Abstract
Sexual orientation-related discrimination experiences have been implicated in elevated rates of anxiety symptoms within sexual minority groups. Theory suggests that chronic discrimination experiences may dampen the ability to tolerate distress, increasing vulnerability for anxiety. This study examined the role of distress tolerance, or the capacity to withstand negative emotions, as a construct underlying associations between discriminatory experiences and anxiety among sexual minority adults. Participants (N=119; Mage= 36.4 ±14.8; 50% cisgender male, 31% cisgender female, 19% transgender; 37% non-Latino white) were recruited from Houston, Texas. Measures administered included the Heterosexist Harassment, Rejection, and Discrimination Scale (discrimination experiences), Distress Tolerance Scale (distress tolerance), and the State-Trait Inventory for Cognitive and Somatic Anxiety (anxiety). The association of discrimination experiences and anxiety through distress tolerance was assessed using covariate-adjusted mediation modeling. Results indicated that sexual orientation-related discrimination experiences were significantly and positively associated with anxiety and that this association was mediated through lower distress tolerance. Significant indirect effects were specific to cognitive (versus somatic) anxiety symptoms. Results suggest that distress tolerance may be an explanatory mechanism in the association between discriminatory experiences and cognitive symptoms of anxiety and a potentially relevant target within clinical interventions to address anxiety-related health disparities among sexual minority adults. However, more sophisticated designs are needed to delineate causal associations.
Keywords: sexual minority, discrimination, anxiety, distress tolerance, emotional dysregulation
INTRODUCTION
Individuals ascribing to non-hetero sexual orientations (e.g., lesbian, gay, bisexual; hereafter referred to as sexual minorities) are at higher risk of anxiety disorders and symptomatology relative to heterosexuals.1–6 Research suggests that minority stressors, such as discrimination experiences, may play a causal role in these elevated anxiety rates.4, 7–9 Discriminatory behaviors, or actions demonstrating intolerance toward those of perceived sexual minority status, can include unfair treatment, verbal or physical harassment, and physical violence. Unfortunately, discrimination experiences are not uncommon among sexual minority individuals.10–12 For example, one study using a national sample cited that 54% of lesbian women, 50% of gay men, 24% of bisexual men, and 17% of bisexual women experienced at least one form of discrimination based on sexual orientation over the past year.12 A link between discrimination experiences and anxiety symptomology among sexual minorities has been largely established by data and is supported by theory.4, 13 Previous studies have suggested that certain coping methods, including not accepting or discussing discrimination experiences with others, may be associated with elevated psychopathology,10 though pathways are likely to be multifaceted and complex.6 Thus, more research on explanatory mechanisms that underlie associations between discrimination experiences and anxiety symptomology is needed.1, 10 The delineation of these underlying constructs can increase understanding of why discrimination experiences are associated with negative mental health outcomes, aid in the identification of factors that may transmit risk for negative mental health symptomatology in response to discrimination experiences, and highlight promising targets for interventions to reduce anxiety-related health disparities among sexual minority groups.
Hatzenbuehler and colleagues proposed a theoretical framework positing that sexual minority stigma has negative effect on mental health through greater emotional dysregulation.14 Specifically, this framework suggests that chronic experiences of discrimination based on sexual orientation may, among other things, erode the capacity to regulate emotional responses,14–17 which can ultimately contribute to psychological symptomatology and disorders.18 Although this framework supports the potential relevance of emotional dysregulation in explaining associations between discrimination experiences and anxiety symptomatology among sexual minorities, empirical literature examining this pathway is scarce.
