Abstract
Objective
To examine whether childhood adversity is associated with depressive symptoms, suicide attempts, or psychiatric hospitalization.
Design
History of seven childhood adversities (physical neglect, verbal abuse, physical abuse, sexual abuse, parental death, parental incarceration, and child welfare system placement) was gathered through in-person interviews. Multivariate models examined associations between history of childhood adversities and moderate to severe depressive symptoms, lifetime history of suicide attempt, or lifetime history of psychiatric hospitalization.
Setting
General community.
Participants
The study enrolled 350 homeless adults, aged 50 and older, in Oakland, CA using population-based sampling methods.
Measurements
Moderate to severe depressive symptoms measured on a Center for Epidemiologic Studies–Depression Scale (CES-D ≥22), self-reported lifetime history of suicide attempt, and self-reported lifetime history of psychiatric hospitalization.
Results
Participants with exposure to one childhood adversity had elevated odds of reporting moderate to severe depressive symptoms (adjusted odds ratio [AOR] 2.0; 95% confidence interval [CI] 1.1–3.7) and lifetime history of suicide attempt (AOR 4.6; 95% CI 1.0–21.6) when compared to those who had none; the odds of these two outcomes increased with exposure to additional childhood adversities. Participants with four or more childhood adversities had higher odds of having a lifetime history of psychiatric hospitalization (AOR 7.1; 95% CI 2.8–18.0); there was no increase with fewer adversities.
Conclusion
Childhood adversities are associated with poor mental health outcomes among older homeless adults. Clinicians should collect information about childhood adversities among this high-risk population to inform risk assessment and treatment recommendations.
Keywords: Geriatrics, homeless persons, depression, suicide, mental health services, epidemiology
INTRODUCTION
Homelessness affects 2.5–3.5 million people in the United States annually.1 The homeless population is aging; the median age of homeless adults is over 50, compared to 37 in the early 1990s.2 Due to poor health, homeless adults are considered older at age 50.3,4 Studies on older homeless populations show high rates of psychiatric morbidity, including depressive symptoms, psychiatric hospitalization, and alcohol use disorders.5 Despite the high prevalence of mental health problems, there is limited research on predictors of psychiatric morbidity among older homeless adults.
A growing body of research links childhood adversity (e.g., child maltreatment, caregiver loss, or out-of-home experiences) with poor mental and physical health outcomes in adulthood.6,7 The Adverse Childhood Experiences (ACE) study, an investigation of adults receiving primary care in a health maintenance organization, found a dose-response relationship between cumulative adverse childhood experiences and poor mental health outcomes, including depression, substance use, and attempted suicide.6,8–11 Studies in the general population have found associations between childhood adversities and poor mental health outcomes in old age.12,13 Long-term longitudinal studies have found that childhood adversity is associated with adult psychopathology.14,15
Childhood adversity is associated with an increased risk of adult homelessness potentially caused by disruptions in social bond formation, decreased familial ties, and limitations in educational options and job attainment.16,17 Although childhood adversity has been associated with worse psychiatric outcomes among a sample of homeless women under age 5018 and among homeless adults with mental illness,19 little is known about the prevalence of and association between childhood adversity and psychiatric morbidity among older homeless adults. Understanding the relationships between childhood adversity and psychiatric morbidities in this population could guide risk stratification and allow for clinical and training guidelines.
In a sample of older homeless adults, we assessed the association between childhood adversities and current and lifetime psychiatric problems. We hypothesized that childhood adversity would be associated with moderate to severe depressive symptoms, lifetime history of suicide attempt, and lifetime history of psychiatric hospitalization. We hypothesized that alcohol or drug use mediates the association between childhood adversity and moderate to severe depressive symptoms.
METHODS
Participants and Procedures
The Health Outcomes of People Experiencing Homelessness in Older Middle Age (HOPE HOME) study recruited homeless adults (age ≥50) in Oakland, CA from all shelters serving adults over age 25 (n=5), all free and low-cost meal programs serving at least three meals per week (n=5), a recycling center (n=1), and randomly selected encampments and outdoor sites where homeless individuals stayed, using population-based sampling methods adapted from our prior work.20 Based on the estimates of the number of unique individuals who used the site annually, we approached potential study participants in a random order and assessed for interest and preliminary eligibility. We invited those who were interested and preliminarily eligible for an enrollment interview at a community-based field site. At the enrollment visit, we conducted an in-depth review of eligibility and offered enrollment to eligible individuals.
We conducted baseline interviews from July 2013 through June 2014. To be included, participants had to be age 50 or older, English-speaking, and homeless as defined by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act.21 We excluded participants if they could not give informed consent, as determined by a teach-back method.22 Trained interviewers conducted in-depth, structured baseline interviews with eligible study participants. Participants received a $5 gift card after completing the enrollment procedures and received a $20 gift card after completing the enrollment interview. The University of California, San Francisco (UCSF) Committee on Human Research approved all study procedures.
