Abstract
Objectives:
This study aimed to assess the effect of voxel size and object location in the field of view (FOV) on diagnostic accuracy of cone beam computed tomography (CBCT) for detection of simulated bone defects.
Materials and Methods:
In this in vitro study, bone defects were drilled in four sections of a dry human mandible. Bone blocks were fixed on a platform parallel to the horizontal plane and CBCT images were acquired using 0.2mm and 0.3mm resolutions and five locations of FOV (anterior, posterior, left, right and center). Three reviewers viewed the images twice and the presence or absence of simulated bone defects was determined in positive and negative cases.
Results:
Sensitivity in different locations of FOV ranged between 0.25–1.0 and 0.75–1.0 in low and high resolutions, respectively. These values were 0.625–1.0 and 0.69–1.0, respectively for specificity. Intra-observer agreements were in the range of 0.84–1.0 and 0.75–1.0 and inter-observer agreements were in the range of 0.3–0.61 and 0.46–0.69 in high and low resolutions, respectively. The highest sensitivity was seen at the center of the FOV and with an increase in resolution from 0.3mm to 0.2mm, the sensitivity increased specially in the posterior region of the FOV while image resolutions and FOV locations did not affect specificity.
Conclusions:
The highest sensitivity values were obtained at the center of the FOV and lowest values were seen in images acquired in the posterior region in low resolution. Diagnostic accuracy improved with increased resolution.
Keywords: Bone and Bones, Sensitivity and Specificity, Cone-Beam Computed Tomography
INTRODUCTION
Cone beam computed tomography (CBCT) is currently a valuable imaging modality with numerous applications in dental implant treatment, endodontic therapy, surgery, orthodontic assessment and evaluation of pathological lesions [1]. The effects of factors such as system resolution and voxel size are undeniable on diagnostic accuracy of images, and there is the possibility of using a smaller voxel size to increase image resolution. However, use of a smaller voxel size to increase the resolution can create noise [2], and thus, significant improvement in the diagnostic value of images may not occur. Also, the scanning time of objects becomes longer by increasing the resolution, the radiation dose increases and there would be higher risk of movement of patient during imaging [3]. Field of view (FOV) refers to the scan volume of a particular CBCT unit. A “voxel” describes the smallest distinguishable box-shaped part of a three-dimensional image. Lowering the resolution may reduce the quality of images, increase noise and artifacts, and reduce the amount of anatomical information of the target areas [2].
Multiple factors such as FOV, voxel size and the number of basis projections and image artifacts significantly affect the CBCT image quality [4]. In most cases, larger FOV decreases resolution due to larger voxels in fixed number of pixels [5]. Previous studies have reported inconsistencies in CBCT measurements depending on the position of object within the FOV [6,7]. The accuracy of linear measurements is lower at the periphery compared to the center of the FOV in CBCT [8,9].
Because of the lack of any current protocol on selection of appropriate voxel size [10] and also the proper location within the FOV for CBCT imaging in dentistry, the present study was conducted to assess the effects of voxel size (resolution) and the location of bone defects in different regions of the FOV on diagnostic accuracy of CBCT for their detection.
MATERIALS AND METHODS
Four pieces of human mandible were selected after soft tissue removal and fixed in formalin. Bone defects with 1×1mm dimensions were drilled using high speed handpiece with a round bur in cortical bone. Bone blocks were then fixed on a platform, which was parallel to the horizontal plane of the CBCT unit; CBCT images of bone defects were obtained using Alphard-3030 unit (Asahi Roentgen Ind. Co., Ltd., Kyoto, Japan) operating at 4mA, 80kVp and 17s time in two different resolutions and five locations in the FOV (Fig. 1). Bone defects were not created in the mandible of the negative (healthy bone) cases (a total of eight cases) and thus CBCT images were obtained only from healthy bone under the same experimental conditions (i.e. five locations in the FOV at both high and low resolutions). Locations in the FOV were center, left, right, anterior and posterior, and resolutions used for CBCT imaging included high resolution (mode I: 0.2mm voxel size, 10×10cm FOV) and low resolution (mode P: 0.3mm voxel size, 15×15cm FOV) (Figs. 2 and 3). Three observers evaluated the images using the same display monitor and Romexis® software (Planmeca, Helsinki, Finland), and then information was recorded in the relevant forms.