Distress tolerance, a potentially lower-order facet of emotional dysregulation, is the perceived capacity or actual ability to endure or tolerate negative affective states.16,19 Individuals with low distress tolerance are less equipped to manage challenging situations and may exhibit a pronounced reaction to stress or distress. Distress tolerance is considered a key transdiagnostic vulnerability factor that is associated with elevated anxiety symptomatology independent of other related constructs like anxiety sensitivity and general negative affect.20 Although associations between lower distress tolerance and greater anxiety symptomatology have been cited among a number of diverse samples, including individuals who were HIV+,21 these associations have not been previously been investigated among a sexual minority sample. Yet if distress tolerance is linked with the onset and/or maintenance of anxiety symptoms among this group, it makes an apt intervention target to combat mental health disorders or distress through the promotion of healthier coping methods and greater emotional regulation in response to provocative stimuli.22
Factors playing a causal or maintenance role in distress tolerance itself, however, are not well understood. Recently, researchers have suggested a potential neurobiological basis to distress tolerance that is complemented by learning experiences, contextual factors, and executive functioning.16 Specifically, they suggest that individuals with low distress tolerance may exhibit behavioral inhibition in the face of provocative situations that leads to perceptions of low control over the stress response.16 Likewise, chronic exposure to discrimination experiences may also lend to the perception of low controllability over an aversive stimuli, especially given that not all contexts offer the benefit of legal protection against discrimination. Moreover, it has been suggested that some individuals may become sensitized to emotionally provocative events and exhibit increased intolerance of them or the affective states they engender over time,16 which suggests a possible causal link between discrimination experiences and low distress tolerance – especially relevant to population subgroups experiencing discrimination events at relatively high rates. Likewise, research has suggested deficits in emotional regulation capacity among sexual minority adolescents relative to heterosexual adolescents,23 and supported links between discrimination experiences and enhanced emotional dysregulation among sexual minority youth17 as well as adults.14, 15 Therefore, discrimination experiences may possibly engender or perpetuate low distress tolerance, a facet of emotional dysregulation, among sexual minority individuals.
The current correlational study represents an important initial step in the empirical study of Hatzenbuehler and colleagues’ theoretical framework14 by examining the indirect effect of distress tolerance in the association of discrimination experiences with anxiety symptomatology among a sample of sexual minority adults. Although the elimination of discrimination based on sexual orientation is likely to be most impactful in the promotion of mental health and wellness, enhanced understanding of the factors that link discrimination and anxiety symptomatology may have implications for the design of clinical interventions to address or prevent anxiety-related health disparities within this minority group in the current social/structural context wherein discrimination experiences are not uncommon.
METHODS
Procedures
Participants were adults recruited from the Houston metropolitan statistical area to participate in Project FRESH AIR (Focused Research to Enhance Social Health Among Individuals in the Rainbow), which was aimed toward understanding associations of stress and health among sexual minority adults. Recruitment for Project FRESH AIR was achieved via strategic flyer posting and through targeted paid mediums, and enrollment into the study spanned February 2015 to October 2015. Eligibility criteria were: 1) adult aged 18 years or older; 2) self-identification as bisexual, gay, or lesbian; 3) provision of valid contact information (home address, functioning phone number); 4) willingness to comply with the study protocol; 5) not currently pregnant or lactating; and 6) had not participated in a companion online study via self-report.
Interested individuals called a devoted study line, were screened for eligibility, and scheduled for an initial in-person appointment if eligible. Written informed consent was obtained at this initial in-person contact at the (omitted for blind review) Lab at the University of (omitted for blind review). Participants then completed study measures, which were administered on a laptop computer. Participants were compensated $30 in department store gift cards for the time and effort associated with the data collection. Study procedures were approved by the Institutional Review Board at the university of (omitted for blind review).
Measures
Sociodemographics
Sociodemographics included age, gender (cisgender male, cisgender female, or transgender), sexual orientation (bisexual vs monosexual), education (≤ high school diploma vs trade school or college degree), and race/ethnicity (non-Latino white vs other race/ethnicity).
Discrimination experiences
Discrimination experiences were assessed using the 14-item self-report Heterosexist Harassment, Rejection, and Discrimination Scale (HHRDS).24 Respondents were asked to report on experiences over the past year on a 6-point scale from never (1) to almost all of the time (6). Rules are presented for each response option; for example, sometimes = “If the event happened less than 10% of the time” and a lot = “If the event happened 26–49% of the time.” Items include: “How many times have you been treated unfairly by your employer, boss, or supervisors because you are a lesbian, gay or bisexual person?” and “How many times have you been verbally insulted because you are a lesbian, gay or bisexual person?” with higher scores indicative of greater experiences with discrimination. This measure has demonstrated excellent reliability and good discriminant and convergent validity in previous research.24, 25 Cronbach’s alpha for the HHRDS was .90 in this sample.
Perceived distress tolerance
Perceived distress tolerance was measured with the 15-item self-report Distress Tolerance Scale (DTS).19 Distress tolerance is defined as one’s perceived capacity to withstand emotional distress or other aversive psychological and/or physical states. Items include: “There’s nothing worse than feeling distressed or upset,” and “Other people seem to be able to tolerate feeling distressed or upset better than I can.” The DTS uses a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5), with higher scores indicating lower levels of distress tolerance. The DTS has been shown to have high discriminant and convergent validity and to be relatively stable over a six-month period.19 Cronbach’s alpha for the DTS was .92 in this sample.