Sociodemographic Characteristics
Sociodemographic characteristics included self-reported age, sex, race/ethnicity (African American, white, Hispanic/Latino, Asian American, or mixed/other and dichotomized as African American versus non-African American), education level (dichotomized as high school graduate or above versus having passed the General Education Development (GED®) test or less), and relationship status (never married nor partnered in a “marriage-like relationship,” separated/divorced, widowed, or married/partnered). We gauged history of military service by asking participants if they had ever been on active duty military service in the armed forces or served in the U.S. military reserves or National Guard.23 We asked participants to report the age they experienced their first episode of adult homelessness. We asked about lifetime homelessness and tallied the cumulative duration of adult homelessness since age 18. We asked participants if they ever used alcohol regularly (used enough to have felt the effects three or more times per week). We asked participants if they ever used illicit drugs regularly (used cannabis, cocaine, amphetamine-type stimulants, inhalants, sedatives, hallucinogens, or non-prescribed opioids, three or more times per week).23
Health and Functional Status
Using questions from the National Health and Nutrition Examination Survey (NHANES), we asked participants to report if a health care provider had ever told them that they had hypertension, coronary artery disease or myocardial infarction, congestive heart failure, diabetes, stroke, chronic obstructive pulmonary disease or asthma, cancer, or HIV/AIDS.24 We categorized responses as zero, one, two, or three or more of these chronic medical conditions. We used the Katz Index of Independence in Activities of Daily Living (ADLs) to assess ADL difficulties, defined as difficulty completing individual ADLs (bathing, dressing, eating, transferring, or toileting) due to a physical, mental, emotional, or memory problem.25 We categorized the number of ADL difficulties as zero, one, or two or more. We used the Brief Instrumental Functioning Scale (BIFS) to assess difficulties in performing individual instrumental activities of daily living (IADLs) (taking transportation, managing medications, managing money, applying for benefits, setting up job interviews, or finding a lawyer)26 and categorized the number of difficulties as zero, one, or two or more. We determined cognitive status using the Modified Mini-Mental State Examination.27 We defined cognitive impairment as a score below the 7th percentile (i.e. 1.5 standard deviations below the mean of a reference cohort).27,28
Childhood Adversities
We asked participants whether or not they had the following experiences before age 18: 1) physical neglect (“From the time you were a baby until you were 18 years old, did anyone you lived with ever leave you without adequate food or shelter?”), 2) verbal abuse (“Did anyone ever call you names, threaten you, swear at you, or make you feel stupid or worthless?”), 3) physical abuse (“Did you ever experience physical violence by another person using an object like a gun or a knife, or did anyone ever slap, hit, punch, kick, choke, or burn you?”), 4) sexual abuse (“Has anyone ever pressured or forced you to have sexual contact, defined as touching your private parts in a sexual way, making you do something sexual, or making you have sex?”), 5) death of either parent, 6) incarceration of either parent for one month or more, and 7) placement in the child welfare system. The questions regarding physical neglect, parental death, parental incarceration, and child welfare system placement were adapted from the National Survey of Homeless Assistance Providers and Clients (NSHAPC).23 The questions regarding verbal, physical, and sexual abuse were adapted from a prior study of childhood abuse among homeless women.29 The questions pertaining to physical neglect, verbal abuse, physical abuse, sexual abuse, and parental incarceration were similar to ACE study items about childhood adversity (Supplementary Table 1).6 We adapted a method used in the ACE study6 to create a cumulative “childhood adversity” variable that is the summation score of each of these seven categories weighted equally (range 0–7). Because of the low prevalence of scores of five or greater, we grouped study participants with four or more childhood adversities together.
Dependent Variables: Adult Psychiatric Morbidity
Our primary dependent variables were moderate to severe depressive symptoms, lifetime history of suicide attempt, and lifetime history of psychiatric hospitalization. We used the Center for Epidemiologic Studies Depression Scale (CES-D) to assess for depressive symptomatology in the prior week,30 shown to be a reliable measure in homeless populations.31 We used a CES-D score of ≥22 to define moderate to severe depressive symptoms32 to ensure specificity for depressive disorders. We asked participants to self-report lifetime histories of suicide attempt and psychiatric hospitalization, both dichotomized as ever versus never.
Statistical Analyses
We used Pearson chi-square and Wilcoxon non-parametric tests to examine demographic differences between study participants with and without any history of childhood adversity. We used logistic regression to measure the association between childhood adversity and psychiatric morbidity, controlling for variables shown to influence both risk of childhood trauma and depression (age, sex, race/ethnicity, and education level).33,34 We included each of these variables in the initial multivariate models, which we reduced using backward elimination until only variables with p-values of 0.05 or lower remained.
After multivariate analysis, we evaluated whether the association between childhood adversity and moderate to severe depression symptoms was mediated by the regular use of alcohol or illicit drug use during young or middle adulthood (age 18–49). For each substance, we compared the bivariate logistic model with the cumulative childhood adversity score as the only independent variable with a model also including use of that substance as an independent variable. We used SAS version 9.4 (SAS Institute, Inc.) to perform all analyses.
