Abstract
Background
Germline mutations in DICER1 increase the risk of various tumors, including pleuropulmonary blastoma. Macrocephaly and symmetric overgrowth has been reported in some, but not all, patients with mosaic DICER1 RNase IIIb mutations; the prevalence of these features in individuals with constitutional germline DICER1 mutations is unknown.
Methods
We analyzed prospectively collected auxology data from 67 DICER1 mutation carriers and 43 family controls. We assessed differences between groups using an exact test for proportions and generalized estimating equations for continuous dependent variables.
Results
Twenty-eight DICER1 mutation carriers (42%) were macrocephalic, and none had an occipital-frontal circumference (OFC) below the 3rd centile, which significantly differed from family controls, of whom five were macrocephalic (12%) and two had OFC below the 3rd centile (5%) (P<0.001). DICER1 mutation carriers were taller than familial controls after controlling for gender (P=0.048), but similar proportions of both groups were above the 97th centile of population norms. Head circumference remained increased after adjusting for differences in height.
Conclusions
For the first time, we establish macrocephaly as a common finding in the DICER1 syndrome. Like some of the other tumor-predisposition disorders, macrocephaly may be a useful, albeit a subtle, clinical clue to the DICER1 syndrome diagnosis.
Key terms: DICER1, macrocephaly
Introduction
Pleuropulmonary blastoma (PPB), an embryonal sarcoma and the most common pediatric primary lung malignancy1, is the hallmark tumor of the DICER1 syndrome2. Somatic second hits in one of five “hotspot” amino acids of the DICER1 RNase IIIb domain are necessary for malignant transformation of PPB and other DICER1-associated tumors3,4. Germline DICER1 mutations are also associated with a variety of other neoplasms, including cystic nephroma, nasal chondromesenchymal hamartoma, ciliary body medulloepithelioma, pituitary blastoma, as well as Sertoli-Leydig cell tumor and other ovarian sex cord-stromal tumors5.
PPB is a serious complication of the DICER1 syndrome. PPB progresses through stages of malignant transformation, from type I (cystic) to type II (partially cystic/solid) and type III (solid). The 5-year overall survival for later-stage patients is 71% (type II) and 53% (type III). Relapse and metastasis, primarily to the central nervous system, is responsible for much of the mortality6,7. Fortunately, early detection and subsequent surgical resection of PPB can be curative8. However, this is feasible only if DICER1 mutation carriers are identified, and screened (by chest CT), as early in life as possible.
The presence of easily detected, non-malignant phenotypic features can prompt alert clinicians to consider the diagnosis of an occult tumor-predisposition disorder in an otherwise healthy child. For example, the distinctive skin findings and increased head circumference in neurofibromatosis type 1 and Cowden syndrome may appear prior to any syndrome-associated neoplasia. In the DICER1 syndrome, lung cysts, cystic nephroma or family history of multinodular goiter have been used to identify DICER1 mutation carriers (hereafter, “DICER1-carriers”) prior to the development of malignancy8,9. Since the DICER1 syndrome was relatively recently recognized, systematic evaluations of growth have not been reported, although there have been accounts of developmental delay, macrocephaly and overgrowth in10 patients with mosaic DICER1 “hotspot” RNase IIIb mutations. Other accounts have not reported overgrowth or developmental delay in these patients11. In our natural history study of the DICER1 syndrome, we comprehensively evaluated individuals with germline DICER1 mutations and family controls. We analyzed auxology data, particularly head circumference and height measurements, from our cohort to characterize previously unrecognized DICER1-associated disease features that may be useful in identifying individuals and families at risk of PPB.
Methods
Study participants
The National Cancer Institute protocol “DICER1-related pleuropulmonary blastoma cancer predisposition syndrome: a natural history study” (NCI protocol 11-C-0034; NCT #01257597) is open to individuals with DICER1-associated tumors and their family members. One hundred thirty-four participants from 31 families were evaluated at the NIH Clinical Center (CC) between November 2011 and December 2014. CLIA-certified germline DICER1 mutation testing was conducted at Ambry Genetics (Aliso Viejo, CA) and Children’s National Medical Center (Washington, DC). Five children without detectable germline DICER1 mutations but who harbored DICER1-associated tumors were considered separately. We compared individuals carrying pathogenic germline DICER1 mutations (n=76) with unaffected family members lacking pathogenic DICER1 mutations (n=53). The study was approved by the National Cancer Institute’s institutional review board, and all participants, or their parents or guardians, provided written, informed consent.
