Abstract
Objectives
Professional burnout is closely related to work stress but less frequently associated with disturbed sleep. This study determines whether job strain and sleep disturbances are associated risk factors of burnout among financial workers.
Design
Observational study.
Participants
1300 employees (725 female) of a financial company.
Primary measures
Self-reported questionnaires (Maslach Burnout Inventory, Job Content Questionnaire, Sleep questionnaire based on ICSD-3 classification), the Epworth sleepiness scale and the Hospital Anxiety and Depression Scale (HADS).
Result
The prevalence of burnout was 10.2% (9.0% moderate and 1.2% severe). 23.3% of workers were considered with high job strain, and 93.1% had a high level of job satisfaction. 16.8% of individuals had insomnia and 97% reported non-restorative sleep. The bivariate analyses demonstrate a higher risk of burnout in participants with insomnia (OR=14.7, 95% CI 9.8 to 21.9), non-restorative sleep (OR=9.9, 95% CI 5.1 to 19.5) and anxiety (OR=10.2, 95% CI 6.8 to 15.3). High job strain was associated with burnout (OR=1.9, 95% CI 1.1 to 3.6). This association was not maintained after adjustment for sleep parameters. Job satisfaction was another independent risk factor for burnout (OR=124, 95% CI 65 to 237).
Conclusions
In our sample of financial workers, job strain represents a burnout risk factor only if associated with insomnia. Insomnia can be considered as a relevant clinical marker that should be targeted in mental health prevention programmes at the workplace.
Keywords: PREVENTIVE MEDICINE, EPIDEMIOLOGY, Insomnia, Job strain, Burnout, Sleep
Strengths and limitations of this study.
Insomnia is strongly associated with burnout (OR=14.7, 95% CI 9.8 to 21.9).
For the first time, we showed that job strain represents a risk factor only if coupled with insomnia.
Insomnia is a relevant clinical marker for burnout and should be targeted in health prevention programmes. Sleep monitoring can improve clinical detection and strengthen the medical survey of burnout, especially in high job strain workers.
The timing of the snapshot is not guaranteed to be representative, as far as there are seasonal variations in professional activity all along the year.
Sleep data were based on self-reports, and might be confirmed using polysomnography.
Introduction
It is well admitted that the word ‘professional burnout’ refers to a psychological syndrome arising in response to chronic emotional and interpersonal stressors on the job. It has been defined by its impact on three dimensions: emotional exhaustion (EE), depersonalisation (DP) and reduced personal accomplishment (PA) (feelings of inefficacy).1 EE refers to the feeling of being overextended and depleted of one's emotional resources. DP is characterised by a negative, cynical and detached response to other people, including colleagues, patients or clients. A reduction in PA occurs when a person feels herself or himself less competent at work.1
Burnout at the workplace has been attributed to different factors, relative to organisational and individual factors. Regarding organisational factors workload, effort reward imbalance, work conflicts, diminished resources, job insecurity and continuing rapid organisational changes have been implicated.2 3 Burnout has been also described as failure to cope with occupational stress in occupations requiring intensive communication and interaction with service recipients.3 Moreover, high job strain for white-collar men (workers in ‘management, business and financial occupations’ and in ‘professional and related occupations’) has been recently evidenced to increase the risk of mortality.4
Originally, the burnout symptoms were only described in client-related occupations, but they actually resulted from all types of work.1 Most of the recent studies that estimate the prevalence of burnout focused on a specific occupational group, primarily for service-related professions such as teachers, correctional officers, hotel employees, residents or nurses.2 5–7 In addition, professional burnout appears to be highly prevalent among medical students and practising physicians with rates ranging from 25% to 60%.8 9 These professions are people oriented (interactions with students, patients, families, etc) and frequently exposed to night shifts. Embriaco et al9 have identified three factors related to night work in the occurrence of burnout: the number of night shifts per month, a longer period of time from the last non-working week, and the presence of one night shift before the day of the survey.
Increasing evidence, based on both questionnaire data and objective polysomnographic recordings, has underlined an association between the occurrence of a burnout syndrome and the presence of past sleep disorders, which may contribute to increased fatigue and impaired restoration.10 11 Previous studies have suggested that individuals with high burnout levels exhibit poorer sleep quality. Especially women scoring high on burnout report greater sleepiness, impaired sleep quality and more frequent awakenings than those scoring low.12 In addition, a persistent association between burnout and insomnia has been established.13 Findings of self-report studies on sleep are highly correlated with objective measures, such as polysomnography (PSG). A study using polysomnographic sleep measures in young individuals with high scores of burnout found more arousals and sleep fragmentation, more wake time and stage-1 sleep, lower sleep efficiency, less slow wave sleep and rapid eye movement sleep, and a lower δ power density in non-rapid eye movement sleep in participants with burnout.11
In France, several studies had already focused on professional burnout specifically in caregivers. Embriaco et al9 found a high prevalence of burnout of 46.5% among intensivists, the burnout being related to organisational factors. Among French general practice trainees, it was found a percentage of trainees with high levels of EE at 16.0%, 33.8% had a high score for DP and 38.9% had a high score for low personal accomplishment, and a prevalence of severe burnout of 6.5%.14 Few French studies concerned other types of working populations such as teachers, but Vercambre et al15 showed that burnout is highly prevalent among teachers and broadly related to contextual covariates, and the same findings are highlighted in managers.
The aim of the present study is first to determine the prevalence of burnout in a specific group of financial workers, namely high level executive white-collar workers. The second objective was to examine whether job strain and sleep disturbances are potential risk factors (predictors) and/or outcomes of burnout.
Methods
Study design and population
A cross-sectional study of employees from a large financial company in France was conducted between September 2012 and September 2014 using both a paper-based self-administered questionnaire and a complete medical examination. During the study period, all employees were invited to participate in this study during their occupational medicine annual visit. A self-administered questionnaire, which included scales on job stressors, demographic characteristics, lifestyle, sleep disturbance and burnout, was delivered to employees before the medical visit. Employees who were suffering from clinical depression were excluded from the study.
All voluntary participants working with the company with a regular contract for at least more than 1 year were invited to have a preventive medical visit, during which they were required to confidentially participate in the survey. Information notice and informed consent were mandatory. The procedures were in accordance with the Declaration of Helsinki and the study was approved by the Ethical Committee of the Hôtel Dieu Hospital, Paris, France.
Questionnaires and clinical interviews
Demographic characteristics included sex, age, marital status, body mass index (BMI), physical activity, smoking and alcohol habits, and job rank. These were assessed using a self-report questionnaire. Age was classified into four groups: 50–64 years, 40–49 years, 30–39 years and 20–29 years. Marital status was classified into three groups: currently married, never married and divorced or widowed. Occupation rank was classified into three groups in regard to the management position: high (leading and directing project), intermediate (work under minimum supervision with limited responsibilities) and low (work under immediate supervision and assigned tasks). The job satisfaction was measured by visual analogue scale (VAS) in the range 0–10.
Burnout
The primary outcome was the burnout syndrome. To assess it, we used the Maslach Burnout Inventory (MBI). The MBI is a questionnaire consisting of 22 items, distributed in three dimensions.16 The score of the participant is calculated by the sum of the points of the items related to each of the dimensions. The validated 22-item Maslach Burnout Inventory—Human Services Survey was used to assess burnout in three subscales: nine items for EE (a drained, depleted feeling arising because of excessive psychological and emotional demands), five items for DP (tendency to view others in an excessively detached, impersonal manner) and eight items for PA (a sense of competence and accomplishment). According to the scoring guidelines by MindGarden (Menlo Park, California), USA), the overall score was categorised into low, moderate and high levels of burnout.
Burnout was considered as:
Low level if EE score was <16, cynicism < 6 and professional efficacy >37.
Moderate level if EE was between 17 and 26, cynicism between 7 and 12, and professional efficacy between 31 and 36.
High level if EE was >27, cynicism >13 and professional efficacy <30.
It was widely demonstrated in a physician population that high levels of EE and DP correlate with burnout, whereas personal achievement is inversely proportional to burnout.17
In our study, we defined as having burnout, respondents with high levels in at least two dimensions (either EE and/or DP, associated or not with a low personal achievement).
In the given study, in order to analyse the internal consistency of the three domains of the MBI (emotional distress, DP and low professional fulfilment), the α Cronbach coefficient was respectively 0.86 for EE, 0.71 for DP and 0.70 for PA.
In order to confirm the burnout syndrome and to exclude clinical depression, alexithymia and other medical conditions that could overlap with burnout, clinical interviews were conducted by the occupational physician during the required medical examination. It is the physician’s discretion to assess a burnout diagnosis because no valid differential diagnostic instrument is available to assign burnout.
Job strain
Job strain level was calculated from job control and job demand scores from the validated French version of the Karasek job content questionnaire.18 Participants were asked to answer questions about the psychosocial aspects of their job. The response categories were a Likert-scale ranging from 1 (strongly disagree) to 4 (strongly agree) and were reverse-coded afterwards if necessary. For each participant, mean response scores were calculated for job demand items (ie, questions about whether the participant had to work very hard, had excessive amounts of work, conflicting demands or insufficient time) and job control items (ie, questions about decision freedom and learning new things at work). Scores on the job demands scale range from 12 to 48, with higher scores (>24) representing high demand. Scores on the job control scale range from 24 to 96, with higher scores representing high control (>72). A low strain job was defined as a job with high control and low demand, a high strain job as a job with low control and high demand, an active job as one with high control and high demand and a passive job as one with low control and low demand. Social support was defined as high if the score was higher than 23. In our study, the following Cronbach's α coefficients were: job demand (0.78), job control (0.76).
Sleep disturbances
Insomnia and other sleep disorders were assessed using a self-administered questionnaire, derived from the ‘Sleep Disorders Questionnaire—French version’ (SDQFV). The SDQFV is a 42-item questionnaire based on the ‘Stanford Sleep Questionnaire and Assessment of Wakefulness’. The French version has been validated in epidemiological studies.19 20 In our study, we used part of the questionnaire that focused on sleep habits and insomnia. To assess insomnia symptoms, we add questions based on reference documents, particularly the ‘International Classification of Sleep Disorders’ (ICSD-3).21 22
Clinical reappraisal was carried out with all participants by an occupational health and sleep medicine specialist. The clinical interviews were carried out by a structured clinical interview to establish a diagnosis of insomnia with Diagnostic and Statistical Manual Fifth Edition (DSM-5). The DSM-5 criteria for insomnia include difficulty of initiating sleep, difficulty of maintaining sleep and early morning awakening, for a period of ≥1 month. In addition, it is a pre-requisite that sleep disturbance significantly impairs daily function.
Severity of insomnia was divided into two groups: moderate insomnia (one trouble) and severe insomnia (at least two troubles).
Non-restorative sleep disorder was assessed separately using the question ‘How frequently are you bothered because your sleep is not refreshing, you don't feel rested even if the duration of your sleep is normal’. Non-restorative sleep was considered present when it was reported to occur 3 to 4 times a week or more and lasted for at least 1 month.
Excessive sleepiness was assessed using the ‘Epworth sleepiness scale’ (ESS).23 On the basis of the total score, patients were classified into two subgroups of sleepiness: no sleepiness=0–10, excessive sleepiness >10.
Mental health (depression and anxiety)
Symptom levels of depression and anxiety were assessed by the Hospital Anxiety and Depression Scale (HADS) consisting of seven items for each dimension.24 Answers are coded on a four-point Likert scale (0=not at all, 3=mostly), giving rise to a total depression and anxiety score ranging between 0 and 21 points. A >10 score is considered as certainly symptomatic.
Statistical analysis
Statistical tests were performed using R studio (V.0.99.175 2009–2014 RStudio, .) and significance (α risk) was fixed at p<0.05. Continuous variables are presented as mean±SD (m±SD) and means were compared (Burnout vs Control) using a t-test. Quantitative variables are presented as occurrence and percentage (n (%)). A χ² test was used to test the relationship between dichotomous variables and a multivariate analysis used for non-dichotomous variables. When significant, the crude OR and its 95% CI (OR (95% CI)) were calculated. Two models were used for adjusted ORs: model 1, in which OR was adjusted for sociodemographic parameters (age, weight, sex, BMI, physical activity and smoking and alcohol habits), and model 2, in which OR was adjusted for sociodemographic, , professional (management position) and sleep parameters (habitual sleep time, weekend sleep time, ESS). Dependence between quantitative variables was checked using a Pearson correlation test (r ≥ 0.6 and p<0.05).
Results
Subjects
About 1502 employees completed the questionnaire. We excluded 46 employees who did not sign the informed consent, 45 who had at least one missing response on the questionnaires, 102 who did not met the inclusion criteria, and nine participants with clinical depression. Finally, a total of 1300 questionnaires (575 men and 725 women) were analysed (86.7%). The participants not included (n=156) did not significantly differ regarding age and demographic characteristics.
Burnout prevalence
The total prevalence of burnout in the study group was 10.2%, 9% (for moderate) and 1.2% (for severe) burnout. The averages were respectively for EE: 24.3±9.4, DP 10.1±5.1, and 39.1±6.4 for PA. Seventy-eight per cent (78.3%) of the participants had a moderate to high score of EE. A high score of DP was seen for 20.1% and a low score for 27.8% of them. About 70.2% had a low score of PA.
Sociodemographic data and lifestyle habits
The participants were divided into 55.7% (725) female and 44.3% (575) male aged 29.1 (±3.2) years (table 1). Most of the participants (78%) were single, 28% were married or living with a partner people, and about 1% were divorced. About 36.4% of them had children. The mean BMI was 22.2±3.2 kg/m², 26 (2%) were obese and 196 (15, 1%) were overweight. About 24.8% of the participants are current smokers and 75.2% have never been smokers. Most of the participants (74.1%) have a physical activity (from ‘every month’ 24.8%, to ‘every day’ 35.9%), while a third of them never practise a physical activity. More than half of the participants in the study drink alcohol at least once a week.
Table 1.
Impact of sociodemographic parameters on burnout
| Burnout |
Crude | |||
|---|---|---|---|---|
| Total | N | Per cent | OR (95% CI) | |
| Sex | ||||
| Male | 725 | 40 | 7.0 | Ref. |
| Female | 575 | 92 | 12.7 | 1.9 (1.3 to 2.9)* |
| Age (years) | ||||
| <24 | 99 | 6 | 6.1 | Ref. |
| 24–29 | 745 | 101 | 13.6 | 2.4 (1.0 to 5.8)* |
| 30–35 | 232 | 6 | 2.6 | 0.4 (0.1 to 1.3) |
| 36–41 | 90 | 14 | 15.6 | 3.5 (1.0 to 7.8)* |
| 42–47 | 80 | 5 | 6.3 | 1.2 (0.7 to 8.5) |
| >48 | 54 | 0 | 0.0 | |
| Marital status | ||||
| Currently married | 345 | 323 | 87.4 | Ref. |
| Single | 872 | 762 | 93.6 | 2.1 (1.3 to 3.4)** |
| Divorced/widowed | 7 | 7 | 100 | |
| Body mass index (BMI/kg/m2) | ||||
| Normal (<25) | 1078 | 114 | 10.6 | Ref. |
| Overweight (25–30) | 196 | 18 | 9.2 | 0.8 (0.5 to 1.4) |
| Obese (>30) | 26 | 0 | 0.0 | |
| Physical activity | ||||
| Every day | 384 | 18 | 4.7 | Ref. |
| Every week | 110 | 31 | 9.3 | 1.2 (0.7 to 1.7) |
| Every month | 265 | 40 | 15.1 | 4.0 (1.7 to 5.3)** |
| Never | 318 | 43 | 13.5 | 3.2 (1.9 to 5.3)** |
| Smoking habit | ||||
| No | 977 | 98 | 10.0 | Ref. |
| Yes | 323 | 34 | 10.5 | 1.1 (0.6 to 1.5) |
| Alcohol | ||||
| Never | 243 | 25 | 10.3 | Ref. |
| Seldom | 911 | 101 | 11.1 | 1.0 (0.7 to 1.7) |
| Regular | 145 | 6 | 4.1 | 0.4 (0.2 to 1.2) |
N, occurrence; OR, OR; Ref., reference; 95% CI, 95% CI.
*p<0.05, **p<0.01.
The following factors were significantly associated with burnout: sex, age, marital status and physical activity.
Sleep and mental health
The mean sleep duration reported during the past month was 7.12±0.84 hours (table 2). In the past week, the mean sleep duration is 7.02±0.79 hours, and during the weekend it increases at 8.62±1.84 hours. Seventy-six per cent of individuals sleep more than 6 to 8 hours per night during the week. About 2.3% are short sleepers and sleep <6 hours per night, and 1.2% of them are long sleepers having sleep of more than 9 hours per night. Seventeen per cent of individuals were insomniacs, 52% with severe insomnia and 97% presented with non-restorative sleep. The mean ESS was 10.3±3.5 in burnout participants versus 7.8 (p<0.01) in non-burnout participants. HAS anxiety was 8.9±3.4 in burnout versus 6.2±2.8 (p<0.01) and depression 4.4±2.7 vs 3.2±2.8 (p<0.001).
Table 2.
Impact of sleep disorders and mental health on burnout
| Burnout |
Crude | Model 1 | |||
|---|---|---|---|---|---|
| Total | N | Per cent | OR (95% CI) | OR (95% CI) | |
| Insomnia DSM-5 | |||||
| No | 1081 | 44 | 4.1 | Ref. | Ref. |
| Yes | 219 | 88 | 40.2 | 14.7 (9.8 to 21.9)** | 13.6 (9.2 to 21.1)** |
| Severity of insomnia | |||||
| Moderate | 106 | 49 | 30.5 | Ref. | Ref. |
| Severe | 113 | 39 | 55.6 | 1.6 (0.4 to 2.1) | 1.9 (0.3 to 1.0) |
| Type of insomnia | |||||
| Difficulties of initiating sleep | |||||
| No | 1205 | 104 | 8.7 | Ref. | Ref. |
| Yes | 95 | 25 | 26.3 | 3.7 (2.2 to 6.1)* | 3.5 (2.0 to 5.9)* |
| Difficulties of maintaining sleep | |||||
| No | 1130 | 72 | 6.4 | Ref. | Ref. |
| Yes | 170 | 58 | 34.1 | 7.5 (5.1 to 11.8)** | 7.1 (5.0 to 11.5)** |
| Early morning awakening | |||||
| No | 1222 | 91 | 7.5 | Ref. | Ref. |
| Yes | 78 | 41 | 52.6 | 13.7 (8.4 to 22.5)** | 11.3 (6.4 to 18.5)** |
| Non-restorative sleep | |||||
| No | 1262 | 109 | 8.6 | Ref. | Ref. |
| Yes | 37 | 18 | 48.6 | 9.9 (5.1 to 19.5)** | 9.4 (4.8 to 17.5)** |
| Epworth sleepiness scale (ESS) | |||||
| ≤10 | 790 | 31 | 3.9 | Ref. | Ref. |
| >10 | 510 | 101 | 19.8 | 6.0 (4.0 to 9.2)* | 5.4 (4.2 to 8.3)* |
| Habitual sleep time (hour) | |||||
| <6 | 30 | 5 | 16.7 | 2.0 (0.8 to 5.5) | 2.3 (1.7 to 6.5)* |
| 6–7 | 270 | 34 | 12.6 | 1.5 (0.9 to 2.3) | 1.0 (0.2 to 1.2) |
| 7–8 | 730 | 65 | 8.9 | Ref. | Ref. |
| 8–9 | 243 | 22 | 9.1 | 1.1 (0.6 to 1.7) | 0.9 (0.5 to 1.2) |
| ≥9 | 16 | 5 | 31.3 | 4.6 (1.4 to 14.3)* | 4.1 (1.2 to 14.1)* |
| Difference between week and weekend sleep time (hour) | |||||
| <0 | 30 | 1 | 3.3 | ||
| 0–1 | 210 | 10 | 4.8 | Ref. | Ref. |
| 1–2 | 503 | 57 | 11.3 | 2.6 (1.3 to 5.1)* | 2.7 (1.4 to 5.2)* |
| 2–3 | 349 | 33 | 9.5 | 1.9 (1.0 to 4.3)* | 2.1 (1.2 to 4.6)* |
| 3–4 | 120 | 17 | 14.2 | 1.6 (1.5 to 7.5)* | 1.8 (1.7 to 8.0)* |
| Mental health | |||||
| Anxiety-HADS | |||||
| ≤10 | 1145 | 70 | 6.1 | Ref. | Ref. |
| >10 | 155 | 62 | 40.0 | 10.2 (6.8 to 15.3)* | 9.8 (5.8 to 14.4)* |
| HADS-D | |||||
| ≤10 | 1244 | 124 | 10.2 | Ref. | Ref. |
| >10 | 56 | 8 | 14.3 | 1.5 (0.6 to 2.1) | 1.3 (0.5 to 2.0) |
Model 1, OR adjusted for sociodemographic parameters (age, weight, sex, BMI, physical activity, smoking and alcohol habits).
*p<0.05, **: p<0.01.
CI 95%, 95% CI; N, occurrence; DSM, Diagnostic and Statistical Manual; HADS-D, Hospital Anxiety and Depression Scale-Depression; HADS-A, Hospital Anxiety and Depression Scale-Anxiety; OR, OR; Ref., reference.
After adjusting (model 1) for demographic parameters (age, gender, marital status, BMI, physical activity, smoking habit and alcohol), the following findings were associated with burnout: insomnia (presence and all types), non-restorative sleep, sleepiness, sleeping time lower than 6 hours and higher than 9 hours per night, sleep debt (sleep duration difference between weekend and week) and anxiety.
Professional parameters
In relation to work characteristics, most of the participants (71.3%) had no management position, the managers represented 6% of the study group and 21% had an intermediate professional rank (table 3). High job strain concerns 23.3% of the study group, low job strain 18.4% and 58.2% are passive or active job. Regarding the job strain level, the job demand and job control average levels were 31.6±24.7 and 75.3±26.7, respectively.
Table 3.
Impact of professional parameters on burnout
| Burnout | Crude | Model 1 | Model 2 | |||
|---|---|---|---|---|---|---|
| Total | N | Per cent | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Management position | ||||||
| Low | 927 | 91 | 9.8 | Ref. | Ref. | Ref. |
| Intermediate | 278 | 39 | 13.5 | 2.8 (1.0 to 2.1)* | 2.2 (0.8 to 1.8) | 2.2 (0.8 to 1.8) |
| High | 81 | 2 | 2.5 | |||
| Job strain | ||||||
| Low strain | 240 | 16 | 6.6 | Ref. | Ref. | Ref. |
| High strain | 303 | 37 | 13.9 | 1.9 (1.1 to 3.6)* | 1.8 (1.1 to 3.1)* | 1.1 (0.6 to 2.1) |
| Active job | 277 | 30 | 10.8 | 1.7 (0.9 to 3.2) | 1.2 (0.7 to 1.9) | 1.1 (0.5 to 1.1) |
| Passive Job | 480 | 48 | 10.0 | 1.6 (0.8 to 2.8) | 1.1 (0.5 to 2.1) | 1.1 (0.4 to 2.1) |
| Social support | ||||||
| High (score >23) | 940 | 79 | 8.4 | Ref. | Ref. | Ref. |
| Low (score <23) | 360 | 53 | 14.7 | 2.8 (1.9 to 4.1)* | 1.2 (0.9 to 2.1) | 1.1 (0.8 to 2.0) |
| Job satisfaction | ||||||
| High (score ≥5) | 1210 | 55 | 4.5 | Ref. | Ref. | Ref. |
| Low (score <5) | 90 | 77 | 85.6 | 124 (65 to 237)** | 108 (48 to 215)** | 108 (48 to 215)** |
Model 1, OR adjusted for sociodemographic parameters (age, weight, sex, BMI, physical activity, smoking and alcohol habits). Model 2, OR adjusted for sociodemographic, professional (management position) and sleep parameters (habitual sleep time, weekend sleep time, ESS).
*p<0.05, **p<0.01, **p<0.001.
N, occurrence; OR, odds ratio; Ref., reference.
BMI, body mass index; ESS, Epworth sleepiness scale.
Most of the participants (77.2%) have a high level of social support. The mean EVA score for job satisfaction is 7.2/10 with an SD of 1.24. Most of the participants have high job satisfaction and <7% have low job satisfaction (score under 5/10).
After adjusting for demographic (model 1) plus sleep parameters (model 2), burnout was associated with job satisfaction only. In particular, the association between job strain and burnout (OR=1.9, 95% CI 1.1 to 3.6) did not persist after adjustment for demographic parameters and sleep parameters. Moreover, the association between social support and burnout disappeared after adjustment for demographic (model 1) or sleep parameters (model 2).
Relationship between burnout and job strain with insomnia, daytime sleepiness and mental health parameters
Table 4 described the impact of insomnia (presence or not), excessive sleepiness (>10), anxiety and depression on the association between strain (high strain, active job and passive job, with low strain serving as reference) and burnout. It shows that the association between burnout and high strain existed only in burnout participants reporting insomnia (OR=3.9, 95% CI 1.2 to 8.5). Taking into account sleepiness, anxiety or depression does not change the relation between burnout and job strain, described previously (table 3).
Table 4.
Cross relationships between burnout and job strain with (A) insomnia, (B) Epworth sleepiness scale (ESS), (C) HADS-A (anxiety) and (D) HADS-D (depression).
| Sub total |
Burnout |
Sub total |
Burnout |
|||||
|---|---|---|---|---|---|---|---|---|
| Total | N | (%) | N | (%) | ||||
| A | Non-insomniac | Insomniac | ||||||
| Chi2=3.5 (NS) | Chi2=8.5 (p=0.03) | |||||||
| Low strain | 240 | 206 | 9 | 4.3 | 34 | 7 | 20.5 | Ref. |
| High strain | 303 | 251 | 10 | 3.9 | 52 | 27 | 51.1 | 3.9 (1.2 – 8.5)* |
| Active job | 277 | 218 | 11 | 5.0 | 59 | 19 | 32.2 | 1.4 (0.5 – 3.7) |
| Passive Job | 480 | 407 | 28 | 5.7 | 73 | 20 | 27.3 | 1.3 (0.6 – 3.6) |
| B | ESS≤10 | ESS>10 | ||||||
| Chi2=1.5 (NS) | Chi2=4.5 (NS) | |||||||
| Low strain | 240 | 158 | 6 | 3.7 | 82 | 10 | 12.1 | