Abstract
Introduction
Immunization information systems (IISs) are highly effective for increasing vaccination rates but information about how primary care physicians use them is limited.
Methods
Pediatricians, family physicians (FPs), and general internists (GIMs) were surveyed by e-mail and mail from January 2015 to April 2015 from all states with an existing IIS. Providers were recruited to be representative of national provider organization memberships. Multivariable log binomial regression examined factors associated with IIS use (October 2015–April 2016).
Results
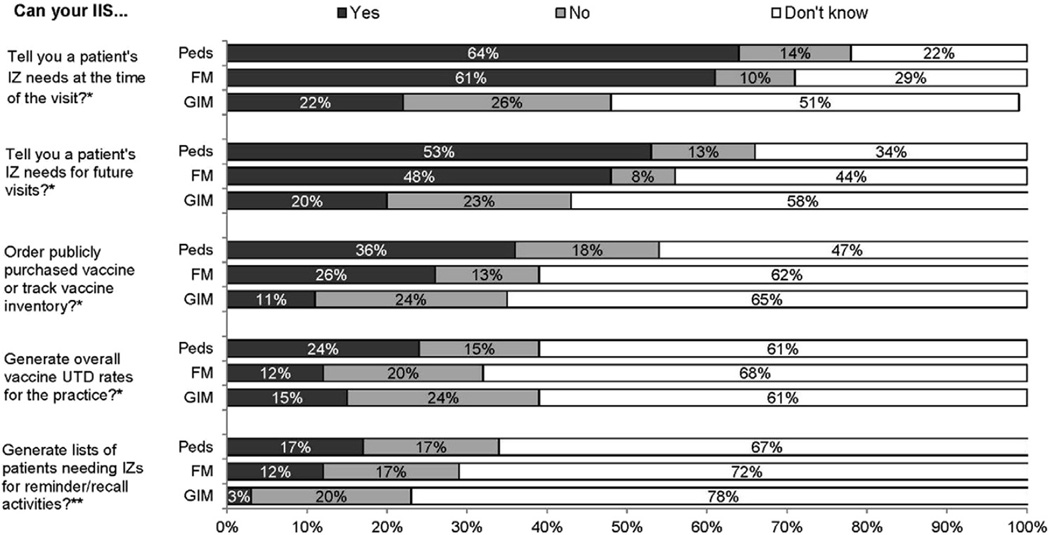
Response rates among pediatricians, FPs, and GIMs, respectively, were 75% (325/435), 68% (310/459), and 63% (272/431). A proportion of pediatricians (5%), FPs (14%), and GIMs (48%) did not know there was a state/local IIS; 81%, 72%, and 27% reported using an IIS (p < 0.0001). Among those who used IISs, 64% of pediatricians, 61% of FPs, and 22% of GIMs thought the IIS could tell them a patient’s immunization needs; 22%, 29%, and 51% did not know. The most frequently reported major barriers to use included the IIS not updating the electronic medical record (29%, 28%, 35%) and lack of ability to submit data electronically (22%, 27%, 31%). Factors associated with lower IIS use included FP (adjusted risk ratio=0.85; 95% CI=0.75, 0.97) or GIM (adjusted risk ratio=0.33; 95% CI=0.25, 0.42) versus pediatric specialty and older versus younger provider age (adjusted risk ratio=0.96; 95 CI%=0.94, 0.98).
Conclusions
There are substantial gaps in knowledge of IIS capabilities, especially among GIMs; barriers to interoperability between IISs and electronic medical records affect all specialties. Closing these gaps may increase use of proven IIS functions including decision support and reminder/recall.
INTRODUCTION
The Centers for Disease Control and Prevention defines immunization information systems (IISs), also known as immunization registries, as confidential, population-based, computerized systems that collect and consolidate vaccination data from vaccination providers for people living in a given geopolitical area.1 The Community Preventive Services Task Force recommends the use of IISs on the basis of strong evidence of effectiveness in increasing vaccination rates and reducing vaccine-preventable diseases.2 IIS functions that support immunization delivery in the primary care setting include2:
determining vaccination status, including vaccine evaluation and forecasting, to determine vaccines due, past due, or due in the future, to guide vaccination decisions at the point of care;
determining vaccination rates, missed vaccination opportunities, and invalid dose administration;
interventions, such as reminders or recalls to patients for upcoming or overdue vaccinations; and
facilitating vaccine management and accountability.
