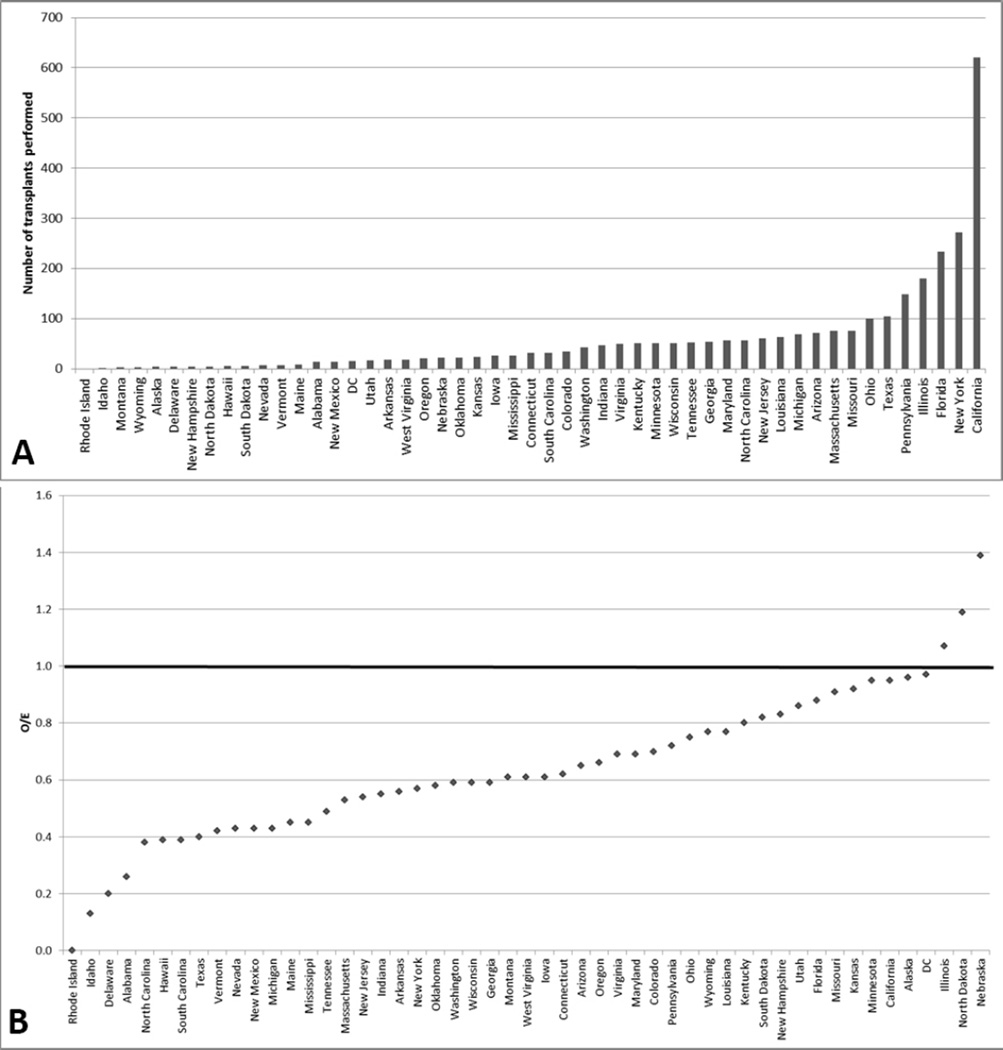
Fewer transplants were performed for Medicaid patients than was expected for all organ types but liver (Figure 1b). The O/E ratio (95%CI) for transplantation in Medicaid patients ranged from liver: 1.21 (0.68, 1.90); heart=0.89 (0.44, 1.49); lung=0.57 (0.22, 1.06); renal=0.32 (0.08, 0.72). The number of transplants performed in Medicaid patients, by state of residence, for all organ types combined, varied from 0–304 (Figure 2a, Supplemental Table 5). The O/E ratio for all organ transplantation in patients insured with Medicaid ranged from 0 to 1.4 but was only at or above 1.0 in 3 states (Figure 2b, Supplemental Table 5).
