Abstract
Background
Recurrence of takotsubo cardiomyopathy (TTC) is a well-known complication. However, current literature lists only a few isolated cases. We aimed to determine the incidence and clinical significance of recurrent TTC.
Methods & Results
Our institutional database constituted a collective of 114 patients diagnosed with TTC since 2003. Close follow-up of these patients revealed a recurrence of TTC in seven of these (6.1%). The time interval between the index event and its recurrence varied between six months and six years. Arterial hypertension was more revealed in the recurrence group of TTC compared to non-recurrence group, (P = 0.02). Chronic obstructive pulmonary disease and/or asthma was more diagnosed in the recurrence group, (P = 0.04). Clinical events like right ventricular involvement, TTC related complications such as life-threatening arrhythmias, pulmonary congestion and in hospital death were observed more frequently in the recurrent episode. Over a mean follow-up of one year the mortality rate was similar in both groups.
Conclusions
Recurrence of TTC within six years after index event is not an uncommon phenomenon. In the event of right ventricular involvement in the relapse phase, it might be associated with a higher complication rate. TTC recurrence should be the first differential diagnosis in patients with a past history of TTC.
Keywords: Biventricular takotsubo cardiomyopathy, Recurrent takotsubo cardiomyopathy, Takotsubo cardiomyopathy related complication
1. Introduction
Takotsubo Cardiomyopathy (TTC) is a transient disorder of ventricular wall dysfunction characterized by a range of wall motion abnormalities. It is usually representative of an acute heart failure syndrome with substantial risk for adverse events. First described in 1990,[1] the term takotsubo is derived from the Japanese word for ‘octopus pot’, and is used to describe the typical ballooning of the left ventricular apex. In addition to the wall motion abnormalities of the middistal and apical regions and decreased ejection fraction (EF), right ventricular (RV) involvement has been described in up to 27% of patients.[2],[3]
An early classification system based on the ballooning pattern of ventricular walls, as diagnosed by transthoracic echocardiography and laevo-cardiography, has made it possible to sort patients into particular groups.[4] The apical form is the most common (81.7%) followed by midventricular form (14.6%), basal (2.2%) and focal form (1.5%). The exact pathophysiological mechanism for selective wall motion abnormality in the absence of significant coronary artery stenosis remains unknown. Patients present with symptoms such as chest pain and dyspnea, which may mimic an acute coronary artery syndrome (ACS). The ECG findings, echocardiographic findings and laboratory parameters could also be similar to ACS and a spontaneous recovery of the myocardium is usually observed within days or weeks. The recurrence of TTC is a rare phenomenon. Current literature details only a few isolated case reports,[5]–[10] however a recent meta-analysis outlines a recurrence rate of up to 20%.[11] The present study was performed to determine the incidence, clinical characteristics and prognostic impact of patients suffering from recurrent TTC.
2. Methods
We observed 114 consecutive patients diagnosed with TTC from January 2003 to September 2015 in the TTC database of our institution. Patients were diagnosed according to the Mayo Clinic Criteria,[12] which outlines the clinical features associated with TTC.
The first criterion describes the transient wall motion abnormality in the left ventricular (LV) mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and frequently, but not always in the event of a stressful trigger. The second criterion stipulates the absence of obstructive coronary disease. The third criterion outlines the appearance of new ECG pathologies, which mimic ACS or modest elevations in cardiac troponin levels. The final criterion is the absence of pheochromocytoma and myocarditis in the patient. The cases were divided into two groups on the basis of presence (acute or chronic) and absence of atrial fibrillation as assessed by ECG at admission.
The angiograms, echocardiograms and ECGs were reviewed by two experienced independent cardiologists to evaluate the diagnosis of TTC. This study was conducted in compliance with the Declaration of Helsinki with regard to investigations in human subjects and the study protocol was approved by the Ethics Committee of University Medical Centre Mannheim.
