Abstract
Objectives
Bile acid diarrhoea (BAD) is an underdiagnosed condition producing diarrhoea, urgency and fear of faecal incontinence. How patients experience these symptoms has not previously been studied. Bile Acid Malabsorption (BAM) Support UK was established in 2015 as a national charity with objectives including to provide details regarding how BAD affects patients, to improve earlier recognition and clinical management.
Design, setting and main outcome
A questionnaire was collected anonymously by BAM Support UK and the Bile Salt Malabsorption Facebook group over 4 weeks at the end of 2015. It comprised 56 questions and aimed to inform patients and clinicians about how BAD affects the respondents.
Results
The first 100 responses were analysed. 91% of the respondents reported a diagnosis of BAD. 58% of total respondents diagnosed following a Selenium-homocholic acid taurine scan, 69% were diagnosed by a gastroenterologist, with type 2 and 3 BAD comprising 38% and 37%, respectively, of total respondents. Symptoms had been experienced for more than 5 years before diagnosis in 44% of respondents. Following treatment, usually with bile acid sequestrants, 60% of participants reported improvement of diarrhoea and most reported their mental health has been positively impacted. Just over half of the cohort felt as though their symptoms had been dismissed during clinical consultations and 28% felt their GPs were unaware of BAD.
Conclusions
BAD requires more recognition by clinicians to address the current delays in diagnosis. Treatment improves physical and mental symptoms in the majority of participants.
Keywords: BILE ACID, DIARRHOEA, IRRITABLE BOWEL SYNDROME, MALABSORPTION
What is already known about this subject?
-
▸
Bile acid diarrhoea (BAD) is an under-recognised condition.
-
▸
Symptoms of BAD are debilitating and negatively affect daily activities of affected individuals.
-
▸
Recent research recommendations advise on the use of Selenium-homocholic acid taurine scan and bile acid sequestrants in investigation and treatment of BAD, respectively.
What are the new findings?
-
▸
The study highlights the delays in diagnosing bile acid diarrhoea (BAD) with many patients waiting for more than 5 years.
-
▸
Patients feel there is lack of awareness about BAD by clinicians and they feel their symptoms are dismissed or labelled as just irritable bowel syndrome.
-
▸
Patients reported improvement in physical and mental symptoms following treatment with bile acid sequestrants. Specially in areas of embarrassment, low self-esteem and feeling nervous leaving home.
How might it impact on clinical practice in the foreseeable future?
-
▸
To encourage clinicians to actively investigate for bile acid diarrhoea (BAD) in patients with chronic diarrhoea.
-
▸
Prescribing bile acid sequestrants for patients leads to significant improvement in mental and physical symptoms.
-
▸
Patients support groups continue to raise public and clinicians' awareness about BAD.
Introduction
Bile acids are produced by the liver, secreted into the duodenum and are necessary for lipid absorption in the small intestine. Bile acids are absorbed from the ileum by specific transporters and undergo an enterohepatic circulation where they are resecreted by the liver. When disruption of the absorption of the bile acids in the ileum occurs, bile acids reach the colon in excess amounts, and this leads to increased secretion, accelerated transit and hence diarrhoea. This disruption can be due to inflammation, as in Crohn's disease and/or ileal resection; this type of diarrhoea is known as bile acid malabsorption or secondary bile acid diarrhoea (BAD). Conversely, primary BAD occurs in those with an intact gut, often seen in those previously thought to have diarrhoea predominant irritable bowel syndrome (IBS) and appears to be the result of excess synthesis.1–3 BAD is commonly reported after cholecystectomy and some other gastrointestinal conditions; a classification based on the order they were recognised is commonly used (box 1).4
Box 1. Types of bile acid diarrhoea.
Type 1: Bile acid malabsorption, secondary to ileal resection, or ileal inflammation (Crohn's disease).
Type 2: Idiopathic/primary bile acid malabsorption.