RESULTS
Sampling
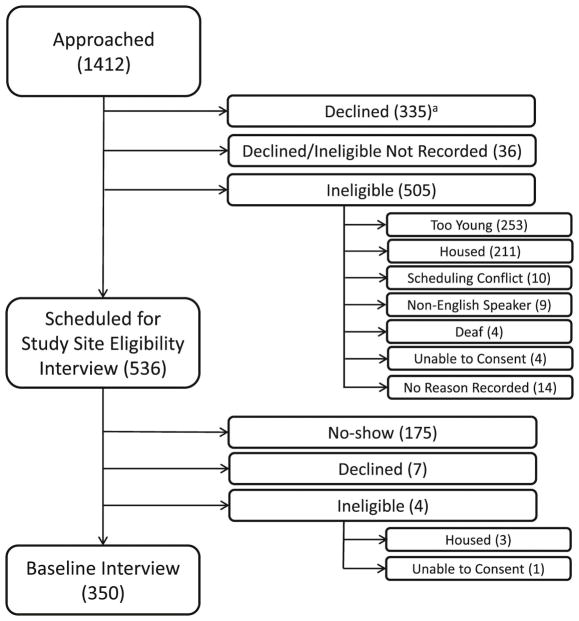
We scheduled 536 people who met basic eligibility criteria for interviews; of the 361 who attended the screening interview, we interviewed 350 who met full criteria and agreed to enrollment (Figure 1).
Figure 1.
Flow-chart of Recruitment of 350 Older Homeless Adultsa
aThis figure shows the number of individuals approached, assessed for eligibility, and enrolled in the study, noting specific reasons for inability to enroll. Values represent the number of individuals in each group.
bParticipants who declined after being approached (335) were not assessed for eligibility. Therefore, the number of participants who were ineligible for the study may have been higher than the numbers presented in this figure.
Sociodemographic Characteristics
The mean age was 58.1 (SD 5.2) years. Over three-quarters (77.1%) were men, and 79.7% were African American. Overall, 68.6% had graduated from high school, 41.4% never married nor partnered and 21.7% served in the military. Almost half (43.4%) experienced their first episode of adult homelessness at age 50 or later. The median total duration of adult homelessness since age 18 was 2.5 years (interquartile range of 0.7–8.0 years). Over half reported a lifetime history of regular alcohol use (61.9%), cannabis use (62.4%), or cocaine use (51.7%) (Table 1).
Table 1.
Characteristics of Participants by History of Childhood Adversity
| Variable | Total (n=350), n (%) | No History of Childhood Adversity (n=99), n (%) | History of Childhood Adversity (n=251), n (%) | P-valuea |
|---|---|---|---|---|
| Age, y | ||||
| 50–54 | 102 (29.1) | 23 (23.2) | 79 (31.5) | 0.32b |
| 55–59 | 117 (33.4) | 38 (38.4) | 79 (31.5) | |
| 60–64 | 89 (25.4) | 28 (28.3) | 61 (24.3) | |
| 65+ | 42 (12.0) | 10 (10.1) | 32 (12.7) | |
| Sex | ||||
| Male | 270 (77.1) | 77 (77.8) | 193 (76.9) | 0.86 |
| Race/ethnicity | ||||
| African American | 279 (79.7) | 83 (83.8) | 196 (78.1) | 0.29b |
| White | 38 (10.9) | 7 (7.1) | 31 (12.4) | |
| Hispanic/Latino | 16 (4.6) | 6 (6.1) | 10 (4.0) | |
| Asian American | 3 (0.9) | 0 (0) | 3 (1.2) | |
| Mixed/other | 14 (4.0) | 3 (3.0) | 11 (4.4) | |
| Education Level | ||||
| High school graduatec or above | 240 (68.6) | 67 (67.7) | 173 (68.9) | 0.82 |
| Marital Status | ||||
| Never married/partnered | 145 (41.4) | 40 (40.4) | 105 (41.8) | 0.87b |
| Separated/divorced | 150 (42.9) | 41 (41.4) | 109 (43.4) | |
| Widowed | 38 (10.9) | 12 (12.1) | 26 (10.4) | |
| Married/partnered | 17 (4.9) | 6 (6.1) | 11 (4.4) | |
| Military Service | ||||
| Active duty/reserves/National Guard | 76 (21.7) | 17 (17.2) | 59 (23.5) | 0.20 |
| Age of First Adult Homeless Episode, y | ||||
| 18–25 | 52 (14.9) | 11 (11.1) | 41 (16.3) | 0.60 |
| 26–49 | 146 (41.7) | 41 (41.4) | 105 (41.8) | |
| 50–59 | 115 (32.9) | 36 (36.4) | 79 (31.5) | |
| 60+ | 37 (10.6) | 11 (11.1) | 26 (10.4) | |
| Median Total Years of Adult Homelessness (IQR) | 2.5 (0.7–8.0) | 2.8 (0.9–8.3) | 2.4 (0.7–8.0) | 0.74d |
| Regular Substance Use, Lifetime Historye | ||||
| Alcohol | 206 (61.9) | 44 (46.8) | 162 (67.8) | <0.001 |
| Cannabis | 216 (62.4) | 54 (55.7) | 162 (65.1) | 0.11 |
| Cocaine | 178 (51.7) | 45 (47.4) | 133 (53.4) | 0.32 |
| Amphetamine-type stimulant | 50 (14.3) | 7 (7.1) | 43 (17.2) | 0.01 |
| Inhalant | 9 (2.6) | 0 | 9 (3.6) | 0.06f |
| Sedative | 15 (4.3) | 0 | 15 (6.0) | 0.01f |
| Hallucinogen | 29 (8.3) | 4 (4.0) | 25 (10.0) | 0.07 |
| Non-prescribed opioid | 52 (14.9) | 13 (13.3) | 39 (15.5) | 0.59 |
| Chronic Medical Conditions | ||||
| Hypertension | 195 (56.0) | 51 (52.6) | 144 (57.4) | 0.42 |
| Coronary artery disease or myocardial infarction | 32 (9.1) | 9 (9.1) | 23 (9.2) | 0.98 |
| Congestive heart failure | 25 (7.1) | 10 (10.1) | 15 (6.0) | 0.18 |
| Diabetes | 49 (14.0) | 18 (18.2) | 31 (12.4) | 0.16 |
| Stroke | 39 (11.2) | 8 (8.1) | 31 (12.4) | 0.25 |
| Chronic obstructive pulmonary disease or asthma | 92 (26.3) | 21 (21.2) | 71 (28.3) | 0.18 |
| Cancerg | 21 (6.0) | 9 (9.1) | 12 (4.8) | 0.13 |
| HIV/AIDS | 19 (5.5) | 4 (4.1) | 15 (6.1) | 0.46 |
