Abstract
Background
Congenital heart disease (CHD) is a common condition in children in Sub-Saharan Africa (SSA), where it is associated with poor outcomes. Diagnosis of CHD in SSA depends essentially on echocardiography, which is available only in few urban referral centers. Our aim was to assess time changes in the pattern of referral for pediatric echocardiography and the subsequent diagnosis of structural CHD in a major SSA city.
Methods
All pediatric echocardiography performed between 2004 and 2013 at the echocardiography laboratory of the Yaounde General Hospital were reviewed. The primary indication of the study and the presence of structural CHD were recorded.
Results
Between 2004 and 2013, 9,390 echocardiograms were performed and 834 (8.9%) children aged 1 day to 15 years underwent echocardiography at the center, and 227 (27.2%) cases of definite structural CHD were diagnosed, with 123 (54.2%) in boys. The most frequent indications for echocardiography were heart murmurs (40%) and the suspicion of CHD (37.4%). The commonest CHD was ventricular septal defect (VSD) (30%) with tetralogy of Fallot being the most frequent cyanotic heart lesion (5.3%). The proportion of pediatric echocardiography decreased from 13.3% in 2004–2005 to 6.1% in 2012–2013 (P=0.001) but not in a linear fashion (P=0.072 for linear trend).The diagnosis of structural CHD increased from 25.1% in 2004–2005 to 27.1% in 2012–2013. This increase however was non-significant (P=0.523) and did not follow a linear trend (P=0.230).
Conclusions
The pattern of referral for pediatric echocardiography at this center has changed over time, but diagnosis of structural CHD has remained the same. Improving access to this diagnostic procedure and subsequent treatment of diagnosed CHD will help improving the outcome of the disease in this setting.
Keywords: Echocardiography, heart disease, congenital, trends, Cameroon
Introduction
Congenital heart diseases (CHD) form a major group of diseases in children where they constitute the commonest cause of death from congenital defects (1,2). It is estimated that very few of the children with CHD reach adulthood either by ways of natural selection or as the result of successful surgical correction (1,3). In Cameroon, the prevalence of CHD in hospital-based setting among children suspected of heart diseases is estimated to range between 9.9% and 13.1% (4,5). Unlike developed countries, the developing ones have insufficient, ill-equipped and unsatisfactorily distributed health services to deal with CHD. In Sub-Saharan Africa (SSA) for instance, timely diagnosis and management of CHD is severely compromised by shortage of qualified health personnel, equipment and financial constraints. As a result, a large number of patients with CHD are undiagnosed or diagnosed with advanced disease with limited possibilities for surgical correction (6).
The significant progresses achieved in the developed world in diagnosing and treating CHD have not benefited countries across SSA at large (7,8). In this setting for instance, the definitive diagnosis of CHD still heavily relies on echocardiography, which is performed essentially in few referral urban centers. On the contrary, developed countries have witnessed advances, such as cardiac catheterization which has contributed to the progress made in the management of patients with CHD, by allowing a better understanding of normal cardiac physiology and the anatomy and pathophysiology of complex heart defects. Echocardiography is indeed considered the gold standard for the diagnosis of CHD (9). It is an accurate, noninvasive, nonionizing, painless, and relatively inexpensive diagnostic tool. The past decade has seen in Cameroon the development of important centers and collaboration focusing on early detection and surgical management of CHD at subsidized prices, while progressively building the capacity of local teams (10). The number of cardiologists in the country has increased with many having expertise in echocardiography. Against this background, we sought to determine whether patterns of referral for pediatric echocardiography and the subsequent diagnosis of structural CHD have changed between January 2004 and December 2013 in a major cardiac referral center in the Capital City, Yaounde.
Methods
Study setting
The Yaounde General Hospital is a major cardiac referral hospital in the capital city of Cameroon. The hospital receives patients referred from other health institutions nationwide for investigation and/or management of suspected heart diseases. At the end of 2013, the echocardiography department was staffed with four cardiologists, with two of them having expertise in pediatric echocardiography and CHD diagnosis.
Recruitment and data collection
The echocardiography laboratory register was surveyed for the period 2004 through 2013 to identify children aged 1 day to 15 years. Those with a definite diagnosis of a structural CHD were retained. Exclusion criterion was a repeated echocardiographic study. A repeated study was considered for children with known cardiac malformation and well-characterized defects referred for a follow-up echocardiography. Using a pre-defined questionnaire, we extracted data on the age at the time of diagnosis, sex, clinical indication for the echocardiography and the CHD diagnosed. For each year, we recorded the total number of echocardiography and the total number of pediatric echocardiography. All children referred to the unit had a cardiac exam performed followed by echocardiography. The study was approved by the institutional review board of Yaoundé General Hospital (Number: 08642014). The hospital granted authorization to access the echocardiography registers. No informed consent was required as it was a retrospective descriptive study. Information obtained from the registers was anonymized.