Anxiety symptoms
The State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA)26 was used to assess anxiety symptoms. The STICSA has a total score and two subscales: somatic and cognitive symptoms. Items include: “I have trouble remembering things,” (cognitive) “I worry that I cannot control my thoughts as well as I would like to,” (cognitive) “My palms feel clammy,” (somatic) and “My muscles feel weak” (somatic). Respondents are asked to rate how often, in general, each statement is true of them. Responses range from not at all (1) to very much so (4), with higher scores indicating greater anxiety. This measure has demonstrated good reliability and convergent and discriminant validity.27 Scores on this measure range from 21 to 84, with a score of 40 indicating a possible anxiety disorder and a score of 43 a likely anxiety disorder.28 However, criterion scores were maintained as continuous for analyses. Cronbach’s alpha for the STICSA total score was .90; with internal consistencies of .84 for the somatic subscale and .89 for the cognitive subscale in this sample.
Data Analysis
Participants were permitted to skip any items that they did not wish to answer; therefore, multi-item measures were mean scored as long as ≥80% of constituent items were completed. Preliminary analyses included descriptive statistics and analysis of correlations between variables. Indirect effects of discrimination experiences and anxiety through distress tolerance were examined using a covariate-adjusted non-parametric, bias-corrected bootstrapping procedure via the PROCESS macro (v 2.15).29, 30 This procedure generated an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect paths using 5000 resamples from the data. A significant indirect effect was evidenced by a 95% confidence interval not containing zero. Covariates in the analytic model were age, gender, sexual orientation, education, and race/ethnicity. To examine the specificity of the model, additional covariate-adjusted reverse models were run wherein the predictor (discrimination experiences) and explanatory variable (distress tolerance) were interchanged and then the criterion (anxiety symptoms) and explanatory variables (distress tolerance) interchanged.30 Following the main model, two additional covariate-adjusted models were run whereby the criterion variable was cognitive and somatic anxiety symptoms, respectively, keeping the random number generator consistent with the main model so that the same resamples from the dataset were used in the bootstrapping process.30 The mediation ratio (ratio of the indirect effect to the total effect) and the index of mediation (completely standardized indirect effect) were used as a measures of effect size.31 All analyses were performed using IBM SPSS Statistics, version 23.
RESULTS
Participants (N = 119) were 36.4 years of age on average (SD = 14.8) and 50% of the sample identified as cisgender male, 31% as cisgender female, and 19% as transgender. Approximately 36% of the sample were educated in trade school or achieved a college degree. The complete list of participant descriptives and the intercorrelations between variables is displayed in Table 1. Overall, 43.7% of the sample screened positive for a possible anxiety disorder and 34.5% a probable anxiety disorder, according to suggested cut-off scores.28 Rates of any anxiety disorder among epidemiological samples of sexual minority samples differ between studies, potentially based on differing definitions of sexual orientation.32 However, for comparison, a previous study suggested a lifetime prevalence of 40.8% to 57.8% among lesbian and bisexual cisgender women and 38.7% and 41.2% among bisexual and gay cisgender men, respectively, with similar past year prevalence rates.6 Of note were universally significant correlations between discrimination experiences, distress tolerance, and anxiety symptoms among this sample. Specifically, shared variance between these variables ranged from 4.8% (discrimination experiences with distress tolerance) to 23% (distress tolerance with cognitive anxiety symptoms).
Table 1.
Participant Characteristics and their Interrelations (N = 119).