Figure 2.
A) Number of solid organ transplants performed in Medicaid patients for each State. B) Observed to expected ratios for Medicaid transplantation for each State.
Heart transplant outcomes
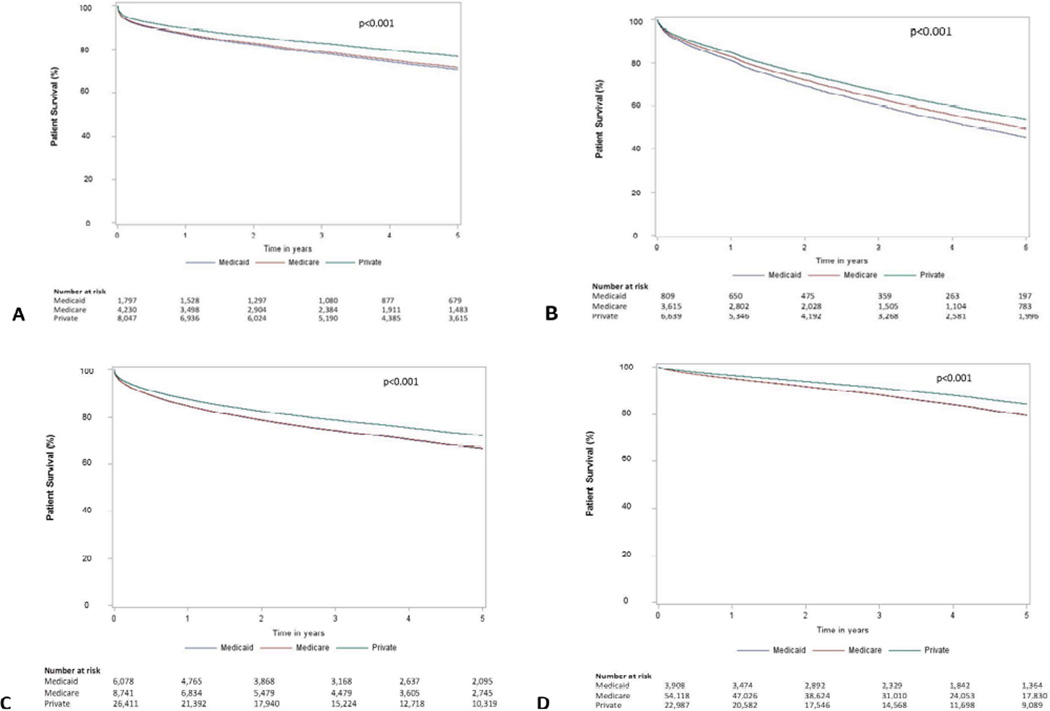
Medicaid patients receiving a heart were more likely to be transplanted as a Status 1A (46.9%), the highest-priority listing, compared to Private (44.3%) or Medicare (40.6%) patients (p<0.001, Table 2). Medicaid heart transplant recipients also had a significantly shorter wait time (66 days) compared to Private (75 days) and Medicare (91 days) patients (p<0.001). Post-heart transplant adjusted survival was lower in Medicaid patients compared to Private but similar to Medicare. (Figure 3a) Among Medicaid recipients, heart transplant survival was 0.8% lower than Medicare and 4.7% lower than Private at 3 years and 0.9% lower than Medicare and 5.9% lower than Private at 5 years. Compared to Private recipients, the adjusted Medicaid mortality HR for heart transplant was 1.10 in the first two years post-transplant (95% CI 0.97, 1.26), increasing to 1.77 after two years (95% CI 1.49, 2.09; Table 3). Similar survival hazard ratios were observed with sensitivity models that included recipient center as a covariate to control for geography. There was no significant correlation between heart transplant survival and center Medicaid volume (r=−0.137, p=0.12). Compared with non-Medicaid patients, the median length of stay was 2 days longer for heart transplant recipients with Medicaid insurance (Table 2).