Type 3: Secondary to various gastrointestinal diseases (cholecystectomy, small intestinal bacterial overgrowth, post radiation, coeliac disease, chronic pancreatitis).
It is estimated that 1% of the population are affected by BAD. One out of three patients with IBS can also have BAD.5 Symptoms of BAD are debilitating and impact considerably on daily activities of patients due to urgency to go to the toilet, increased bowel frequency and the fear of incontinence. BAD can be diagnosed by measuring faecal bile acids or the Selenium-homocholic acid taurine (SeHCAT) test. The Se-labelled bile acid is administered orally and the total body retention is measured with a gamma camera after 7 days. Retention value of <15% is considered abnormal and indicative of BAD.6 The mainstay of treatment for BAD is bile acid sequestrants (BAS). The three commercially available BAS are colestyramine, colestipol and colsevelam. BAS bind to the bile acids to prevent the secretory effects of bile acids on the colon, hence improving diarrhoea in the majority of patients who have BAD.
Early diagnosis of BAD is predicted to lead to decreased morbidity, increased quality of life and fewer referrals to the gastroenterologists.7–9 However, little is known about how people with this condition experience their symptoms, diagnosis and treatment. Patient support groups have only recently been established. This manuscript reports the findings of the first study of patient-reported symptoms and outcomes.
Methods and design of study
The study was designed by BAM Support UK. This is a national charity group set up in April 2015 in Coventry, UK, with the main aim to increase awareness about BAD (http://bamsupportuk.org). Its vision is to empower patients to live life to the full and build a network of local patient groups across the UK to provide support and improve earlier recognition of the condition and ongoing clinical management.
BAM Support UK, with help from the Bile Salt Malabsorption Facebook Group members (current membership exceeds 1300), conducted an online questionnaire via a Facebook link page. The questionnaire included 56 different questions divided into demography of the respondents, how and when diagnosis was made, symptoms before and after treatment and different types of diet used by the respondents.
The main outcome was to inform patients and clinicians about how BAD affects the responders. The questionnaire was collected anonymously between November and December 2015 and analysed when 100 responses had been obtained. Patient responses were collated and analysed. Statistical comparisons of frequencies of symptoms before and after treatment were compared by two-tailed Fisher's exact test.
Results
The total number of respondents was 100 comprising 91 (91%) women and 9 (9%) men. Nine respondents (9%) were excluded from the results because they had not been formally diagnosed with BAD. The rest of this analysis will focus on the responses of those who have received a diagnosis (91%) as the sample group of those undiagnosed is too small to have any statistical significance.
Diagnosis
At the time of the diagnosis, about half (52%) of the respondents were aged between 36 and 55 years, with 20% aged 56 years or above. The majority of respondents (79%) lived in the UK, while 14% lived in North America.
Sixty-nine per cent of the total respondents have been diagnosed after consulting a gastroenterologist. Fifty-eight per cent (n=58) of the total respondents were diagnosed following a SeHCAT scan. Thirty-three per cent (n=33) of the total respondents were diagnosed following a successful trial of bile binding medication or by symptoms alone. Patients with type 2 and type 3 of BAD represented 38% and 37%, respectively. Sixty-seven per cent of patients with BAD were diagnosed with IBS.
Seventy-eight per cent of respondents had more than one test before diagnosed, while 59% had more than two tests. Most of the respondents were investigated by a lower gastrointestinal endoscopy in addition to blood tests. Twenty-nine per cent of the respondents who had a SeHCAT scan had severe BAD with a retention score of 5% or less (figure 1).
Figure 1.
Severity of bile acid diarrhoea according to SeHCAT 7-day retention values.