| No chronic medical conditionh | 89 (25.4) | 32 (32.3) | 57 (22.7) | 0.07 |
| 1 chronic medical conditionh | 117 (33.4) | 29 (29.3) | 88 (35.1) | |
| 2 chronic medical conditionsh | 101 (28.9) | 22 (22.2) | 79 (31.5) | |
| 3+ chronic medical conditionsh | 43 (12.3) | 16 (16.2) | 27 (10.8) | |
| Functional Status | ||||
| No ADL difficultiesi | 214 (61.1) | 71 (71.7) | 143 (57.0) | 0.04 |
| 1 ADL difficultyi | 44 (12.6) | 8 (8.1) | 36 (14.3) | |
| 2+ ADL difficultiesi | 92 (26.3) | 20 (20.2) | 72 (28.7) | |
| No IADL difficultiesj | 177 (50.6) | 57 (57.6) | 120 (47.8) | 0.24 |
| 1 IADL difficultyj | 83 (23.7) | 19 (19.2) | 64 (25.5) | |
| 2+ IADL difficultiesj | 90 (25.7) | 23 (23.2) | 67 (26.7) | |
| Cognitive Impairmentk | 90 (25.8) | 30 (30.3) | 60 (24.0) | 0.23 |
Abbreviations: IQR, interquartile range; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome; ADL, activities of daily living; IADL, instrumental activities of daily living
Pearson chi-square with 1 degree of freedom, except as noted
Pearson chi-square with 3 degrees of freedom
High school graduates excluded participants who passed the General Education Development (GED®) test.
Wilcoxon non-parametric test
Regular alcohol use was defined as using three or more times per week during which the participant reported feeling the effects of the alcohol. Regular illicit drug use was defined as using the substance three or more times per week.
Fisher exact test
Cancer excluded non-melanoma skin cancer.
Chronic medical condition was defined as hypertension, coronary artery disease or myocardial infarction, congestive heart failure, diabetes, stroke, chronic obstructive pulmonary disease or asthma, cancer (excluding non-melanoma skin cancer), or HIV/AIDS.
ADL difficulty was defined as difficulty completing bathing, dressing, eating, transferring, or toileting.
IADL difficulty was defined as difficulty taking transportation, managing medications, managing money, applying for benefits, setting up job interviews, or finding a lawyer.
Cognitive impairment was defined as a score of <7th percentile (i.e. 1.5 standard deviation below the mean of a reference cohort) on the Modified Mini-Mental Status Exam.
Health and Functional Status
One-third (33.4%) of participants reported having one chronic medical condition, 28.9% reported two, and 12.3% reported three or more. Over one-third (38.9%) of participants had difficulty performing at least one ADL. Almost half (49.4%) of participants had difficulty performing at least one IADL. A quarter (25.8%) met criteria for cognitive impairment. (Table 1).
Childhood Adversities
The most commonly reported childhood adversities were verbal abuse (49.3%), physical abuse (33.3%), and parental death (21.4%); the least common was parental incarceration (5.5%). Overall, 71.7% of participants reported at least one childhood adversity, and 8.3% reported four or more. Of those who stated only one childhood adversity (32.6%, n=114), the most frequently reported categories were verbal abuse (49.1%), parental death (25.4%), and physical abuse (17.5%). Of those who reported four or more items of childhood adversity (8.3%, n=29), the most common categories were verbal abuse (100%), physical abuse (93.1%), and sexual abuse (75.9%) (Table 2).
Table 2.
Prevalence of Self-reported Childhood Adversities (Before Age 18)
| Variable | Total (n=350), n (%) |
|---|---|
| Physical neglecta | 38 (11.0) |
| Verbal abuseb | 172 (49.3) |
| Physical abusec | 116 (33.3) |
| Sexual abused | 46 (13.2) |
| Parental incarceratione | 19 (5.5) |
| Parental deathf | 75 (21.4) |
| Child welfare system placement | 29 (8.3) |
| Cumulative Number of Childhood Adversitiesg | |
| 0 | 99 (28.3) |
| 1 | 114 (32.6) |
| 2 | 71 (20.3) |
| 3 | 37 (10.6) |
| 4+ | 29 (8.3) |
Physical neglect was defined as being left without adequate food or shelter.
Verbal abuse was defined as being called names, threatened, sworn at, or made to feel stupid or worthless.
Physical abuse was defined as experiencing physical violence perpetrated by another person using an object or being slapped, hit, punched, kicked, choked, or burned.
