Summary
Substantial research attention has been devoted to understanding the importance and impact of sleep in children and adolescents. Traditionally, this has focused on mean sleep variables (e.g., a child’s “typical” or average sleep duration), yet research increasingly suggests that intraindividual variability (IIV) of sleep/wake patterns (sometimes referred to as sleep variability or night-to-night variability) regularly occurs and may have implications for adjustment. A systematic search of five electronic databases identified 52 empirical studies published between 2000 and 2015 that examined correlates of sleep IIV in children and adolescents, with a recent increase in the publication rate of such studies. Identified studies were often atheoretical and included post hoc analyses, though IIV in select aspects of sleep does appear to be associated with increasing age/pubertal status, non-White race, physical and neurodevelopmental conditions (e.g., attention-deficit/hyperactivity disorder; autism), psychopathology symptoms (e.g., anxiety, depression, inattention), body weight, stress, aspects of cognitive functioning, and poorer sleep functioning/habits. The limited intervention work examining sleep IIV in adolescents is promising, though studies are needed using more rigorous intervention designs. Clinical sleep recommendations may not only need to address overall sleep duration and sleep habits but also the stability of sleep duration and timing. It will be important for future research examining sleep IIV in children and adolescents to use a developmental framework in advancing theory pertaining to the causes, mechanisms, moderators, and outcomes of sleep IIV in youth, and a conceptual model is proposed to help guide such efforts.
Keywords: ADHD, day-to-day, development, fluctuation, intraindividual, night-to-night, sleep, variability, variation, youth
Introduction
Sleep plays a crucial role in development across the life span [1–3]. Given the vast developmental changes that occur in the first two decades of life, substantial research attention has been devoted to understanding the importance and impact of sleep in children and adolescents [4–9]. The majority of this research has focused on sleep duration [10,11], and studies convincingly demonstrate that insufficient sleep is associated with adverse cognitive, behavioral, mental health, and physical health consequences in youth [4–9,12–14]. These findings have led to widely-disseminated recommendations for optimal sleep duration in children and adolescents [15], as well as policy statements regarding school start time in an effort to increase sleep duration, specifically among adolescents [16]. While important, these recommendations relate to overall nightly sleep duration and do not address daily variations in sleep. Yet research increasingly demonstrates that intraindividual variability (IIV) of sleep/wake patterns (sometimes referred to as night-to-night variability) regularly occurs and may have implications for adjustment [17–20].
Sleep IIV may be particularly common and relevant in childhood and adolescence given the rapid developmental maturation, complex familial and peer systems, and environmental demands occurring during these developmental periods [21–23], all embedded within an increasingly “24/7” lifestyle for many youth [24,25]. However, children’s sleep IIV has received relatively little attention compared to other sleep parameters, and no review has systematically identified and integrated the extant literature. This review fills that void. Following a recently-published systematic review of sleep IIV in adults, we chose to adopt the methods used by Bei et al. [26] for this review of the pediatric literature. Similar to Bei et al. [26], this systematic review aims to:
Examine the scope and characteristics of studies examining correlates of sleep IIV in children and adolescents;
Review the extent to which sleep IIV is associated with developmental and external correlates; and
Identify gaps in the literature and propose a model to guide future research.
Methods
Methods were consistent with those used by Bei and colleagues [26] as well as with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [27].
Search Strategy
Systematic searches were conducted in five databases (CINAHL, Embase, PsycINFO, PubMed, Scopus) on December 4, 2015. Filters were applied to include studies published in English on human children and adolescents ≤ 18 years old. Search terms were selected to include all of the following three components: (1) “sleep” in the title or abstract; (2) an implied presence of daily sleep measures, operationalized as containing any of the following terms in the title or abstract: “actigraph*”, “diary”, “diaries”, “log(s)”, “daily”, “everyday”, “night*”, “day*”, “week*”, “month*”; and (3) an implied examination of sleep IIV, operationalized as containing any of the following terms in the title or abstract: “variability”, “variation”, “(in)stability”, “fluctuation”, “(ir)regularity”, “(ir)regular sleep*”, “(ir)regular bedtime”, “(ir)regular rise*”.
Selection Criteria
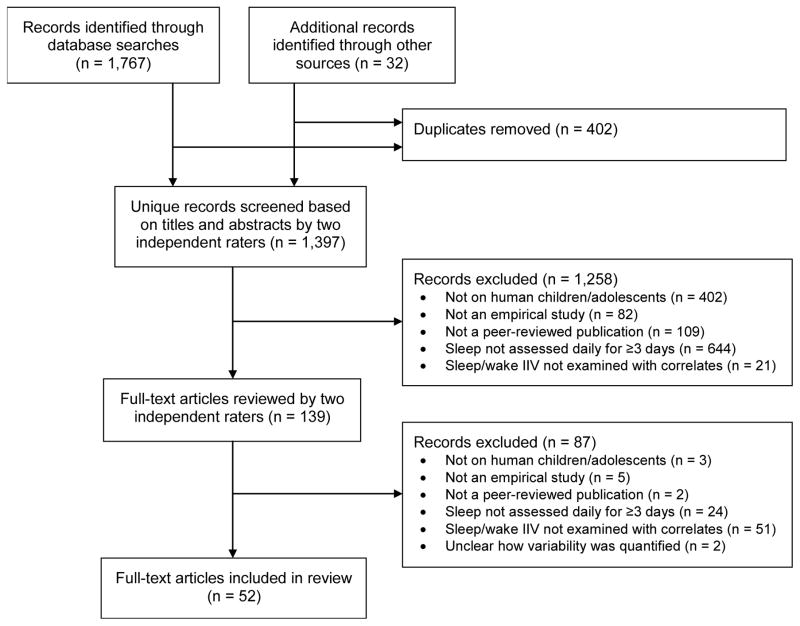
Figure 1 provides a flow diagram of the literature search and study selection process. After duplicate records were removed, two authors (SPB and CAS) independently screened each title and abstract for meeting the following inclusion criteria: (1) children or adolescents (mean age ≤ 18 years); (2) empirical study (not a review, commentary, or letter to editor); (3) peer-reviewed article; (4) assessed sleep daily for at least three days; (5) quantitatively examined sleep IIV in relation to non-sleep related factors. Disagreements regarding study eligibility were resolved by discussion. Full-texts of the remaining records were further assessed by both authors independently for inclusion eligibility, with excellent inter-rater reliability (Cohen’s kappa = 0.91). Finally, the reference lists of included studies were reviewed for potential additional papers.
Figure 1.
Flow diagram of study selection.
Note. n = number of studies, IIV = intraindividual variability.
Data Extraction and Synthesis
Based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [28], the authors developed a data extraction form to ensure systematic coding of study characteristics and quality. Two authors (SPB, CAS) independently conducted the data extraction, with a random selection of 20% of the studies extracted by both authors. Agreement between raters was excellent (95% for study characteristics, 92% for quality assessment).
Quality Assessment
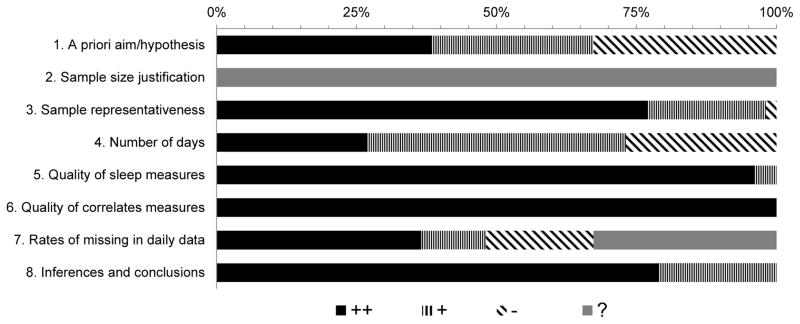
Bei et al. [26] created a study quality rating form based on the Methods Guide for Effectiveness and Comparative Effective Reviews developed by the Agency for Healthcare Research and Quality [29], and the same study quality rating form was used in this review. The study quality domains coded were: (1) having a priori aims/hypotheses regarding sleep IIV, (2) providing a justification of sample size for sleep IIV analyses, (3) sample representativeness for intended study population, (4) the number of continuous days used for evaluating sleep IIV, (5) quality of sleep measures, (6) quality of correlates measures, (7) rates of missing daily data, and (8) quality of inferences and conclusions drawn. See the caption of Figure 2 for the specific codes used for each of the study quality domains.
Figure 2.
Summary of quality assessment for included studies.
Note. 1. A priori aim/hypothesis: whether there were aims/hypotheses specific to intraindividual variability (IIV) of sleep/wake patterns; “++” indicates specific aims/hypotheses related to IIV; “+” indicates IIV implied but not explicitly stated, e.g., difference in sleep patterns; “-” indicates no aim/hypothesis specific to IIV. 2. Sample size justification: whether sample size was justified; “++” indicates justified, “+” indicates justified based on outcomes other than sleep/wake variability, “?” indicates unjustified. 3. Sample representativeness: representativeness of samples for the intended study population and for conclusions drawn, with “++”, “+”, and “-” indicating “good”, “fair”, and “poor”. 4. Number of days: the number of continuous days variability was based on; “++” indicates ≥ 14, “+” indicates ≥7 and <14, and “-” indicates <7. 5. Quality of sleep measures: “++” indicates well validated, “+” indicates not well validated. 6. Quality of correlates measured: “++” indicates well validated, “+” indicates not well validated. 7. Rates of missing in daily data: “++” indicates ≤10%, “+” indicates ≤20% and >10%, “-” indicates >20%, and “?” indicates not reported. 8. Inferences and conclusions: quality of inferences and conclusions drawn, with “++”, “+”, and “-” indicating “good”, “fair”, and “poor”.
Results
Search Results
The systematic search procedures described above resulted in 1,397 unique records for title and abstract screening. Of these, 139 records were retained for full-text screening, and 52 met full criteria for data extraction and inclusion in the review (see Figure 1).
Study Characteristics
The characteristics of included studies, in addition to findings pertaining to sleep IIV, are summarized in Table 1.
Table 1.