Dysmorphology and reference curves
Height was measured by clinical staff at the NIH CC using stadiometers. Head occipitofrontal circumference (OFC), arm span, and lower segment length were recorded using measuring tapes, as described by Gripp et al.12. Upper segment length was calculated by subtracting lower segment length (distance from top of pubic symphysis to floor) from height. The upper segment length/lower segment length (US/LS) ratio was then calculated. We compared observed measurements with age- and gender-appropriate reference charts for height13 and OFC14. OFC and height are strongly correlated, and we used OFC-for-height references for those age 18 years and older15. We considered abnormal height to be below the 3rd centile or above the 97th centile, and macrocephaly as greater than the 97th centile in published reference populations.
Statistical analyses
We tested differences in proportions using either a chi-squared test or an exact test when frequencies were low (n<5). We assessed differences in continuous descriptive characteristics using the Wilcoxon rank-sum test. We fit generalized estimating equations (GEE) to the continuous measurements of OFC and height in adults to account for correlation within families, and used robust standard errors. All tests were two-sided; we considered P<0.05 significant, and analyses were performed using Stata/SE 13.1 (Stata Corp., College Station, TX, USA).
Results
Individuals (n=19) were excluded from our analyses due to missing data on any of the following: OFC (n=14), US/LS ratio (n=11), or arm span (n=9). The remaining 110 participants comprised the analytic dataset. Cohort demographics are described in Supplemental Table 1.
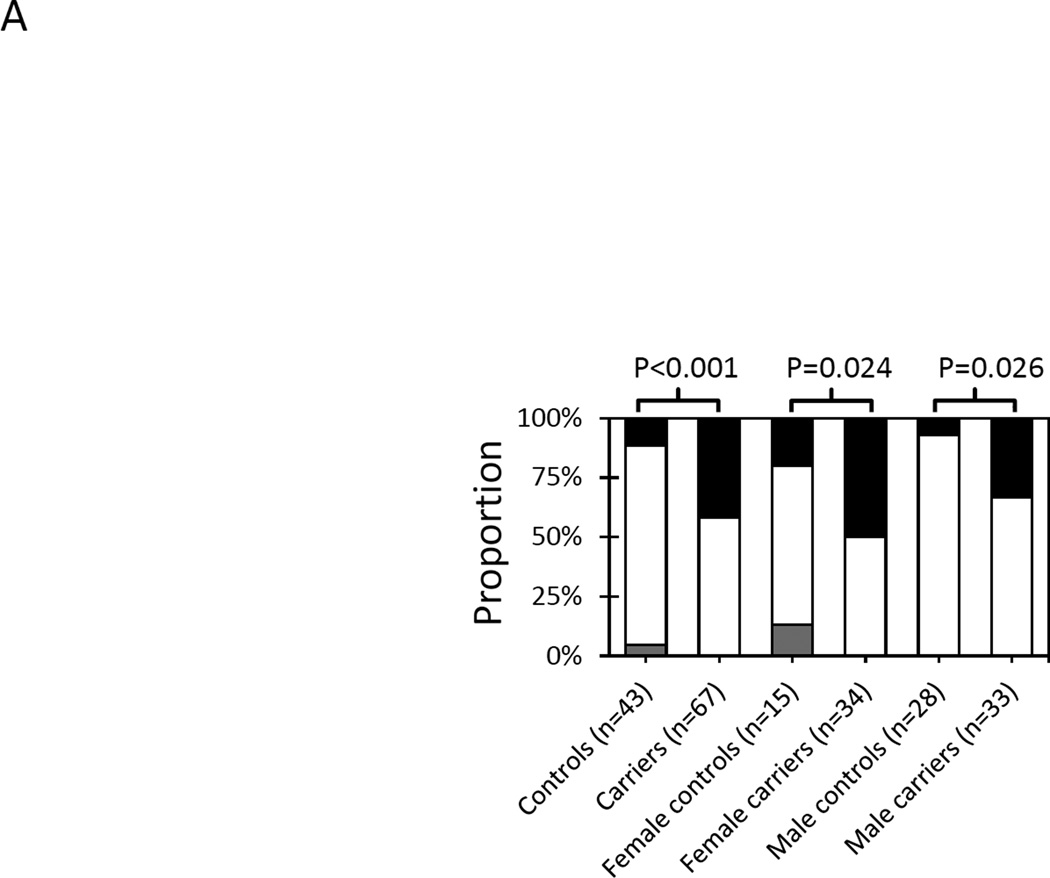