| Variables | 1 | 2a | 2b | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Mean (SD) / % [N] |
Min | Max |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1 | 36.41 (14.85) | 18 | 76 | |||||||||
| 2. Gender | |||||||||||||
| cisgender male (REF) | - | 50.4 [60] | |||||||||||
| a. cisgender female | .251** | 1 | 31.1 [37] | ||||||||||
| b. transgender | .277** | - | 1 | 18.5 [22] | |||||||||
| 3. Sexual Orientation | |||||||||||||
| monosexual (REF) | - | - | - | 52.9 [63] | |||||||||
| bisexual | −.004 | .203* | .115 | 1 | 47.1 [56] | ||||||||
| 4. Education | |||||||||||||
| Trade school/college degree (REF) |
- | - | - | - | 36.1 [43] | ||||||||
| ≤High school diploma | .132 | .165 | .043 | .254** | 1 | 63.9 [76] | |||||||
| 5. Race/Ethnicity | |||||||||||||
| non-Latino White (REF) | - | - | - | - | - | 37.0 [44] | |||||||
| other race/ethnicity | −.243** | −.050 | −.173 | .164 | .221* | 1 | 63.0 [75] | ||||||
| 6. Discrimination Experiences |
−.040 | .049 | −.140 | −.022 | −.106 | −.155 | 1 | 2.16 (.80) | 1 | 4.29 | |||
| 7. Distress Tolerance | −.012 | −.156 | .107 | −.121 | −.174 | .019 | .221* | 1 | 2.61 (.92) | 1 | 4.83 | ||
| 8. Anxiety Symptoms | −.027 | −.108 | −.059 | −.198* | −.150 | .028 | .349** | .399* | 1 | 39.14 (11.21) | 21 | 75 | |
| 9. Somatic Symptoms | .083 | −.113 | −.002 | −.250** | −.172 | −.030 | .298** | .203* | .864** | 1 | 18.63 (5.77) | 11 | 39 |
| 10. Cognitive Symptoms | −.112 | −.083 | −.091 | −.112 | −.099 | .071 | .320** | .482** | .908** | .572** | 20.50 (6.91) | 10 | 40 |
Note:
p< .05;
p<.01.
Interrelations between participant characteristics were evaluated using Pearson correlations for continuous-continuous variable associations, Point-biserial correlations for continuous-binary associations, and Phi coefficients for binary-binary associations. Discrimination experiences were assessed with the Heterosexist Harassment, Rejection, and Discrimination Scale; Distress tolerance was assessed with the Distress Tolerance Scale; and Anxiety symptoms with the State-Trait Inventory for Cognitive and Somatic Anxiety. Gander was dummy coded for analyses and presented as coded in the table. Note that higher scores on the Distress Tolerance Scale are indicative of lower levels of perceived distress tolerance. Data on the following subscales were limited to N=118 due to missingness: the somatic subscale of the State-Trait Inventory for Cognitive and Somatic Anxiety.
Of the 14 discrimination items administered, the top 5 endorsed more frequently than never were: “How many times have you been called a heterosexist name like dyke, lezzie, fag or other names?” (endorsed by 80.7% of the sample); “How many times have you been verbally insulted because you are a lesbian, gay or bisexual person?” and “How many times have you heard anti-lesbian/anti-gay/anti-bisexual remarks from family members?” (each endorsed by 77.3% of the sample); “How many times have you been treated unfairly by strangers because you are a lesbian, gay or bisexual person?” (endorsed by 71.4% of the sample); “How many times have you been treated unfairly by your co-workers, fellow students, or colleagues because you are a lesbian, gay or bisexual person?” (endorsed by 68.1% of the sample); and “How many times have you been treated unfairly by your family because you are a lesbian, gay or bisexual person?” (endorsed by 66.4% of the sample).
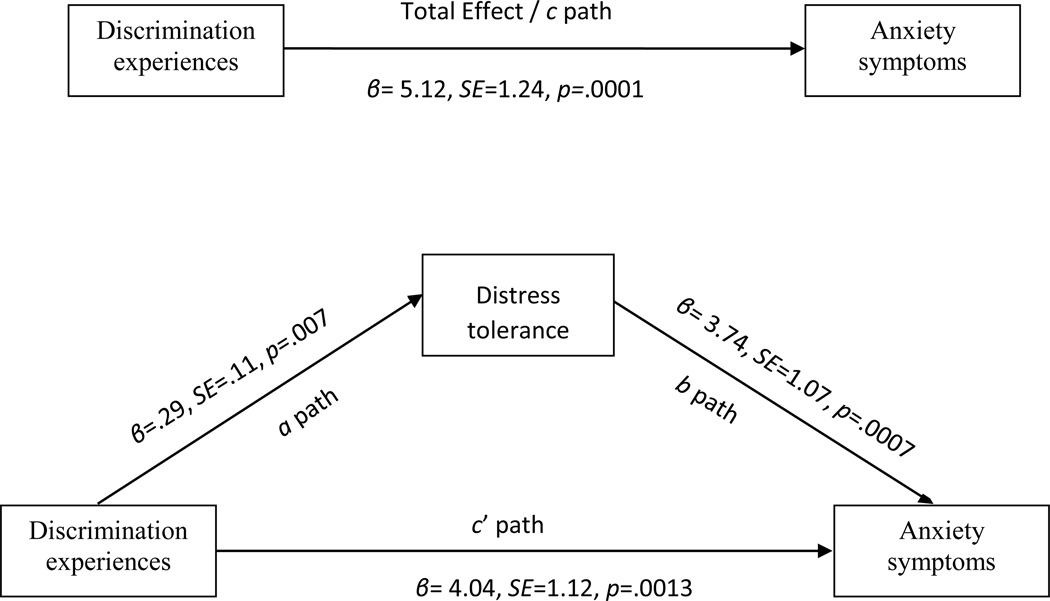
Results of the main analysis indicated a significant total effect of discrimination experiences on anxiety symptoms. Moreover, there was a significant indirect effect for distress tolerance on the association between discrimination experiences and anxiety (ab = 1.07, SE=.57; 95% CI = [.221, 2.516]). Specifically, more discrimination experiences were associated with lower distress tolerance, which was associated with greater anxiety in the covariate-adjusted model. See Figure 1. The mediation ratio was Pm = .210, SE = .171; 95% CI (.047, .589), suggesting that distress tolerance mediated approximately 21% of the total effect of discrimination experiences on anxiety symptoms. The index of mediation was abcs = .077, SE = .038; 95% CI (.016, .170), indicating that anxiety symptoms increased by .077 a standard deviation for every 1 standard deviation increase in discrimination indirectly via distress intolerance. However, it is also important to note that the indirect effects in the reverse models also emerged as significant (x & m reversed: ab = .885, SE = .48; 95% CI = [.177, 2.125]; y & m reversed: ab = .137, SE = .06; 95% CI = [.043, .290]).