Fig. 1:
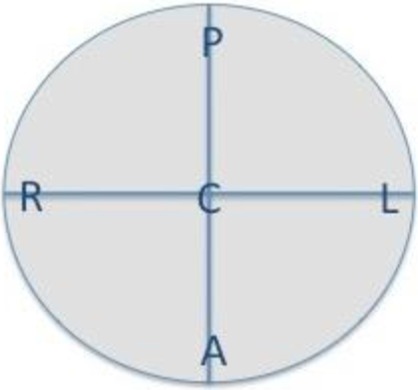
The bone blocks were scanned at five different areas within the field of view of the CBCT system A: Anterior; C: Center; L: Left; R: Right; P: Posterior
Fig. 2:
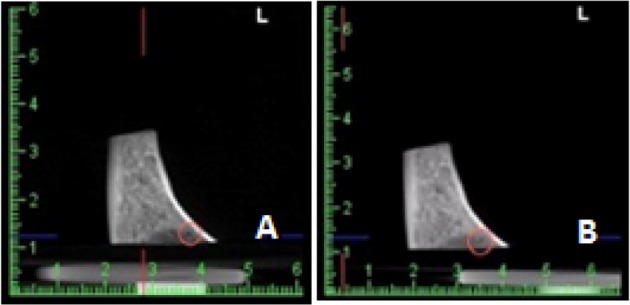
CBCT scan obtained with 0.2mm voxel size of a mandibular bone defect; (A) Center of the field of view; (B) Posterior region of the field of view
Fig. 3:
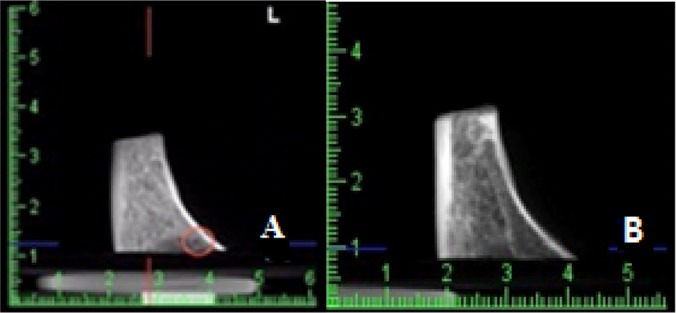
CBCT scan obtained with 0.3mm voxel size of a mandibular bone defect; (A) Center of the field of view, (B) Posterior region of the field of view
In the first session, the observers were trained to record the information in the relevant forms. Then, each sample was coded and the images were randomly presented to the observers. The ability to detect bone defects was assessed using a dichotomous scale (seen and not seen). The second session of observation was held after 10 days. The images were coded again and randomly shown to the observers; the related information was recorded. Detection of bone defects (seen and not seen) was determined in positive cases (bone defects) and negative cases (healthy bone) based on the opinion of the observers; the frequency of observations, high and low resolutions, and the location of object in the FOV, and reported using number and percentage. Diagnostic indices including sensitivity, specificity and 95% confidence interval were also calculated. Intra- and inter-observer agreements for the detection of bone defects were calculated at different resolutions and locations in the FOV using the Kappa test.
RESULTS
The sensitivity, specificity and 95% confidence interval values are presented in Tables 1 to 3. The sensitivity value was higher in high-resolution CBCT images. The highest sensitivity was found in the central region in both high and low resolutions, which was significantly different from other FOV regions at 95% confidence level using the Wilson formula. Also, the least sensitivity was recorded in the posterior region of the FOV at low resolution and significantly increased by increasing the resolution (Table 1). Resolution of images (0.3mm and 0.2mm) and FOV regions had insignificant effects on the specificity values; because it was observed that the values were almost the same in all three observers in two resolutions and five different regions (Table 2). The value of inter-observer agreement in different FOV regions was 0.3 to 0.69 in high-resolution images and 0.46 to 0.69 in low-resolution images, and the lowest value was obtained in the posterior region in high resolution (0.3). The highest value was obtained at the center of the FOV in both resolutions (0.69). The intra-observer agreement coefficients for all groups were adequately high (kappa≥0.75).