In-hospital events, arrhythmias, cardiac rupture, thromboembolic events, pulmonary congestion with use of non-invasive positive-pressure ventilation, intubation, use of a temporary pacemaker, use of inotropic agents, and in-hospital death were assessed based on chart review. The primary end point of our study was a recurrence of TTC and prognostic impact as assessed by chart review and/or telephone review.
Data are presented as means ± SD for continuous variables with a normal distribution, median (interquartile range) for continuous variables with a non-normal distribution, and as frequency (%) for categorical variables. The Kolmogorov-Smirnov test was used to assess normal distribution. Student's t-test and the Mann-Whitney U-test were used to compare continuous variables with normal and non-normal distributions, respectively. The Chi-squared-test or Fisher's exact test was used to compare categorical variables. The log-rank test was used to compare the survival curves between the recurrence group and the non-recurrence group. Statistical analysis was performed with SPSS in all analyses, P ≤ 0.05 (two-tailed) was taken to indicate statistical significance.
3. Results
3.1. Clinical features of TTC patients
Mean age of whole TTC patients was 67 ± 11 years, with a predominance of female gender (83%). A total of 70% of patients were admitted to the hospital with clinical signs of ACS. The most common clinical symptom was chest pain (50.8%) followed by dyspnea (37%). ST-segment elevation in ECG was observed in 34 patients (30%) and inverted T-waves in 102 patients (89.5%). Patient history revealed emotional and physical stress in 29% and 56% of cases, respectively. Mild elevation of cardiac enzymes, troponin I and creatine kinase (CK), was confirmed in 95% and 43%. LV function was moderate reduced at admission (EF: 38.3%) measured by transthoracic echocardiography and laevo-cardiography. RV involvement was presented in 22.8% of cases. Apical type TTC was observed in 72.8% of patients (Figure 1), whereas midventricular type (Figure 1) and reversed type were revealed in 24.5% and 0.9%, respectively. The most frequent complications have been investigated to be life-threatening arrhythmia (11.4%), pulmonary congestion with need for invasive respiratory support (20%), thromboembolism events (12.2%), cardiogenic shock (19.2%) and in-hospital death (7.8%).
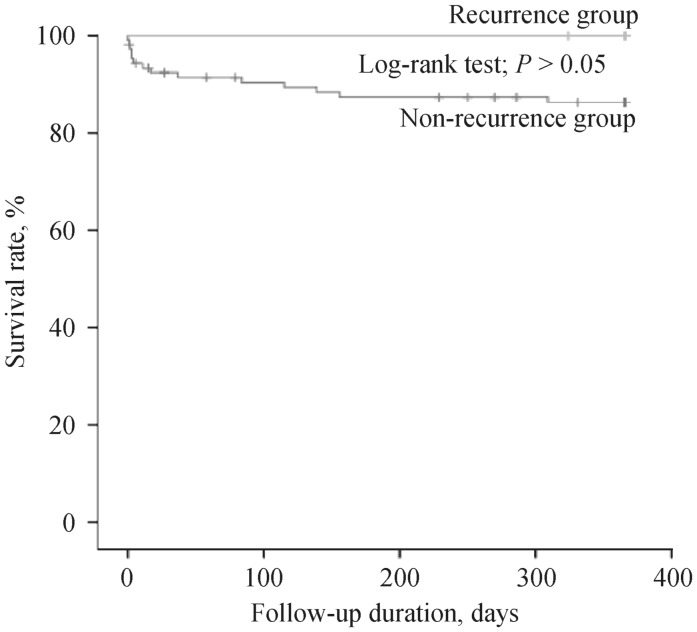
Figure 1. Short- and long-term mortality of TTC patients in presence and absence of recurrent TTC.
TTC: takotsubo cardiomyopathy.