Table 2.
Waiting Time, Organ-Specific Disease Score, Post-Transplant Length of Stay, and Post-Transplant Survival Stratified by Organ Type and Insurance Group.
| Variable | Total | Private | Medicare | Medicaid | p Value |
|---|---|---|---|---|---|
| Heart, n | 17,239 | 9,925 | 5,157 | 2,157 | |
| Waiting time, d, median (IQR) | 78 (23–223) | 75 (23– 209) |
91 (27–271) | 66 (20–181) | <.001 |
| Status at Tx, n (%) | |||||
| Status 1A | 7,495 (43.5) | 4,394 (44.3) |
2,090 (40.6) | 1,011 (46.9) | <.001 |
| Status 1B | 6,778 (39.3) | 3,789 (38.2) |
2,134 (41.4) | 855 (39.7) | |
| Status 2 | 2,960 (17.2) | 1,741 (17.5) |
930 (18.0) | 289 (13.4) | |
| Postop length of stay, d, median (IQR) |
14 (10–21) | 13 (10–20) | 14 (10–22) | 15 (10–22) | <.001 |
| Follow-up time, y, median (IQR) |
3.9 (1.8–5.0) | 4.0 (1.9– 5.0) |
3.1 (1.1–5.0) | 3.8 (1.8–5.0) | <.001 |
| 5-year survival, %* | 74.3 | 77.2 | 71.1 | 67.9 | <.001 |
| Lung, n | 13,206 | 7,964 | 4,271 | 971 | |
| Waiting time, d, median (IQR) | 107 (29–329.5) | 108 (30– 325.5) |
106 (28– 342.5) |
105.5 (31– 331) |
0.8 |
| LAS at Tx†, median (IQR) | 39.1 (34–48) | 39.6 (35– 49) |
38.1 (34–47) | 39.1 (34–49) | <.001 |
| Postop length of stay, d, median (IQR) |
15 (10–26) | 15 (10– 25) |
15 (10–26) | 17 (12–28) | <.001 |
| Follow-up time, y, median (IQR) |
2.7 (1.0–5.0) | 2.9 (1.1– 5.0) |
2.1 (1.0–4.3) | 2.3 (1.0–4.6) | <.001 |
| 5-year survival, %* | 52.0 | 54.9 | 47.6 | 45.0 | <.001 |
| Liver, n | 48,201 | 30,941 | 10,158 | 7,102 | |
| Waiting time, d, median (IQR) | 72 (15–256) | 71 (14– 248) |
90 (20–331) | 51 (10–203) | <.001 |
| MELD at Tx, median (IQR) | 19 (14–27) | 19 (13–27) | 18 (13–25) | 21 (15–30) | <.001 |
| Postop length of stay, d, median (IQR) |
10 (7–17) | 10 (7–16) | 10 (7–18) | 11 (8–19) | <.001 |
| Follow-up time, y, median (IQR) |
3.1 (1.1–5.0) | 3.5 (1.3– 5.0) |
3.0 (1.0–5.0) | 3.0 (1.1–5.0) | <.001 |
| 5-year survival, %* | 70.1 | 72.3 | 64.8 | 67.6 | <.001 |
| Renal, n | 90,548 | 25,970 | 60,217 | 4,361 | |
| Waiting time, d, median (IQR) | 704 (302–1222) | 527 (223– 956) |
778 (351– 1314) |
799 (326– 1441) |
<.001 |
| Dialysis time, y, median (IQR) | 3.2 (1.5–5.2) | 1.8 (0.5– 3.1) |
3.8 (2.2–5.7) | 3.9 (1.9–6.4) | <.001 |
| Postop length of stay, d, median (IQR) |
6 (5–9) | 5 (4–8) | 6 (5–9) | 6 (5–9) | <.001 |
| Follow-up time, y, median (IQR) |
3.7 (1.9–5.0) | 4.0 (2.0– 5.0) |
3.4 (1.8–5.0) | 3.8 (1.9–5.0) | <.001 |
| 5-year survival, %* | 80.2 | 84.6 | 78.0 | 82.9 | <.001 |
Estimated 5-year survival (unadjusted) calculated via Kaplan Meier methods and compared using Log Rank test
LAS missing for 50% prior to implementation in 2006
Tx, transplant; IQR, interquartile range; LAS, lung allocation score; MELD, Model for End-Stage Liver Disease
Figure 3.