Currently, IISs exist in five cities, the District of Columbia, and in all U.S. states excluding New Hampshire.3 Participation rates for U.S. children in IISs have been increasing, with the latest IIS Annual Report in 2014 showing that 88% of U.S. children aged < 6 years have two or more vaccinations recorded in their state or regional IIS.4 Adult participation has lagged, but is increasing, with 33% of U.S. adults having at least one adult immunizations in their IIS in 2014.4 However, because many states do not mandate reporting of immunizations by providers, the level of completeness of IIS vaccination records and the level of participation by providers varies substantially by state and region.5
The Community Preventive Services Task Force identified the lack of information about the use and utility of IISs in clinical settings2 as a critical gap in evidence in 2015. This study sought to address this gap by surveying pediatricians, family physicians (FPs), and general internists (GIMs) nationally and comparing responses from physicians in the three specialties with respect to their:
knowledge and use of different functionalities of state/local IISs;
knowledge of mandated reporting requirements for children and adults;
reported barriers to use of state/local IISs; and
physician and practice characteristics associated with use of their state/local IIS.
METHODS
Study Design and Population
From January 2015 to April 2015, a survey was administered to three networks of primary care physicians recruited as part of a program to perform rapid turnaround surveys about vaccination issues.6 National networks were developed by recruiting pediatricians, FPs, and GIMs from the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians, respectively. Quota sampling7 was conducted to ensure network physicians were similar to the memberships of the national organizations with respect to region, urban versus rural location, practice setting, and practice type. A previous publication has demonstrated that network physicians and physicians randomly sampled from American Medical Association physician databases had similar demographic characteristics, practice attributes, and attitudes about a range of vaccination issues.7 The human subjects review board approved this study as exempt research.
The survey instrument was developed jointly with Centers for Disease Control and Prevention subject matter experts. The survey defined state/local registry as “an immunization information system (IIS), also known as an immunization registry, which operates at the state, city, or county level. It does not refer to practice-based registries.” Four-point Likert scales were used for questions assessing barriers to use of IISs ranging from major barrier to not a barrier at all. Three national advisory panels of pediatricians, FPs, and GIMs (n=16) discussed each question and 189 providers nationally piloted the entire survey, with modifications after each process.
Physicians were surveyed by Internet (with up to eight e-mail reminders) or mail (with up to two mailed reminders) based on their preference. A web-based program (Verint) was used to administer Internet surveys. Internet survey non-respondents were sent one mail survey in case of e-mail failures. The mail protocol was patterned on Dillman’s tailored design method.8
Statistical Analysis
Analyses were conducted from October 2015 to April 2016. Internet and mail surveys were pooled, as studies have found similar physician attitudes by either method.9 Respondents from New Hampshire were excluded. Respondents were compared to non-respondents using Wilcoxon and chi-square analyses and responses between specialties using chi-square and Mantel –Haenszel chi-square tests; 95% CIs for point estimates were reported when comparisons with previously published results were made. Based on data from the Survey of State Immunization Information System Legislation,10 actual provider reporting mandates by jurisdiction were compared to physician perception of mandates, excluding respondents from states where there was mandated reporting for public sites only or only for vaccines purchased through the Vaccines for Children program (n=152 respondents), which may not have been relevant to respondents’ practices.
Multivariable log binomial regression was conducted with the dependent variable being respondents who reported using their IIS for any purpose. Independent variables included how electronic medical or health records (EMRs/EHRs) were used at the practice, whether financial decisions were made at a larger system level, and characteristics of the practices and their patient populations. Characteristics significant at p≤0.25 in bivariate analyses were tested in multivariable models, using backwards elimination resulting in retention of only those factors that were significant at p < 0.05 in the final model, with the exception of region, which was retained because of the importance of regional differences in IISs. The final model was assessed for goodness of fit, associations between covariates, and influential observations. Risk ratios were calculated because of the tendency of ORs to overestimate effect sizes when outcomes are common.11,12 Calculation of adjusted risk ratios was conducted using R-3.2.3 (function glm2)13,14 and all other analysis using SAS, version 9.4.
RESULTS
Response rates were 75% (325/435) among pediatricians, 68% (310/459) among FPs, and 63% (272/431) among GIMs, yielding an overall response rate of 68% (907/1,325). Table 1 shows characteristics of respondents compared with non-respondents. The only significant difference between respondents and non-respondents was among FPs, where fewer men responded. Eight pediatricians, three FPs, and four GIMs did not administer vaccines and were excluded.
Table 1.