3.2. Baseline demographics of patients with recurrent TTC
We studied clinical and echocardiographic data of 114 patients with TTC and a mean follow-up of 1521 ± 1121 days. Baseline demographics with a predominance of postmenopausal females in both groups were presented in Table 1. Patients were divided in two groups according to the presence (n = 7, 6.1%) or absence (n = 107, 93.9%) of recurrent TTC. Compared with the non-recurrence group the incidence of arterial hypertension was higher in the recurrence group. Additionally, more pulmonary disease such as chronic obstructive pulmonary disease and/or asthma was presented in the recurrent group. Recurrent TTC patients were similar treated with beta-blocking drugs, digitalis and therapeutic anticoagulation at admission as compared to the non-recurrent patients. ECG data revealed higher prevalence of valvular heart disease in the recurrence group. There were no significant differences with relation to LVEF. RV involvement was significantly more revealed in patients with recurrent TTC compared to non-recurrent TT patients. The detailed baseline characteristics of patients suffering from recurrent TTC are figured out in Table 2.
Table 1. Baseline characteristics of 114 patients initially presenting with TTC.
| Variables | Non-recurrence group (n = 107) | Recurrence group (n = 7) | P value * |
| Demographics | |||
| Age | 67.02 ± 11.17 | 69.29 ± 12.97 | 0.44 |
| Female | 88 (82.2%) | 7 (100%) | 0.22 |
| Symptoms | |||
| Dyspnea | 38 (35.5%) | 5 (71.4%) | 0.10 |
| Chest pain | 54 (50.4%) | 6 (85.7%) | 0.11 |
| Clinic parameter | |||
| Systolic BP, mmHg | 129.3 ± 31.3 | 159 ± 33.4 | 0.01 |
| Diastolic BP, mmHg | 76.3 ± 17.4 | 82.5 ± 22 | 0.49 |
| Heart rate, bpm | 100 ± 27 | 107 ± 19.6 | 0.52 |
| ECG Data | |||
| ST-segment elevation | 31 (29%) | 4 (57.1%) | 0.19 |
| PQ-interval | 160.2 ± 29.4 | 165.1 ± 27.5 | 0.66 |
| QTc-interval, ms | 478.8 ± 53.3 | 481 ± 35.7 | 0.91 |
| Stress factor | |||
| Emotional stress | 29 (27.1%) | 1 (14.3%) | 0.67 |
| Physical stress | 60 (56%) | 3 (42.8%) | 0.69 |
| Laboratory values | |||
| Troponin I, U/L | 3.9 ± 5.5 | 0.7 ± 0.6 | 0.12 |
| Creatine phosphatkinase, U/L | 683.0 ± 2731.3 | 197.1 ± 211.5 | 0.64 |
| C-reactivated protein, mg/L | 50.0 ± 80.9 | 39.3 ± 59.2 | 0.75 |
| Hemoglobin, g/dL | 12.1 ± 2.0 | 12.2 ± 1.9 | 0.94 |
| Creatinine, mg/dL | 1.1 ± 0.7 | 1.0 ± 0.3 | 0.68 |
| Echocardiography data | |||
| LVEF, % | 38.10 ± 9.49 | 42.43 ± 8.82 | 0.24 |
| Right ventricular involvement | 22 (19.2%) | 4 (57.1%) | 0.04 |
| Apical ballooning | 77 (72%) | 5 (71.5%) | 1.00 |
| Non-apical ballooning | 30 (28%) | 2 (28.5%) | 1.00 |
| Mitral regurgitation | 54 (50.4%) | 6 (85.7%) | 0.11 |
| Tricuspid regurgitation | 44 (41%) | 5 (71.4%) | 0.13 |
| Medical history | |||
| Smoking | 32 (29.9%) | 4 (57.1%) | 0.20 |
| Diabetes mellitus | 23 (21.5%) | 3 (42.8%) | 0.19 |
| BMI > 25 kg/m2 | 29 (27.1%) | 2 (28.6%) | 0.70 |
| Hypertension | 59 (55.1%) | 7 (100%) | 0.02 |
| COPD and or asthma | 22 (20.5%) | 4 (57.1%) | 0.04 |
| Atrial fibrillation | 21 (19.6%) | 0 | 0.34 |
| Coronary artery disease | 21 (19.6%) | 1 (14.3%) | 1.00 |
| History of malignancy | 15 (14%) | 1 (14.3%) | 1.00 |
| Drugs on admission | |||
| Beta-blocker | 32 (30%) | 3 (42.8%) | 0.69 |
| ACE inhibitor | 33 (30.8%) | 2 (28.6%) | 1.00 |
| Digitalis | 1 (0.9%) | 0 | 1.00 |
| Aspirin | 26 (24.3%) | 3 (42.8%) | 0.41 |
| Therapeutic anticoagulation | 7 (6.5%) | 0 | 1.00 |
*P values for the comparison between non-recurrence and recurrence group. Data are presented as n (%) or mean ± SD. ACE: Angiotensin-convetring-enzyme; BMI: body-mass-index; COPD: Chronic obstructive pulmonary disease; LVEF: left ventricular ejection fraction; TTC: takotsubo cardiomyopathy.