Direct adjusted survivor functions for A) heart, B) lung, C) liver, and D) renal transplant recipients stratified by insurance type.
Table 3.
Multivariable Analysis of Mortality Risk Factors after Transplantation Stratified by Organ Type.
| Organ type | aHR | 95% CI | p Value |
|---|---|---|---|
| Heart* | |||
| Within 2 years | |||
| Medicare vs private | 1.18 | 1.07–1.30 | <.001 |
| Medicaid vs private | 1.10 | 0.97–1.26 | 0.15 |
| After 2 years‖ | |||
| Medicare vs private | 1.39 | 1.20–1.60 | <.001 |
| Medicaid vs private | 1.77 | 1.49–2.09 | <.001 |
| Lung† | |||
| Within 2 years | |||
| Medicare vs private | 1.10 | 1.01–1.19 | 0.03 |
| Medicaid vs private | 1.15 | 1.00–1.33 | 0.05 |
| After 2 years‖ | |||
| Medicare vs private | 1.18 | 1.06–1.31 | 0.004 |
| Medicaid vs private | 1.44 | 1.20–1.72 | <.001 |
| Liver‡ | |||
| Medicare vs private | 1.24 | 1.18–1.30 | <.001 |
| Medicaid vs private | 1.25 | 1.18–1.32 | <.001 |
| Renal§ | |||
| Medicare vs private | 1.36 | 1.30–1.42 | <.001 |
| Medicaid vs private | 1.37 | 1.24–1.51 | <.001 |
adjusted for recipient age, race, gender, heart status, diabetes, hypertension, albumin, creatinine, and transplant year
adjusted for recipient age, race, gender, hypertension, albumin, creatinine, and transplant year
adjusted for age, race, gender, diabetes, hypertension, MELD, and transplant year
adjusted for age, race, gender, years on dialysis, diabetes, hypertension, creatinine, and transplant year
Model splined at 2 years post-transplant to account for violation of the proportional hazards assumption by the Medicare variable. Patients contributed time at risk for the first 2 years at which point they were censored if they were still alive. Those patients who died within 2 years only contributed time-at-risk until death date and were not included in the post-2 year estimate of risk. The post-2 year estimate includes only those who survived for more than 2 years post-transplant with time at risk beginning at 2 years and continuing until death or 5 years post-transplant.
aHR, adjusted hazard ratio
Lung transplant outcomes
The LAS, a priority lung listing score, for Medicaid recipients (39.1) was less than Private (39.6) but more than Medicare (38.1) patients at the time of transplantation (Table 2). There was no difference in waiting time between insurance cohorts for lung transplants (p=0.8). Post-lung transplant adjusted survival in Medicaid recipients was significantly worse compared to Medicare and Private insurance recipients (Figure 3b). Among Medicaid recipients, post-lung transplant survival was 3.3% lower than Medicare and 6.7% lower than Private at 3 years and 3.8% lower than Medicare and 8.0% lower than Private at 5 years. Compared to Private, the adjusted Medicaid mortality HR for lung transplant was 1.15 within the first two years post-transplant (95% CI 1.00, 1.33), then increased to 1.44 after two years (95% CI 1.20, 1.72; Table 3). Similar survival hazard ratios were observed with sensitivity models that included recipient center as a covariate to control for geography. There was no significant correlation between lung transplant survival and center Medicaid volume (r=0.058, p=0.64). Compared with non-Medicaid patients, the median length of stay was 2 days longer for lung transplant recipients with Medicaid insurance (Table 2).