Table 1:
Sensitivity for detection of simulated bone defects at different object locations in the field of view (FOV) and two different resolutions of CBCT
| Object location in the FOV | Observer 1 | Observer 2 | Observer 3 | |||
|---|---|---|---|---|---|---|
| High resolution | Low resolution | High resolution | Low resolution | High resolution | Low resolution | |
| Anterior | 1 | 0.75 | 1 | 0.625 | 0.75 | 0.25 |
| Posterior | 0.75 | 0 | 0.75 | 0 | 0.875 | 0 |
| Left | 0.75 | 0.75 | 1 | 0.625 | 0.75 | 0.75 |
| Right | 0.875 | 0.625 | 1 | 0.625 | 1 | 0.75 |
| Center | 1 | 1 | 1 | 1 | 0.875 | 1 |
Table 3:
Mean (95% confidence interval) of simulated bone defects measured at different object locations in the field of view (FOV) and two different resolutions of the CBCT system
| Object location in the FOV | High resolution (0.2 mm) | Low resolution (0.3 mm) |
|---|---|---|
| Anterior | 0.82 (0.76–0.88) | 0.625 (0.54–0.71) |
| Posterior | 0.75 (0.68–0.82) | 0.02 (0–0.04) |
| Left | 0.875 (0.82–0.93) | 0.75 (0.68–0.82) |
| Right | 0.875 (0.82–0.93) | .625 (0.54–0.71) |
| Center | 0.98 (0.96–1) | 0.98 (0.96–1) |
Table 2:
Specificity for detection of simulated bone defects at different object locations in the field of view (FOV) and two different resolutions of CBCT system
| Object location in the FOV | Observer 1 | Observer 2 | Observer 3 | |||
|---|---|---|---|---|---|---|
| High resolution | Low resolution | High resolution | Low resolution | High resolution | Low resolution | |
| Anterior | 1 | 1 | 0.625 | 0.75 | 0.625 | 0.75 |
| Posterior | 1 | 1 | 0.69 | 0.82 | 0.625 | 0.75 |
| Left | 1 | 1 | 0.69 | 0.94 | 0.625 | 0.75 |
| Right | 1 | 1 | 0.75 | 1 | 0.625 | 0.75 |
| Center | 1 | 1 | 0.625 | 0.94 | 0.625 | 0.69 |
DISCUSSION
According to the results of this study, some variations were observed in the diagnostic accuracy of CBCT for bone defect detection in positive and negative cases during scanning in different regions of the FOV. Although the sensitivity significantly decreased in CBCT images with the object in the posterior region of the FOV in low resolution, it increased in high resolution, especially in the posterior region. High sensitivity was observed by increasing the resolution of CBCT images from 0.3mm to 0.2mm; and the values were significantly higher at the center of the FOV compared to other regions in both high and low resolutions at 95% confidence interval using the Wilson formula. In a study by Ibrahim et al, [4] in 2014 on the effects of different locations of object in the FOV in two CBCT systems, a significant difference in trabecular bone microstructure measurements in the central region was found relative to the peripheral areas in the FOV in NewTom system, but this difference was not significant in the Accuitomo system, which may be due to differences between the two systems. The inherent artefacts of the system and the object region in a limited FOV could also result in deviations of measurements. These factors increase the linear measurement values at the periphery compared to the central region of the FOV of the CBCT system [8,9]. In the current study, defects were observed best at the center of the FOV and had statistically significant difference with object in other regions. This may be because of the increased beam intensity in the central region. The non-uniformity of the beam intensity causes inconsistency in grey values within the CBCT FOV, in which it is relatively higher at the center than at the peripheral regions. A higher quality image can be obtained with the object at the center. In the current study, the lowest sensitivity was observed in the posterior region of the FOV in low resolution, which could be due to under-sampling from the posterior region of the FOV compared to other regions because of of device limitations. Variations in diagnostic parameters with the object in different regions of the FOV have also been observed in high-resolution peripheral CT and multislice CT [11]. Voxel size [12], contrast-to-noise ratio [13] and image artifacts are among the factors associated with the FOV. A small voxel size [14] with a small FOV [15] is generally recommended to improve diagnostic accuracy. Variations in the quality of images of bone defects in different FOVs and resolutions may be attributed to increased image artefacts particularly in smaller FOVs [12,13]. Also, an image with a bigger voxel and a higher contrast-to-noise ratio can have a higher resolution than an image with a smaller voxel and lower contrast-to-noise ratio [14]. Therefore, while the selection of voxel size depends on the nature of the diagnostic task, the clinician should be aware of the variations of resolution and selected FOV regions. Although CBCT has been reported as a precise technique for assessment and detection of bone defects, some limitations of the systems should be well acknowledged.