Sexual abuse was defined as being pressured or forced to have sexual contact, to do something sexual, or to have sex.
Parental incarceration was defined as having either parent incarcerated in jail or prison for a month or more before the participant reached age 18.
Parental death was defined as experiencing the death of either parent before the participant reached age 18.
Childhood adversities included any report of the following seven categories: physical neglect, verbal abuse, physical abuse, sexual abuse, parental incarceration, parental death, or child welfare system placement; each item was weighted equally.
Adult Psychiatric Morbidity
Over a third of participants (38.3%) scored 22 or higher on the CES-D, indicating moderate to severe depressive symptoms. In a multivariate model for moderate to severe depressive symptoms, only age and adverse childhood experiences remained in the model. The adjusted odds ratio (AOR) of adverse experiences exhibited a dose-response relationship, with increasing odds of moderate to severe depressive symptoms with each increase in the level of adversity. Those with exposure to one childhood adversity had a two-fold increase in odds of reporting moderate to severe depressive symptoms (AOR 2.0; 95% CI 1.1–3.7), while those with exposure to four or more childhood adversities had a six-fold increase (AOR 6.0; 95% CI 2.4–15.4), compared to those with no adverse events (Table 3). In our evaluation of mediation of current depressive symptoms by substance use, the OR for cocaine use among those with a trauma score of 4+ versus 0, increased from 7.7 to 9.0 (17%). The remaining ORs changed from +7.6% to −11.0%.
Table 3.
Factors Associated with Psychiatric Morbidity in Older Homeless Adults
| Moderate to Severe Depressive Symptoms (CES-D Score ≥22) (n=133) | History of Suicide Attempt (Lifetime) (n=45) | History of Psychiatric Hospitalization (Lifetime) (n=66) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalence of depressive symptoms, n (%) | Bivariate OR (95% CI) | Multivariate AOR (95% CI) | Prevalence of suicide attempt, n (%) | Bivariate OR (95% CI) | Multivariate AOR (95% CI) | Prevalence of psychiatric hospitalization, n (%) | Bivariate OR (95% CI) | Multivariate AOR (95% CI) | |
| Cumulative Number of Childhood Adversities†a | |||||||||
| 0 | 22 (22.5) | REF | REF | 2 (2.0) | REF | REF | 13 (13.1) | REF | REF |
| 1 | 40 (35.4) | 1.9 (1.0–3.5)* | 2.0 (1.1–3.7)* | 10 (8.8) | 4.6 (1.0–21.9) | 4.6 (1.0–21.6) | 18 (15.8) | 1.2 (0.6–2.7) | 1.2 (0.6–2.7) |
| 2 | 32 (45.7) | 2.9 (1.5–5.7)* | 2.9 (1.5–5.7)* | 9 (13.0) | 7.2 (1.5–35.0)* | 7.8 (1.6–37.4)* | 11 (15.5) | 1.2 (0.5–2.9) | 1.2 (0.5–2.9) |
| 3 | 19 (51.4) | 3.7 (1.6–8.2)* | 4.2 (1.9–9.7)** | 10 (27.0) | 17.8 (3.6–87.5)** | 20.0 (4.1–98.1)** | 9 (24.3) | 2.1 (0.8–5.6) | 2.1 (0.8–5.5) |
| 4+ | 20 (69.0) | 7.7 (3.0–19.4)** | 6.0 (2.4–15.4)** | 14 (48.3) | 44.8 (9.1–220.7)** | 44.7 (9.1–219.2)** | 15 (51.7) | 7.1 (2.8–18.2)** | 7.1 (2.8–18.0)** |
| Age (+5 y) | - | 0.6 (0.5–0.8)** | 0.9 (0.9–1.0)** | - | - | ||||
| Graduated High Schoolb | |||||||||
| No | 86 (36.1) | REF | 24 (10.0) | REF | REF | 47 (19.6) | REF | ||
| Yes | 47 (43.1) | 1.3 (0.8–2.1) | 21 (19.4) | 2.2 (1.1–4.1)* | 2.4 (1.2–4.8)* | 19 (17.3) | 0.9 (0.5–1.6) | ||
| Sex | |||||||||
| Male | 101 (37.7) | REF | 30 (11.2) | REF | 45 (16.7) | REF | |||
| Female | 32 (40.5) | 1.1 (0.7–1.9) | 15 (19.0) | 1.9 (0.9–3.7) | 21 (26.3) | 1.8 (1.0–3.2) | |||
| Race/ethnicity | |||||||||
| African American | 97 (35.1) | REF | 33 (12.0) | REF | 47 (16.9) | REF | |||
| Non-African American | 36 (50.7) | 1.9 (1.1–3.2)* | 12 (16.9) | 1.5 (0.7–3.1) | 19 (26.8) | 1.8 (1.0–3.4) | |||
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; OR, odds ratio; AOR, adjusted odds ratio
In all models, the overall (Type 3) p-value for childhood adversity score was <0.001.
Wald chi-square p-value <0.05 with 1 degree of freedom, except for childhood adversities, which has 4 degrees of freedom
Wald chi-square p-value <0.001 with 1 degree of freedom, except for childhood adversities, which has 4 degrees of freedom
Childhood adversities include any report of the following seven categories: physical neglect, verbal abuse, physical abuse, sexual abuse, parental incarceration, parental death, or child welfare system placement; each item was weighted equally.