Characteristics of included studies and summary of study findings
| Study | Design | Sample: N, type, country |
Age range (M±SD)a |
% male | Race/ Ethnicity |
IIV method: NR of days/weeks, measures, quantification |
Theme(s) | Covariate(s) | Findings on sleep IIV |
|---|---|---|---|---|---|---|---|---|---|
| Acebo et al. (2005) [34] | Obs. | N=169; community; USA | 12–60 mths | 50% | 91% White, 6% Multiracial, 2% African American, 0.5% Asian American, 0.5% Hispanic. | ~7 days; actigraphy & diary (PR); CV based on actigraphy | A: Development B: Fam/Cultural/Environmental C: Physical |
Age, sex |
|
| Anders et al. (2011) [73] | Obs.: short-term longit. with 3 groups | T1 N=194 (AUT n=68; DD w/o AUT n=57; TYP n=69) T2 N=179 T3 N=173; clinical; USA |
T1: 2.0–5.5 (3.7±0.9) T2: 3 mths after T1 T3: 6 mths after T1 |
AUT=81 %, DD=74%, TYP=70% | White: AUT=59%, DD=47%, TYP=70%. Other races/ethnicities NR. | 7 days at each time point; actigraphy & diary (PR); ISD based on actigraphy | F: Neurodev. | Ethnicity; mother’s age, marital status, and education |
|
| Araújo et al. (2013) [64] | Obs. | N=31; school; Brazil | 10.0±1.5 | 46.2% | NR | 15 days; diary (PR); variation | E: Cognition/Learning | N/A |
|
| Bagley et al. (2015) [47] | Obs. | N=271; community; USA | 10–12.67 (11.33±7.74 mths) | 53% | 62% White, 38% Black. | ~7 days; actigraphy & diary (PR); CV based on actigraphy | B: Fam/Cultural/Environmental D: Psychosocial G: Sleep |
Sex, ethnicity, medication use, BMI |
|
| Bates et al. (2002) [52] | Obs. | N=202 (n=184 for primary analyses); low-income community; USA | 4–5 (4.9±0.51 for n=167 Head Start families; 4.9±0.71 for n=35 university preschool families) | 53% and 43% of Head Start and university preschool families, respectively | Head Start (University): 90% (86%) White, 7% (3%) African American, 3% (11%) Asian American/Other. | 4 weeks; diary (PR); squared deviation | B: Fam/Cultural/Environmental D: Psychosocial |
N/A |
|
| Bei et al. (2013) [78] | Interv.: 6-session school program | N=10 (n=9 who completed the program); school sample with self-reported poor sleep; Australia | 13–15 | 0% | NR | 7 days (immediately before and after the school term when the intervention was conducted); actigraphy; ISD | H: Intervention | N/A |
|
| Bei et al. (2014) [59] | Obs.: compare school year and vacation | N=146; community; Australia | 16.2±1.0 | 47.3% | 59.59% Australian, 26.71% Asian, 5.48% European, 2.05% African, 2.05% Middle Eastern, 4.11% Other. | 4 weeks (last week of school and the following 2 weeks of vacation, and first week of next term); actigraphy; variation | C: Physical G: Sleep |
N/A |
|
| Buckhalt et al. (2007) [36] | Obs. | N=166; community; USA | 7–11 (8.72±0.29) | 45% | 69% White, 31% Black | 7 days; actigraphy & diary (PR); CV based on actigraphy | A: Development B: Fam/Cultural/Environmental C: Physical E: Cognition/Learning |
Age, sex, puberty status |
|
| de Souza et al. (2012) [42] | Obs. | N=165; school; Brazil | Sample 1: 15±0.5 Sample 2: 15±0.6 |
Sample 1: 37% Sample 2: 43% |
NR | 7 days; diary (SR); SD | A: Development | N/A |
|
| Doane et al. (2015) [43] | Longit. | T1 N=82, T2 N=76, T3 N=71; university; USA | T1: 18.05±0.41 (spring of high school senior year); T2 5.2±0.96 mths after T1 (fall of first college year); T3 4.1±0.84 mths after T2 (spring of first college year) | T1 & T2: 24% T3: 23% |
54% White, 23% Hispanic, 13% Multiracial, 5% Black, 5% Asian American/Pacific Islander | 4 nights; actigraphy & diary (SR); ISD based on actigraphy | A: Development D: Psychosocial |
|
|
| El-Sheikh et al. (2013) [37] | Obs. | N=276; community; USA | 9.44±0.71 | 52% | 66% White, 34% Black | 7 nights; actigraphy; CV | A: Development B: Fam/Cultural/Environmental G: Sleep |
Age, single-parent household, medications, presence of asthma |
|
| Erath & El-Sheikh (2015) [45] | Longit. | N=339 (T1 N=282; T2 N=211; some additional children were recruited at T2 who did not participate at T1); community; USA | T1: 8–10 (9.42±0.71) T2: 10.42±0.67 |
T1: 46% T2: 45% |
T1: 64% White, 36% Black T2: 63% White, 37% Black |
7 nights; actigraphy; CV | B: Fam/Cultural/Environmental C: Physical G: Sleep |
Sex, race, BMI, SES, presence of asthma |
|
| Fuligni & Hardway (2006) [46] | Obs. | N=761; school; USA | “approximately 14–15 years of age” (9th grade students) | 49% | 30.0% Mexican; 4.5% Other Latino; 29.9% Chinese; 10.8% Other Asian; 17.9% White; 12.7% Other (e.g., Black, Middle Eastern); 1.3% Unknown | 14 nights; daily diary (SR); variance | B: Fam/Cultural/Environmental C: Physical G: Sleep |
Total sleep duration |
|
| Gillen-O’Neel et al. (2013) [57] | Longit. | N=535; school; USA | T1: 9th grade; 13.94–16.22 (14.88±0.39) T2: 10th grade T3: 12th grade |
47.9% | 44% Asian American; 36% Latino; 20% European American | 14 days; diary (SR); multilevel modeling | B: Fam/Cultural/Environmental | Having a test/quiz at school that day |
|
| Goodlin-Jones et al. (2008) [74] | Obs./Group | N=194 (AUT n=68; DD w/o AUT n=57; TYP n=69); clinical; USA | 2–5 (3.7±0.93) | 75% | NR (see Goodlin-Jones et al., 2009) | 7 nights; actigraphy & diary (PR); ISD based on actigraphy | F: Neurodev. | N/A |
|
| Goodlin-Jones et al. (2009) [75] | Obs./Group | N=186 (AUT n=66; DD w/o AUT n=53; TYP n=67); clinical; USA | 2–5 (3.68±0.93) | 75% | 60% White, 10% Hispanic, 3% Black, 3% Asian American, 24% Multiracial | 7 nights; actigraphy & diary (PR); ISD based on actigraphy | F: Neurodev. | N/A |
|
| Gould et al. (2000) [76] | Obs./Group | N=21 (fragile X syndrome n=13; controls n=8); clinical; Australia | Fragile X group: 4.7–11 (8.04±1.65) Control group: 6.1–11 (8.14±1.83 |
100% | NR | 14 days; diary (PR); variance | F: Neurodev. | N/A |
|
| Gruber & Sadeh (2004) [66] | Obs./Group | N=49 (ADHD n=24; controls n=24); clinical; Israel | ADHD: 7–11 (8.94±1.25) Controls: 7–10 (8.83±1.01) |
100% | NR | 5 nights; actigraphy; ISD | E: Cognition/Learning F: Neurodev. |
N/A |
|
| Gruber et al. (2000) [68] | Obs./Group | N=102 (ADHD n=38; controls n=64); clinical; Israel | ADHD: 6–14 (9.6±2.7) Controls: 7.5–11.5 (9.4±1.7) |
100% | NR | 5 nights; actigraphy and diary (SR); ISD using both actigraphy and diary (separately) | F: Neurodev. | Age |
|
| He et al. (2015) [32] | Obs. | N=305; community; USA | 16.72±2.3 | 52.46% | 78.7% White | 7 nights; actigraphy and diary (SR); ISD | C: Physical | Age, race, sex, BMI percentile, Tanner stage |
|
| He et al. (2015) [60] | Obs. | N=324; community; USA | 16.72±2.27 | 51.85% | 79.32% White | 7 nights; actigraphy and diary (SR); ISD | C: Physical | Age, sex, race, BMI percentile |
|
| Hoyniak et al. (2015) [65] | Obs. | N=15; community; USA | 2–3 (2.79±0.28) | 45% | NR | 7 days; actigraphy and diary (PR); SD based on actigraphy | E: Cognition/Learning | Age, # target trials kept, % of correct trials |
|
| Hvolby et al. (2008) [69] | Obs./Group | N=206 (n=45 with ADHD; n=64 psychiatric controls; n=97 healthy controls); clinical; Denmark | 5.75–12.33 (8.42±NR) | 74% | NR | 5 days; actigraphy and diary (PR); variance based on actigraphy | F: Neurodev. | Sex, family type |
|
| Kelly & El-Sheikh (2011) [53] | Longit. | N=176 (T2 n=142); community; USA | T1: 8.68±0.36 T2: 2 years after T1 |
44% | 69% European American; 31% African American | 7 nights; actigraphy and diary (PR); CV based on actigraphy | B: Fam/Cultural/Environmental | Sex, ethnicity, age, SES, externalizing and internalizing symptoms |
|
| Kjeldsen et al. (2014) [61] | Obs. | N=676; school; Denmark | 8–11 (~10.0±0.6) | ~52% | ~6.7% had 0 parents born in Denmark; 12.6% had 1 parent born in Denmark; 80.7% had both parents born in Denmark | 8 nights; actigraphy and diary (PR and SR); variance based on actigraphy | C: Physical G: Sleep |
Age, sex, pubertal status, height, weight, screen time, physical activity, parental education, ethnicity, mean sleep duration |
|
| Könen et al. (2015) [30] | Obs. | N=110; school; Germany | 8–11 (9.88±0.61) | 59% | NR (77% were native German-speakers) | 31 days; diary (SR); ISD & multilevel modeling | E: Cognition/Learning | N/A |
|
| Kuo et al. (2015) [48] | Longit. | N=246; community; USA | T1: 17.72±0.57 T2: 19.60±0.66 |
49% | 100% Mexican American | 7 nights; nightly phone calls at T1; variance | B: Fam/Cultural/Environmental C: Physical D: Psychosocial |
Sex, family SES |
|
| Landau et al. (2010) [67] | Obs./Group | N=44 (n=26 at familial risk for ADHD; n=18 controls); clinical; Israel | 7 weeks (45 days±0.15) | 100% | NR | 5 days; actigraphy and diary (PR); ISD using both actigraphy and diary (separately) | F: Neurodev. | Age |
|
| Marco et al. (2012) [49] | Obs. | N=155; school; USA | 12.6±0.6 (7th grade students) | 40% | 47.1% White; 24.5% Hispanic; 9% Black; 7.1% Asian; 2.6% Native American; 3.9% Other; 5.8% Unknown | 1 week; actigraphy and diary (SR); ISD using actigraphy | B: Fam/Cultural/Environmental | Sex, pubertal status, race, # of medical conditions, # of psychological conditions |
|
| McHale et al. (2011) [39] | Obs/Group | N= 469; community; USA | Older Sibling (15.7±1.6) Younger Sibling (12.8±0.58) |
49.5% | 100% Mexican American | 7 days; telephone interview (SR); sum of difference scores across nights | A: Development B: Fam/Cultural/Environmental C: Physical D: Psychosocial E: Cognition/Learning |
N/A |
|
| McHale et al. (2015) [41] | Interv.: Employee work-place interv. | N=93 (intervention n=57, control n=36); employee children; USA | BL: 9–17 (13.34±2.30) FU: 12 months later |
~50%b | 67% White; 20% Asian/Pacific Islander; 9.6% Hispanic; 1.6% Black; 1.6% Multiracial | 8 days; telephone interview (SR); ISD | A: Development B: Fam/Cultural/Environmental H: Intervention |
Income, ethnicity, workplace interv. targets, age, sex, day in study |
|
| Moore et al. (2009) [62] | Obs. | N=247; community; USA | 13–16 (13.6±0.7) | 51.4% | 54.3% non-White, 45.7% White | 5–7 days; actigraphy; ISD | C: Physical D: Psychosocial |