Comparison of Respondents and Non-Respondents by Group (n=1,325)
| Variable | Pediatrics | Family medicine | General internal medicine | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Respondents (n=325) |
Non- respondents (n=110) |
p- value |
Respondents (n=310) |
Non- respondents (n=149) |
p- value |
Respondents (n=272) |
Non- respondents (n=159) |
p-value | |
| Gender, % | 0.95 | 0.005 | 0.29 | ||||||
| Male | 36 | 36 | 52 | 66 | 64 | 69 | |||
| Female | 64 | 64 | 48 | 34 | 36 | 31 | |||
| Setting, % | 0.31 | 0.19 | 0.18 | ||||||
| Private practice | 78 | 75 | 66 | 73 | 72 | 70 | |||
| Hospital or clinic | 19 | 24 | 24 | 17 | 19 | 25 | |||
| HMO | 2 | 1 | 10 | 10 | 9 | 5 | |||
| Location, % | 0.71 | 0.60 | 0.57 | ||||||
| Urban | 13 | 16 | 39 | 34 | 60 | 55 | |||
| Suburban | 77 | 74 | 53 | 56 | 36 | 42 | |||
| Rural | 10 | 10 | 8 | 10 | 3 | 3 | |||
| Region, % | 0.69 | 0.46 | 0.11 | ||||||
| Midwest | 20 | 19 | 30 | 26 | 18 | 27 | |||
| Northeast | 21 | 26 | 13 | 13 | 26 | 24 | |||
| South | 36 | 31 | 34 | 41 | 33 | 31 | |||
| West | 23 | 24 | 23 | 20 | 23 | 18 | |||
| Age, years, M (SD)/median | 50.8 (10.5)/51 | 49.7 (11.2)/49 | 0.32 | 53.2 (7.7)/54 | 53.9 (8.5)/53 | 0.48 | 55.9 (8.3)/57 | 55.7 (10.1)/57 | 0.98 |
| Reported using an EMR or EHR, % | 92 | 95 | 94 | ||||||
| Proportion of non-Hispanic white patients, % | |||||||||
| 0–24% | 21 | 12 | 11 | ||||||
| 25–49% | 24 | 24 | 21 | ||||||
| ≥50% | 55 | 64 | 68 | ||||||
| Proportion of black or African-American patients, % | |||||||||
| 0–24% | 79 | 81 | 80 | ||||||
| 25–49% | 16 | 15 | 16 | ||||||
| ≥50% | 5 | 4 | 4 | ||||||
| Proportion of patients with Medicare, % | |||||||||
| 0–24% | NA | 49 | 25 | ||||||
| 25–49% | NA | 39 | 45 | ||||||
| ≥50% | NA | 13 | 30 | ||||||
| Proportion of adult patients with Medicaid, % | |||||||||
| 0–24% | NA | 76 | 86 | ||||||
| 25–49% | NA | 20 | 10 | ||||||
| ≥50% | NA | 4 | 4 | ||||||
| Proportion of child/ adolescent patients with Medicaid or CHIP, % | |||||||||
| 0–24% | 42 | 60 | NA | ||||||
| 25–49% | 27 | 16 | NA | ||||||
| ≥50% | 31 | 24 | NA | ||||||
| Proportion of adult patients with private insurance, % | |||||||||
| 0–24% | NA | 19 | 27 | ||||||
| 25–49% | NA | 34 | 42 | ||||||
| ≥50% | NA | 46 | 31 | ||||||
| Proportion of child/ adolescent patients with private insurance, % | |||||||||
| 0–24% | 27 | 27 | NA | ||||||
| 25–49% | 18 | 17 | NA | ||||||
| ≥50% | 55 | 55 | NA | ||||||
Note: Boldface indicates statistical significance (p < 0.05). Percentages may not add to 100 due to rounding.
CHIP, Child Health Insurance Plan; EHR, electronic health record; EMR, electronic medical record; HMO, health maintenance organization; NA, not applicable.
Physicians’ knowledge of the existence of a state/local IIS and reported IIS use differed markedly by specialty; 91% (289/317) of pediatricians, 82% (252/307) of FPs, and 41% (110/268) of GIMs thought there was an IIS in their locality; 5%, 14%, and 48%, respectively, did not know; and 4%, 4%, and 11%, respectively, reported there was no IIS. Among those who thought there was an IIS, 89% (257/289) of pediatricians, 88% (221/252) of FPs, and 67% (74/110) of GIMs reported using it for any purpose. Among all respondents, 81% (257/317, 95% CI=76, 85) of pediatricians, 72% (221/307, 95% CI=67, 77) of FPs, and 27% (74/268, 95% CI=22, 33) of GIMs (p < 0.0001) reported using an IIS.
Among pediatricians, 75% of all respondents (94% of those who used an IIS) reported submitting child/adolescent immunization data to the IIS; among FPs, 63% (92% among users) entered pediatric data. Only 38% of all FPs reported submitting adult immunization data to the IIS (55% of IIS users), whereas 20% of all GIMs (80% of IIS users) reported submitting adult data. Among all respondents, 73% (95% CI=88, 95) of pediatricians, 62% (95% CI=56, 67) of FPs, and 16% (95% CI=12, 21) of GIMs reported using the IIS to look up patients’ vaccinations (p < 0.0001). Among IIS users, these percentages were 92%, 89%, and 64%, respectively (p < 0.0001).