Symptoms
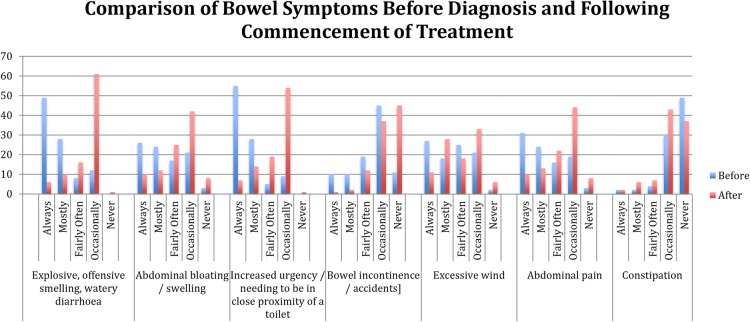
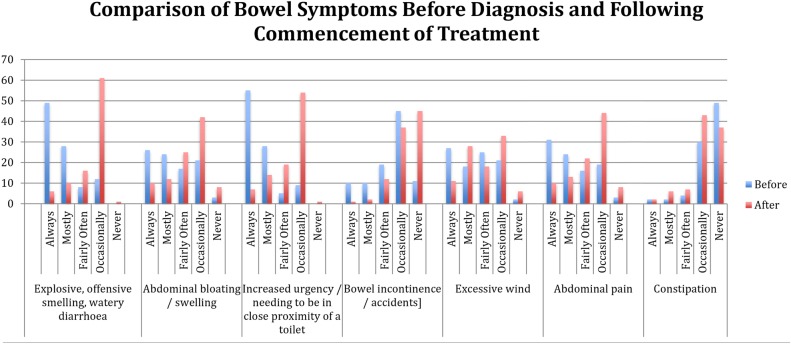
Forty-four per cent of respondents had experienced symptoms for more than 5 years before diagnosis, with the range being between 1 and 30 years. The frequency of individual symptoms and the change after treatment is shown in figure 2. These symptoms included explosive, offensive, smelly or watery diarrhoea (recorded as ‘always’ or ‘mostly’) in 80%, urgency in 85%, abdominal swelling/bloating in 54%, pain in 59%, at least occasional incontinence in 88% and also wind and tiredness. Around 60% of participants experienced a reduction in diarrhoea following treatment, so that only 17% still experienced this as ‘always’ or ‘mostly’ (p<0.001 Fisher's exact test) and a similar reduction was found for urgency (p<0.001). Just over 40% occasionally experienced constipation since being diagnosed and treated.
Figure 2.
Comparison of bowel symptoms before and after treatment.
Fifty-two per cent of respondents felt they needed to be in close proximity to a toilet due to an increased urgency; following treatment, 51% of respondents report that they only experience this symptom occasionally.
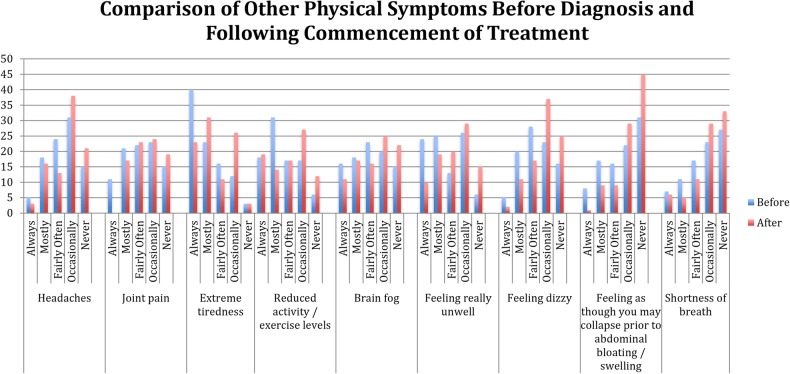
Nearly 40% reported that they always experienced extreme tiredness before diagnosis which has dropped to quarter of the respondents following treatment. Headaches, dizziness and ‘feeling as though you may collapse’ were symptoms that improved after diagnosis (figure 3). Thirty-five per cent of respondents reported that they still have nausea which has slightly increased before initiation of the treatment for BAD.
Figure 3.
Comparison of other physical symptoms before and after treatment.