High school graduate does not include participants who passed the General Education Development (GED®) test.
Of the participants, 13.0% reported a lifetime history of suicide attempt. In multivariate analysis, the odds of reporting a suicide attempt exhibited a dose-response relationship. Those with exposure to one childhood adversity had a non-significantly elevated odds of having a suicide attempt (AOR 4.6; 95% CI 1.0–21.6). Those with exposure to four or more childhood adversities had a 45-fold increase (AOR 44.7; 95% CI 9.1–219.2), compared to those with no adversities. (Table 3)
Almost a fifth (18.9%) of participants reported a lifetime history of psychiatric hospitalization. In a multivariate model having exposures to one, two or three types of childhood adversity was not associated with having had a psychiatric hospitalization. However, having exposure to four or more childhood adversities was significantly associated (AOR 7.1; 95% CI 2.8–18.0). (Table 3).
DISCUSSION
In this sample of older homeless adults, we found a high prevalence of childhood adversity when compared to the general population.35 Our findings advance prior research by demonstrating that older homeless adults have a similarly high prevalence of childhood adversity as do younger homeless populations.36 As in the general population, we found a dose-response association between childhood adversities and psychiatric morbidities, despite the high prevalence of both childhood adversities and psychiatric morbidities.
The prevalence of childhood physical abuse was higher in this sample than in the general population (33.3% versus 14.8%),35 but was comparable to a national sample of younger homeless adults.23 We found a high prevalence of parental death occurring during the participants’ childhood when compared to the general population (21.4% versus 0.3%).37 Early parental death may have repercussions on subsequent development, given the psychological and financial impact on the family system.
Childhood adversity is a known risk factor for homelessness,17 but has not been explored in older homeless adults. Despite the fact that over 40% of the participants in our study first experienced homelessness at age 50 or later, the high prevalence of childhood adversity suggests the lingering effects of adverse childhood events, which can cause homelessness through a variety of mechanisms.38,39 Childhood adversity disrupts the formation of social bonds and is associated with decreased familial social support.40 These disruptions create vulnerabilities to homelessness throughout the life course by limiting educational and employment options, increasing risk for criminal justice system involvement and later life victimization, and decreasing the likelihood of forming marital bonds. These may cause homelessness directly by creating barriers to employment and housing or indirectly by decreasing the ability for an individual to withstand income shocks, lack of affordable housing, or health crises through familial support.39
Participants had a high prevalence of psychiatric morbidity consistent with the literature on younger homeless adults.41 The relationship between mental health problems and homelessness is complex and bi-directional.42 Mental illness and psychiatric hospitalizations are presumed to have direct effects on homelessness, via decreased opportunities for educational attainment and employment and decreased formation of social ties.38,39 Homelessness is a risk factor for the development and worsening of mental health problems, due to the stress of homelessness, disruption of social ties, and poor access to mental health care.39
We found an independent, dose-response relationship between exposure to childhood adversity and both moderate to severe depressive symptoms and lifetime history of suicide attempt, consistent with the ACE literature.8,11 Exposure to childhood adversity was associated independently with a lifetime history of psychiatric hospitalization, but only for individuals with four or more adversities. We hypothesized that the association between childhood adversities and depressive symptoms would be mediated by substance use in adulthood, but we did not find evidence of this, which may be a function of the high prevalence of substance use in our study population. These findings suggest that, even at older ages, childhood adversity contributes to psychiatric morbidity in this high-risk population.
The association between exposure to childhood adversity and psychiatric morbidity has implications for clinical practice and training. Although the Substance Abuse and Mental Health Services Administration (SAMHSA) recommends that providers screen for physical and sexual trauma in all patients43 because of the strong evidence of the influence this trauma has on future psychiatric morbidity,44 there is no such recommendation to screen for parental loss. Our findings suggest that mental health and primary care providers should consider screening older homeless adults for all childhood adversities. This may enhance suicide risk assessment by identifying those with multiple adversities, who are at highest risk.
Older homeless adults have a high rate of medical complexity, including high rates of chronic diseases and geriatric conditions.3 The high prevalence of cognitive impairment in this population could be due to dementia, depression, or acute substance use. Their functional status is worse than those 20 years older in the general population.4 This burden of chronic medical conditions, cognitive impairment, and poor functional status in our study population has implications for mental health treatment. For instance, individuals with multiple co-morbid medical and psychiatric issues, as well as poor functional status and cognitive impairment may have a challenging time managing multiple health care visits and may be at risk for the negative health effects of polypharmacy. Individuals with cognitive impairment may not be able to benefit from traditional psychotherapies. Current interventions aimed at housed geriatric populations, such as home visits from psychiatric teams, may be more challenging to implement among homeless older populations.