Among those who reported using the state/local IIS, 38% (95% CI=32, 44) of pediatricians, 40% (95% CI=34, 47) of FPs, and 18% (95% CI=10, 29) of GIMs reported they manually entered immunization data; 23%, 10%, and 11%, respectively, reported that data were uploaded in batches; and 20%, 17%, and 33% reported that data were sent in real time to the IIS from their EMR/EHR. Eighty-five percent of pediatricians, 79% of FPs, and 51% of GIMs reported accessing data from the IIS through an Internet interface and only 6%, 5%, and 8%, respectively, reported that data were sent in real time from the IIS to their EMR/EHR. Overall, based on respondent report, only 4% (95% CI=2, 7), 3% (95% CI=1, 6), and 4% (95% CI=1, 12), respectively, thought their practice had bidirectional connectivity with their IIS.
As shown in Figure 1, only 3%–22% of GIMs thought their IIS could do any standard IIS functions and the majority reported they did not know about IIS functionality. Although most pediatricians and FPs reported using the IIS to look up individual patients’ vaccinations, only 61%–64% of these physicians reported their IIS could determine a patient’s immunization needs at the time of a visit and only about half reported it could forecast immunization needs for future visits. Among those who thought their IIS could tell them a patient’s immunization needs at the time of a visit, 81% (130/160) of pediatricians and 85% (110/128) of FPs reported their practice was using this functionality. Although pediatricians and FPs were more knowledgeable than GIMs regarding most IIS functionalities, the majority did not know if their IIS could be used to order publicly purchased vaccines or track inventory, generate up-to-date rates, or generate lists of patients for reminder/recall.
Figure 1.
Among those that use immunization information system (IIS), providers’ knowledge of IIS functionality (Peds, n=257; FP, n=221; GIM, n=74).
Note: *p ≤ 0.01 for differences between specialties; **p < 0.05 for difference between specialties FP, family physician; GIM, general internists; IIS, immunization information system; IZ, immunization; Peds, pediatricians; UTD, up to date.
Among pediatricians and FPs, respectively, 24% and 29% thought their state mandated reporting of child or adolescent vaccines to the IIS; 34% and 41% did not know. Among FPs and GIMs, respectively, 6% of both groups thought their state mandated reporting adult immunizations, whereas 40% and 43% did not know. Among respondents from states with a definitive reporting mandate for children/adolescent immunizations, 48% (61/127) of pediatricians and 38% (28/74) of FPs reported there was such a mandate. Among respondents from states with a mandate for reporting of adult vaccines, 10% (2/21) of FPs and 13% (4/31) of GIMs were aware of the mandate.
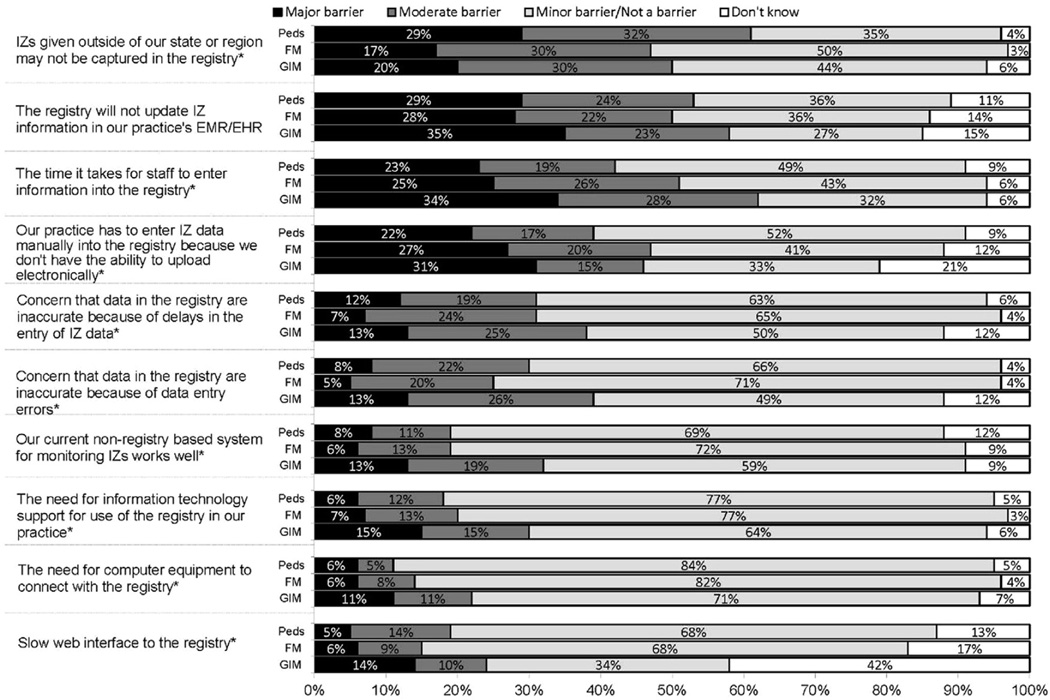
As shown in Figure 2, the major reported barriers to IIS use were related to the time and difficulty of entering information, the fact that vaccinations could not be updated in the practice’s EMR/EHR from the IIS, and concerns about the IIS not capturing data about immunizations given outside of the region or state. Barriers related to information technology needs or slow web interface were infrequently cited. GIMs reported almost all barriers more frequently than the other specialties (Figure 2). In addition to the barriers, respondents were asked whether they agreed or disagreed with the following statement: Assuming that technical problems could be solved, I think using the registry would be valuable for our practice. Seventy-four percent of pediatricians, 73% of FPs, and 41% of GIM respondents strongly agreed, while an additional 20%, 20%, and 41%, respectively, somewhat agreed.