Treatment
Ninety-four per cent have been prescribed medication to control their symptoms. Of these, 22% have had to pay for a private prescription and 13 people in the UK (13%) have had to pay privately for a prescription for bile binding medication.
Just under a quarter of respondents reported that they are taking different types of bile binding medication. The majority of respondents were taking colestyramine as treatment. Fifty per cent of respondents were taking the more expensive tablet version of bile binder colesevelam. Sixty-one per cent of respondents received a prescription from a gastroenterologist and nearly one-quarter received prescriptions from a combination of consultants, GP's and other healthcare practitioners. Exactly half of the cohort have been prescribed loperamide by health professionals and 46% have received prescriptions for medicines other than bile binders and loperamide. The most common of these are combinations of drugs, including amitriptyline, vitamin supplements, codeine-based painkillers of differing strengths and proton pump inhibitors, for example, omeprazole. About 36.5% of respondents are also using over-the-counter drugs to complement the prescriptions from health professionals. These include vitamin supplements, psyllium husk and indigestion medications.
Mental health and well-being
Issues relating to well-being and mental health were very common and included embarrassment (reported as ‘often’ or ‘sometimes’ in >90%), nervousness leaving home (>90%), depression, isolation, helplessness and low self-esteem (all >80%). Most respondents to the survey reported that their mental health has been positively impacted by the use of bile binding medication. In almost all areas, there was an improvement, but most significant improvement was seen in areas of embarrassment, low self-esteem and feeling nervous leaving home.
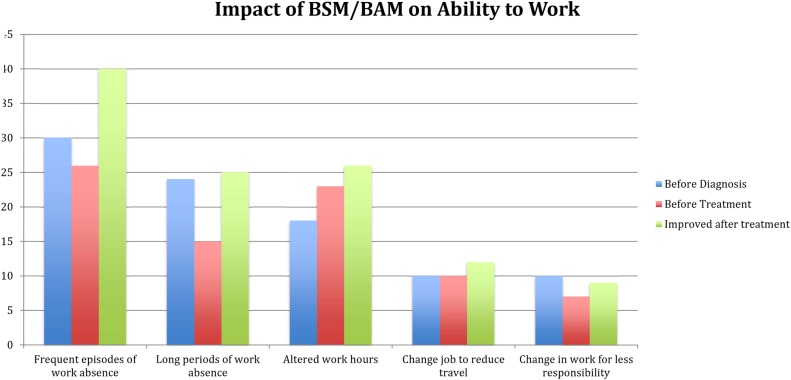
Almost all respondents have had a positive impact on their employment since beginning treatment. The survey shows that most people feel well supported by their immediate family; however, 44% of respondents feel the support they receive at work is not adequate. Although treatment seems to improve patients' ability to work, it seems that there is still not enough support in the workplace (figure 4).
Figure 4.
Impact of bile acid diarrhoea on ability to work.
Of those people who feel unsupported by their friends, family and work colleagues, 37% feel as though they were unable to discuss their medical issues with the people closest to them, 42% feel as though others would not believe them if they share details about their condition and just over a quarter feel as though they are a burden to others. Other reasons given for not feeling supported include others being ‘rude or insensitive’, not understanding the severity of the condition or being told ‘it's just IBS’.
Dietary changes
Just over one-third of the respondents are following multiple exclusion diets to control the symptoms of BAD. Seventy-eight per cent of respondents specifically avoid certain foods in their diet. The most commonly avoided food is dairy, which includes milk and cheese. High-fat foods are the second most frequent trigger food reported by respondents in this group. Other diets excluded by the respondents were sugar-free diet, low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) and low-fibre/low-residue diets. Vegetables and onion/garlic are also a large trigger group of foods for BAD sufferers. One-third of respondents follow a specific diet to try and control the symptoms. Table 1 shows the most popular exclusion diets selected by respondents. Despite following a low-fat diet, 75% of respondents report that they are more likely to gain weight with this condition and they are more likely to gain 5–10 kg with this condition. However, some respondents have reported significant weight loss since their symptoms began (figure 5).