Table 2. Detailed clinical and echocardiographic characteristics of patients suffering from recurrent TTC.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| Variables | |||||||
| Age | 77 | 77 | 50 | 86 | 71 | 63 | 73 |
| Sex | Female | Female | Female | Female | Female | Female | Female |
| Angina pecotris | + | + | + | + | − | + | + |
| Collapse | 0 | 0 | 0 | 0 | − | 0 | 0 |
| ST-segment elevation | + | 0 | + | 0 | + | 0 | + |
| Inverted T-waves | + | + | + | + | + | + | 0 |
| QTc-interval, ms | 620 | 504 | 483 | 405 | 462 | 486 | − |
| Emotional sress | 0 | 0 | 0 | 0 | − | 0 | + |
| Physical stress | 0 | 0 | + | + | − | + | 0 |
| Troponin I, µg/L | 1.7 | 0.02 | 0.5 | 0.09 | − | 0.3 | 0.93 |
| Creatine phosphatkinase, U/L | 143 | 42 | 533 | 144 | − | 176 | 126 |
| LV EF, % | 38 | 56 | 47 | 40 | 44 | 50 | 32 |
| Right ventricular involvement | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Apical type | + | + | 0 | + | + | 0 | + |
| Midventricular type | 0 | 0 | + | 0 | 0 | + | 0 |
| Reversed type | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Life-threatening arrhythmias | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Invasive respiratory support | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Thromboembloic events | + | 0 | 0 | 0 | 0 | 0 | 0 |
| Cardiogenic shock | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| In-hospital death | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Recurrent episode | |||||||
| Age | 80 | 78 | 56 | 88 | 72 | 65 | 74 |
| Angina pecotris | + | + | + | 0 | + | + | + |
| Collapse | 0 | 0 | 0 | + | 0 | 0 | 0 |
| ST-segment elevation | + | 0 | + | 0 | + | 0 | 0 |
| Inverted T-waves | + | + | + | 0 | + | + | + |
| QTc-interval, ms | 510 | 458 | 429 | 523 | 503 | 488 | 380 |
| Emotional sress | + | 0 | 0 | 0 | + | 0 | 0 |
| Physical stress | 0 | 0 | + | + | 0 | + | + |
| Troponin I, µg/L | 1.3 | 0.98 | 3.2 | 3.8 | 0 | 0.71 | 0.26 |
| Creatine phosphatkinase, U/L | 88 | 75 | 227 | 335 | 0 | 127 | 42 |
| LV EF, % | 43 | 60 | 47 | 42 | 45 | 35 | 45 |
| Right ventricular involvement | + | 0 | 0 | 0 | + | + | + |
| Apical type | + | + | 0 | + | + | 0 | + |
| Midventricular type | 0 | 0 | + | 0 | 0 | + | 0 |
| Reversed type | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Life-threatening arrhythmias | 0 | + | 0 | + | 0 | 0 | 0 |
| Invasive respiratory support | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Thromboembloic events | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cardiogenic shock | 0 | 0 | 0 | 0 | 0 | 0 | + |
| In-hospital death | 0 | 0 | 0 | 0 | 0 | 0 | + |
*+, positive; 0, negative; −, no information available. LVEF: left ventricular ejection fraction; TTC: takotsubo cardiomyopathy.