Macrocephaly was more frequent in DICER1-carriers compared with family controls
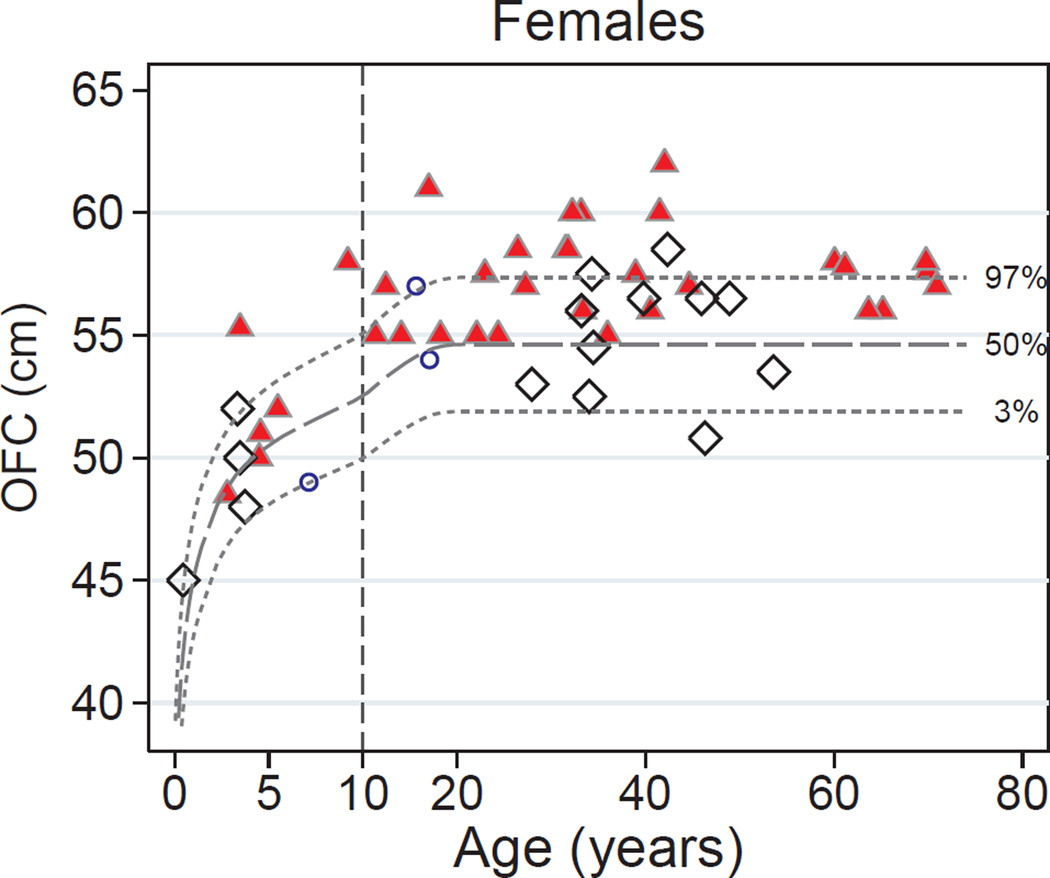
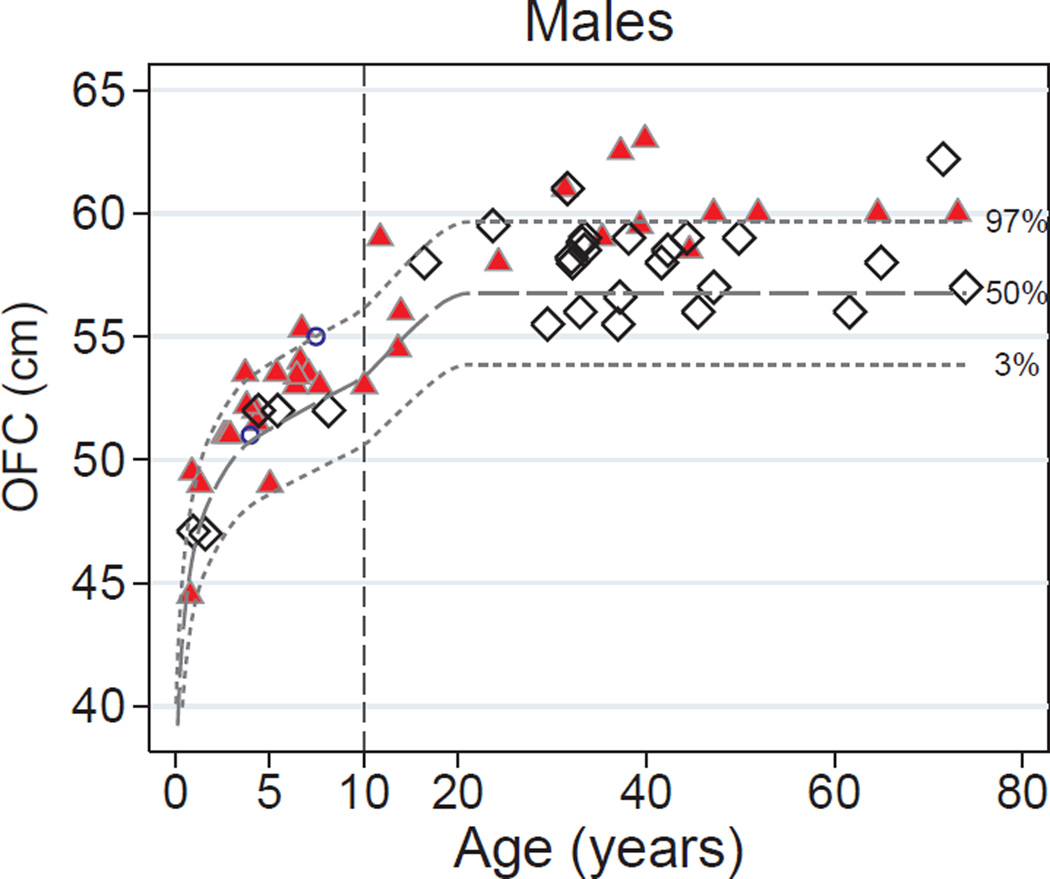
DICER1-carriers differed from family controls in the distribution of head circumference (Figure 1A): 28 DICER1-carriers (42%) were macrocephalic, and none had an OFC below the 3rd centile, versus family controls, of whom five were macrocephalic (12%) and two had OFC below the 3rd centile (5%) (P<0.001). This difference between DICER1-carriers and controls remained significant after stratification by gender. Seventeen females with a DICER1 mutation (50%) were macrocephalic, and none had an OFC below the 3rd centile, versus three controls with macrocephaly (20%) and two with OFC <3rd centile (13%) (P=0.024). Similarly, 11 males with a DICER1 mutation (33%) were macrocephalic compared with only two controls (7%) (P=0.026). When plotted against the reference curves published in Rollins et al.14, OFC was systematically increased in DICER1-carriers compared with both population norms and family controls (Figure 1B–C). Among those age ≥ 18 years, DICER1-carriers had a 2.25 cm increase in OFC (95% CI=1.2 - 3.3; P<0.001), after adjusting for gender. We did not estimate the magnitude of the increase in children because the small number of pediatric controls precluded modeling of the non-linear relationship between age and OFC. However, 8 DICER1-carriers age < 18 years (25%) were macrocephalic compared with one control age < 18 years (10%), though the difference was not statistically significant (P=0.219). The five children with a DICER1-associated tumor but no detectable DICER1 germline mutation had a distribution of OFC similar to that of family controls (Figure 1B–C). OFC did not correlate with DICER1 mutation location or type (Supplemental Figure S1 and Supplemental Table S2).