There is a high prevalence of housing stress among individuals age 50 and older, which may reflect lack of affordable housing in the context of fixed or shrinking incomes.45 As an increasing proportion of adults 50 and older are at risk for homelessness, due to a birth-cohort effect, and a mismatch between fixed incomes and a lack of affordable housing for older Americans, psychiatrists working with low-income, older populations should screen for homelessness. The high prevalence of psychiatric morbidity in this medically complex population presents challenges to the mental health workforce amidst a shortage of geriatric psychiatrists.46
Limitations
Our study has several limitations. We cannot compare the rates of adversity we measured directly with studies that used the ACE score.6 We employed validated measures used in other studies of homeless populations, including the nationally representative study of homeless individuals.23 Second, we used a cross-sectional design, so we are unable to draw causal inferences about the association between childhood adversity and psychiatric morbidity. Third, as in other studies examining childhood adversity,6,35 our estimates of childhood adversity may be underreported. Finally, we did not use measures to diagnose clinical depression, but we did use a validated instrument to detect depressive symptoms that allowed for comparison to other studies.30,31
Conclusion
Childhood adversity is prevalent and has enduring effects on psychiatric morbidity among a sample of older homeless adults. Interventions to reduce or ameliorate childhood adversity may have an impact on homelessness throughout the life course. The high rates of moderate to severe depressive symptoms, lifetime history of psychiatric hospitalization and suicide attempt suggest an ongoing risk for suicide in this population. Screening for childhood adversity may enhance suicide risk assessment among older depressed homeless adults. The range of childhood adversity and the cumulative risk suggest that screens should include a range of adverse experiences to gauge risk. Given the shortage of geriatric mental health providers, screening for childhood adversities should be undertaken by all providers who care for older homeless adults.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge their colleagues Angela Allen, Pamela Olsen, Nina Fiellin, Tauni Marin, and Kenneth Perez for their invaluable contributions to the HOPE HOME study; Bernard Lee for help in manuscript preparation; and the staff at St. Mary’s Center and the HOPE HOME Community Advisory Board for their guidance and partnership.
Funding:
This work was supported by grants from the National Institute on Aging (NIA) at the National Institutes of Health (NIH) [K24AG046372 to MK, LT, and DG and R01AG041860 to MK, CP, and DG]; National Institute of Mental Health (NIMH) at the NIH [R25MH060482 to CML, K23MH093689 to CM]; and the Substance Abuse and Mental Health Services Administration (SAMHSA) [SM060562 to CML]. These funding sources had no role in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions:
Drs. Lee and Kushel had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Lee, Kushel
Acquisition of data: Ponath, Kushel
Statistical analysis: Lee, Guzman, Kushel
Analysis and interpretation of data: Lee, Guzman, Kushel
Drafting of the manuscript: Lee, Mangurian, Tieu, Guzman, Kushel
Critical revision of the manuscript for important intellectual content: Lee, Mangurian, Tieu, Ponath, Guzman, Kushel
Conflicts of Interest:
M.B. Kushel is a member of the leadership board of Everyone Home, which seeks to end homelessness in Alameda County, CA. No other conflicts of interest were reported.
Previous Presentation:
This work was presented at poster presentations during the American Psychiatric Association Annual Meeting (APA) in Toronto, Canada, May 16–20, 2015 and during the APA Institute on Psychiatric Services Meeting in New York, NY, October 8–11, 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014 Oct;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006 Jul;21(7):775–778. doi: 10.1111/j.1525-1497.2006.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown RT, Hemati K, Riley ED, et al. Geriatric Conditions in a Population-Based Sample of Older Homeless Adults. Gerontologist. 2016 Feb; doi: 10.1093/geront/gnw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med. 2012 Jan;27(1):16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stergiopoulos V, Herrmann N. Old and homeless: a review and survey of older adults who use shelters in an urban setting. Can J Psychiatry. 2003 Jul;48(6):374–380. doi: 10.1177/070674370304800603. [DOI] [PubMed] [Google Scholar]
- 6.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 7.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004 Oct;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 9.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav 2002. 2002 Sep-Oct;27(5):713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 10.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003 Mar;111(3):564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 11.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001 Dec;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 12.Raposo SM, Mackenzie CS, Henriksen CA, Afifi TO. Time does not heal all wounds: older adults who experienced childhood adversities have higher odds of mood, anxiety, and personality disorders. Am J Geriatr Psychiatry. 2014 Nov;22(11):1241–1250. doi: 10.1016/j.jagp.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Ege MA, Messias E, Thapa PB, Krain LP. Adverse childhood experiences and geriatric depression: results from the 2010 BRFSS. Am J Geriatr Psychiatry. 2015 Jan;23(1):110–114. doi: 10.1016/j.jagp.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, Koenen KC. Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depress Anxiety. 2010 Dec;27(12):1087–1094. doi: 10.1002/da.20762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010 May;20(5):385–394. doi: 10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Roos LE, Mota N, Afifi TO, Katz LY, Distasio J, Sareen J. Relationship between adverse childhood experiences and homelessness and the impact of axis I and II disorders. Am J Public Health. 2013 Dec;103(Suppl 2):S275–281. doi: 10.2105/AJPH.2013.301323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koegel P, Melamid E, Burnam A. Childhood risk factors for homelessness among homeless adults. Am J Public Health. 1995 Dec;85(12):1642–1649. doi: 10.2105/ajph.85.12.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein JA, Leslie MB, Nyamathi A. Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: mediating roles of self-esteem and abuse in adulthood. Child Abuse Negl. 2002 Oct;26(10):1011–1027. doi: 10.1016/s0145-2134(02)00382-4. [DOI] [PubMed] [Google Scholar]