Figure 1.
Hypothesized conceptual model of the total (c path) and indirect effect (ab path) of discrimination experiences on anxiety symptoms through distress tolerance, controlling for age, gender, sexual orientation, education, and race/ethnicity.
Follow-up analyses examined whether indirect effects were specific to somatic or cognitive anxiety symptoms using subscales of the STICSA anxiety measure in the covariate-adjusted model. These results indicated that significant indirect effects were limited to the cognitive symptoms (ab = .093, SE = .04; 95% CI = [.021, .198]) and did not extend to the somatic symptoms (ab = .013, SE = .02; 95% CI = [−.011, .058]). See Table 2 for model pathways and measures of effect size.
Table 2.
Model Pathways for Mediation of Discrimination Experiences on Somatic and Cognitive Anxiety Symptoms through Distress Tolerance.
| Criterion Variable | ||
| Model Information | Somatic Anxiety Symptoms | Cognitive Anxiety Symptoms |
| a path | β = .29, SE = .11, p = .008 | β =.29, SE = .11, p = .007 |
| b path | β = .05, SE = .05, p = .385 | β = .32, SE = .06, p <.0001 |
| c path | β = .21, SE = .06, p <.001 | β = .29, SE = .08, p <.001 |
| c′ path | β = .19, SE = .06, p = .002 | β = .19, SE = .07, p = .009 |
| Mediation ratio | Pm =.064, SE = .19 (95% CI [−.083, .370]) | Pm = .324, SE = .28 (95% CI [.088, .839]) |
| Index of mediation | abcs =.021, SE = .03 (95% CI [−.018, .087]) | abcs = .106, SE = .05 (95% CI [.026, .218]) |
Note: Somatic and cognitive anxiety symptoms were assessed using the subscales of the State-Trait Inventory for Cognitive and Somatic Anxiety. The a paths in these models differed slightly because of the reduced sample size for somatic anxiety symptoms. The mediation ratio is the ratio of the indirect effect to the total effect, and the index of mediation is the completely standardized indirect effect. Note that higher scores on the Distress Tolerance Scale are indicative of lower levels of perceived distress tolerance.
DISCUSSION
The current study supported the role of low perceived distress tolerance in associations between discrimination experiences and anxiety symptomatology among a community-based convenience sample of sexual minority adults, and suggested a unique pathway that explained 21% of the covariance in anxiety symptomatology and approximately 32% of the covariance in cognitive anxiety symptoms specifically. Results lend support to Hatzenbuehler’s theoretical framework about how sexual minority stigma affects mental health among sexual minority individuals via (a particular facet of) emotional dysregulation14 and extend it to highlight the relative importance of cognitive processes versus somatic symptoms. It may be that the experience of repeated and chronic discrimination related to sexual orientation functions to erode distress tolerance over time and contributes to emotional dysregulation,14–17 ultimately resulting in anxiety-related symptomatology and other behavioral sequalae16 heightening the risk of health disparities among sexual minorities.18 However, these results should be considered with caution for two primary reasons: 1) although guided by theory, underlying data were cross-sectional; and 2) significant indirect effects were not limited to the main analysis, but also emerged in alternate reverse models. The cross-sectional nature of the work cannot speak to causation between constructs and more sophisticated designs, such as cross-lagged models, have been recommended due to potential over-inflation or under-estimation of effects when variables are measured concurrently.33 Additionally, the covariance between variables may have contributed to significance of reversed models. Thus, although the directionality of these results cannot be determined, the study represents the first to our knowledge to test this specific pathway among an adult sexual minority sample, suggesting the potential relevance of continued study in this area to bolster extant theory and inform clinical work to address anxiety symptomatology among this at-risk group.