Age, sex, minority status, parent education, parent income, BMI, preterm status, vacation status, asthma |
|
| Moore et al. (2011) [40] | Obs. | N=247; community; USA | 12.94–16.67 (13.67±0.75) | 51.4% | 54.3% non-White, 45.7% White | 3–7 days; actigraphy; CV | A: Development B: Fam/Cultural/Environmental C: Physical F: Neurodev. |
Age, health |
|
| Moreau et al. (2014) [70] | Obs. | N=82 (ADHD n=41; controls n=41); clinical; Canada | 6–13 (ADHD: 9.7±1.7; controls: 9.6±1.6) | 58.5% | NR | 7 days; actigraphy and diary (PR); ISD based on actigraphy | F: Neurodev. | N/A |
|
| Owens et al. (2009) [71] | Obs./Group | N=125 (ADHD medication naïve n=80; controls n=45); clinical; USA | 6–14 (ADHD: 10.2±2.0; controls: 10.3±2.6) | 67% (ADHD: 77%, controls: 50%) | 84% White 16% non-White |
5–12 days; actigraphy and diary (SR&PR); ISD based on actigraphy | F: Neurodev. | N/A |
|
| Poirier & Corkum (2015) [72] | Obs./Group | N=100 (ADHD medication naïve n=50;controls n=50); clinical; USA | ADHD: 8.99±1.68; controls: 9.37±1.64 | 82% | NR | 4–7 days; actigraphy; ISD | F: Neurodev. | N/A |
|
| Sousa et al. (2007) [79] | Interv.: week-long (50 min./day) sleep hygiene program | N=58; school; Brazil | 15.98±0.93 | 22% | NR | 2 weeks each at baseline and post-intervention; diary (SR); ISD | H: Intervention | N/A |
|
| Sousa et al. (2013) [80] | Interv,: week-long (50 min./day) sleep hygiene program | N=34 (intervention n=18, control n=16); school; Brazil | (16.8±0.6) | 16% | 100% Brazilian | 7 days; diary (SR); ISD | H: Intervention | N/A |
|
| Spilsbury et al. (2004) [38] | Obs. | N=755; community; USA | 8–11 (9.5±0.8) | 50% | 64.6% White, 31.3% African American, 2.1% Biracial, 1.3% Hispanic, 0.4% Native American, 0.3% Asian | 7 days; diary (SR); CV | A: Development B: Fam/Cultural/Environmental C: Physical |
Vacation status, health problems, behavioral problems, sleep disorders, caregiver education, preterm status. |
|
| Spilsbury et al. (2005) [54] | Obs. | N=449; community; USA | 8–11 (9.5±0.9) | 50% | 53.7% White, 46.3% Black | 7 days; diary (SR); CV | B: Fam/Cultural/Environmental | Age, sex, ethnicity, preterm, health conditions, school or vacation status, caregiver education, median annual income |
|
| Spilsbury et al. (2014) [58] | Obs./Short-term longit. | T1 N=46, T2 N=33; community; USA | T1: 8–16 (11.4±2.5) T2: 3 mths. later |
43.5% | 60.9% Black, 23.9% White, 6.5% Hispanic, 8.7% Multiracial | 7 days; actigraphy and diary (SR); CV based on actigraphy | B: Fam/Cultural/Environmental | Age, sex, ethnicity, health problems, caregiver education, preterm status, income, school or vacation status, PTS sx, previous year’s exposure to violence, violence program services |
|
| Spruyt et al. (2011) [56] | Obs./Group | N=308 (normal weight n=155, overweight n=53, obese n=100); clinical; USA | 4–10 (7.2±1.3) | 49% | 71.4% White 18.8% Black 9.7% Other |
7 days; actigraphy; CV | C: Physical | Age |
|
| Spruyt et al. (2012) [31] | Obs. | N=18 (ADHD n=15; other disorders n=3); clinical (STP); USA | 9.4±1.7 | 83% | 88.9% Caucasian | 7 days; actigraphy and diary (PR); variance | B: Fam/Cultural/Environmental C: Physical G: Sleep |
N/A |
|
| Spruyt et al. (2015) [77] | Obs. | N=24; community; USA | 3–9 (5.4±1.7) | 45.8% | 100% Black | 14 days at 3 separate time points over 3 months; actigraphy; ISD | G: Sleep | N/A |
|
| Storfer-Isser et al. (2013) [55] | Obs. | N=517; community; USA | 16–19 (17.7±0.4) | 50% | 60% White 36% Black 2% Other |
5–7 days; actigraphy & diary (SR); CV based on actigraphy | B: Fam/Cultural/Environmental G: Sleep |
N/A |
|
| Suratt et al. (2007) [44] | Obs./Group | N=56 (low snore n= 20, high snore n= 36); children with adenotonsillar hypertrophy; USA | 6–12 (8.69±1.93) | 46% | 64% White 34% Black 2% Asian |
6 days; actigraphy and diary (SR), CV based on actigraphy | B: Fam/Cultural/Environmental E: Cognition/Learning G: Sleep |
Snore group status |
|
| Telzer et al. (2015) [33] | Longit. | N=48; community, USA | T1 (14.8) T2 approximately 1 year later (15.9) DTI scan 3 months later (16.4) |
44% | Not reported | 14 days at each time point; diary (SR), ISD | A: Development C: Physical G: Sleep |
Mean sleep duration & weekend-weekday sleep time difference |
|
| Tininenko et al. (2010) [51] | Obs./Group | N=79 (therapeutic foster care n=17, regular foster care n=15, low income community n=18, upper middle income community n=29); community; USA | 3–7 (5.25±1.05) | 48% | 82.3% White 7.6% Latino 6.3% Native American 3.8% Black |
5 days; actigraphy and diary (PR), ISD based on actigraphy | B: Fam/Cultural/Environmental | N/A |
|
| Troxel et al. (2014) [50] | Obs. | N=242; community; USA | 14–19 (15.7±1.3) | 47% | 57% Black 43% White |
7 days; actigraphy and diary (SR); ISD based on diary | B: Fam/Cultural/Environmental | Age, sex, BMI, depressive sx, financial strain, family conflict, parental education |
|
| Vaughn et al. (2015) [35] | Obs. | N=62; school; USA | 3–5 (4.15±0.62) | 65% | 66% White 29% Black 5% Other |
7 days; actigraphy, diary (PR); ISD based on actigraphy | A: Development B: Fam/Cultural/Environmental C: Physical D: Psychosocial E: Cognition/Learning G: Sleep |
Age, ethnicity, sex |
|
| Weiss et al. (2006) [81] | Interv.: Sleep hygiene followed by crossover melatonin trial | N=27 with ADHD and initial insomnia (>60min); clinical; Canada | 6.5–14.7 (10.29) | 90.9% | 87.9% White, 6.1% Aboriginal, 3.0% Asian, 3.0% Black | 40 days (10 baseline, 10 following sleep hygiene interv., 10 on melatonin, and 10 during placebo); actigraphy and diary (PR); ISD using both actigraphy and diary (separately) | H: Intervention | N/A |
|
| Yokomaku et al. (2008) [63] | Obs./Group | N=135 (late BTc group n=68, non-late BT group n=67); school; Japan | 4–6 (late BT=4.7±0.6; non-late BT=4.6±0.6) | 50% | 100% Japanese | 2 weeks; diary (PR); variation | D: Psychosocial G: Sleep |
N/A |
|
Note. ADHD = attention-deficit/hyperactivity disorder; ANS = automatic nervous system; AUT = autism; BMI = body mass index; BT = bedtime; CBCL = Child Behavior Checklist; Com = community sample; CPT = continuous performance test; Ctrl = control group; CV = coefficient of variance (calculated as the standard deviation of sleep duration divided by mean sleep duration); DD = developmental delay; diary = daily record such as sleep diary or sleep log; DTI = diffusion tensor imaging; FA = fractional anisotropy; Fam = Family; ICC = intraclass correlation; IIV = intraindividual variability; IQ = intelligence quotient; Interv. = intervention; ISD = individual standard deviation; longit. = longitudinal; mths = months; Neurodev. = Neurodevelopmental. ODD = oppositional defiant disorder; PR = parent-report; PSG = polysomnography; PTS = posttraumatic stress; SD = standard deviation; SE = sleep efficiency; SES = socioeconomic status; SOL = sleep onset latency; SR =self-report; STP = Summer Treatment Program (day treatment camp for children with ADHD); sx = symptoms; TIB = time-in-bed; TRF = Teacher’s Report Form; TST = total sleep time; TV = television; TYP = typically developing; TWT = total wake time; wk = week; WASO = wake after sleep onset; WISC-III = Wechsler Intelligence Scale for Children Third Edition; WM = working memory; w/o = without; WRAML = Wide Range Assessment of Memory and Learning; WT = wake time.
All ages are in years unless otherwise specified.
Text states the sample to be 47.22% male, whereas table indicates the sample to be 50.54% male.
Late bedtime defined as meeting one of the following three criteria: going out from their home with adults after 21:00hr ≥ 2 nights/week, going to bed after 23:00hr ≥4 nights/week, and returning home after 21:00hr ≥3 nights/week.
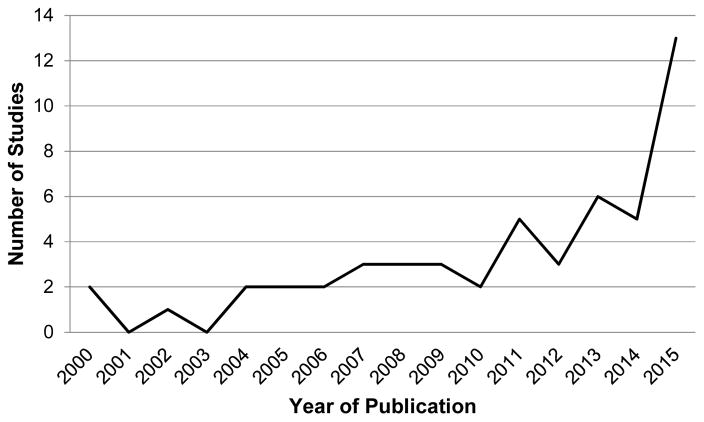
Context and Design
The 52 studies were published between 2000 and 2015. As shown in Figure 3, there has been a recent increase in the number of studies examining sleep IIV in children and adolescents, with over half (n = 27; 52%) of the identified studies published since 2012 and 25% (n = 13) of identified studies published or in-press and accessible in 2015 alone (the last year included in the systematic search). The majority of studies (n = 47; 90%) used an observational design, and five (10%) used an intervention design; no studies were identified that used an experimental design.
Figure 3.
Number of articles included in review by year of publication.
Note. One of the 2015 articles is an advance online publication awaiting pagination in a journal issue.
Characteristics of the Samples
Most studies (n = 36; 69%) were conducted in the United States in predominantly non-Hispanic White samples, with remaining studies conducted in Brazil (n = 4), Australia (n = 3), Israel (n = 3), Denmark (n = 2), Canada (n = 2), Germany (n = 1), and Japan (n = 1). The full developmental span from infancy through late adolescence was represented, including 2 studies (4%) conducted with infants/toddlers (ages 0–2 years), 9 (17%) with preschool-aged children (ages 3–5), 23 (44%) with school-aged children (ages 6–12), and 18 (35%) with adolescents (ages 13–18)1. Almost three-fourths of studies (n = 37; 71%) focused on youth from general community or school-based samples, with most other studies including youth with mental health or physical health conditions (n = 14; 27%). One intervention study recruited female adolescents with self-reported poor sleep.
Measurements and Analysis of IIV
Studies assessed daily sleep using actigraphy (n = 36), parent-completed sleep diaries (n = 19), and youth-completed sleep diaries (n = 20); studies frequently used both actigraphy and a daily sleep diary and one study used daily phone calls to the adolescent and their parent. The most common indicators for quantifying sleep IIV were individual standard deviation (ISD; n = 27; 52%) and coefficient of variance (CV; n = 13; 25%); the remaining studies used other methods such as variance and multi-level modeling.