- 19.Patterson ML, Moniruzzaman A, Somers JM. Setting the stage for chronic health problems: cumulative childhood adversity among homeless adults with mental illness in Vancouver, British Columbia. BMC Public Health. 2014;14:350. doi: 10.1186/1471-2458-14-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiser SD, Hatcher A, Frongillo EA, et al. Food insecurity is associated with greater acute care utilization among HIV-infected homeless and marginally housed individuals in San Francisco. J Gen Intern Med. 2013 Jan;28(1):91–98. doi: 10.1007/s11606-012-2176-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shelton KH, Taylor PJ, Bonner A, van den Bree M. Risk factors for homelessness: evidence from a population-based study. Psychiatr Serv. 2009 Apr;60(4):465–472. doi: 10.1176/ps.2009.60.4.465. [DOI] [PubMed] [Google Scholar]
- 22.Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D. Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. 2006 Aug;21(8):867–873. doi: 10.1111/j.1525-1497.2006.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burt MR United States. Interagency Council on the Homeless., Urban Institute. Homelessness: programs and the people they serve: findings of the National Survey of Homeless Assistance Providers and Clients: summary. Washington, DC: U.S. Dept. of Housing and Urban Development; 1999. [Google Scholar]
- 24.National Health and Nutrition Examination Survey Questionnaire (NHANES) Hyattsville, MD: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 25.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983 Dec;31(12):721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 26.Sullivan G, Dumenci L, Burnam A, Koegel P. Validation of the brief instrumental functioning scale in a homeless population. Psychiatr Serv. 2001 Aug;52(8):1097–1099. doi: 10.1176/appi.ps.52.8.1097. [DOI] [PubMed] [Google Scholar]
- 27.Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Can J Psychiatry. 2001 Aug;46(6):506–510. doi: 10.1177/070674370104600604. [DOI] [PubMed] [Google Scholar]
- 28.Bravo G, Hébert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. 1997 Oct;12(10):1008–1018. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 29.Green HD, Jr, Tucker JS, Wenzel SL, et al. Association of childhood abuse with homeless women’s social networks. Child Abuse Negl. 2012 Jan;36(1):21–31. doi: 10.1016/j.chiabu.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977:385–401. [Google Scholar]
- 31.Ritchey FJ, La Gory M, Fitzpatrick KM, Mullis J. A comparison of homeless, community-wide, and selected distressed samples on the CES-Depression Scale. Am J Public Health. 1990 Nov;80(11):1384–1386. doi: 10.2105/ajph.80.11.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haringsma R, Engels GI, Beekman AT, Spinhoven P. The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. International journal of geriatric psychiatry. 2004 Jun;19(6):558–563. doi: 10.1002/gps.1130. [DOI] [PubMed] [Google Scholar]
- 33.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003 Jun;160(6):1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 34.González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. 2010 Nov;44(15):1043–1051. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1609–1613. [PubMed] [Google Scholar]
- 36.Tam TW, Zlotnick C, Robertson MJ. Longitudinal perspective: adverse childhood events, substance use, and labor force participation among homeless adults. Am J Drug Alcohol Abuse. 2003;29(4):829–846. doi: 10.1081/ada-120026263. [DOI] [PubMed] [Google Scholar]
- 37.Slopen N, Shonkoff JP, Albert MA, et al. Racial Disparities in Child Adversity in the U.S.: Interactions With Family Immigration History and Income. Am J Prev Med. 2015 Sep; doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 38.Craig TK, Hodson S. Homeless youth in London: I. Childhood antecedents and psychiatric disorder. Psychol Med. 1998 Nov;28(6):1379–1388. doi: 10.1017/s0033291798007351. [DOI] [PubMed] [Google Scholar]
- 39.Tsai J, Edens EL, Rosenheck RA. A typology of childhood problems among chronically homeless adults and its association with housing and clinical outcomes. J Health Care Poor Underserved. 2011 Aug;22(3):853–870. doi: 10.1353/hpu.2011.0081. [DOI] [PubMed] [Google Scholar]
- 40.Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl. 2002 Jun;26(6–7):715–729. doi: 10.1016/s0145-2134(02)00343-5. [DOI] [PubMed] [Google Scholar]
- 41.DeMallie DA, North CS, Smith EM. Psychiatric disorders among the homeless: a comparison of older and younger groups. Gerontologist. 1997 Feb;37(1):61–66. doi: 10.1093/geront/37.1.61. [DOI] [PubMed] [Google Scholar]
- 42.Cohen CI, Thompson KS. Homeless mentally ill or mentally ill homeless? Am J Psychiatry. 1992 Jun;149(6):816–823. doi: 10.1176/ajp.149.6.816. [DOI] [PubMed] [Google Scholar]
- 43.Trauma-Informed Care in Behavioral Health Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [PubMed] [Google Scholar]
- 44.Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol. 2001;13(3):733–753. doi: 10.1017/s0954579401003170. [DOI] [PubMed] [Google Scholar]
- 45.Baker K, Baldwin P, Donahue K, et al. Housing America’s Older Adults: Meetings the Needs of an Aging Population. Cambridge, MA: Joint Center for Housing Studies of Harvard University; 2014. [Google Scholar]
- 46.Bartels SJ, Naslund JA. The underside of the silver tsunami--older adults and mental health care. N Engl J Med. 2013 Feb;368(6):493–496. doi: 10.1056/NEJMp1211456. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.