Liver transplant outcomes
The lab-MELD score, a priority liver wait listing score, was highest in Medicaid (21) compared to Private (19) and Medicare (18) patients at the time of transplantation (Table 2). Medicaid liver transplant recipients also had shorter wait times (51 days) compared to Private (71 days) and Medicare (90 days) patients. Post-liver transplant adjusted survival was lower in Medicaid patients compared to Private but similar to Medicare. (Figure 3c) Compared to Private recipients, liver transplant survival was 2.8% lower in Medicaid at 1 year, 4.5% lower at 3 years and 5.4% lower at 5 years. Compared to Private, the adjusted Medicaid mortality HR for liver transplant was 1.25 (95%CI 1.18, 1.32; Table 3). Similar survival hazard ratios were observed with sensitivity models that included recipient center as a covariate to control for geography. There was no significant correlation between liver transplant survival and center Medicaid volume (r=−0.065, p=0.48). Compared with non-Medicaid patients, the median length of stay was 1 day longer for liver transplant recipients with Medicaid insurance (Table 2).
Renal transplant outcomes
Medicaid renal transplant patients had the longest time spent on dialysis (3.9 years) compared to Private (1.8 years) and Medicare (3.8 years) patients (Table 2). Post-renal transplant adjusted survival was lower in Medicaid patients compared to Private but similar to Medicare. (Figure 3d) Compared to Private recipients, renal transplant survival for Medicaid patients was 1.4% lower at 1 year, 3.0% lower at 3 years, and 4.9% lower at 5 years. Similar survival distributions were observed when excluding pre-emptive Renal transplants. Compared to Privately insured recipients, the adjusted Medicaid mortality HR for renal transplant was 1.37 (95%CI 1.24–1.51; Table 3). Similar survival hazard ratios were observed with sensitivity models that included recipient center as a covariate to control for geography. There was a statistically significant inverse correlation between renal transplant survival and center Medicaid volume (r=−0.346, p=< 0.0001). The median length of stay was not different in Medicaid and non-Medicaid renal transplant recipients (Table 2).
Transplant outcomes in Medicaid Expansion states
Of all Medicaid transplants performed, 69.8% were among states that have implemented Medicaid expansion as of February 2015, and 30.2% were among those not currently planning to expand. Among the 31 states (including the District of Columbia) that have implemented Medicaid expansion (21), the average O/E ratio for Medicaid organ transplants was similar compared to those not planning to expand (expansion states: 0.61 vs. non-expansion states: 0.59, p=0.89). Among all organs, there was no difference in 5-year survival for Medicaid organ transplants among expansion states compared to non-expansion states (expansion states: 70.6% vs. non-expansion states: 70.4%, p=0.91). There was no difference in 5-year survival for Medicaid heart transplant (expansion states: 68.5%; non-expansion states: 67.8%, p=0.96), or Medicaid lung transplant (expansion states: 45.6% vs. non-expansion states: 42.6%, p=0.72). Five-year survival was significantly lower in Medicaid liver transplant in expansion states (expansion states: 65.7% vs. non-expansion states: 70.4%, p=0.005). There was no difference in 5-year survival in Medicaid renal transplant in expansion states (expansion states: 83.5% vs. non-expansion states: 82.1%, p=0.36).