Based on the results, the observer’s performance with regard to CBCT images taken at high resolution was estimated to be better than that with images with low resolution; thus, the sensitivity values improved by increasing the resolution of CBCT images from 0.3mm to 0.2mm; and the frequency of correct diagnoses increased in both positive and negative cases. By rotation of X-ray beam around the patient’s head in CBCT scanners, a cylindrical volume is acquired. The size of FOV is variable for different CBCT devices [16,17]. The selected FOV should provide the necessary information for diagnosis and treatment planning. However, as patients vary in size, the FOV parameter would be different as well. In addition, the selected FOV remains the most important scanning parameter in limiting the radiation dose and image quality [18]. Theoretically, more uniform images can be obtained in the maxillofacial region due to high-density structures. Substantial amount of scattered beams is produced in CBCT technique that negatively affects the image quality [19]. Scattered radiation affects low-density structures more than maxillofacial regions. In selected smaller FOVs, anatomical structures located outside the defined area are imaged by the detector, and since only a small imaging range evaluates the tissue, the resulting images will not be uniform [20,21].
Kwong et al, [22] in 2008 used 6-inch FOV and showed that the resultant images had the highest resolution and the lowest voxel size; although high resolution alone does not necessarily mean higher image quality. Different FOVs contain various voxel sizes and CBCT devices also vary in voxel size for each FOV.
Hassan et al, [12] in 2010 showed that voxels larger than 0.6, 0.9, or 1.2 mm in the x and y plane significantly reduced the visibility of occlusal surfaces of the teeth, interproximal spaces between the teeth and alveolar bone; whereas, the choice of larger voxels reduces the image noise [23]. Factors such as voxel size in imaging, exposure factors, various applied FOVs, slice thickness, imaging systems and detectors are effective in diagnostic results [24]. These parameters vary between the CBCT units and different imaging protocols in the same unit [25].
Although short scanning time and low patient radiation dose are important factors in diagnostic imaging, risk of misdiagnosis and consequent complications should also be taken into account. In general, voxel size should be determined based on the severity of patient’s condition and treatment plan.
Image quality variations can be reduced or increased by altering the FOV, and the image reconstruction parameters and post-processing methods are studied based on the type of CBCT system used. The selected FOV for CBCT images is directly related to voxel size and affects the resolution and contrast. Extended FOV creates lower contrast and resolution compared to smaller FOV and thus directly affects the detection of anatomical structures on CBCT images [26]. In accordance with the results of the current study, FOV position seems to have little impact on diagnostic specificity because the values were more or less the same in all three observers at five different positions. Appropriate diagnostic accuracy of CBCT images for bone defects in the FOV and different resolutions in this study may be related to adequate ability and skills of the observers, good quality of CBCT scans and lack of motion artifacts in images. In this study, bone defects caused by drilling had distinctive and appropriate form, enhancing their detection by the observers.
Also, Kamburoglu et al, [27] in 2014 reported the same performance of observers in detection of simulated buccal peri-implant defects using different parameters of FOV and various resolutions. In another study, no difference was observed in diagnostic accuracy of CBCT images for detection of simulated buccal peri-implant defects with and without pattern artifact reduction in Planmeca ProMax system [28]. Pattern artifact reduction was not used in this study or in the study by Kamburoglu et al, [27] in 2014. According to the results of the current study, the sensitivity for detecting bone defects by the observers and the frequency of detection was in the range of 0.25–1 in low resolution and 0.875–1 in high resolution at different FOV regions, showing that sensitivity was enhanced by increasing the resolution. On the other hand, the specificity value was between 0.75 and 1 for high-resolution images and 0.69–1 for low-resolution images. In the study by Hedesiu et al, [29] in 2012, sensitivity for diagnosis of apical defects in CBCT scans was estimated to be 0.72–0.8 and specificity was between 0.6–0.77. However, higher levels (a rate of 1) of sensitivity and specificity for CBCT system were recorded in examining the human mandible by Patel et al, [30] in 2009. The sensitivity parameter for CBCT images in the study by Patel et al, [31] in 2014 was in the range of 79.2%–91.7%. Significant effects of resolution on sensitivity were not observed in the current study, which is different from the results of the above-mentioned studies. In total, the highest sensitivity was recorded in the central position in both high and low resolutions; increased resolution generally led to improved sensitivity especially in the posterior region of the FOV, but had no effect on specificity. The FOV parameter in CBCT should be adjusted to reduce patient radiation exposure for detection of bone defects. Concerning some false-positive results in the negative cases, CBCT should be used as an adjunct to clinical examination to make a correct diagnosis and for treatment planning. If the diagnostic purpose can be achieved by minimum radiation dose in the FOV, there is no need to change this parameter or increase the absorbed dose of patient.