To facilitate interpretability and readability, sleep IIV variables are described in six categories in the primary findings below: duration IIV (including sleep duration, time-in-bed, and total sleep time variables), onset IIV (including bedtime and sleep onset latency variables), waking IIV (including wake time and wake onset variables), quality IIV (including sleep efficiency, night wakings, and nocturnal movement variables), habits IIV (including sleep habits, night routines, and sleep schedule variables), and sleepiness IIV (see Table 1 for the specific methods/variables used by individual studies in assessing sleep IIV).
Quality Assessment
Study quality is summarized in Figure 2 (see Table S1 in supplement materials for the quality assessment of individual studies). Similar to the review by Bei and colleagues of sleep IIV in adults [26], 77% of studies were judged to have good sample representativeness, 79% were judged to make appropriate inferences and conclusions, 96% used well-validated measures for assessing sleep IIV, and 100% used well-validated measures for assessing correlates. Also as in adults [26], several limitations have been common in studies of sleep IIV in children and adolescents. Only 38% of studies had a priori aims or hypotheses related to sleep IIV, and no studies provided a sample size justification for analyses pertaining to IIV. Approximately one-fourth of studies (27%) examined sleep IIV based on measuring sleep for 14 or more days, and only one-third of studies (37%) had ≤ 10% of data missing.
Primary Findings
To understand correlates of sleep IIV, findings from the 52 studies were grouped into eight themes (see Table 1), recognizing that some findings could logically fit with multiple themes and that developmental context is potentially relevant across all themes. Studies could report separate findings from multiple themes. Further, in an attempt to parse out the variance specific to sleep IIV as opposed to sleep functioning more broadly, findings pertaining to sleep IIV when controlling for mean sleep indicators are described when such analyses were conducted.
Theme A: Development (n = 11)
Age (n = 11)
No studies were identified that compared sleep IIV across different age groups. Separate studies indicate that duration IIV is approximately 1 hour in school-aged children [30,31] and approximately 1.5 hours in adolescence [32,33].
Most studies examining age have examined whether sleep IIV is associated with continuously-measured age within a particular age group. Prior to adolescence, the link between age and sleep IIV is unclear. Two studies examined the relation between age and sleep IIV in preschool-aged children [34,35]. Vaughn et al. [35] found no association between age and waking IIV. In contrast, Acebo et al. [34] found greater quality IIV in 36-month-old children as compared to both younger or older children, which the authors suggest may be due to a reorganization of the sleep/wake system around three years of age. Mixed findings have also been reported in samples of school-aged children [36–38]. One study found older age to be significantly associated with both onset IIV and waking IIV [36], whereas another study found no association between age and onset IIV [37]. Another study found mixed findings across age groups depending on the child’s race and sex, with non-White boys aged 9–11 years having the greatest duration IIV [38]. Each of these studies had a restricted age span of no more than four years.
There is some evidence of an association between age and sleep IIV in adolescent samples [39–41]. In a study with older and younger adolescent siblings residing in the same family, McHale et al. [39] reported greater duration IIV in older adolescents compared to younger adolescents. Moore et al. [40] found the association between age and duration IIV to remain significant when controlling for demographic and environmental variables. Another study found adolescents to have greater onset IIV and waking IIV compared to teachers with the same morning school start time [42]. Two longitudinal studies examined sleep IIV over time in mid [33] or late [43] adolescence. Telzer et al. [33] found no difference in duration IIV or onset IIV across a single year during mid-adolescence (average ages 14.8 years to 15.9 years). In a longer longitudinal study across the transition from high school to college, there was no change in onset IIV, whereas waking IIV increased over time [43].
Pubertal status (n = 2)
Two of the studies that examined age also examined pubertal status in relation to sleep IIV [36,40]. Buckhalt et al. [36] did not find pubertal status to be related to either onset IIV or waking IIV in school-aged children. Moore et al. [40] found more advanced pubertal status during adolescence to be associated with duration IIV, but not after controlling for various demographic and environmental variables.
Theme B: Family, cultural, and environmental factors (n = 23)
Race/ethnicity (n = 9)
All nine studies examining sleep IIV in relation to race/ethnicity were conducted in the United States, where race/ethnic differences may be particularly relevant. Four studies found at least some evidence for greater sleep IIV among non-White youth as compared to White youth [36,38,40,44], whereas five studies found no race/ethnicity differences in sleep IIV [35,37,41,45,46]. The specific sleep domain examined may explain in part these conflicting findings: three of the studies that found a significant association each examined duration IIV whereas three of the studies reporting a nonsignificant association examined onset IIV [37,45] or waking IIV [35]. Thus, any association between non-White race/ethnicity and sleep IIV may be specific to sleep duration (and related measures). Importantly, one study found the association between non-White race and duration IIV to remain significant after controlling for parent education, family income, and neighborhood distress [40].
Socioeconomic status (SES) (n = 9)
Studies examining family income, income-to-needs ratio, parent education level, and SES composite indices (e.g., Hollingshead) have yielded mixed findings [34,37,39–41,45,47–49]. Of the three studies that examined family income [39–41] two found lower income to be related to greater habits IIV and duration IIV [39,40]. However, an association between lower income and greater duration IIV was no longer significant when controlling for other family and environmental factors [40]. Consistent with this latter finding, a series of studies by El-Sheikh and colleagues found income-to-needs ratio to be generally unassociated with onset IIV or habits IIV [37,45,47], though in one study family economic hardship was significantly associated with children having greater onset IIV [37]. Studies have not found an association between parent education level and children’s onset IIV [37,40] or duration IIV when controlling for other important demographic/environmental variables such as age and parent income [37,40]. Among studies that used a composite measure of SES, one did not report an association with duration IIV when the composite included family income and parent education measured five years prior to the sleep assessment [48]. In contrast, two other studies using more indicators to assess SES found lower SES to be associated with greater onset IIV and greater duration IIV [34,49]. There may be complex interrelations with other family, cultural, and environmental factors. El-Sheikh et al. [37] did not find income-to-needs ratio to be bivariately associated with onset IIV, but rather income-to-needs ratio interacted with child race in predicting onset IIV: Black children whose families were worse off financially had greater onset IIV than other Black children, whereas no significant effect was found for White children regardless of family income-to-needs ratio.
Family structure and functioning (n = 8)
Whereas El-Sheikh et al. [37] did not find single parent status to be associated with children’s onset IIV, Troxel et al. [50] found a complex association. White adolescents from two-parent homes had lower onset IIV compared to White adolescents from single-parent homes, whereas no association was found between family structure and onset IIV for Black adolescents [50]. Another study found inconsistent evidence for children in regular or therapeutic foster care to have greater or similar duration IIV, onset IIV, quality IIV, or habits IIV than children not in foster care, with findings generally indicating similar sleep IIV patterns between children in or not in foster care [51].
Family stress and conflict may be more relevant than family structure. In a study of preschool-aged children from low-income families, family stress and the impact of family stressors on the child were both associated with greater duration IIV and onset IIV, although parenting behaviors were unassociated with duration IIV or onset IIV [52]. Mixed findings were also reported in a study of adolescents, which found most family variables to be unassociated with duration IIV, although both less adolescent-father intimacy and greater adolescent-mother conflict were associated with greater duration IIV [48]. In a study of Mexican American adolescents, McHale et al. [39] found greater adolescent-parent conflict (with both mothers and fathers) to be associated with greater duration IIV. In a longitudinal study of school-aged children, marital conflict predicted greater onset IIV two years later, and onset IIV was reciprocally associated with greater marital conflict over time [53]. This study also found complex associations between marital conflict and race as well as SES in relation to onset IIV, with the association between marital conflict and greater onset IIV limited to Black children and children from lower SES backgrounds [53]. Spilsbury et al. [54] found home environment to be unassociated with duration IIV when covariates were controlled. In contrast, greater encouragement of children’s social maturity (e.g., consistent enforcement of family rules, enacting self-care routines) was associated with less duration IIV, though this association was found only for girls and not for boys [54].
Sleep environment (n = 4)
Sleep environment appears to be associated with sleep IIV [36,47,55,56]. Buckhalt et al. [36] found that sharing a bedroom, as well as a higher number of individuals sharing the child’s bedroom, is associated with greater onset IIV and greater waking IIV. Storfer-Isser et al. [55] found that a poorer sleep environment (e.g, falling asleep while listening to loud music, watching television, with lights on) was associated with greater duration IIV amongst adolescents. Spruyt et al. [56] found more adaptive bedtime routines (e.g., bedtime hugs, putting on pajamas) to be associated with less duration IIV and less quality IIV. Finally, Bagley et al. [47] found that most individual sleep environment variables (e.g., noise, uncomfortable bed) were unassociated with children’s habits IIV, with the sole exception of warmer temperature being associated with greater IIV. However, a sleep environment composite (e.g., noise, uncomfortable bed, room temperature, electronics in room) was found to be a significant intervening variable of the association between income-to-needs ratio and greater habits IIV [47].
Time spent on activities (n = 3)
How much time is spent on after-school activities is heavily influenced by family, cultural, and environmental demands and expectations, and is associated with adolescents’ duration IIV [46,48,57]. Kuo et al. [48] found more time spent with peers and less time spent at school to be associated with greater duration IIV. Fuligni and Hardway [46] similarly found that more time spent socializing with friends and playing a computer outside of school were significantly associated with greater duration IIV, whereas time spent studying, watching television, or helping the family were unassociated with duration IIV. In a longitudinal study assessing sleep on three occasions across adolescence (9th, 10th, and 12th grades), nightly increases in time spent studying outside of school was followed by shorter sleep that night, with this association increasing in strength across high school [57].
Community factors (n = 3)
Paralleling findings on families, community structure may be less linked to youth sleep IIV than community-related stress [37,40,58]. One study found community poverty to be unassociated with onset IIV [37]. Another study found more neighborhood distress to be significantly correlated with duration IIV, though this association was no longer significant when controlling for other demographic and environmental variables [40]. In a three-month longitudinal study of children exposed to violence (either intimate-partner or community violence), Spilsbury et al. [58] found that children who were physically assaulted during the violent event did not differ in duration IIV from children who were not physically assaulted. However, children who had witnessed a homicide during the violence exposure event tended to have greater duration IIV than children who did not witness a homicide during the violence exposure event [58].
Theme C: Physical factors and health (n = 18)
Sex (n = 9)
Studies have not found sex differences in sleep IIV in preschool-aged [34,35] or school-aged [36,45] children. One study spanning childhood and adolescence also found no association between sex and duration IIV [41]. There is some indication that females may have greater onset IIV [59] and greater duration IIV [46,48], though mixed findings are reported based on the specific onset IIV and duration IIV variables examined and no sex differences were found in waking IIV or quality IIV [59]. Another study also conducted with adolescents did not find any sex difference in duration IIV [60].
Body mass index (BMI), obesity, and nutrition (n = 10)
No relation was found between sleep IIV with BMI in three studies conducted with school-aged children [31,45,56]. In contrast, in a community sample of adolescents greater duration IIV was significantly associated with higher BMI, and this association remained significant when controlling for a range of other variables associated with BMI [40]. However, neither of the two studies that compared obese and non-obese youth found differences in sleep IIV [56,60], and two studies drawing from the same sample of Mexican-American adolescents did not find duration IIV to be associated with BMI [39,48].