DISCUSSION
An objective of Medicaid Expansion is to ensure access to quality, culturally competent care for vulnerable populations. (22) The Medicaid program currently provides transplant care to a diverse patient population. Despite providing transplant care to a higher proportion of vulnerable patients, there remains a large disparity in the frequency of solid organ transplantation in Medicaid patients. The O/E transplant ratio for Medicaid was <1.0 for all organ types but liver. Furthermore, only 3/50 states performed solid organ transplants at a frequency equal to the proportion of population insured by Medicaid. This is an especially alarming statistic because higher rates of organ dysfunction and failure are observed in patients with lower socioeconomic status, (23–25) the same patients who are over-represented in the Medicaid population.
Development of an infrastructure to increase timely referral as a part of the Medicaid Expansion program may improve outcomes. Currently, Medicaid transplant recipients were listed with more severe organ failure, experienced shorter transplant wait times, and longer time on dialysis, hallmarks of a pattern of late referral for transplant evaluation. It is likely that Medicaid patients in many states will be managed via some form of Managed Care Organization (MCO) in the future. (21) MCOs may reduce barriers to transplantation and increase the likelihood of early referral via prompt diagnosis and an established network of transplant providers. Earlier referral may ameliorate the advanced organ failure observed in the Medicaid population at the time of transplantation.
A second challenge for the Medicaid Expansion Program is to improve post-transplant survival outcomes. Compared to Private insurance, post-transplant survival in Medicaid patients dropped off soon after transplant and then continued to slowly diverge for all organ types. A similar survival outcome was observed for both Medicaid and Medicare patients, despite the fact that these public insurance programs cover vastly different patient populations. Medicare covers the elderly and disabled whereas Medicaid covers patients living at or near poverty. Worsened outcomes among Medicaid patients are especially disturbing given the younger age of the Medicaid cohort when compared to Medicare patients. Although Medicaid patients had higher disease severity scores at the time of transplantation, post-transplant survival was significantly reduced even when controlling for this covariate.
Studies demonstrate that adverse predictors of post-transplant survival were over-expressed in the Medicaid population, especially patients with lower education and lower social support. (7, 8, 10, 24) We expected that there would be a volume-outcome relationship, with high-volume Medicaid transplant centers having a discriminating evaluation process and/or a more rigorous infrastructure for post-transplant care. However, no statistical relationship between Medicaid transplant volume and post-transplant survival was demonstrated. There also was no statistically significant difference in post-transplant survival outcomes between states that adopted Medicaid Expansion and those that did not. Achieving good outcomes in this vulnerable population was a challenge for all centers.
It may be advisable for transplant programs to use Medicaid insurance status as a surrogate marker of poorer post-transplant survival and implement specific post-transplant care practices in an attempt to ameliorate decreased survival observed in this population. Policies that encourage more frequent long-term follow-up clinic appointments in Medicaid insured patients also might reduce the disparity in post-transplant survival outcomes. Improving long-term survival outcomes is especially important given the current practice of using measures of utility in the lung allocation system (16) and the consideration of adding utility to the renal (26) and liver (27) allocation systems. Younger Medicaid patients have high utility potential (i.e., should have more life-years gained with transplantation), but only if improved post-transplant survival rates can be achieved.
This study has several limitations inherent to retrospective analyses of large cohort studies, including limited data granularity and missingness. Not all patients were followed for 5 years for the survival analysis. Moreover, these data did not allow for a direct measure of access to transplant, as they lack referral information. A better measure of transplant access would be O/E ratio of Medicaid patients referred for transplantation, but SRTR data lack this information. These analyses utilized past Medicaid outcomes to predict how the ACA will impact transplant outcomes, although many of those gaining insurance via Medicaid expansion were previously without insurance. Although uninsured would be a better comparison group, this group has not had transplant coverage and thus outcomes in this group are not known. Furthermore, the assumption of these analyses were that past Medicaid outcomes will be predictive of future outcomes which may or may not be the case given the change in the population insured by Medicaid expansion efforts. Finally, insurance type was assigned at the time of transplantation, and it is possible that patients may have changed their insurance type during the follow-up period of the study.