Statistical analysis
Data were analyzed with the use of Stata 12 (StataCorp, Texas, USA). Descriptive statistics including frequencies were generated and stratified by age group, gender, and congenital heart lesions as appropriate. We have presented the results as count and percentage for qualitative variables. Differences in pediatric echocardiography and diagnosis of CHD across years of study were investigated via Fisher-Halton test and linearity in the trend across years assessed with the Cochran-Armitage trend test; children were grouped by clusters of two consecutive years of observations. A P value <0.05 was used to characterize statistically significant results.
Results
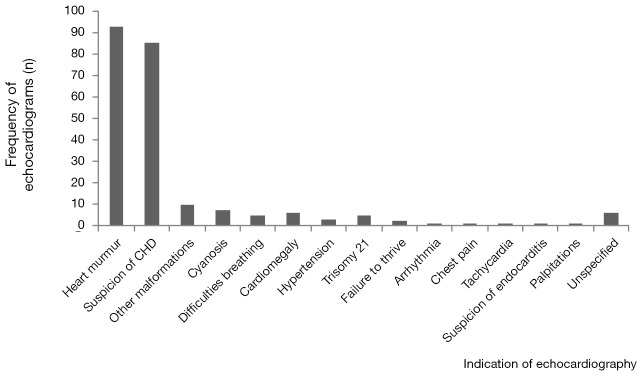
Between January 2004 and December 2013, a total of 9,390 echocardiograms were performed in the echocardiography laboratory including 834 (8.9%) pediatric echocardiograms (aged from 1 day to 15 years). Of the 834 pediatric echocardiograms, 227 (27.2%) children were diagnosed with a definite structural CHD with 123 (54.2%) being boys. The most common affected age group was children less than 1 year old (Figure 1). The proportion of pediatric echocardiography decreased from 13.3% in 2004–2005 to 6.1% in 2012–2013 (P=0.001) but not in a linear fashion (P=0.072 for linear trend) (Table 1). The diagnosis of structural CHD increased from 25.1% in 2004–2005 to 27.1% in 2012–2013 (P=0.523). The trend was not linear (P=0.230).
Figure 1.
Distribution of children with congenital heart defects by age and sex.
Table 1. Proportion of congenital heart defects in relation to the overall number of echocardiograms in children by time period.
| Year | Overall number of echocardiography (n)a | Pediatric echocardiography (n)b | Pediatric echocardiography (%) | CHD (n)c | CHD (%) |
|---|---|---|---|---|---|
| 2004–2005 | 1,614 | 215 | 13.3 | 54 | 25.1 |
| 2006–2007 | 1,914 | 189 | 9.9 | 61 | 32.3 |
| 2008–2009 | 2,009 | 203 | 10.1 | 55 | 27.1 |
| 2010–2011 | 2,090 | 120 | 5.7 | 28 | 23.3 |
| 2012–2013 | 1,763 | 107 | 6.1 | 29 | 27.1 |
a, p-trend =0.424; b, p-trend =0.072; c, p-trend =0.230 (Cochran-Armitage test). CHD, congenital heart disease.
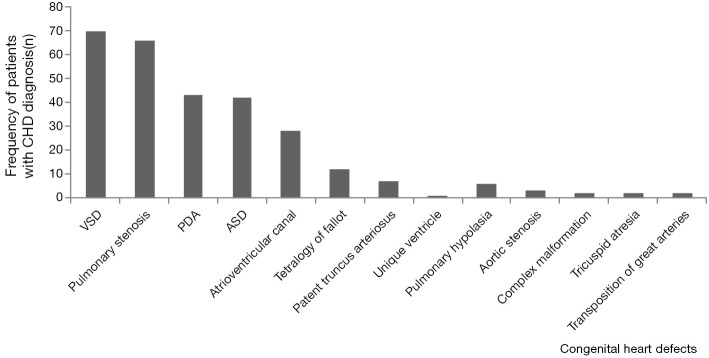
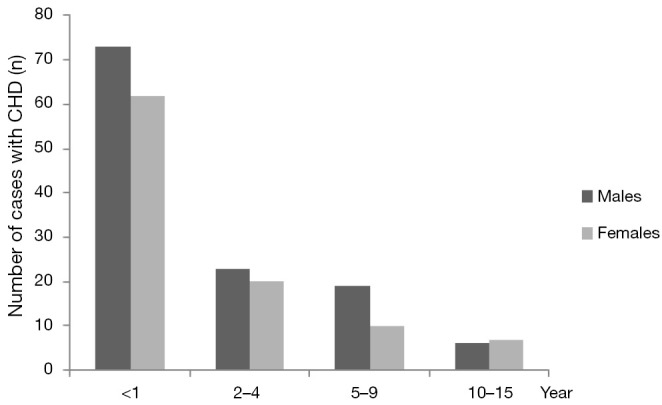
The most commonly reported indication for pediatric echocardiography (Figure 2) in children with CHD was the presence of a heart murmur on physical examination in 93 children (40%) followed by the suspicion of CHD in 85 children (37.4%) and the presence of other malformations in 10 children (4.4%).Ventricular septal defect (VSD) was the most common congenital heart lesion found in 70 (30.8%) children followed by pulmonary stenosis and patent ductus arteriosus (PDA) in 66 (29.1%) and 43 (18.9%) children respectively. The most common cyanotic lesion was tetralogy of Fallot seen in 12 (5.3%) children (Figure 3).