Nevertheless, these and other studies have found sleep IIV to be associated with some adverse metabolic and nutrition outcomes. In a study of school-aged children, duration IIV was unassociated with most metabolic markers (e.g., glucose, cholesterol) but was associated with significantly higher triglyceride levels in obese children specifically [56]. Another study of school-aged children found duration IIV to be unassociated with food energy density, plasma leptin, or plasma ghrelin, but duration IIV was associated with a higher daily intake of sugar from sugar-sweetened beverages as well as greater dietary energy from added sugar, even when controlling for mean sleep duration [61]. In a sample of adolescents, greater duration IIV was associated with higher daily caloric, fat, and carbohydrate intake, but not protein intake, beyond demographic characteristics and mean sleep duration [60]. Duration IIV was also associated with greater consumption outside of meals, particularly after dinner [60]. In the same sample, duration IIV, but not mean sleep duration, was significantly positively associated with multiple abdominal obesity measures (e.g., android/gynoid fat mass ratio, visceral and subcutaneous adipose tissue, total fat area), and mediation analyses indicated that the association between duration IIV and abdominal obesity measures is accounted for in part by greater energy intake, especially from fats and carbohydrates [32]. The one study examining caffeine use did not find an association between caffeine intake and onset IIV or waking IIV [36].
Other (n = 6)
Scattered studies looked at other health outcomes. Having asthma was significantly associated with greater onset IIV in children [45] but not with duration IIV in adolescents [40]. The one study examining sleep IIV in relation to autonomic nervous system functioning did not find onset IIV to be related to respiratory sinus arrhythmia reactivity or skin conductance level reactivity [45]. One study examined adolescents’ duration IIV in relation to white matter microstructure in the brain, and found that one index of duration IIV (but not mean sleep duration) was associated with lower white matter integrity 1.5 years later [33]. Two studies examined duration IIV in relation to subjective measures of perceived physical health, with differing results. In a cross-sectional study in mid-adolescence, duration IIV was unassociated with either parent- or youth-reported perceived health [62]. In a longitudinal study in late adolescence, duration IIV at the first time-point (T1) was significantly associated with poorer self-rated physical health at the follow-up time-point approximately two years later (T2), even when controlling for sex, family SES, T1 mean sleep duration, and T1 physical health [48].
Theme D: Psychosocial, emotional, and behavioral functioning (n = 10)
Emotional functioning (n = 8)
Studies examining sleep IIV in relation to anxiety and depressive symptoms report mixed findings. In a sample of preschool-aged children, both onset IIV and waking IIV were associated with greater parent-reported internalizing problems, and onset IIV was also associated with more anxious/depressed behaviors specifically [63]. The only study conducted with school-aged children focused on pre-sleep worries and found more worrying about schoolwork (but not worries about family, friends, or other things) to be associated with greater habits IIV [47]. In adolescence, some studies report no association between duration IIV and mood [48,62]. However, two larger studies link greater duration IIV to greater adolescent anxiety/depression [39,46], even after controlling for mean nightly sleep duration and the difference between weekend and weekday sleep duration [46]. One study reported different effects based on the sleep domain examined, whereby anxiety or depression were unassociated with waking IIV concurrently or over time but did predict greater onset IIV approximately 6 months later [43]. Reciprocal associations were also found in that onset IIV predicted greater anxiety (but not depression) over time [43]. Finally, one study conducted with youth exposed to a violent event did not find an association between duration IIV and posttraumatic stress symptoms specifically [58].
Behavioral functioning (n = 6)
Studies generally report a significant association between sleep IIV and poorer behavioral functioning. In a seminal study of preschool students, Bates et al. [52] found both duration IIV and onset IIV to be associated with poorer teacher-rated preschool adjustment and behavior, whereas having a late bedtime, mean nightly sleep duration, and total daily sleep were unassociated with preschool functioning. In another preschool study, greater onset IIV was positively associated with a measure of behavioral reactivity, although waking IIV was unassociated with teacher-rated inattention problems [35]. In contrast, another study showed that preschoolers’ waking IIV, but not onset IIV, was associated with more parent-rated inattention problems, and both waking IIV and onset IIV were associated with higher parent-rated externalizing behavior problems and aggression specifically [63]. Among adolescents, one study did not find an association between duration IIV and either parent- or teacher-rated externalizing behavior problems [62]. However, a longitudinal study of Mexican-American adolescents found duration IIV to be positively associated with adolescent self-ratings of engaging in risky behavior (e.g., getting drunk/high, skipping school), both concurrently [39] and prospectively over a two-year period when controlling for baseline risky behaviors as well as mean sleep duration [48].
Social functioning (n = 2)
Both studies that examined onset IIV and waking IIV in relation to social functioning were conducted in preschool-aged children, with mixed findings [35,63]. Vaughn et al. [35] found onset IIV to be associated with children initiating more negative interactions assessed using classroom observations, but waking IIV was not associated with peer acceptance assessed using sociometric nominations and mean sleep duration was more clearly associated with preschoolers’ social functioning. Yokomaku et al. [63] found that waking IIV was associated with greater social problems and withdrawn behaviors specifically, whereas onset IIV was unassociated with social problems or withdrawal.
Theme E: Cognition and learning (n = 8)
Intellectual ability (n = 3)
Studies examining sleep IIV in relation to children’s intellectual ability report mixed findings. Araújo et al. [64] did not generally find an association between onset IIV and children’s visuospatial IQ scores. Similarly, Suratt et al. [44] did not find an association between duration IIV and children’s scores on an intelligence subtest measuring visual-construction skills, but did find greater duration IIV to be associated with poorer performance on subtests measuring word knowledge and verbal reasoning. Buckhalt et al. [36] also found waking IIV and onset IIV to be associated with lower overall IQ and onset IIV was associated with poorer verbal ability specifically, but these associations were only present for Black children and not White children.
Specific neurocognitive functions (n = 5)
Two studies examined sleep IIV in relation to preschoolers’ neurocognitive functioning [35,65]. Vaughn et al. [35] found greater waking IIV to be associated with poorer effortful control but unassociated with receptive vocabulary. Hoyniak et al. [65] did not find an association between a composite measure of sleep IIV (including duration IIV and onset IIV domains) and sustained attention, though sleep IIV was associated with longer target P3 latencies assessed with electroencephalography (EEG) which is a neurophysiological measure of attentional processing. Three studies examined sleep IIV in relation to the neurocognitive functioning of school-aged children [30,44,66]. Consistent with the findings by Hoyniak and colleagues [65], Suratt et al. [44] found no association between duration IIV and sustained attention and also found no association with working memory. Another study examining working memory found effects based on time of day, with quality IIV and duration IIV both associated with poorer working memory performance in the morning but not in the afternoon [30]. Further, children with lower overall working memory performance were particularly vulnerable to the previous night’s sleep quality, and a quadratic effect was found for duration IIV whereby morning working memory performance was poorer when sleep duration deviated from the average by either “too little” or “too much” [30]. Finally, Gruber and Sadeh [66] found greater duration IIV and quality IIV to be associated with poorer performance on complicated neurocognitive tasks requiring sustained attention for extended periods of time and working memory but not simple neurocognitive tasks requiring motor skills and short-term memory, and only for typically developing boys and not boys with attention-deficit/hyperactivity disorder (ADHD).
Academics (n = 1)
The one study examining school grades did not find an association between duration IIV and adolescents’ grades [39].
Theme F: Neurodevelopmental disorders (n = 12)
ADHD (n = 8)
One study examined sleep patterns in 7-week-old boys at familial risk for ADHD [67]. Though infants at familial risk for ADHD did not differ from comparison infants in nighttime duration IIV (i.e., 7p.m.–7a.m.), the infants at risk for ADHD did have greater daytime duration IIV (i.e., 7a.m.–7p.m.) than comparison infants [67]. Studies directly examining sleep IIV in children with ADHD compared to typically developing peers report mixed findings [66,68–72]. Gruber et al. [68] found that boys with ADHD did not differ from boys without ADHD in sleep IIV (i.e., onset IIV, duration IIV, waking IIV, sleepiness IIV) assessed with daily diaries, but boys with ADHD did have greater onset IIV and duration IIV assessed with actigraphy. Further, one index of duration IIV was better able than mean sleep variables or other sleep IIV variables to distinguish between boys with and without ADHD [68]. Other studies have found greater onset IIV in children with ADHD than in comparison children, but report mixed evidence regarding any differences between children with and without ADHD in measures of waking IIV, duration IIV, or quality IIV [66,69,70]. Hvolby et al. [69] found children with ADHD to have greater onset IIV than healthy controls as well as psychiatric controls. In contrast, two other studies did not find evidence for greater sleep IIV (i.e., duration IIV, onset IIV, or waking IIV) in children with ADHD compared to children without ADHD [71,72], and another study did not find diagnosis/medication of ADHD to be associated with adolescents’ duration IIV [40]. It is important to note, however, that one of these studies used baseline data from a medication trial during which families were asked to maintain a set bedtime, which may have impacted the ability to detect night-to-night variability [71]. In addition, the two studies that failed to find any group differences in sleep IIV in children with and without ADHD excluded children taking medication for ADHD [72] and/or with an internalizing comorbidity [71,72], which may have resulted in children with more severe ADHD being excluded from participation. Findings are mixed in whether taking medication for ADHD or having a comorbid psychiatric diagnosis impacts sleep IIV in children with ADHD [69–71].
Autism and other developmental disabilities (n = 3)
The three studies examining sleep IIV in children with autism and other developmental disabilities were drawn from the same sample of children [73–75]. An initial cross-sectional study did not find differences in sleep IIV (i.e., onset IIV, duration IIV, waking IIV, quality IIV) between children with autism, children with a developmental delay (but not autism), or typically developing children [74]. Further analyses found no differences in sleep IIV when children in these three groups were subdivided into those with and without elevated ADHD symptoms [75]. A follow-up study examined sleep IIV over a six-month period and found that children in either of the neurodevelopmental disorder groups had greater duration IIV and quality IIV than their typically developing peers, though within-child variability was greater than between-child variability for all three groups [73]. Less mature developmental age was also associated with greater waking IIV, duration IIV, and quality IIV [74].
Fragile X syndrome (n = 1)
One study found greater duration IIV, onset IIV, and duration IIV in boys with fragile X syndrome compared to control children [76].
Theme G: Sleep functioning (n = 13)
Mean sleep variables (n = 8)
Sleep IIV is generally unassociated with mean sleep variables (i.e., mean sleep duration, mean sleep quality, mean sleep latency) in preschool-aged children, aside from an association between waking IIV and greater mean sleep activity [35]. Studies examining sleep IIV and mean sleep variables in school-aged children offer mixed findings. One study found onset IIV to be associated with greater mean sleep activity, shorter mean sleep duration, and poorer mean sleep quality [36]. Other studies found onset IIV to be associated with shorter mean sleep duration but unassociated with mean sleep quality [37,45]. Duration IIV does appear to be associated with children having shorter mean sleep duration [44,61]. Likewise, greater onset IIV and duration IIV are associated with shorter mean sleep duration in adolescents [33,46].
Sleep schedule, habits, and problems (n = 8)
Onset IIV, waking IIV, and habits IIV are not associated with children’s self-reported sleep/wake problems [36,37,47]. Preschoolers with a late bedtime have greater onset IIV and waking IIV than other preschoolers [63]. School-aged children have greater duration IIV on weekends than weekdays, but greater waking variability on weekdays than weekends [77]. Similar, adolescents have greater onset IIV and waking IIV during vacation periods than school periods [59], and greater duration IIV is likewise associated with a larger difference between weekday and weekend sleep duration [33]. Adolescents with good overall sleep hygiene have less duration IIV than adolescents with poor sleep hygiene [55].