Figure 2.
Barriers to use immunization information system in practice, Peds (n=317), FP (n=307), GIM (n=268).
Note: Barriers <5% in Peds excluded; *barriers differ between specialties at p < 0.01. EHR, electronic health record; EMR, electronic medical record; FP, family physician; GIM, general internists; IZ, immunization; Peds, pediatricians.
As shown in Table 2, FPs and GIMs were significantly less likely than pediatricians to use an IIS, with GIM being the least likely of the primary care specialties. Older physicians were also significantly less likely to use an IIS than younger physicians.
Table 2.
Multivariable Model Predicting Use of the State/Local Registry for Any Function (n=892)
| Variable | Do not use (n=340 [38%]) |
Use registry (n=552 [62%]) |
Unadjusted RR (95% CI) |
Adjusted RR (95% CI) |
|---|---|---|---|---|
| Provider gender, % | NS | |||
| Female | 40.6 | 56.2 | 1.27 (1.14, 1.41) ** | |
| Male | 59.4 | 43.8 | ref | |
| Practice specialty, % | ||||
| Family medicine | 25.3 | 40.0 | 0.89 (0.81, 0.97) ** | 0.91 (0.84, 0.99) ** |
| Pediatrics | 17.7 | 46.6 | ref | ref |
| General internal medicine | 57.0 | 13.4 | 0.34 (0.28, 0.42) ** | 0.37 (0.30, 0.45) ** |
| Practice setting, % | NS | |||
| CHC/public/university | 18.8 | 21.9 | 1.07 (0.95, 1.21) | |
| HMO | 7.7 | 6.5 | 0.95 (0.76, 1.18) | |
| Private | 73.5 | 71.6 | ref | |
| Practice location, % | NS | |||
| Rural | 3.2 | 10.0 | 1.26 (1.11, 1.43) ** | |
| Urban, non-inner city | 46.5 | 29.7 | ref | |
| Urban, inner city | 50.3 | 60.3 | 0.77 (0.68, 0.87) ** | |
| Region, % | ||||
| Midwest | 18.2 | 26.3 | ref | ref |
| Northeast | 26.2 | 16.3 | 0.72 (0.61, 0.85) ** | 0.84 (0.74, 0.96) |
| South | 34.1 | 33.7 | 0.88 (0.78, 1.00) ** | 0.94 (0.86, 1.03) |
| West | 21.5 | 23.7 | 0.92 (0.80, 1.05) ** | 0.96 (0.87–1.05) |
| Provider age, years, M (SD) | 55.6 (8.5) | 51.7 (9.3) | 0.92 (0.89, 0.94) ** | 0.96 (0.94, 0.98) ** |
| Use current EMR/EHR to tell you a patient's immunization needs at the time of the visit, % |
NS | |||
| No | 36.3 | 36.6 | ref | |
| Yes, and we use it | 63.7 | 63.4 | 1.00 (0.89, 1.11) | |
| Use current EMR/EHR to tell you a patient's immunization needs at future visits, % |
NS | |||
| No | 67.6 | 58.3 | ref | |
| Yes, and we use it | 32.4 | 41.7 | 1.15 (1.04, 1.27)** | |
| In your primary outpatient practice, roughly what percent of your patients have private insurance? % |
NS | |||
| 0–24% | 21.7 | 23.7 | ref | |
| ≥25% | 78.4 | 76.3 | 0.96 (0.85, 1.08) | |
| In your primary outpatient practice, roughly what percentage of your patients are Hispanic/Latino or black/African American? % |
NS | |||
| 0–24% | 73.8 | 66.3 | ref | |
| ≥25% | 26.2 | 33.7 | 1.14 (1.03, 1.27)* |
Note: Boldface indicates statistical significance (*p < 0.05; **p < 0.01).