Figure 2.
Frequency of various indications of echocardiography in children identified with congenital heart disease.
Figure 3.
Frequency of different congenital heart defects in the study population. ASD, atrial septal defect; VDS, ventricular septal defect; PDA, patent ductus arteriosus.
Discussion
This study aimed at determining whether the pattern of referral for pediatric echocardiography and the subsequent yield for structural CHD have changed in a major cardiac referral hospital in the capital city of Cameroon between 2004 and 2013. We found that 27.2% of children between 1 day of age and 15 years referred for pediatric echocardiography had a structural CHD, the rate of pediatric echocardiography decreased between 2004 and 2013 by more than half but the proportion of diagnosed structural CHD did not change significantly between 2004 and 2013.The most common heart lesion was VSD, while tetralogy of Fallot was the most common cyanotic lesion.
The relative frequencies of the different types of CHD in our study are consistent with previous reports from Cameroon and other parts of SSA with VSD being the most common acyanotic lesion and tetralogy of Fallot the most cyanotic lesion (5,11,12). More than fifty percent of the children with confirmed diagnosis of CHD were less than 1 year old which is comparable to a recent report in India (13). The finding of heart murmur on clinical examination was the main reason for referral for pediatric echocardiography as demonstrated by a previous report in the country (5). This suggests that auscultation of children for abnormal heart sounds should be encouraged.
Echocardiography is a major imaging modality in cardiovascular diagnosis. It has become the most important and routinely applied noninvasive imaging modality for the diagnosis and follow up of patients with CHD (9). The diagnostic accuracy for describing cardiac morphology is very high, with a reported incidence of less than 100 errors in more than 50,000 echocardiograms (14). It is the sole imaging modality for the evaluation of children with suspected CHD in our setting and in many other SSA countries. In our report, the trend in pediatric echocardiography decreased in the study setting from 2004 and 2013 but the diagnosis of structural CHD did not change reflecting changes in referral pattern in children with suspected heart disease. In this SSA setting (Cameroon), the past decade has witnessed an increase in the number of centers and cardiologist with expertise in pediatric echocardiography, and the increasing north and south collaboration for the diagnosis and management of cardiac diseases including CHD in other centers locally (10) and abroad. This probably accounts for the change in the referral pattern for pediatric echocardiography observed in this referral center, without a change in diagnosed CHD, although we do not have data on other centers regarding their echo volume. This north and south collaboration has enabled the development of the capacity of local personnel.
In a recent review of pediatric echocardiograms in children less than 16 years, the authors reported that the diagnostic inaccuracy was highest when the echocardiogram was performed in non-tertiary centers and when the echocardiogram performer was a non-pediatric cardiologist (13). In our report, all the pediatric echocardiograms were performed in a tertiary centre by cardiologists with expertise in pediatric cardiology and pediatric echocardiography and have been collaborating for more than a decade. This may have reduced the rate of inaccurate diagnosis and interobserver variability. In some reports, diagnostic inaccuracies have been reported in up to 40% of echocardiograms performed by non-pediatric cardiologists (15-17). The fact the trend in pediatric echocardiography changed but the yield for CHD did not change during the study period strengthens the important role of echocardiography in the diagnosis of CHD in resource limited settings like ours especially when performed at tertiary centers with qualified personnel. This suggests echocardiography should be made widely available with adequately trained personnel in resource limited settings like ours.
Limitations
One of the limitations of our study is that we retrospectively studied an established clinical database. There may have been some inaccuracies in data entry. The studies were not evaluated by outside echocardiographers to assess accuracy. Also we were not able to assess the outcome of children diagnosed with CHD. However, all the pediatric echocardiograms were performed by two cardiologists who had expertise in pediatric cardiology and pediatric echocardiography and had been working together for more than 10 years. This might have reduced inaccurate diagnosis and interobserver discrepancies.