From an interventions perspective, if future studies confirm suggested associations, sexual minority adults experiencing discrimination in the past year who also present clinically with anxiety symptomatology may benefit from attention to developing healthier coping methods and emotional regulation skills, inasmuch as distress tolerance might be a key underlying vulnerability factor.22 Several evidenced-based clinical approaches are geared toward enhancing emotion regulation (for a brief overview, see16), and may be particularly useful when tailored to the unique stressors of the targeted population.34–36 Still, literature regarding the specific therapeutic benefits of enhancing distress tolerance to ameliorate anxiety symptomatology is in its nascent stage at the present time, and would benefit from additional empirical study.16 Additionally, it is important to acknowledge that distress tolerance may represent only part of the potentially broader construct of emotional dysregulation.16 Therefore, other key emotional dysregulation factors (e.g., heightened emotional intensity, difficulty understanding or identifying feelings) may also be important to assess for their role in these associations and to address within clinical interventions for anxiety.
The extent to which discrimination experiences contribute to low distress tolerance, as has been suggested in the literature,14–17 or co-occur along with it cannot be determined from the present study due to its cross-sectional nature. However, to the extent that they might be contributory highlights the relevance of societal, legal, organizational and social interventions to reduce mental health disparities on a population level, which might be the most impactful way to combat the ill effects of discriminatory experiences based on sexual orientation. Likewise, whether low distress tolerance is the cause or consequence of anxiety symptomatology cannot be determined from these data. Future studies will benefit from longitudinal designs to address causal relations between variables of interest. Additionally, future work may benefit from more sophisticated modeling of Hatzenbuehler’s framework14, 15 by including both distal and proximal stigma-based stressors and assessing more potential mechanisms such as social interpersonal problems and specific cognitive processes (e.g., pessimism, self-schemas). Also, a limitation of the present study is the absence of diagnostic (interview-based) data on anxiety disorders and other related psychiatric disturbances. Future work should address the potential for distress tolerance to mediate associations between discrimination experiences and clinical disorders. Finally, it is notable that the current study assessed perceived distress tolerance, as opposed to the behavioral action of distress tolerance.16 Because there may be distinct differences between these related conceptualizations of distress tolerance,16 future research in this area should expand to assess more behavioral or biobehavioral manifestations of distress tolerance (e.g., via Breath-Holding, Mirror Tracing Persistence, or cold pressor tasks) to complement the self-report of perceived distress tolerance used in the present study. Given the current pattern of results whereby distress tolerance mediated the relations between discrimination experiences and cognitive – but not somatic – anxiety, it is possible that tapping into true biobehavioral capacity for distress tolerance via an experimental paradigm would yield different results.
An additional weakness of the current study is the use of a convenience sample from a single metropolitan statistical area in Texas. Therefore, the extent to which findings generalize to other samples or the overall population of sexual minority adults is not known. To the degree that repeated discrimination experiences may engender low distress tolerance among those with an extant diathesis, there are several reasons why a multi-site study might be of interest: a) greater legal protections against discrimination on the basis of sexual identity have been linked to reduced experiences of discrimination37 and a lower likelihood of mental health problems;38 b) anti-discriminatory policies about marriage may also be linked with lower risk of mental health disorders;39 and c) residence in areas with higher proportions of sexual minorities may confer mental health benefits.40 Consequently, because places (e.g., cities, states) vary on their support for anti-discriminatory practices and their sexual-orientation composition, the extent to which place moderates the associations examined herein is of interest and has clear implications for public policy.