Daytime sleepiness and napping (n = 4)
Two studies did not find an association between onset IIV, waking IIV, or habits IIV and children’s daytime sleepiness [36,47]. However, the time of day when sleepiness is assessed may be important when examining associations with sleep IIV: Spruyt et al. [31] found that sleepiness rated early in the day was unassociated with duration IIV or onset IIV whereas sleepiness rated in the afternoon was associated with multiple sleep domains including greater onset IIV and greater duration IIV. There does appear to be an association between napping and greater onset IIV, waking IIV, and duration IIV [36,77].
Snoring (n = 1)
Among children with adenotonsillar hypertrophy, those who snored most nights had greater duration IIV than children who did not snore on most nights [44].
Theme H: Sleep interventions (n = 5)
Three studies have examined school-based interventions aimed at improving adolescents’ sleep functioning [78–80]. Bei et al. [78] conducted a pilot study of a six-session mindfulness-based group in nine adolescent females with self-rated poor sleep. Though some positive intervention effects were found for sleep generally, findings for sleep IIV were mixed [78]. Sousa and colleagues evaluated a one-week sleep hygiene program delivered to students in 11th [79] and 12th [80] grades. An initial open trial found reduced onset IIV following the sleep hygiene program [79], and a subsequent study found that students randomized to receive the program had less onset IIV and waking IIV following the program compared to baseline whereas no change in sleep IIV was found in the control group [80]. McHale et al. [41] examined whether a workplace intervention designed to reduce employees’ work-family conflict impacted the duration IIV of employees’ children in a group-randomized trial (work teams were randomized to intervention or usual practice conditions). No change in duration IIV was found in children whose parents received the intervention, whereas children in the control group had increased duration IIV from baseline to follow-up one year later [41]. Finally, children with ADHD and initial insomnia had decreased onset IIV following a brief sleep hygiene intervention [81]. Children who continued to have initial insomnia following the sleep hygiene intervention entered into a double-blind crossover trial of melatonin, and no difference in onset IIV was found between melatonin and placebo [81]. Of note, intervention studies examining sleep IIV in children and adolescents are largely limited by small sample sizes, short follow-up periods, lack of a randomized design, and absence of active control groups.
Discussion
Summary of Findings
Intraindividual variability (i.e., night-to-night changes within a person, rather than across people) in sleep/wake patterns is common [17,46] and may be especially characteristic of child and adolescent sleep [30,42,59,82]. However, until very recently this aspect of sleep has largely been ignored in both youth and adults, despite emerging literature suggesting that sleep IIV may be just as important as mean sleep duration [30,32,48,52,60,68]. Bei and colleagues [26] systematically reviewed the adult literature and reported sleep IIV to be related to a variety of demographic, physical, and mental health outcomes. Recognizing that sleep patterns and correlates likely differ across the developmental spectrum, this review uniquely focused on correlates of sleep IIV in children and adolescents.
Overall, effect sizes tended to be small and results were mixed across many domains. Even so, several sets of findings were more consistent and point to promising areas of investigation. First, there is greater duration IIV and onset/waking IIV with more advanced pubertal status and age, suggesting that adolescence may be a developmental period when sleep IIV may be particularly impactful [5]. The mechanisms contributing to pronounced sleep IIV in adolescence will be important to evaluate in future research. Potential mechanisms include biological changes associated with puberty and brain maturation, increased academic and extra-curricular demands, and shifting interpersonal relationships including increasing prioritization of the peer group and decreasing parental supervision/monitoring [5,6]. Interestingly, Bei and colleagues [26] found younger age to be associated with greater sleep IIV in adults. It is tempting to conclude that adolescence and early adulthood may be when sleep IIV is most prevalent. However, no published study has examined sleep IIV across the full pediatric developmental spectrum, much less the lifespan. It is thus premature to draw conclusions regarding the possibility that the prevalence and impact of sleep IIV follows an inverted U-shaped curve across the lifespan, though this possibility should be investigated in future research.
Second, sleep IIV was frequently associated with poorer behavioral functioning, including externalizing behavior, aggression, inattention, and risky behavior. These associations were largely consistent across age ranges and reporters (e.g., adolescents, parents, teachers). Intriguingly, although studies examining sleep IIV in relation to global measures of social functioning (e.g., peer acceptance, social problems) reported mixed findings, sleep IIV was associated with adolescents spending more time with their peers. Although this latter finding could be viewed as evidence of sleep IIV being associated with better peer functioning, additional studies are needed. Spending more time with friends can be a positive aspect of peer functioning and social acceptance, but those friends could engage in and encourage externalizing behaviors (e.g., delinquency, alcohol/substance use, risk-taking) that may themselves be associated with greater sleep IIV. Moreover, it is likely that associations between sleep IIV and peer functioning and associated outcomes are moderated by parental monitoring and the quality of the parent-teen relationship [83]. These considerations underscore the importance of future research considering both costs and benefits, as well as moderating factors, that may be associated with sleep IIV.
Third, several studies examined sleep environments/schedules and sleep interventions that may impact – or stabilize – sleep IIV. Similar to the findings of Bei et al. [26], less optimal sleep environments (e.g., watching TV) and less structured environmental schedules (e.g., weekends, vacation periods) were reliably found to be related to increased sleep IIV. This suggests that clinical sleep recommendations around optimizing environmental factors may both address sleep duration and stabilize sleep. Although promising, sleep intervention findings were mixed with respect to sleep IIV, perhaps due to differences in intervention types and study designs.
Finally, several other interesting and important correlates of sleep IIV were identified, although with more mixed evidence. As in the adult literature [26], studies conducted in children and adolescents indicate that sleep IIV is associated with race/ethnicity (non-White youth having greater sleep IIV), physical health conditions (conditions such as asthma associated with greater sleep IIV), body weight (higher BMI correlated with more sleep IIV in adolescents), psychopathology (greater symptom severity associated with greater sleep IIV), and worse sleep parameters (greater sleep activity and shorter sleep duration associated with greater sleep IIV). Stress also appeared to be associated with more sleep IIV in both adults and youth; however, the types of stressors differed in a developmentally consistent manner; family stress and conflict, lower family SES, and community stress were particularly salient in youth. Napping has also been examined within both youth and adults but with different correlates: daytime napping was associated with greater nighttime sleep IIV in youth, whereas daytime napping IIV was associated with younger age and self-reported health conditions in adults [26].
Several significant correlates were identified in the present review within youth, but have yet to receive empirical attention in adults. These include: ADHD (diagnosis associated with greater sleep IIV), nutrition (higher sugar, fat, carbohydrate, and daily calories associated with greater sleep IIV), aspects of intellectual functioning (lower perceptual organization and verbal comprehension associated with greater sleep IIV), complex neurocognitive tasks (poorer performance associated with more sleep IIV), developmental disability (autism and other developmental disabilities associated with greater sleep IIV), and snoring (presence of snoring associated with sleep duration IIV). In sum, in children and adolescents sleep IIV is correlated with a wide range of outcomes, though in many instances a particular outcome was examined in only a few studies, making replication in new samples an important direction for future research which should also shed light on the discrepant findings reported in studies to date.
There may be several reasons for the mixed results among studies examining sleep IIV in children and adolescents. First, some associations became nonsignificant when controlling for other factors, but not all studies included similar (or any) covariates. This suggests the potential for complex relationships and the need for more sophisticated methodological (e.g., experimental and longitudinal designs) and statistical (e.g., structural equation modeling, multilevel modeling) approaches. Likewise, studies differed in whether they controlled for mean sleep functioning variables (e.g., mean sleep duration) when examining sleep IIV in relation to external correlates. Such covariation is critical in order to evaluate whether sleep IIV is uniquely associated with adjustment above and beyond the contribution of mean sleep functioning (and vice versa). Of note, multiple studies that did control for mean sleep functioning did find unique effects for sleep IIV specifically [33,39,46,48,52,60,61]. Second, most studies examined youth within a restricted age range. Many associations (e.g., sex, BMI) were found in adolescents that were not found in younger children, further highlighting adolescence as a particularly important stage in development to examine the impact of sleep IIV. Third, significant correlates within domains often depended on the aspect of sleep variability examined (e.g., variability in duration versus timing), and many studies reported on only selected aspects of sleep IIV. Fourth, and especially relevant for adolescence [84–86], studies did not routinely specify whether sleep IIV was specific to school nights, or whether weekends or vacation/holiday periods were also included. The few studies that differentiated between school night and non-school night sleep suggest that adolescents have greater sleep IIV on weekends or during vacation periods [59,77], though the impact of this increase in sleep IIV remains unexamined and is a key direction for future research. Finally, because much of the research conducted was post hoc, it is likely that differing aspects of study designs contributed to mixed findings. For example, in regards to the relationship of sleep IIV with ADHD diagnosis, studies that excluded youth for taking medications or having comorbidities may have selected youth with less severe symptomology or less chaotic home environments, and therefore less variable sleep.
Future Directions
Theoretical Context
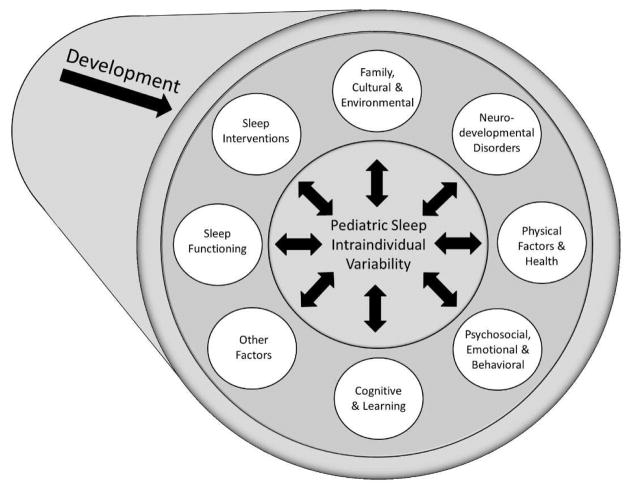
Notably lacking from the pediatric sleep IIV literature is a unifying theory to guide hypothesis-driven, systematic research. As Bei and colleagues [26] suggest, nightly variations in sleep may have a distinct etiology from an individual’s mean overall sleep and thus it is important to understand (1) factors related to sleep IIV, (2) mechanisms of such nightly variability, and (3) the directionality of these relationships, all within the context of youth development. Figure 4 depicts a proposed theoretical model to guide future research addressing these questions. The themes identified in this review establish an initial set of factors that appear to be related, potentially bidirectionally, to pediatric sleep IIV. These factors are also often interrelated in complex ways. For example, while physical health and emotional and behavioral functioning may independently be related to sleep IIV, their interrelations [87–89] suggests the need for research to consider moderating and mediating factors as well as cascading interrelations across development.
Figure 4.
Proposed theoretical model for intraindividual variability (IIV) of sleep/wake patterns in children and adolescents.
Importantly, a theoretical model of sleep IIV in youth should be considered within a developmental framework. Sleep IIV and its related factors must be regarded both within their present context and within the context of prior relevant events and milestones. Factors most salient during infancy are likely different from those in childhood and adolescence and a “one size fits all” approach is inadequate. By extension, future studies should be designed within a developmental framework and should contribute to the understanding of how sleep IIV may differ – and have a differential impact – across the developmental spectrum.