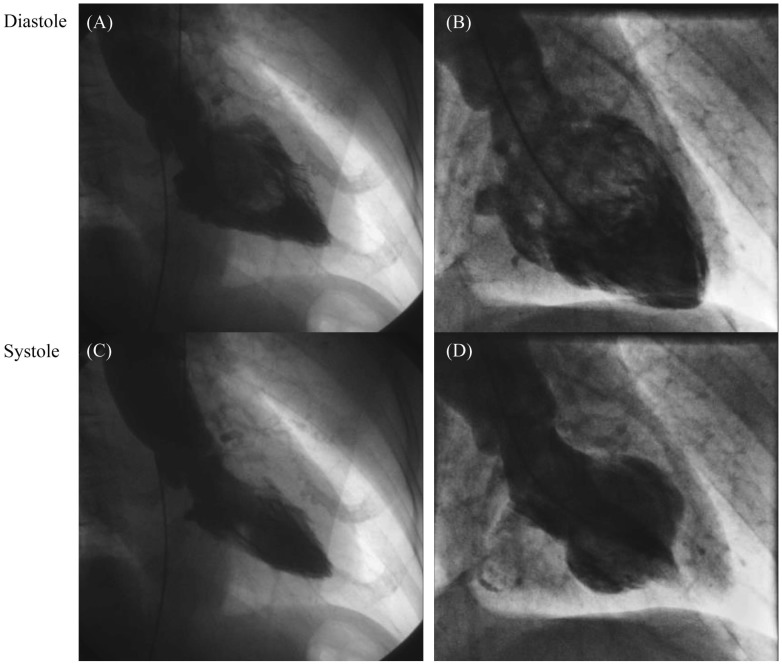
Figure 2. Laevo-cardiography of patients with recurrent apical TTC (left panel) and recurrent midventricular TTC (right panel).
TTC: takotsubo cardiomyopathy. (A) & (C): severe akinesia/dyskinesia of the apical portions of left ventricular. (B) & (D): present severe akinesie/dyskinesia of the mid portions of left ventricular.
3.3. Long-term prognosis
Patients suffering from recurrent TTC revealed similar in-hospital mortality, similar 30-day mortality as well as similar long-term mortality compared to patients without recurrent TTC (Figure 1).
4. Discussion
In the current issue, we performed a retrospective clinical investigation in 114 consecutive TTC patients, and showed that (1): recurrent TTC is not uncommon; (2): patients with recurrent TTC have more arterial hypertension and pulmonary disease; (3): the in-hospital morbidity and mortality rates as well as the long term mortality was similar in these patients compared to non-recurrent TTC patient.
All patients with recurrent TTC are postmenopausal women, who are usually more affected than men.[13]–[15] The basis for this observation remains unknown. Estrogen, which has a beneficial effect on cardiomyocytes, is usually low in this situation, offering a probable explanation.[16] The disease is also generally provoked by emotional or physical stress.[13]–[15],[17],[18] Furthermore, coronary vasospasm and widespread coronary microvascular dysfunction[14],[19] might play a role in the mechanism of TTC. Nef, et al.[20] have proposed that oxidative stress, triggered by excessive catecholamines, may contribute to the pathophysiology of TTC.
The recurrence rate of TTC in our analysis is 6.1% during a mean follow-up of six years. Elesber, et al.[2] have reported a 11.4% recurrence rate in a mean follow-up of four years. Clinical presentation was similar to the index-event.
Recurrent episodes of TTC can present with ST-segment elevation, inverted T-waves and almost in all cases QTc-interval prolongation in at least one of the episodes if not both. The prevalence of QTc-interval prolongation has been reported to be up to 50% of all TTC cases.[21]
In this study, patients with recurrent TTC had higher prevalence of arterial hypertension and chronic obstructive pulmonary disease as well as asthma. Patients with pulmonary disease, who use frequently inhaled beta-receptor agonists might be more affected to recurrent TTC.