Figure 1.
Occipital-frontal circumference-for-age in the DICER1 syndrome. (A) Abnormal OFC-for-age. Proportions between the 3rd and 97th centiles (white), below the 3rd centile (gray), or above the 97th centile (black) in DICER1 mutation carriers and family controls. P values are for Fisher’s exact test of differences between groups. (B) Females. Red triangles indicate DICER1-mutation carriers. White diamonds represent family controls. Blue circles represent girls without a detectable germline DICER1 mutation but who harbor a DICER1-associated tumor (7-year-old: type II PPB; 15.5-year-old: Sertoli-Leydig cell tumor; 17-year-old: type II PPB). The dashed lines indicate the 97th, 50th, and 3rd centiles of OFC-for-age reported in Rollins, 2010. The vertical dashed line at age 10 years indicates a change in the scale of the x-axis to allow for better resolution of children’s values. (C) Males. Blue circles represent boys without a detectable germline DICER1 mutation but who harbor at least one DICER1-associated tumor (4-year-old: type I PPB and cystic nephroma; 7.7-year-old: type II PPB only). OFC = occipital-frontal circumference.
There were no differences in height between DICER1-carriers and controls
Although DICER1 mutation carriers were taller than familial controls after controlling for gender (P=0.048), the proportion of individuals with height >97th general population centile was similar between DICER1-carriers (12%) and controls (7%) (P=0.52) (data not shown). Tall stature was not more prevalent in either females (P=0.414) or males (P=1.0) with the DICER1 syndrome. The DICER1 syndrome in adults was not associated with greater height after adjusting for gender (difference=2.5cm, 95% CI=−1.0 – 6.1; P=0.160).