CONCLUSION
Improving the CBCT image resolution from 0.3mm to 0.2mm increased the sensitivity values for detection of simulated bone defects. Image resolution and position of the object in the FOV seem to have little impact on specificity values. Also, comparison of different FOV regions revealed that the highest sensitivity rates were recorded in the central position in both high and low resolutions, and sensitivity significantly decreased in the posterior position at low resolution
REFERENCES
- 1-.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006. February;72(1):75–80. [PubMed] [Google Scholar]
- 2-.Swennen GR, Schutyser FA, Hausamen JE, editors. Three-dimensional cephalometry: a color atlas and manual. Heidelberg, Springer Science & Business Media, 2005:97–100. [Google Scholar]
- 3-.Damstra J, Fourie Z, Slater JJ, Ren Y. Accuracy of linear measurements from cone-beam computed tomography-derived surface models of different voxel sizes. Am J Orthod Dentofacial Orthop 2010. January;137(1):16–e1. [DOI] [PubMed] [Google Scholar]
- 4-.Ibrahim N, Parsa A, Hassan B, van der Stelt P, Aartman IHA, Nambiar P. Influence of object location in different FOVs on trabecular bone micro-structure measurements of human mandible: a cone beam CT study. Dentomaxillofac Radiol 2014. January;43(2):20130329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5-.White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th Ed Amsterdam, Elsevier Health Sciences, 2014:185–97. [Google Scholar]
- 6-.Bryant JA, Drage NA, Richmond S. Study of the scan uniformity from an i-CAT cone beam computed tomography dental imaging system. Dentomaxillofac Radiol. 2008. October;37(7):365–74. [DOI] [PubMed] [Google Scholar]
- 7-.Nackaerts O, Maes F, Yan H, Couto Souza P, Pauwels R, Jacobs R. Analysis of intensity variability in multi-slice and cone beam computed tomography. Clin Oral Implants Res. 2011. August;22(8):873–9. [DOI] [PubMed] [Google Scholar]
- 8-.Nithiananthan S, Schafer S, Uneri A, Mirota DJ, Stayman JW, Zbijewski W, et al. Demons deformable registration of CT and cone-beam CT using an iterative intensity matching approach. Med Phys 2011. April;38(4):1785–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9-.Tsutsumi K, Chikui T, Okamura K, Yoshiura K. Accuracy of linear measurement and the measurement limits of thin objects with cone beam computed tomography: effects of measurement directions and of phantom locations in the fields of view. Int J Oral Maxillofac Implants. 2011. Jan-Feb;26(1):91–100. [PubMed] [Google Scholar]
- 10-.Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging. 2013. August;26(4):813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11-.Tjong W, Kazakia GJ, Burghardt AJ, Majumdar S. The effect of voxel size on high-resolution peripheral computed tomography measurements of trabecular and cortical bone microstructure. Med Phys 2012. April;39(4):1893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12-.Hassan B, Couto Souza P, Jacobs R, de Azambuja Berti S, van der Stelt P. Influence of scanning and reconstruction parameters on quality of three-dimensional surface models of the dental arches from cone beam computed tomography. Clin Oral Investig 2010. June;14(3):303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13-.Bechara B, McMahan CA, Moore WS, Noujeim M, Geha H, Teixeira FB. Contrast-to-noise ratio difference in small field of view cone beam computed tomography machines. J Oral Sci. 2012. September;54(3):227–32. [DOI] [PubMed] [Google Scholar]