Furthermore, our study revealed that during recurrence episode, variable patterns of TTC could occur. Four patients had RV involvement with the second episode, but presented with a similar left ventricular pattern. This variable form of TTC in the same patient could not be explained by the previously proposed association of TTC with a beta-receptor gradient. Singh, et al.[5] have also reported variable patterns of LV involvement. Although myocardial responsiveness to adrenergic stimulation is increased in the apical region,[22] norepinephrine content is lower in the apex than in the base.[23] Individual variation in the regional myocardial vulnerability might determine the location which could be affected in TTC patients.[24]–[26]
The death of two patients with recurrent TTC in this study is probably related to TTC. The first patient (Case 1) was found dead in her bathroom. An arrhythmic disorder as a cause of her death due to the recurrent TTC episode could be a probable cause of death. The second patient died due to cardiogenic shock. TTC related complications such as congestive heart failure, cardiogenic shock, respiratory distress and lethal arrhythmias have been documented.[27]
In conclusion, recurrence of TTC is not an uncommon phenomenon and occurs mostly within three years after the index event. Arterial hypertension and chronic pulmonary disease might be positive predictors of recurrent TTC. Due to the additional involvement of the RV in the second episode it could be associated with a higher rate of adverse events. In summary, it is pertinent to consider TTC recurrence as the first differential diagnosis in patients with a history of TTC.
References
- 1.Dote K, Sato H, Tateishi H, et al. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol. 1991;21:203–214. [PubMed] [Google Scholar]
- 2.Elesber A, Lerman A, Bybee KA, et al. Myocardial perfusion in apical ballooning syndrome: correlate of myocardial injury. Am Heart J. 2006;152:469 e469–e413. doi: 10.1016/j.ahj.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Haghi D, Papavassiliu T, Fluchter S, et al. Variant form of the acute apical ballooning syndrome (takotsubo cardiomyopathy): observations on a novel entity. Heart. 2006;92:392–394. doi: 10.1136/hrt.2005.061044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Templin C, Ghadri JR, Diekmann J, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 5.Singh K, Parsaik A, Singh B. Recurrent takotsubo cardiomyopathy: variable pattern of ventricular involvement. Herz. 2014;39:963–967. doi: 10.1007/s00059-013-3896-x. [DOI] [PubMed] [Google Scholar]
- 6.Ratanapo S, Srivali N, Cheungpasitporn W, et al. Reported cases of recurrent takotsubo cardiomyopathy with variant forms of left ventricular dysfunction. Am J Med. 2013;126:e27. doi: 10.1016/j.amjmed.2012.12.025. [DOI] [PubMed] [Google Scholar]
- 7.Mainali NR, Aryal MR, Pradhan R, et al. An unusual cause of recurrent chest pain in an adult woman: a case of recurrent stress-induced (Takotsubo) cardiomyopathy. BMJ Case Rep. 2013;pii:bcr2013009546. doi: 10.1136/bcr-2013-009546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sardar MR, Kuntz C, Mazurek JA, et al. Recurrent takotsubo cardiomyopathy in the setting of transient neurological symptoms: a case report. J Med Case Rep. 2011;5:412. doi: 10.1186/1752-1947-5-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pathak H, Esses J, Pathak S, et al. A unique case of recurrent takotsubo cardiomyopathy. South Med J. 2010;103:805–806. doi: 10.1097/SMJ.0b013e3181e631ce. [DOI] [PubMed] [Google Scholar]