Larger head circumference in DICER1-carriers was independent from differences in height
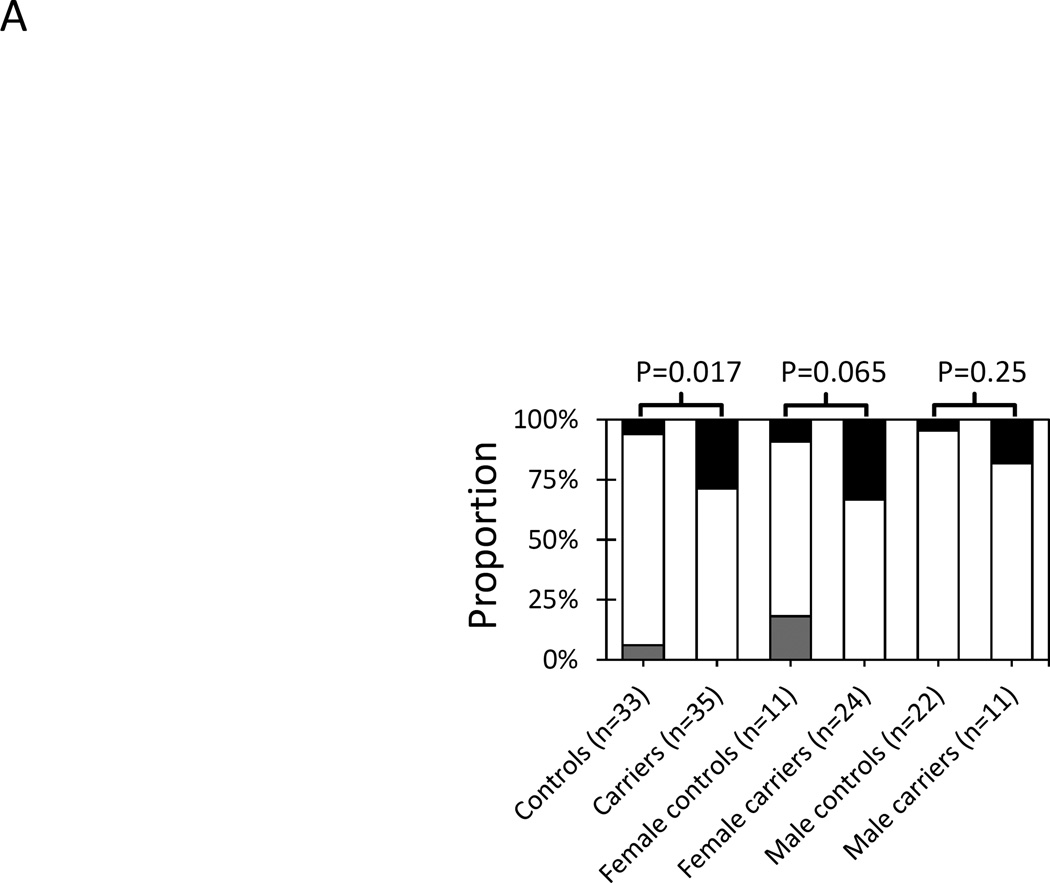
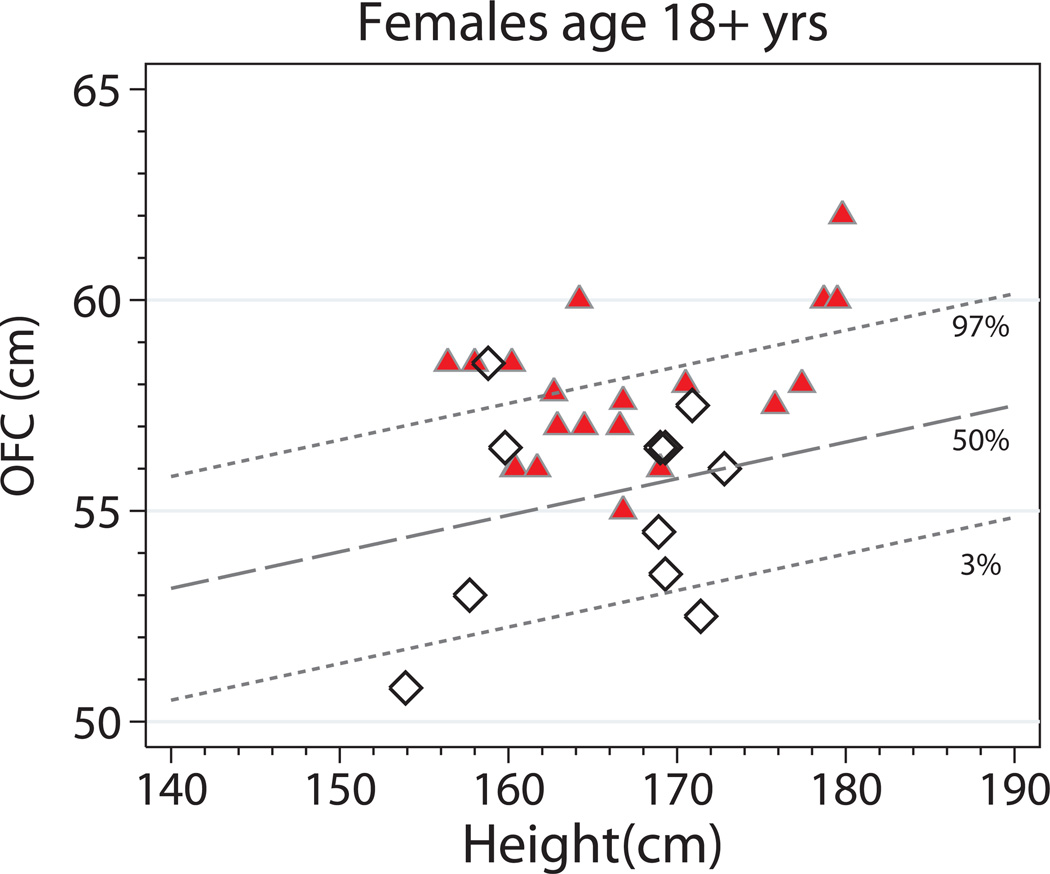
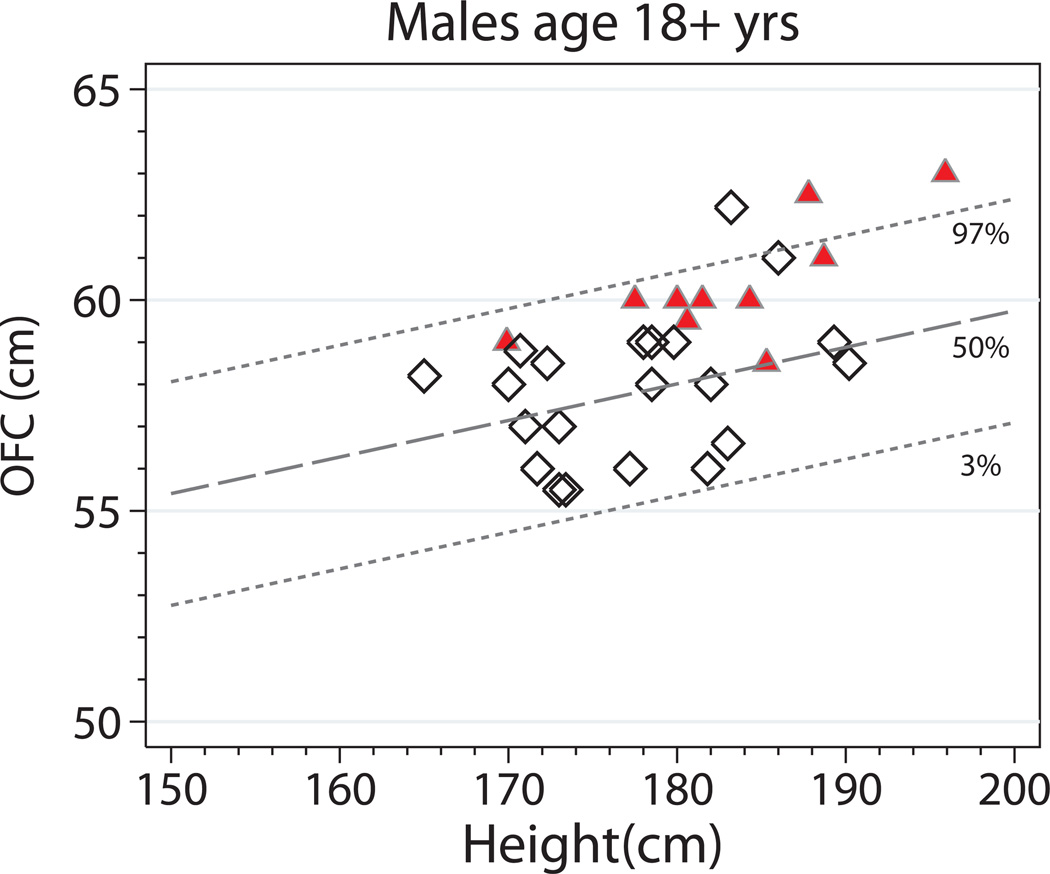
As noted above, OFC and height are strongly correlated in the general population. Using the reference curves from Bushby et al.15 that adjust for height among those age ≥16 years, the distribution of OFC-for-height among adults (age ≥18 years) with DICER1 differed significantly from that of family controls (Figure 2A). Ten adults with the DICER1 syndrome (29%) had an OFC > 97th centile and none had an OFC <3rd centile, versus two controls with OFC > 97th centile (6%) and two controls with OFC <3rd centile (6%) (P=0.017). Stratifying by gender did not detect significant differences between groups. Eight women with DICER1 syndrome (33%) had an OFC>97th centile and none with OFC <3rd centile compared with one woman control (9%) with OFC>97th centile and two (18%) with OFC <3rd centile (P=0.065). Two males with the DICER1 syndrome had OFC >97th centile (18%) compared with one male control (5%) (P=0.25). Qualitatively, OFC-for-height in DICER1-carriers was larger than expected (Figure 2B–C). Among adults, the DICER1 syndrome was associated with an average increase in OFC of 1.92 cm (95% CI=1.1–2.8; P<0.001) after adjusting for gender and height.
Figure 2.