- 14-.Vandenberghe B, Luchsinger S, Hostens J, Dhoore E, Jacobs R, SEDENTEXCT Project Consortium The influence of exposure parameters on jawbone model accuracy using cone beam CT and multislice CT. Dentomaxillofac Radiol. 2012. September;41(6):466–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15-.Librizzi ZT, Tadinada AS, Valiyaparambil JV, Lurie AG, Mallyad SM. Cone-beam computed tomography to detect erosions of the temporomandibular joint: Effect of field of view and voxel size on diagnostic efficacy and effective dose. Am J Orthod Dentofacial Orthop 2011. July;140(1):e25–30. [DOI] [PubMed] [Google Scholar]
- 16-.Hatcher DC. Operational principles for cone-beam computed tomography. J Am Dent Assoc. 2010. October;141 Suppl 3:3S–6S. [DOI] [PubMed] [Google Scholar]
- 17-.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008. October;52(4):707–30. [DOI] [PubMed] [Google Scholar]
- 18-.Farman AG. Field of view. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. October;108(4):477–8. [DOI] [PubMed] [Google Scholar]
- 19-.Endo M, Tsunoo T, Nakamori N, Yoshida T. Effect of scattered radiation on image noise in cone beam CT. Med Phys. 2001. April;28(4):469–74. [DOI] [PubMed] [Google Scholar]
- 20-.Siltanen S, Kolehmainen V, Jarvenpaa S, Kaipio JP, Koistinen P, Lassas M, et al. Statistical inversion for medical x-ray tomography with few radiographs: 1. General theory. Phys Med Biol. 2003. May 21;48(10):1437–63. [DOI] [PubMed] [Google Scholar]
- 21-.Katsevich AI. Local tomography for the limited-angle problem. J Math Anal Appl 1997. September;213(1):160–82. [Google Scholar]
- 22-.Kwong JC, Palomo M, Landers MA, Figueroa A, Hans MG. Image quality produced by different cone-beam computed tomography settings. Am J Orthod Dentofacial Orthop. 2008. February;133(2):317–27. [DOI] [PubMed] [Google Scholar]
- 23-.Salvado O, Hillenbrand CM, Wilson DL. Partial volume reduction by interpolation with reverse diffusion. Int J Biomed Imaging. 2006;2006:92092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24-.Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. Effects of image artifacts on gray-value density in limited-volume cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. December;104(6):829–36. [DOI] [PubMed] [Google Scholar]
- 25-.Costa FF, Gai BR, Umetsubo OS, Pinheiro LR, Tortamano IP, Cavalcanti MGP. Use of large-volume cone-beam computed tomography in identification and localization of horizontal root fracture in the presence and absence of intracanal metallic post. J Endod. 2012. June;38(6):856–9. [DOI] [PubMed] [Google Scholar]
- 26-.Hassan B, Metska M, Ozok A, VanderStelt P, Wesselink P. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod. 2010. January;36(1):126–9. [DOI] [PubMed] [Google Scholar]
- 27-.Kamburoglu K, Murat S, Kılıç C, Yuksel S, Avsever H, Farman A, et al. Accuracy of CBCT images in the assessment of buccal marginal alveolar peri-implant defects: effect of field of view. Dentomaxillofac Radiol. 2014;43(4):20130332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28-.Kamburoğlu K, Kolsuz E, Murat S, Eren H, Yüksel S, Paksoy CS. Assessment of buccal marginal alveolar peri-implant and periodontal defects using a cone beam CT system with and without the application of metal artefact reduction mode. Dentomaxillofac Radiol 2013. August;42(8):20130176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29-.Hedesiu M, Baciut M, Baciut G, Nackaerts O, Jacobs R, SEDENTEXCT Consortium Comparison of cone beam CT device and field of view for the detection of simulated periapical lesions. Dentomaxillofac Radiol. 2012. October;41(7):548–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30-.Patel S, Dawood A, Mannocci F, Wilson R, PittFord T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009. June;42(6):507–15. [DOI] [PubMed] [Google Scholar]
- 31-.Patel A, Tee BC, Fields H, Jones E, Chaudhry J, Sun Z. Evaluation of cone-beam computed tomography in the diagnosis of simulated small osseous defects in the mandibular condyle. Am J Orthod Dentofacial Orthop. 2014. February;145(2):143–56. [DOI] [PubMed] [Google Scholar]