Table 1.
Types of diet consumed by responders
| Low fat | Gluten-free | Low carb | Lactose-free | Wheat-free | Multiple exclusion |
|---|---|---|---|---|---|
| 43.8% | 14.3% | 6.7% | 11.4% | 14.3% | 34.3% |
Figure 5.
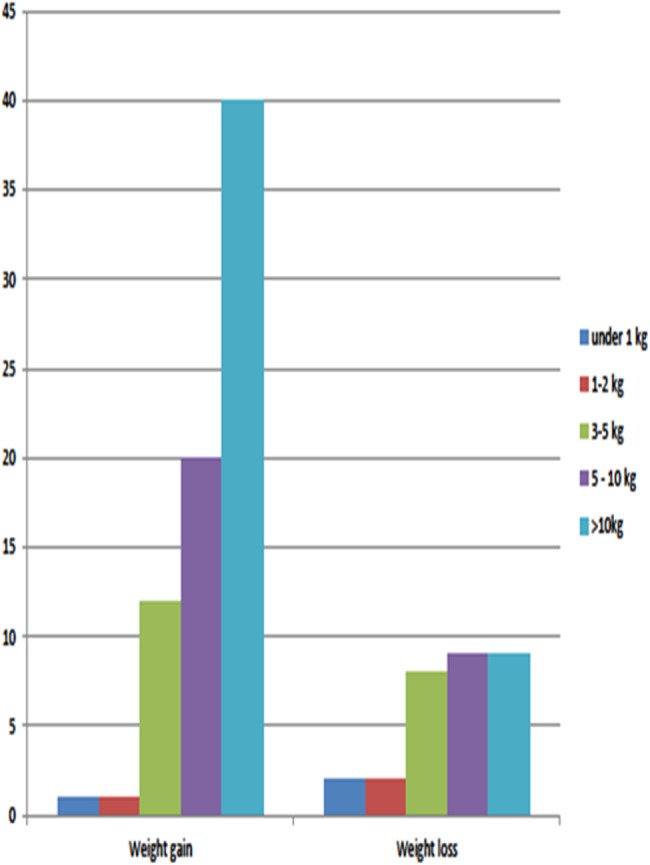
Number of respondents reporting weight loss and weight gain.
Contact with health professionals
Ninety-two per cent of respondents reported that they consulted a medical professional before diagnosis with BAD. Of these, 19% saw only their GP and 43% saw their GP and a gastroenterologist. Almost three-quarters saw multiple healthcare professionals before diagnosis with the condition, including GPs, gastroenterologists, dietitians or surgeons. Three-quarters of respondents report that they are currently under the care of a medical professional, leaving 26% of respondents not receiving medical support. Thirty per cent report being under the care of more than one health professional and just over half are under the care of their GP.
Of the respondents that were unsatisfied with medical care they received, 35% felt like they were not taken seriously by the medical professionals consulted. Just over half of the cohort felt as though their symptoms were dismissed and 28% encountered GPs who were unaware of the condition. Thirty-nine per cent were told by medical professionals that nothing could be performed about the symptoms they were experiencing. Eighteen respondents reported that their GP refuses to prescribe the tablet form of bile binding medication after they have been diagnosed.
However, the most frequent reason given for patients feeling very disappointed with their medical care following diagnosis is that the medical staff do not seem to have an understanding of BAD. Thirty-nine respondents felt that the medical professional they have seen for their condition did not understand BAD and 23 respondents felt that there was a lack of coordination between different medical professionals that they have been seeing.
Two-thirds of the patients had received a diagnosis of IBS from medical professionals before being diagnosed with BAD. Thirty-one per cent reported between 1 and 10 interactions with medical staff before receiving a diagnosis, while 38% of patients reported 20 or more interactions with medical professionals before receiving a diagnosis of BAD.