Conclusions
This is one of the largest series of pediatric echocardiography in a cardiac referral hospital in Cameroon and suggests that the pattern of referral for pediatric echocardiography has changed but the subsequent diagnosis of structural CHD has not changed. This is likely explained by the evolving health system in the country, with north-south collaborative partnership around improvement of CHD diagnosis and treatment in SSA while progressively building the capacity of local teams. Echocardiography is still a good, accurate diagnostic method for CHD in resource limited settings. Thus more skilled personnel and pediatric echocardiography should be made available to help diagnose CHD early with limited diagnostic error to limit the devastating consequences of late diagnosis.
Acknowledgements
None.
Ethical Statement: The study was approved by the institutional review board of Yaoundé General Hospital (Number: 08642014). The hospital granted authorization to access the echocardiography registers. No informed consent was required as it was a retrospective descriptive study. Information obtained from the registers was anonymized.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births. Incidence and natural history. Circulation 1971;43:323-32. 10.1161/01.CIR.43.3.323 [DOI] [PubMed] [Google Scholar]
- 2.Boneva RS, Botto LD, Moore CA, et al. Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979-1997. Circulation 2001;103:2376-81. 10.1161/01.CIR.103.19.2376 [DOI] [PubMed] [Google Scholar]
- 3.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. 10.1016/S0735-1097(02)01886-7 [DOI] [PubMed] [Google Scholar]
- 4.Tantchou Tchoumi JC, Ambassa JC, Chelo D, et al. Pattern and clinical aspects of congenital heart diseases and their management in Cameroon. Bull Soc Pathol Exot 2011;104:25-8. 10.1007/s13149-010-0091-7 [DOI] [PubMed] [Google Scholar]
- 5.Tantchou Tchoumi JC, Butera G, Giamberti A, et al. Occurrence and pattern of congenital heart diseases in a rural area of sub-Saharan Africa. Cardiovasc J Afr 2011;22:63-6. 10.5830/CVJA-2010-046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zühlke L, Mirabel M, Marijon E. Congenital heart disease and rheumatic heart disease in Africa: recent advances and current priorities. Heart 2013;99:1554-61. 10.1136/heartjnl-2013-303896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mocumbi AO, Lameira E, Yaksh A, et al. Challenges on the management of congenital heart disease in developing countries. Int J Cardiol 2011;148:285-8. 10.1016/j.ijcard.2009.11.006 [DOI] [PubMed] [Google Scholar]
- 8.Mocumbi AO. The challenges of cardiac surgery for African children. Cardiovasc J Afr 2012;23:165-7. 10.5830/CVJA-2012-013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mertens L, Friedberg MK. The gold standard for noninvasive imaging in congenital heart disease: echocardiography. Curr Opin Cardiol 2009;24:119-24. [DOI] [PubMed] [Google Scholar]
- 10.Budzee SA, Tchoumi JT, Giamberti A, et al. African experiences of humanitarian cardiovascular medicine: the Cardiac Centre of St. Elizabeth Catholic General Hospital, Shisong. Cardiovasc Diagn Ther 2012;2:165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okoromah CA, Ekure EN, Ojo OO, et al. Structural heart disease in children in Lagos: profile, problems and prospects. Niger Postgrad Med J 2008;15:82-8. [PubMed] [Google Scholar]
- 12.van der Horst RL. The pattern and frequency of congenital heart disease among blacks. S Afr Med J 1985;68:375-8. [PubMed] [Google Scholar]
- 13.Saraf RP, Suresh P, Maheshwari S, et al. Pediatric echocardiograms performed at primary centers: Diagnostic errors and missing links! Ann Pediatr Cardiol 2015;8:20-4. 10.4103/0974-2069.149514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benavidez OJ, Gauvreau K, Jenkins KJ, et al. Diagnostic errors in pediatric echocardiography: development of taxonomy and identification of risk factors. Circulation 2008;117:2995-3001. 10.1161/CIRCULATIONAHA.107.758532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurwitz RA, Caldwell RL. Should pediatric echocardiography be performed in adult laboratories? Pediatrics 1998;102:e15. 10.1542/peds.102.2.e15 [DOI] [PubMed] [Google Scholar]
- 16.Ward CJ, Purdie J. Diagnostic accuracy of paediatric echocardiograms interpreted by individuals other than paediatric cardiologists. J Paediatr Child Health 2001;37:331-6. 10.1046/j.1440-1754.2001.00695.x [DOI] [PubMed] [Google Scholar]
- 17.Stanger P, Silverman NH, Foster E. Diagnostic accuracy of pediatric echocardiograms performed in adult laboratories. Am J Cardiol 1999;83:908-14. 10.1016/S0002-9149(98)01063-7 [DOI] [PubMed] [Google Scholar]