Despite limitations, the current study lends preliminary support to a theoretical framework linking discrimination experiences with low distress tolerance and anxiety symptomatology among a sample of sexual minority adults and provides a basis for future investigation in an area that is worthy of additional study. Although the link between discriminatory experiences and anxiety is known,4 the current study benefitted from attention to a potential underlying mechanism of distress tolerance and focused on a sexual minority sample, which represents a unique addition to the literature. Future studies would benefit from longitudinal approaches to assess directional associations between constructs.
CONCLUSIONS
The present study was the first, to our knowledge, to examine the extent to which perceived distress tolerance contributed to covariance in the association between discriminatory experiences and anxiety symptoms among sexual minority adults. Findings suggest a potential explanatory role of low distress tolerance in relations of sexual orientation-related discrimination and anxiety symptoms, particularly cognitive anxiety symptoms, among sexual minority adults. Results are significant for their contribution to the examination of a population-specific theoretical framework to explain extant mental health disparities,15 and represent a preliminary step in the ultimate goal of mapping the etiology of stigma-related anxiety symptomatology among a vulnerable population and learning how to address it in the context of clinical intervention.
Highlights.
Sexual minority adults experience discrimination and anxiety at high rates.
Discrimination may dampen distress tolerance, increasing anxiety vulnerability.
Here, distress tolerance mediated the discrimination-anxiety association (N=119).
Sexual orientation discrimination may link to anxiety through distress tolerance.
As such, distress tolerance may be a target in clinical interventions for anxiety.
Acknowledgments
FUNDING
This project, jointly led by NG Smith and LR Reitzel, was supported by their institutional funding from the University of Houston. Manuscript authorship was further supported by the National Institute on Drug Abuse at the National Institutes of Health through R01 DA034739 (to co-investigator EM Obasi). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
Authors would like to acknowledge the research staff at the University of Houston who assisted with implementation of the project including Sarah Childress, Kate Winderman, Staci Ouch, Alexis Moisiuc, Daniel Kish, Alison Shellman, Hannah LeBlanc, Quentaxia Wrighting, Desiree Woolard, Jorge Garza, Dinh Thai, Kat Bergez, Jasmin Prudon, Pooja Agrawal, Edna Paredes, Lucia Cavanagh, and Erin “Charli” Washington.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DECLARATION OF INTERESTS
Authors have no competing interests pertaining to this research.
REFERENCES
- 1.Gilman SE, Cochran SD, Mays VM, et al. Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. Am J Public Health. 2001;91(6):933–939. doi: 10.2105/ajph.91.6.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.King M, Semlyen J, Tai SS, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis NM. Mental health in sexual minorities: recent indicators, trends, and their relationships to place in North America and Europe. Health Place. 2009;15(4):1029–1045. doi: 10.1016/j.healthplace.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Bostwick WB, Boyd CJ, Hughes TL, et al. Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. Am J Public Health. 2010;100(3):468–475. doi: 10.2105/AJPH.2008.152942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frisell T, Lichtenstein P, Rahman Q, et al. Psychiatric morbidity associated with same-sex sexual behaviour: influence of minority stress and familial factors. Psychol Med. 2010;40(2):315–324. doi: 10.1017/S0033291709005996. [DOI] [PubMed] [Google Scholar]
- 8.Yang MF, Manning D, van den Berg JJ, et al. Stigmatization and Mental Health in a Diverse Sample of Transgender Women. LGBT Health. 2015;2(4):306–312. doi: 10.1089/lgbt.2014.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mays VM, Cochran SD. Mental health correlates of perceived discrimination among lesbian, gay, and, bisexual adults in the United States. Am J Public Health. 2001;91(11):1869–1876. doi: 10.2105/ajph.91.11.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health. 2010;100(8):1477–1484. doi: 10.2105/AJPH.2009.181586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swim JK, Pearson NB, Johnston KE. Daily encounters with heterosexism: a week in the life of lesbian, gay, and bisexual individuals. J Homosex. 2007;53(4):31–48. doi: 10.1080/00918360802101179. [DOI] [PubMed] [Google Scholar]