Methodological and Analytical Considerations
Correlational research is helpful, but there is evidence of bidirectional relationships in this area of research, or even cyclic relationships [90]. Directional research, including experimental work, longitudinal studies, and treatment trials, can help untangle such interrelations, inform research on underlying mechanisms, and provide critical information on the most effective and temporally critical points of intervention. More advanced statistical models also should be considered when exploring predictors or outcomes of sleep IIV. For example, more complex mediation and moderation analyses are needed to advance the theoretical framework for sleep IIV [91]. Researchers also should move toward daily-level examination of constructs. Objectively assessed sleep is almost always measured on a daily basis, yet most studies thus far report only averaged or mean variability values. Presenting the combination of averaged and daily-level statistics is appropriate to best understand the relative impact of within-person fluctuation in sleep and the relationship between constructs beyond between-person differences. Finally, likely an artifact of the post hoc nature of this research, sample size justifications and a priori power analyses were not included in studies. It is possible that some effects were nonsignificant due to being underpowered and may have contributed to mixed findings. In line with the need for systematic, hypothesis-driven research, future studies should consistently report effect sizes and whenever possible be conducted with sufficient power to detect effects. Relatedly, as discussed in Bei et al. [26], there are limitations to some of the commonly-used metrics for assessing sleep IIV (e.g., without controlling for mean sleep duration, larger variability metrics can be an artifact of larger means); the field would benefit from using more sophisticated methods that allow for computing variability in studies with small sample sizes and few measurement points [92]. Although many of the limitations in this body of research relate to the post hoc nature of studies, this is not to say these studies are not important or needed. In fact, it is likely that there are many existing datasets that have examined only mean sleep variables, and it is recommended that investigators leverage these existing datasets to further advance the study of sleep IIV.
Limitations
As also seems to be the case with adults [26] research into pediatric sleep IIV has been too heterogeneous to allow for a meta-analysis or to assess risk of reporting and publication bias. For many domains there were so few studies that it was difficult to draw conclusions. Indeed, there are developmentally-relevant outcome domains which appear not to have been studied with respect to sleep IIV at all (e.g., alcohol/substance use, delinquent behaviors, suicidality). Further, many of the included studies did not include sleep IIV as a primary focus, but happened to present relevant findings (e.g., tables showing standard deviations across different groups). Although including this information in the current review provided a more comprehensive picture of the literature, this approach may also weaken inferences. It is also possible that studies examined sleep IIV but did not report null findings, either in text or tables, which may contribute to publication bias in this area. In addition, we limited our review to published studies written in English, although it is worth noting that many studies included in in this review were conducted outside of English-speaking countries.
Conclusion
This is the first systematic review of the correlates of sleep IIV among children and adolescents. Although findings were mixed across many domains, it is important to note the variety of developmental, psychosocial, physical health, cognitive, and emotional and behavioral correlates of pediatric sleep variability that have either been shown consistently or seem promising. Given the rapid acceleration in studies on sleep variability, we are optimistic that more refined, developmentally-sensitive, theory-driven, and directional research will clarify the causes, mechanisms, and consequences of daily fluctuations in the sleep of youth.
Supplementary Material
Practice Points.
A systematic review examining the correlates of sleep IIV in children and adolescents identified 52 studies published between 2000 and 2015, with a recent increase in the number of studies examining sleep IIV in children.
The limited literature with varied methodological and assessment procedures limit drawing firm conclusions, though sleep IIV in youth does appear to be associated with increased age/pubertal status, non-White race, physical and neurodevelopmental conditions, psychopathology, body weight, stress, aspects of cognitive functioning, and poorer sleep functioning/habits.
The limited intervention work examining sleep IIV in adolescents is promising, though more work is required using more rigorous intervention designs.
Clinical sleep recommendations around optimizing environmental factors may need to address stability of sleep duration and timing, in addition to overall sleep duration and sleep habits.
Research Agenda.
Research examining sleep intraindividual variability (IIV) in children and adolescents is generally post hoc and atheoretical, with a clear need for studies that advance theory pertaining to the cause, mechanisms, moderators, and outcomes of sleep IIV.
It is important for research examining sleep IIV to be rooted in a developmental framework.
Cross-sectional observational studies will continue to have merit, but studies using prospective and experimental designs are particularly needed.
Intervention studies are needed that use larger sample sizes, longer follow-up periods, and the presence of an active control group within a randomized design.
Empirically and theoretically relevant covariates should be included in studies examining sleep IIV in youth, and it is important to also control for mean sleep variables in order to evaluate the role and importance of sleep IIV specifically.
It is important for future studies to report bivariate associations pertaining to sleep IIV, including both null and significant correlations.
We recommend consistent terminology in future studies, and following Bei et al. [26] recommend the term “intraindividual variability” (IIV).
Acknowledgments
Stephen Becker is supported by award number K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Abbreviations
- ADHD
attention-deficit/hyperactivity disorder
- BMI
body mass index
- CV
coefficient of variance
- EEG
electroencephalography
- IIV
intraindividual variability
- IQ
intelligence quotient
- ISD
individual standard deviation
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SES
socioeconomic status
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
Footnotes
When a study spanned across multiple age groups the mean sample age was used for descriptive categorization purposes.
Conflict of interest: The authors do not have any conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
*The most important references are denoted by an asterisk.
- *1.Dahl RE. The regulation of sleep and arousal: development and psychopathology. Dev Psychopath. 1996;8:3–27. [Google Scholar]
- 2.Colrain IM, Baker FC. Changes in sleep as a function of adolescent development. Neuropsychol Rev. 2011;21:5–21. doi: 10.1007/s11065-010-9155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- *4.Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58:649–65. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *5.Becker SP, Langberg JM, Byars KC. Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. J Youth Adolesc. 2015;44:239–70. doi: 10.1007/s10964-014-0248-y. [DOI] [PubMed] [Google Scholar]
- 6.Carskadon MA. Adolescent sleep patterns : biological, social, and psychological influences. Cambridge; New York: Cambridge University Press; 2002. p. xvii.p. 297. [Google Scholar]
- 7.Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Semin Pediatr Neurol. 1996;3:44–50. doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- 8.Owens JA Adolescent Sleep Working Group. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134:e921–32. doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18:75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 10.Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012;16:213–22. doi: 10.1016/j.smrv.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 12.Gregory AM, Sadeh A. Annual research review: Sleep problems in childhood psychiatric disorders - a review of the latest science. J Child Psychol Psychiatry. 2015;57:296–317. doi: 10.1111/jcpp.12469. [DOI] [PubMed] [Google Scholar]
- 13.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14:179–89. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16:137–49. doi: 10.1111/obr.12245. [DOI] [PubMed] [Google Scholar]
- 15.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–3. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics. School start times for adolescents. Pediatrics. 2014;134:642–9. doi: 10.1542/peds.2014-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *17.Dillon HR, Lichstein KL, Dautovich ND, Taylor DJ, Riedel BW, Bush AJ. Variability in self-reported normal sleep across the adult age span. J Gerontol B Psychol Sci Soc Sci. 2015;70:46–56. doi: 10.1093/geronb/gbu035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suh S, Nowakowski S, Bernert RA, Ong JC, Siebern AT, Dowdle CL, et al. Clinical significance of night-to-night sleep variability in insomnia. Sleep Med. 2012;13:469–75. doi: 10.1016/j.sleep.2011.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sánchez-Ortuño MM, Carney CE, Edinger JD, Wyatt JK, Harris A. Moving beyond average values: Assessing the night-to-night instability of sleep and arousal in DSM-IV-TR insomnia subtypes. Sleep. 2011;34:531–9. doi: 10.1093/sleep/34.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sánchez-Ortuño MM, Edinger JD. Internight sleep variability: its clinical significance and responsiveness to treatment in primary and comorbid insomnia. J Sleep Res. 2012;21:527–34. doi: 10.1111/j.1365-2869.2012.01010.x. [DOI] [PubMed] [Google Scholar]
- 21.Bronfenbrenner U. The ecology of human development : Experiments by nature and design. Cambridge, Mass: Harvard University Press; 1979. p. xv.p. 330. [Google Scholar]
- 22.Steinberg L, Morris AS. Adolescent development. Annual review of psychology. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 23.Sameroff A. A unified theory of development: a dialectic integration of nature and nurture. Child Dev. 2010;81:6–22. doi: 10.1111/j.1467-8624.2009.01378.x. [DOI] [PubMed] [Google Scholar]
- 24.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 25.Rideout V, Foehr UG, Roberts DF. Generation M2: Media in the lives of 8–18 year-olds. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2010. [Google Scholar]
- *26.Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: A systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med Rev. 2016;28:104–20. doi: 10.1016/j.smrv.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 29.Agency for Healthcare Research and Quality. Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- *30.Könen T, Dirk J, Schmiedek F. Cognitive benefits of last night’s sleep: Daily variations in children’s sleep behavior are related to working memory fluctuations. J Child Psychol Psychiatry. 2015;56:171–82. doi: 10.1111/jcpp.12296. [DOI] [PubMed] [Google Scholar]
- 31.Spruyt K, Raubuck DL, Grogan K, Gozal D, Stein MA. Variable sleep schedules and outcomes in children with psychopathological problems: preliminary observations. Nature Science Sleep. 2012;4:9–17. doi: 10.2147/NSS.S29299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He F, Bixler EO, Liao J, Berg A, Imamura Kawasawa Y, Fernandez-Mendoza J, et al. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015;16:1489–94. doi: 10.1016/j.sleep.2015.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Telzer EH, Goldenberg D, Fuligni AJ, Lieberman MD, Gálvan A. Sleep variability in adolescence is associated with altered brain development. Dev Cog Neuroscience. 2015;14:16–22. doi: 10.1016/j.dcn.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep. 2005;28:1568–77. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- 35.Vaughn BE, Elmore-Staton L, Shin N, El-Sheikh M. Sleep as a support for social competence, peer relations, and cognitive functioning in preschool children. Behav Sleep Med. 2015;13:92–106. doi: 10.1080/15402002.2013.845778. [DOI] [PubMed] [Google Scholar]