CHC, community health center; EHR, electronic health record; EMR, electronic medical record; HMO, health maintenance organization; NS, not significant; RR, relative risk
DISCUSSION
Strong evidence supports the effectiveness of IISs for facilitating immunization delivery in primary care and increasing immunization rates.15,16 However, this study demonstrates that many primary care physicians are unaware of the existence of a state/local IIS, its functionalities, or state mandates for reporting data into an IIS. Lack of knowledge and use was especially marked among GIMs, with only a quarter reporting any IIS use. This study also demonstrates variation between specialties regarding inputting immunization data into IISs and, among FP practices who care for both children and adults, higher rates of inputting data for children versus adults. Although most pediatricians and FPs report providing immunization data to the IIS and looking up individual patient data in the IIS, the majority either do not know or think their IIS does not have the ability to forecast needed immunizations or assist with reminder/recall, vaccine ordering, or inventory functions.
There are limited data regarding primary care physicians’ knowledge of and use of IISs with which to compare the data reported here. A survey of pediatricians using the same network methodology conducted from September 2011 to January 2012 found that 74% (95% CI=69, 79) of respondents thought their state/region had an IIS and, overall, 59% (95% CI=53, 64) reported using the IIS17 for any purpose. Of those participating, 58% (95% CI=50, 65) reported entering data manually. The current survey, using identical methodology, demonstrated increases in awareness of the existence of an IIS of 17 absolute percentage points and increases in reported use of IISs of 22 absolute percentage points among pediatricians (non-overlapping CIs for both comparisons). A decrease of 20 absolute percentage points was also seen in the proportion of pediatricians who entered data manually rather than electronically reported to the IIS. Although these data do not directly address the reasons for increased use of IISs, they do support the premise that increasing ability to upload immunization data electronically may be a driving factor.
The differences in knowledge and use of IISs by specialty mirror the fact that IISs have historically been focused on childhood vaccines owing to the dominant role that immunizations play in pediatric practice. Reflective of this, FPs were intermediate in IIS use and reported higher rates of reporting immunizations for pediatric versus adult patients. Although IIS use by physicians for adults has lagged, 53 state/local IISs have the capacity to include adult immunizations.4 Physicians who care for adults have compelling reasons to use an IIS. Adult vaccination rates have continued to fall short of Healthy People 2020 targets.18 In addition, new adult vaccines are being recommended and the site of vaccine delivery has shifted away from primary care settings for vaccines such as seasonal influenza vaccinations.19 These factors magnify the importance of using an IIS to consolidate records and increase rates for adults.
The data show that many physicians are unaware of state mandates for reporting immunizations or of state/local IISs functionalities. A recent survey of 53 IISs demonstrated that 59% mandate that at least one type of provider or entity report immunizations to the IIS, 23% mandate that immunizations for all age groups be reported, and 32% that immunizations for children, adolescents, and younger adults be reported.20 All but three IISs have several of the functionalities about which the survey inquired, including a forecasting function for routine childhood immunizations to guide providers about needed recommended immunizations, a vaccine inventory function, the ability to generate lists of patients needing vaccinations for reminder/recall, and the ability to create provider site coverage reports.4,21,22 The majority of GIMs who knew of the existence of an IIS did not know if it had any of these basic functionalities.4,22 Most pediatricians and FPs who reported using an IIS did not know if the IIS could tell them a patient’s immunization needs at the time of a visit. Previous studies have documented private practices’ low use of IIS reminder/recall functions.23–26 The data also demonstrate that few physicians think their IIS can generate lists of patients needing immunizations for conducting reminder/recall, despite this being a basic functionality of almost all IISs.22
The most frequently perceived barriers to IIS use were related to interoperability issues between EMR/EHRs and IISs and time required for manual data entry because of lack of ability to electronically upload data. More than 90% reported they used an EMR/EHR, a rate that is consistent with data from the 2014 National Electronic Health Records Survey.27 Despite this, almost 40% of pediatricians and FPs reported they had to manually enter data into the IIS, and only 3%–4% thought they had bidirectional data transfer. Though most IISs can send and receive basic Health Level 7 messages,4 the disparity between high EMR/EHR use and low ability to communicate electronically with an IIS in one or in both directions seen in this study underlines many EMR/EHRs’ limitations in interfacing with IISs and potential backlogs in state/local onboarding practices to facilitate these interfaces. Although the Centers for Medicare and Medicaid Services has, since 2011, provided financial incentives to ensure “meaningful use” of EHRs by connecting them with other health information systems such as IISs, the data demonstrate that practices continue to face barriers to connectivity,28–31 which will need to be improved to broaden IIS use. The Inability of IISs to capture immunizations given outside of the state or region was another barrier identified by many providers. In 2012, a total of 36 (68%) of IIS programs reported that they could transmit or allow access to immunization data across state borders, although only 29 programs are currently doing so, largely because of legislative authority and other issues.20
The multivariable findings underline the important between specialty differences in IIS use, especially for GIMs. The finding that increasing age of the reporting physician was associated with lower IIS use has not been reported previously, but may be related to greater discomfort with technology or differences in immunization delivery in practices with older providers.