Discussion
This survey conducted by patient groups provides insights into how patients perceive their symptoms and outcomes in BAD. These include a long history of bowel and mental health symptoms. Patients reported that their quality of life and productivity were negatively affected and they experienced lack of support at their work place. Many avoided certain types of food in an attempt to help control their symptoms. Treatment with BAS offered significant reduction in physical and mental symptoms.
Patients also reported their experiences with health professionals which was less favourable due to the lack of awareness among clinicians. Patients can wait between 6 and 30 years before being diagnosed with BAD. Many patients were subjected to many tests before having a SeHCAT scan. Many patients received a diagnosis of IBS and due to the limitations of the questionnaire, it was unclear if health professionals validated their symptoms using the Rome criteria.10
This survey is limited because questionnaire respondents may read the questions differently and enter answers based on their own differing interpretations. Furthermore, the respondents were a select group of motivated patients who had signed up online for the Bile Salt Malabsorption group and/or were members of BAM Support UK. Whether the demographics and the clinical condition of these participants is typical of the broader group of people diagnosed with BAD is uncertain, but it does in many ways seem to be similar to those recently reported in a nationwide survey of SeHCAT use.8
Despite these limitations, the information gained will help increase awareness of this condition to the public and health professionals about BAD. This is the first such report in BAD; patient feelings of delay in diagnosis, poor quality of life, lack of understanding and difficulty at work seem to be at least as severe as those found in other chronic bowel conditions such as inflammatory bowel disease or coeliac disease.
We conclude that BAD needs more recognition by clinicians to reduce the time for diagnosis from around 5 years. More research is needed to estimate the personal and health economic impact of the condition. Bile acid sequestrant drugs improve physical and mental symptoms in the majority of patients, but research is needed to identify other therapeutic approaches and if possible find ways to prevent the development of this disorder.
Footnotes
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Walters JR. Bile acid diarrhoea and FGF19: new views on diagnosis, pathogenesis and therapy. Nat Rev Gastroenterol Hepatol 2014;11:426–34. doi:10.1038/nrgastro.2014.32 [DOI] [PubMed] [Google Scholar]
- 2.Sadik R, Abrahamsson H, Ung K-A, et al. Accelerated regional bowel transit and overweight shown in idiopathic bile acid malabsorption. Am J Gastroenterol 2004;99:711–18. [DOI] [PubMed] [Google Scholar]
- 3.Thaysen E, Pedersen L. Idiopathic bile acid catharsis. Gut 1976;17:965–70. doi:10.1136/gut.17.12.965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fromm H, Malavolti M. Bile acid induced diarrhoea. Clin Gastroenterol 1986;15:567–82. [PubMed] [Google Scholar]
- 5.Wedlake L, A'Hern R, Russell D, et al. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther 2009;30:707–17. doi:10.1111/j.1365-2036.2009.04081.x [DOI] [PubMed] [Google Scholar]
- 6.Arasaradnam R, Cullis J, Nwokolo C, et al. Bile acid malabsorption and SeHCAT: the ‘Cinderella’ will be going to the Nuclear Medicine Ball! Nucl Med Commun 2012;33:449–51. doi:10.1097/MNM.0b013e328351d516 [DOI] [PubMed] [Google Scholar]
- 7.Pattni S, Walters J. Recent advances in the understanding of bile acid malabsorption. Br Med Bul 2009;92:79–93. doi:10.1093/bmb/ldp032 [DOI] [PubMed] [Google Scholar]
- 8.Woolson K, Sherfi H, Sulkin T, et al. SeHCAT: nice or not nice? Gut 2014;63:A258–9. [Google Scholar]
- 9.Summers A, Peacock J, Coker B, et al. Multicentre prospective survey of SeHCAT provision and practice in the UK. BMJ Open Gastro 2016;3:e000091 doi:10.1136/bmjgast-2016-000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006;130:1377–90. doi:10.1053/j.gastro.2006.03.008 [DOI] [PubMed] [Google Scholar]