- 36.Buckhalt JA, El-Sheikh M, Keller P. Children’s sleep and cognitive functioning: race and socioeconomic status as moderators of effects. Child Dev. 2007;78:213–31. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 37.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: multiple indicators and moderation of effects. Health Psychol. 2013;32:849–59. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner LH, Benham H, et al. Sleep behavior in an urban US sample of school-aged children. Arch Ped Adolesc Med. 2004;158:988–94. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 39.McHale SM, Kim JY, Kan M, Updegraff KA. Sleep in Mexican-American adolescents: Social ecological and well-being correlates. J Youth Adolesc. 2011;40:666–79. doi: 10.1007/s10964-010-9574-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S. Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep Med. 2011;12:239–45. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McHale SM, Lawson KM, Davis KD, Casper L, Kelly EL, Buxton O. Effects of a workplace intervention on sleep in employees’ children. J Adolesc Health. 2015;56:672–7. doi: 10.1016/j.jadohealth.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Souza JC, de Sousa IC, Leão Maia AP, de Azevedo CVM. Sleep patterns of teachers and adolescents who attend school in the morning. Biol Rhythm Res. 2012;43:65–72. [Google Scholar]
- 43.Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolesc. 2015;44:389–404. doi: 10.1007/s10964-014-0150-7. [DOI] [PubMed] [Google Scholar]
- 44.Suratt PM, Barth JT, Diamond R, D’Andrea L, Nikova M, Perriello VA, Jr, et al. Reduced time in bed and obstructive sleep-disordered breathing in children are associated with cognitive impairment. Pediatrics. 2007;119:320–9. doi: 10.1542/peds.2006-1969. [DOI] [PubMed] [Google Scholar]
- 45.Erath S, El-Sheikh M. Linking bioregulatory systems: reciprocal autonomic activation predicts sleep over 1 year in middle childhood. Dev Psychobiology. 2015;57:17–24. doi: 10.1002/dev.21246. [DOI] [PubMed] [Google Scholar]
- *46.Fuligni AJ, Hardway C. Daily variation in adolescents’ sleep, activities, and psychological well-being. J Res Adolescence. 2006;16:353–77. [Google Scholar]
- 47.Bagley EJ, Kelly RJ, Buckhalt JA, El-Sheikh M. What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Med. 2015;16:496–502. doi: 10.1016/j.sleep.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuo SI, Updegraff KA, Zeiders KH, McHale SM, Umana-Taylor AJ, De Jesus SA. Mexican American adolescents’ sleep patterns: contextual correlates and implications for health and adjustment in young adulthood. J Youth Adolesc. 2015;44:346–61. doi: 10.1007/s10964-014-0156-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marco CA, Wolfson AR, Sparling M, Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behav Sleep Med. 2012;10:70–80. doi: 10.1080/15402002.2012.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Troxel WM, Lee L, Hall M, Matthews KA. Single-parent family structure and sleep problems in Black and White adolescents. Sleep Med. 2014;15:255–61. doi: 10.1016/j.sleep.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tininenko JR, Fisher PA, Bruce J, Pears KC. Sleep disruption in young foster children. Child Psychiatry Hum Dev. 2010;41:409–24. doi: 10.1007/s10578-010-0177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *52.Bates JE, Viken RJ, Alexander DB, Beyers J, Stockton L. Sleep and adjustment in preschool children: sleep diary reports by mothers relate to behavior reports by teachers. Child Dev. 2002;73:62–74. doi: 10.1111/1467-8624.00392. [DOI] [PubMed] [Google Scholar]
- 53.Kelly RJ, El-Sheikh M. Marital conflict and children’s sleep: reciprocal relations and socioeconomic effects. J Fam Psychol. 2011;25:412–22. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- 54.Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner HL, Redline S. Effects of the home environment on school-aged children’s sleep. Sleep. 2005;28:1419–27. doi: 10.1093/sleep/28.11.1419. [DOI] [PubMed] [Google Scholar]
- 55.Storfer-Isser A, Lebourgeois MK, Harsh J, Tompsett CJ, Redline S. Psychometric properties of the Adolescent Sleep Hygiene Scale. J Sleep Res. 2013;22:707–16. doi: 10.1111/jsr.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127:e345–52. doi: 10.1542/peds.2010-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gillen-O’Neel C, Huynh VW, Fuligni AJ. To study or to sleep? The academic costs of extra studying at the expense of sleep. Child Dev. 2013;84:133–42. doi: 10.1111/j.1467-8624.2012.01834.x. [DOI] [PubMed] [Google Scholar]
- 58.Spilsbury JC, Babineau DC, Frame J, Juhas K, Rork K. Association between children’s exposure to a violent event and objectively and subjectively measured sleep characteristics: a pilot longitudinal study. J Sleep Res. 2014;23:585–94. doi: 10.1111/jsr.12162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bei B, Allen NB, Nicholas CL, Dudgeon P, Murray G, Trinder J. Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents. J Sleep Res. 2014;23:107–17. doi: 10.1111/jsr.12080. [DOI] [PubMed] [Google Scholar]
- *60.He F, Bixler EO, Berg A, Kawasawa YI, Vgontzas AN, Fernandez-Mendoza J, et al. Habitual sleep variability, not sleep duration, is associated with caloric intake in adolescents. Sleep Med. 2015;16:856–61. doi: 10.1016/j.sleep.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int J Obesity. 2014;38:32–9. doi: 10.1038/ijo.2013.147. [DOI] [PubMed] [Google Scholar]
- 62.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Ancoli-Israel S, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34:1175–83. doi: 10.1093/jpepsy/jsp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yokomaku A, Misao K, Omoto F, Yamagishi R, Tanaka K, Takada K, et al. A study of the association between sleep habits and problematic behaviors in preschool children. Chronobiol Int. 2008;25:549–64. doi: 10.1080/07420520802261705. [DOI] [PubMed] [Google Scholar]
- 64.Araújo DF, Soares CS, Almondes KM. Relation between sleep and visuospatial skills in students from a public school. Estudos de Psicologia. 2013;18:109–16. [Google Scholar]
- 65.Hoyniak CP, Petersen IT, McQuillan ME, Staples AD, Bates JE. Less efficient neural processing related to irregular sleep and less sustained attention in toddlers. Dev Neuropsychol. 2015;40:155–66. doi: 10.1080/87565641.2015.1016162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gruber R, Sadeh A. Sleep and neurobehavioral functioning in boys with attention-deficit/hyperactivity disorder and no reported breathing problems. Sleep. 2004;27:267–73. doi: 10.1093/sleep/27.2.267. [DOI] [PubMed] [Google Scholar]
- 67.Landau R, Sadeh A, Vassoly P, Berger A, Atzaba-Poria N, Auerbach JG. Sleep patterns of 7-week-old infants at familial risk for attention deficit hyperactivity disorder. Infant Mental Health Journal. 2010;31:630–46. doi: 10.1002/imhj.20275. [DOI] [PubMed] [Google Scholar]
- *68.Gruber R, Sadeh A, Raviv A. Instability of sleep patterns in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adoelsc Psychiatry. 2000;39:495–501. doi: 10.1097/00004583-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 69.Hvolby A, Jorgensen J, Bilenberg N. Actigraphic and parental reports of sleep difficulties in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2008;162:323–9. doi: 10.1001/archpedi.162.4.323. [DOI] [PubMed] [Google Scholar]
- 70.Moreau V, Rouleau N, Morin CM. Sleep of children with attention deficit hyperactivity disorder: actigraphic and parental reports. Behav Sleep Med. 2014;12:69–83. doi: 10.1080/15402002.2013.764526. [DOI] [PubMed] [Google Scholar]
- 71.Owens JA, Sangal RB, Sutton VK, Bakken R, Allen AJ, Kelsey D. Subjective and objective measures of sleep in children with attention-deficit/hyperactivity disorder. Sleep Med. 2009;10:446–56. doi: 10.1016/j.sleep.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 72.Poirier A, Corkum P. Night-to-night variability of sleep in children with ADHD and typically developing controls. J Atten Disord. 2015 doi: 10.1177/1087054715575065. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 73.Anders TF, Iosif AM, Schwichtenberg AJ, Tang K, Goodlin-Jones BL. Six-month sleep-wake organization and stability in preschool-age children with autism, developmental delay, and typical development. Behav Sleep Med. 2011;9:92–106. doi: 10.1080/15402002.2011.557991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Goodlin-Jones BL, Tang K, Liu J, Anders TF. Sleep patterns in preschool-age children with autism, developmental delay, and typical development. J Am Acad Child Adoelsc Psychiatry. 2008;47:930–8. doi: 10.1097/CHI.ObO13e3181799f7c. [DOI] [PubMed] [Google Scholar]
- 75.Goodlin-Jones BL, Waters S, Anders TF. Objective sleep measurement in typically and atypically developing preschool children with ADHD-like profiles. Child Psychiatry Hum Dev. 2009;40:257–68. doi: 10.1007/s10578-009-0124-2. [DOI] [PubMed] [Google Scholar]
- 76.Gould EL, Loesch DZ, Martin MJ, Hagerman RJ, Armstrong SM, Huggins RM. Melatonin profiles and sleep characteristics in boys with fragile X syndrome: a preliminary study. Am J Med Genetics. 2000;95:307–15. [PubMed] [Google Scholar]
- 77.Spruyt K, Alaribe CU, Nwabara OU. To sleep or not to sleep: a repeated daily challenge for African American children. CNS Neuroscience Therapeutics. 2015;21:23–31. doi: 10.1111/cns.12319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bei B, Byrne ML, Ivens C, Waloszek J, Woods MJ, Dudgeon P, et al. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early Interv Psychiatry. 2013;7:213–20. doi: 10.1111/j.1751-7893.2012.00382.x. [DOI] [PubMed] [Google Scholar]
- 79.Sousa IC, Araújo JF, Azevedo CVM. The effect of a sleep hygiene education program on the sleep-wake cycle of Brazilian adolescent students. Sleep Biol Rhythms. 2007;5:251–8. [Google Scholar]
- 80.Sousa IC, Souza JC, Louzada FM, Azevedo CVM. Changes in sleep habits and knowledge after an educational sleep program in 12th grade students. Sleep Biol Rhythms. 2013;11:144–53. [Google Scholar]
- 81.Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. J Am Acad Child Adoelsc Psychiatry. 2006;45:512–9. [PubMed] [Google Scholar]
- 82.Acebo C, Carskadon MA. Influence of irregular sleep patterns on waking behavior. In: Carskadon MA, Carskadon MA, editors. Adolescent sleep patterns: Biological, social, and psychological influences. New York, NY, US: Cambridge University Press; 2002. pp. 220–35. [Google Scholar]
- 83.Boyer TW. The development of risk-taking: A multi-perspective review. Dev Rev. 2006;26:291–345. [Google Scholar]
- 84.Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005;115:1555–61. doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 85.Hasler BP, Dahl RE, Holm SM, Jakubcak JL, Ryan ND, Silk JS, et al. Weekend-weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biological psychology. 2012;91:334–41. doi: 10.1016/j.biopsycho.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kang SG, Lee YJ, Kim SJ, Lim W, Lee HJ, Park YM, et al. Weekend catch-up sleep is independently associated with suicide attempts and self-injury in Korean adolescents. Comprehensive psychiatry. 2014;55:319–25. doi: 10.1016/j.comppsych.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 87.Randler C. Association between morningness-eveningness and mental and physical health in adolescents. Psychol Health Med. 2011;16:29–38. doi: 10.1080/13548506.2010.521564. [DOI] [PubMed] [Google Scholar]
- 88.Ahn S, Fedewa AL. A meta-analysis of the relationship between children’s physical activity and mental health. Journal of pediatric psychology. 2011;36:385–97. doi: 10.1093/jpepsy/jsq107. [DOI] [PubMed] [Google Scholar]
- 89.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2009. Vital Health Stat. 2010;10:1–82. [PubMed] [Google Scholar]
- 90.Van Dyk TR, Thompson RW, Nelson TD. Daily bidirectional relationships between sleep and mental health symptoms in youth With emotional and behavioral problems. J Pediatr Psychol. 2016 doi: 10.1093/jpepsy/jsw040. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 91.Karazsia BT, Berlin KS, Armstrong B, Janicke DM, Darling KE. Integrating mediation and moderation to advance theory development and testing. Journal of pediatric psychology. 2014;39:163–73. doi: 10.1093/jpepsy/jst080. [DOI] [PubMed] [Google Scholar]
- 92.Wiley JF, Bei B, Trinder J, Manber R. Variability as a predictor: a Bayesian variability model for small samples and few repeated measures: arXir [stat.AP] 2014 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.