Limitations
There are limitations to the reported findings. The responses of sentinel physicians may not be fully generalizable, although previous work has demonstrated the sampling methods described herein yield similar responses to the most commonly employed method of sampling physicians nationally.7 Non-respondents may have had different views than respondents, although the high reported response rates mitigate against this source of bias. In addition, physicians may have been unaware of immunization activities within their practice if they are less involved in immunization delivery and management and could have under- or over-reported IIS use in the practice. The survey relied on reported measures of practice activities rather than direct observation of immunization delivery activities. Lastly, the reporting mandate analysis relied on summarized information from the Centers for Disease Control and Prevention and reported information about physician characteristics, which could have resulted in some misclassification.
CONCLUSIONS
The data highlight the need to increase primary care physicians’ awareness of the existence of IISs, their capabilities, and state mandates about their use, especially among physicians caring for adults. Although comparisons with previous data do show increased IIS use over time by pediatricians and some progress in the ability to electronically upload data, findings of this study also demonstrate that continued problems with interoperability between EMR/EHRs and IISs are major barriers to expanded use by primary care physicians. The majority of physicians believed IISs could be valuable to their practice if technical problems could be resolved. However, the promise of IISs in guiding immunization decisions in real time and aiding activities, such as reminder/recall and vaccine purchasing and tracking, will not be realized in primary care until barriers to efficient data transfer are eliminated and providers become more aware of the full range of functionality that IISs have to offer.
Acknowledgments
The authors would like to thank Lynn Olson, PhD, and Karen O’Connor from the Department of Research, American Academy of Pediatrics (AAP), Bellinda Schoof, MHA, at the American Academy of Family Physicians (AAFP), Arlene Weissman, PhD and Linda Harris from the American College of Physicians (ACP), and the leaders of the AAP, AAFP, and ACP for collaborating in the establishment of the sentinel networks in pediatrics and family medicine. We would also like to thank all pediatricians and family medicine physicians in the networks for participating and responding to this survey. Finally, the authors appreciate the contribution of SAS code by Dr. Lawrence C. Kleinman and Professor Edward C. Norton to assist with the regression risk analysis.
Funding for this study is from Centers for Disease Control and Prevention, grant 1U01IP000849-01.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Centers for Disease Control and Prevention. Progress in immunization information systems—United States, 2010. MMWR Morbid Mortal Weekly Rep. 2012;61(25):464–467. [PubMed] [Google Scholar]
- 2.Guide to Community Preventive Services. Increasing appropriate vaccination: vaccination programs in schools and organized child care centers. [Accessed June 22, 2016]; www.thecommunityguide.org/vaccines/schools_childcare.html. [Google Scholar]
- 3.Centers for Disease Control and Prevention. IIS state/territory/city registry staff - main & technical contacts. [Accessed September 16, 2015]; www.cdc.gov/vaccines/programs/iis/contacts-registry-staff.html#nh. Published 2015.
- 4.Centers for Disease Control and Prevention. Immunization Information Systems Annual Reports 2014. [Accessed June 22, 2016]; www2a.cdc.gov/nip/registry/IISAR/IISAR_QUERY.asp.
- 5.Centers for Disease Control and Prevention. Progress in immunization information systems—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(49):1005–1008. [PMC free article] [PubMed] [Google Scholar]
- 6.University of Colorado. Vaccine Policy Collaborative Initiative. [Accessed August 10, 2015]; http://www.ucdenver.edu/academics/colleges/medicalschool/programs/ACCORDS/childrensoutcomesreserach/VaccinePolicyCollaborativeInitiative/Pages/default.aspx. [Google Scholar]
- 7.Crane LA, Daley MF, Barrow J, et al. Sentinel physician networks as a technique for rapid immunization policy surveys. Eval Health Prof. 2008;31(1):43–64. doi: 10.1177/0163278707311872. http://dx.doi.org/10.1177/0163278707311872. [DOI] [PubMed] [Google Scholar]
- 8.Dillman DA, Smyth J, Christian LM. Internet, Mail and Mixed-Mode Surveys: The Tailored Design Method. 3rd. New York, NY: John Wiley Co; 2009. [Google Scholar]
- 9.McMahon SR, Iwamoto M, Massoudi MS, et al. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics. 2003;111(4 Pt 1):e299–e303. doi: 10.1542/peds.111.4.e299. http://dx.doi.org/10.1542/peds.111.4.e299. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Survey of State Immunization Information System Legislation. [Accessed January 12, 2016]; www2a.cdc.gov/vaccines/iis/iissurvey/legislation-survey.asp. Published 2015.