- 10.Maroules CD, Linz NA, Boswell GE. Recurrent takotsubo cardiomyopathy. J Cardiovasc Comput Tomogr. 2009;3:187–189. doi: 10.1016/j.jcct.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Singh K, Carson K, Usmani Z, et al. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol. 2014;174:696–701. doi: 10.1016/j.ijcard.2014.04.221. [DOI] [PubMed] [Google Scholar]
- 12.Madhavan M, Prasad A. Proposed mayo clinic criteria for the diagnosis of Tako-Tsubo cardiomyopathy and long-term prognosis. Herz. 2010;35:240–243. doi: 10.1007/s00059-010-3339-x. [DOI] [PubMed] [Google Scholar]
- 13.Ito K, Sugihara H, Kawasaki T, et al. Assessment of ampulla (Takotsubo) cardiomyopathy with coronary angiography, two-dimensional echocardiography and 99mTc-tetrofosmin myocardial single photon emission computed tomography. Ann Nucl Med. 2001;15:351–355. doi: 10.1007/BF02988242. [DOI] [PubMed] [Google Scholar]
- 14.Kurisu S, Inoue I, Kawagoe T. Conditions associated with left ventricular apical ballooning. Clin Cardiol. 2010;33:E123–124. doi: 10.1002/clc.20726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. doi: 10.1016/j.ahj.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Movahed MR, Donohue D. Review: transient left ventricular apical ballooning, broken heart syndrome, ampulla cardiomyopathy, atypical apical ballooning, or Tako-Tsubo cardiomyopathy. Cardiovasc Revasc Med. 2007;8:289–292. doi: 10.1016/j.carrev.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Akashi YJ, Goldstein DS, Barbaro G, et al. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118:2754–2762. doi: 10.1161/CIRCULATIONAHA.108.767012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bybee KA, Prasad A, Barsness GW, et al. Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am J Cardiol. 2004;94:343–346. doi: 10.1016/j.amjcard.2004.04.030. [DOI] [PubMed] [Google Scholar]
- 19.Tsuchihashi K, Ueshima K, Uchida T, et al. Angina Pectoris-Myocardial Infarction Investigations in J. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 20.Nef HM, Mollmann H, Troidl C, et al. Expression profiling of cardiac genes in Tako-Tsubo cardiomyopathy: insight into a new cardiac entity. J Mol Cell Cardiol. 2008;44:395–404. doi: 10.1016/j.yjmcc.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 21.Song BG, Chung SM, Kim SH, et al. The QT prolongation and clinical features in patients with takotsubo cardiomyopathy: experiences of two tertiary cardiovascular centers. Anadolu Kardiyol Derg. 2014;14:162–169. doi: 10.5152/akd.2013.4745. [DOI] [PubMed] [Google Scholar]
- 22.Mori H, Ishikawa S, Kojima S, et al. Increased responsiveness of left ventricular apical myocardium to adrenergic stimuli. Cardiovasc Res. 1993;27:192–198. doi: 10.1093/cvr/27.2.192. [DOI] [PubMed] [Google Scholar]
- 23.Pierpont GL, DeMaster EG, Cohn JN. Regional differences in adrenergic function within the left ventricle. Am J Physiol. 1984;246:H824–H829. doi: 10.1152/ajpheart.1984.246.6.H824. [DOI] [PubMed] [Google Scholar]
- 24.Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 25.Gogas BD, Antoniadis AG, Zacharoulis AA, et al. Recurrent apical ballooning syndrome “The masquerading acute cardiac syndrome”. Int J Cardiol. 2011;150:e17–19. doi: 10.1016/j.ijcard.2009.07.038. [DOI] [PubMed] [Google Scholar]
- 26.Koeth O, Mark B, Zahn R, et al. Midventricular form of takotsubo cardiomyopathy as a recurrence 1 year after typical apical ballooning: a case report. Cases J. 2008;1:331. doi: 10.1186/1757-1626-1-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stiermaier T, Eitel C, Denef S, et al. Prevalence and clinical significance of life-threatening arrhythmias in takotsubo cardiomyopathy. J Am Coll Cardiol. 2015;65:2148–2150. doi: 10.1016/j.jacc.2015.02.062. [DOI] [PubMed] [Google Scholar]