CONCLUSION
A higher proportion of women and minorities with Medicaid insurance received a solid organ transplant compared to Private insurance or Medicare. However, with the exception of liver, Medicaid patients were transplanted at a much lower proportion than would be expected for all other organ groups. The ACA affords the opportunity to develop and implement strategies that will increase overall referrals and the likelihood of early referral for transplant evaluation. Moreover, current ACA implementation practices may improve Medicaid practice infrastructure to reduce the significant disparity in post-transplant survival between Medicaid and Private insurance recipients.
Supplementary Material
Acknowledgments
The University of Alabama at Birmingham Comprehensive Transplant Institute Outcomes Research Center provided methodological and statistical support. The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the Organ Procurement and Transplantation Network and the Minneapolis Medical Research Foundation as the contractor for the SRTR.
Support: This research was funded by National Institutes of Health grant numbers 1 K23 DK091514 (DD), 1 R03 DK106432 (DD), and 1 K23 DK 103918 (JL).
ABBREVIATIONS
- ACA
Affordable Care Act
- HR
Hazard Ratio
- LAS
Lung Allocation Score
- MCO
Managed Care Organization
- MELD
Model for End stage Liver Disease
- O/E
observed/ expected ratio
- p
Probability
- SRTR
Scientific Registry of Transplant Recipients
- UNOS
United Network for Organ Sharing
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Disclaimer: The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by Scientific Registry of Transplant Recipients, Organ Procurement and Transplantation Network, or the US Government.
REFERENCES
- 1.Anonymous. OBAMA CAREFACTS dispelling the myths. [Accessed December 17, 2013]; Available at: http://obamacarefacts.com/obamacares-medicaid-expansion.php. [Google Scholar]
- 2.Anonymous. About the Law. [Accessed August 18, 2014];Health and Human Services: Healthcare. Available at: http://www.hhs.gov/healthcare/rights/
- 3.Anonymous. The coverage gap: Uninsured poor adults in states that do not expand Medicaid. [Accessed October 28, 2014];Health Reform. Available at: http://kff.org/health-reform/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/ [Google Scholar]
- 4.Tavernise S, Gebeloff R. Millions of poor are left uncovered by health law. The New York Times. 2013 Oct 2; [Google Scholar]
- 5.Allen JG, Arnaoutakis GJ, Orens JB, et al. Insurance status is an independent predictor of long-term survival after lung transplantation in the United States. J Heart Lung Transplant. 2011 Jan;30(1):45–53. doi: 10.1016/j.healun.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Kemmer N, Zacharias V, Kaiser TE, Neff GW. Access to liver transplantation in the MELD era: role of ethnicity and insurance. Dig Dis Sci. 2009 Aug;54(8):1794–1797. doi: 10.1007/s10620-008-0567-5. [DOI] [PubMed] [Google Scholar]
- 7.Allen JG, Weiss ES, Arnaoutakis GJ, et al. Insurance and education predict long-term survival after orthotopic heart transplantation in the United States. J Heart Lung Transplant. 2012 Jan;31(1):52–60. doi: 10.1016/j.healun.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 8.Goldfarb-Rumyantzev AS, Koford JK, Baird BC, et al. Role of socioeconomic status in kidney transplant outcome. Clin J Am Soc Nephrol. 2006 Mar;1(2):313–322. doi: 10.2215/CJN.00630805. [DOI] [PubMed] [Google Scholar]
- 9.Yoo HY, Thuluvath PJ. Outcome of liver transplantation in adult recipients: influence of neighborhood income, education, and insurance. Liver Transpl. 2004 Feb;10(2):235–243. doi: 10.1002/lt.20069. [DOI] [PubMed] [Google Scholar]
- 10.Keith D, Ashby VB, Port FK, Leichtman AB. Insurance type and minority status associated with large disparities in prelisting dialysis among candidates for kidney transplantation. Clin J Am Soc Nephrol. 2008 Mar;3(2):463–470. doi: 10.2215/CJN.02220507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bryce CL, Angus DC, Arnold RM, et al. Sociodemographic differences in early access to liver transplantation services. Am J Transplant. 2009 Sep;9(9):2092–2101. doi: 10.1111/j.1600-6143.2009.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansen KL, Zhang R, Huang Y, et al. Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol. 2012 Sep;7(9):1490–1497. doi: 10.2215/CJN.13151211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glueckert LN, Redden D, Thompson MA, et al. What liver transplant outcomes can be expected in the uninsured who become insured via the Affordable Care Act? Am J Transplant. 2013 Jun;13(6):1533–1540. doi: 10.1111/ajt.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehra MR, Kobashigawa J, Starling R, et al. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant. 2006 Sep;25(9):1024–1042. doi: 10.1016/j.healun.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Final Rule. Department of Health and Human Services. Organ Procurement and Transplantation Network. p. Federal Register. 42 CFR-Part 121. p56649-61. [Google Scholar]
- 16.Egan TM, Kotloff RM. Pro/Con debate: lung allocation should be based on medical urgency and transplant survival and not on waiting time. Chest. 2005 Jul;128(1):407–415. doi: 10.1378/chest.128.1.407. [DOI] [PubMed] [Google Scholar]
- 17.Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001 Feb;33(2):464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 18.Meier-Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 2002 Nov 27;74(10):1377–1381. doi: 10.1097/00007890-200211270-00005. [DOI] [PubMed] [Google Scholar]
- 19.Anonymous. Health Coverage and Uninsured. [Accessed October 28, 2014];State Health Facts. Available at: http://kff.org/state-category/health-coverage-uninsured/ [Google Scholar]
- 20.Bharat Thakkar KH, Henderson WG, Oprian C. A Method to Generate Kaplan-Meier and Adjusted Survival Curves using SAS. [Accessed April 4, 2016]; Available at: http://www2.sas.com/proceedings/sugi23/Stats/p226.pdf. [Google Scholar]
- 21.Anonymous. Status of state action on the Medicaid expansion decision. [Accessed October 28, 2014];State Health Facts. Available at: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Google Scholar]
- 22.Anonymous. U.S. Department of Health and Human Services. [Accessed December 17, 2013]; Available at: http://www.hhs.gov/secretary/about/goal1.html.
- 23.Singh GK, Hoyert DL. Social epidemiology of chronic liver disease and cirrhosis mortality in the United States, 1935–1997: trends and differentials by ethnicity, socioeconomic status, and alcohol consumption. Hum Biol. 2000 Oct;72(5):801–820. [PubMed] [Google Scholar]
- 24.Foraker RE, Rose KM, Suchindran CM, et al. Socioeconomic status, Medicaid coverage, clinical comorbidity, and rehospitalization or death after an incident heart failure hospitalization: Atherosclerosis Risk in Communities cohort (1987 to 2004) Circ Heart Fail. 2011 May;4(3):308–316. doi: 10.1161/CIRCHEARTFAILURE.110.959031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volkova N, McClellan W, Klein M, et al. Neighborhood poverty and racial differences in ESRD incidence. Journal of the American Society of Nephrology : JASN. 2008 Feb;19(2):356–364. doi: 10.1681/ASN.2006080934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolfe RA, McCullough KP, Schaubel DE, et al. Calculating life years from transplant (LYFT): methods for kidney and kidney-pancreas candidates. Am J Transplant. 2008 Apr;8(4 Pt 2):997–1011. doi: 10.1111/j.1600-6143.2008.02177.x. [DOI] [PubMed] [Google Scholar]
- 27.Mulligan D. Liver Committee Chair on status of liver distribution discussion. [Accessed July 9, 2015];UNOS Transplant Pro. 2015 Available at: http://transplantpro.org/liver-committee-chair-status-liver-distribution-discussion/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.