- 11.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1691. doi: 10.1001/jama.280.19.1690. http://dx.doi.org/10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 12.Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44(1):288–302. doi: 10.1111/j.1475-6773.2008.00900.x. http://dx.doi.org/10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marschner IC. glm2: fitting generalized linear models with convergence problems. R J. 2011;3(2):12–15. [Google Scholar]
- 14.R Development Core Team. R: a language and environment for statistical computing. [Accessed June 22, 2016];2016 www.R-project.org/ [Google Scholar]
- 15.Groom H, Hopkins DP, Pabst LJ, et al. Immunization information systems to increase vaccination rates: a community guide systematic review. J Public Health Manag Pract. 2015;21(3):227–248. doi: 10.1097/PHH.0000000000000069. http://dx.doi.org/10.1097/PHH.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 16.The Community Guide. Guide to Community Preventive Services. [Accessed June 22, 2016];Increasing appropriate vaccination: immunization information systems. www.thecommunityguide.org/vaccines/imminfosystems.html. Updated July 17, 2014. [Google Scholar]
- 17.O’Leary ST, Hurley LP, Kennedy ED, et al. Provider attitudes regarding vaccine tracking systems in pediatric practices. Acad Pediatr. 2016;16(1):34–41. doi: 10.1016/j.acap.2015.04.038. http://dx.doi.org/10.1016/j.acap.2015.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Vaccination coverage among adults, excluding influenza vaccination—United States 2013. MMWR Morb Mortal Wkly Rep. 2013;64(04):95–102. [PMC free article] [PubMed] [Google Scholar]
- 19.Hurley LP, Bridges CB, Harpaz R, et al. U.S. physicians’ perspective of adult vaccine delivery. Ann Intern Med. 2014;160(3):161. doi: 10.7326/M13-2332. http://dx.doi.org/10.7326/M13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin DW, Lowery NE, Brand B, Gold R, Horlick G. Immunization information systems: a decade of progress in law and policy. J Public Health Manag Pract. 2015;21(3):296–303. doi: 10.1097/PHH.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Progress in immunization information systems—United States 2012. MMWR Morb Mortal Wkly Rep. 2012;62(49):1005–1008. [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Immunization Information System Annual Report. [Accessed November 7, 2015]; www.cdc.gov/vaccines/programs/iis/annual-report-iisar/rates-maps-table.html. Published 2012.
- 23.Saville AW, Albright K, Nowels C, et al. Getting under the hood: exploring issues that affect provider-based recall using an immunization information system. Acad Pediatr. 2011;11(1):44–49. doi: 10.1016/j.acap.2010.12.009. http://dx.doi.org/10.1016/j.acap.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Kempe A, Saville AW, Dickinson LM, et al. Collaborative centralized reminder/recall notification to increase immunization rates among young children: a comparative effectiveness trial. JAMA Pediatr. 2015;169(4):365–373. doi: 10.1001/jamapediatrics.2014.3670. http://dx.doi.org/10.1001/jamapediatrics.2014.3670. [DOI] [PubMed] [Google Scholar]
- 25.Kempe A, Saville A, Dickinson LM, et al. Population-based versus practice-based recall for childhood immunizations: a randomized controlled comparative effectiveness trial. Am J Public Health. 2013;103(6):1116–1123. doi: 10.2105/AJPH.2012.301035. http://dx.doi.org/10.2105/AJPH.2012.301035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dombkowski KJ, Cowan AE, Harrington LB, et al. Feasibility of initiating and sustaining registry-based immunization recall in private practices. Acad Pediatr. 2012;12(2):104–109. doi: 10.1016/j.acap.2012.01.002. http://dx.doi.org/10.1016/j.acap.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Office of the National Coordinator for Health Information Technology. [Accessed April 2016];Office-based Physician Health IT Adoption. http://dashboard.healthit.gov/dashboards/physician-health-it-adoption.php. Published 2016.
- 28.Centers for Disease Control and Prevention. Meaningful use and immunization information systems. [Accessed January 12, 2016]; www.cdc.gov/vaccines/programs/iis/meaningful-use/index.html. Published 2012.
- 29.Centers for Disease Control and Prevention. Meaningful use. [Accessed January 12, 2016]; www.cdc.gov/ehrmeaningfuluse/introduction.html. Published 2012.
- 30.Centers for Medicare and Medicaid Services. Electronic Health Records (EHR) Incentive Programs Regulations and Guidance 2016. [Accessed January 12, 2016]; http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html.
- 31.Cardemil CV, Cullen KA, Harris L, Greby SM, Santibanez TA. Factors associated with provider reporting of child and adolescent vaccination history to immunization information systems: results from the National Immunization Survey, 2006–2012. J Public Health Manag Pract. 2016;22(3):245–254. doi: 10.1097/PHH.0000000000000278. http://dx.doi.org/10.1097/PHH.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]