- 12.Bostwick WB, Boyd CJ, Hughes TL, et al. Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. Am J Orthopsychiatry. 2014;84(1):35–45. doi: 10.1037/h0098851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reisner SL, White Hughto JM, Gamarel KE, et al. Discriminatory experiences associated with Posttraumatic Stress Disorder symptoms among transgender adults. J Couns Psychol. 2016 doi: 10.1037/cou0000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma "get under the skin"?: the mediating role of emotion regulation. Psychol Sci. 2009;20(10):1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatzenbuehler ML. How does sexual minority stigma "get under the skin"? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychol Bull. 2010;136(4):576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. J Consult Clin Psychol. 2009;77(5):894–904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLaughlin KA, Hatzenbuehler ML, Mennin DS, et al. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. 2011;49(9):544–554. doi: 10.1016/j.brat.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simons JS, Gaher RM. The distress tolerance scale: development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- 20.Keough ME, Riccardi CJ, Timpano KR, et al. Anxiety symptomatology: the association with distress tolerance and anxiety sensitivity. Behav Ther. 2010;41(4):567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brandt CP, Zvolensky MJ, Bonn-Miller MO. Distress tolerance, emotion dysregulation, and anxiety and depressive symptoms among HIV + individuals. Cogn Ther Res. 2013;37:446–455. [Google Scholar]
- 22.Zvolensky MJ, Leventhal AM. Affect and Health Behavior Co-Occurrence: The Emerging Roles of Transdiagnostic Factors and Sociocultural Factors. Behav Modif. 2016;40(1–2):3–6. doi: 10.1177/0145445515627307. [DOI] [PubMed] [Google Scholar]
- 23.Hatzenbuehler ML, McLaughlin KA, Nolen-Hoeksema S. Emotion regulation and internalizing symptoms in a longitudinal study of sexual minority and heterosexual adolescents. J Child Psychol Psychiatry. 2008;49(12):1270–1278. doi: 10.1111/j.1469-7610.2008.01924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szymanski DM. Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles. 2006;54:227–234. [Google Scholar]
- 25.Szymanski DM. Examining Potential Moderators of the Link Between Heterosexist Events and Gay and Bisexual Men’s Psychological Distress. Journal of Counseling Psychology. 2009;56:142–151. [Google Scholar]
- 26.Ree MJ, MacLeod C, French D, et al. The State–Trait Inventory for Cognitive and Somatic Anxiety: Development and validation. Poster presented at the annual meeting of the Association for the Advancement of Behavior Therapy. New Orleans, LA. 2000 Nov [Google Scholar]
- 27.Gros DF, Antony MM, Simms LJ, et al. Psychometric properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): comparison to the State-Trait Anxiety Inventory (STAI) Psychol Assess. 2007;19(4):369–381. doi: 10.1037/1040-3590.19.4.369. [DOI] [PubMed] [Google Scholar]
- 28.Van Dam NT, Gros DF, Earleywine M, Antony MM. Establishing a trait anxiety threashold that signals likellihood of anxiety disorders. Anxiety Stress Coping. 2013;26(1):70–86. doi: 10.1080/10615806.2011.631525. [DOI] [PubMed] [Google Scholar]
- 29.Hayes AF. Introduction to Mediation, Moderation and Conditional Process Analysis. New York, NY: Guilford Press; 2013. [Google Scholar]
- 30.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 31.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 32.Cohen JM, Blasey C, Taylor CB, et al. Anxiety and related disorders and its concealment in sexual minority young adults. Behav Ther. 2016;47:91–101. doi: 10.1016/j.beth.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Preacher KJ. Advances in mediation analysis: A survey and synthesis of new developments. Annu Rev Psychol. 2015;66:825–852. doi: 10.1146/annurev-psych-010814-015258. [DOI] [PubMed] [Google Scholar]
- 34.Safren SA, Rogers T. Cognitive-behavioral therapy with gay, lesbian, and bisexual clients. J Clin Psychol. 2001;57(5):629–643. doi: 10.1002/jclp.1033. [DOI] [PubMed] [Google Scholar]
- 35.Pachankis JE, Hatzenbuehler ML, Rendina HJ, et al. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol. 2015;83(5):875–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pachankis JE. A transdiagnostic minority stress treatment approach for gay and bisexual men's syndemic health conditions. Arch Sex Behav. 2015;44(7):1843–1860. doi: 10.1007/s10508-015-0480-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hatzenbuehler ML, Schwab-Reese L, Ranapurwala SI, et al. Associations Between Antibullying Policies and Bullying in 25 States. JAMA Pediatr. 2015;169(10):e152411. doi: 10.1001/jamapediatrics.2015.2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health. 2009;99(12):2275–2281. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hatzenbuehler ML, McLaughlin KA, Keyes KM, et al. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hatzenbuehler ML, Keyes KM, McLaughlin KA. The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. Int J Epidemiol. 2011;40(4):1071–1080. doi: 10.1093/ije/dyr019. [DOI] [PMC free article] [PubMed] [Google Scholar]