Occipital-frontal circumference-for-height in the DICER1 syndrome (mutation carriers and controls ≥ 18 years). (A) Abnormal head circumference-for-height. Proportions between the 3rd and 97th centiles (white), below the 3rd centile (gray), or above the 97th centile (black) in DICER1 mutation carriers and family controls. P values are for Fisher’s exact test of differences between groups. (B) Females. Red triangles indicate DICER1 mutation carriers. White diamonds represent family controls. The dashed lines indicate the 97th, 50th, and 3rd centiles of OFC-for-height reported in Bushby et al., 1992. (C) Males. OFC = occipital-frontal circumference.
Arm span/height ratio and long bone growth in the DICER1 syndrome were proportional
No significant differences in the US/LS or arm span/height ratios were observed. The US/LS ratio of DICER1-carriers (mean = 0.977; SD=0.087) was similar to that of family controls (mean=0.950; SD=0.087) (P=0.443) among those age 18 years and older. The relationship between arm span and height were linear, as is expected in the general population, and no significant differences were observed between DICER1-carriers (mean=1.022; SD=0.043) and controls (mean= 1.024; SD=0.028) (P=0.747). Neither adjustment for gender or age meaningfully affected the results (data not shown).
Discussion
In our study, macrocephaly was observed in 42% of DICER1-carriers evaluated at the NIH CC. Other growth measurements were normal relative to the general population, i.e., DICER1-carriers were not abnormally tall, but adults with DICER1 were taller on average compared with family controls. After adjusting for these differences in height, the association between macrocephaly and DICER1 mutation status persisted. Measurements of long bone growth (arm span/height and US/LS ratios) were within normal ranges.
In mice Dicer1 is a haploinsufficient tumor-suppressor gene16; our data show for the first time that human macrocephaly is a phenotype significantly associated with DICER1 haploinsufficiency. In the DICER1 syndrome, the macrocephaly is relatively (but not disproportionately) increased and is not associated with somatic overgrowth17. Klein et al. reported macrocephaly and symmetric overgrowth in two children with mosaic missense “hotspot” mutations in the RNase IIIb domain of DICER1, along with developmental delay and Wilms tumor, in a constellation of findings they termed the “GLOW” (Global developmental delay, Lung cysts, Overgrowth and Wilms tumor) syndrome10. The authors also identified ten candidate dysregulated 3p microRNAs that target negative regulators of the mTOR, TGF-β and MAPK signaling pathways, including PTEN, TSC and NF1. They hypothesize that an imbalance in specific 3p microRNAs arising from the DICER1 RNase IIIb mutations lead to excessive cell and tissue growth and tumor predisposition. Mosaic DICER1 RNase IIIb domain mutations are associated with a more severe neoplastic phenotype11,18. Many of the “GLOW” phenotype features, including macrocephaly and overgrowth, were not observed in a set of four patients with mosaic DICER1 RNase IIIb mutations11. The differences in these studies may be attributable to the pleiotropy and phenotypic variability inherent in mosaicism and highlight the need for a systematic, statistically-grounded approach to syndrome delineation.
It is well-known that haploinsufficiency of PTEN (Cowden, Bannayan-Riley-Ruvalcaba syndromes) and NF1 (neurofibromatosis type 1) is associated with macrocephaly. It is interesting to note that these genes are also dysregulated in DICER1 mosaicism10. Increased head circumference in NF1 is hypothesized to be a secondary skeletal manifestation of brain overgrowth19, presumably due to dysregulation of key growth pathways. The often-pronounced macrocephaly in these disorders can be a useful clinical clue to their diagnosis. The role of these genes as intermediaries of posited brain overgrowth with secondary skeletal growth in the DICER1 syndrome phenotype merits further study.
Our analysis is limited by the biases inherent in using cross-sectional data to assess growth. Longitudinal analyses are needed to discern when OFC increases, and would inform future studies into the underlying mechanism of this growth. Moreover, families enrolled in the study were accessioned because of a history of a DICER1-associated tumor. Ascertainment bias may have missed clinically asymptomatic DICER1-carriers with milder phenotypes. Lastly, measurements were made by multiple observers rather than a single physician. However, the measurements of OFC, arm span, and height are unlikely to vary substantially enough between observers to account for the large difference observed in DICER1-carriers in this study.
In summary, our study is the first to document macrocephaly as a non-neoplastic feature of the DICER1 syndrome. Further analyses of longitudinal data may shed light on the developmental processes underlying the macrocephaly, and point to the role of DICER1 in auxology. Like other better-known tumor-predisposition disorders, macrocephaly may be a useful, if subtle, clinical clue to the diagnoses of the DICER1 syndrome.
Supplementary Material
Acknowledgments
We thank D. Ashley Hill, MD (Children’s National Medical Center, Washington, DC) for DICER1 sequencing. This work was supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics of the National Cancer Institute, Rockville, MD.
Footnotes
Disclosure Statement: The authors have no conflicts of interest to disclose.
References
- 1.Dishop MK, Kuruvilla S. Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children's hospital. Arch Pathol Lab Med. 2008;132(7):1079–1103. doi: 10.5858/2008-132-1079-PAMLTI. [DOI] [PubMed] [Google Scholar]
- 2.Hill DA, Ivanovich J, Priest JR, et al. DICER1 mutations in familial pleuropulmonary blastoma. Science. 2009;325(5943):965. doi: 10.1126/science.1174334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pugh TJ, Yu W, Yang J, et al. Exome sequencing of pleuropulmonary blastoma reveals frequent biallelic loss of TP53 and two hits in DICER1 resulting in retention of 5p-derived miRNA hairpin loop sequences. Oncogene. 2014 doi: 10.1038/onc.2014.150. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart DR, Messinger Y, Williams GM, et al. Nasal chondromesenchymal hamartomas arise secondary to germline and somatic mutations of DICER1 in the pleuropulmonary blastoma tumor predisposition disorder. Hum Genet. 2014;133(11):1443–1450. doi: 10.1007/s00439-014-1474-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doros L, Schultz KA, Stewart DR, et al. DICER1-related disorders. In: Pagon RA, editor. GeneReviews. Seattle (WA): University of Washington; 2014. [Google Scholar]
- 6.Messinger YH, Stewart DR, Priest JR, et al. Pleuropulmonary blastoma: a report on 350 central pathology-confirmed pleuropulmonary blastoma cases by the International Pleuropulmonary Blastoma Registry. Cancer. 2015;121(2):276–285. doi: 10.1002/cncr.29032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Priest JR, Magnuson J, Williams GM, et al. Cerebral metastasis and other central nervous system complications of pleuropulmonary blastoma. Pediatr Blood Cancer. 2007;49(3):266–273. doi: 10.1002/pbc.20937. [DOI] [PubMed] [Google Scholar]
- 8.Schultz KA, Harris A, Williams GM, et al. Judicious DICER1 testing and surveillance imaging facilitates early diagnosis and cure of pleuropulmonary blastoma. Pediatr Blood Cancer. 2014;61(9):1695–1697. doi: 10.1002/pbc.25092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rath SR, Bartley A, Charles A, et al. Multinodular Goiter in children: an important pointer to a germline DICER1 mutation. The Journal of clinical endocrinology and metabolism. 2014;99(6):1947–1948. doi: 10.1210/jc.2013-3932. [DOI] [PubMed] [Google Scholar]
- 10.Klein S, Lee H, Ghahremani S, et al. Expanding the phenotype of mutations in DICER1: mosaic missense mutations in the RNase IIIb domain of DICER1 cause GLOW syndrome. J Med Genet. 2014;51(5):294–302. doi: 10.1136/jmedgenet-2013-101943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Kock L, Wang YC, Revil T, et al. High-sensitivity sequencing reveals multi-organ somatic mosaicism causing DICER1 syndrome. J Med Genet. 2016;53(1):43–52. doi: 10.1136/jmedgenet-2015-103428. [DOI] [PubMed] [Google Scholar]
- 12.Gripp KW, Slavotinek AM, Hall JG, Allanson JE. Handbook of Physical Measurements. Oxford: Oxford University Press; 2013. [Google Scholar]
- 13.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 14.Rollins JD, Collins JS, Holden KR. United States head circumference growth reference charts: birth to 21 years. J Pediatr. 2010;156(6):907–913. doi: 10.1016/j.jpeds.2010.01.009. 913 e901-902. [DOI] [PubMed] [Google Scholar]
- 15.Bushby KM, Cole T, Matthews JN, Goodship JA. Centiles for adult head circumference. Arch Dis Child. 1992;67(10):1286–1287. doi: 10.1136/adc.67.10.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar MS, Pester RE, Chen CY, et al. Dicer1 functions as a haploinsufficient tumor suppressor. Genes Dev. 2009;23(23):2700–2704. doi: 10.1101/gad.1848209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein S, Sharifi-Hannauer P, Martinez-Agosto JA. Macrocephaly as a clinical indicator of genetic subtypes in autism. Autism Res. 2013;6(1):51–56. doi: 10.1002/aur.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brenneman MA, Field A, Yang J, et al. Temporal order of RNase IIIb and loss-of-function mutations during development determines phenotype in DICER1 syndrome: a unique variant of the two-hit tumor suppression model. F1000 Research. 2015;4:214. doi: 10.12688/f1000research.6746.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedman JM, Gutmann DH, MacCollin M, Riccardi VM, editors. Neurofibromatosis: Phenotype, Natural History and Pathogenesis. Third. Baltimore: Johns Hopkins University Press; 1999. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.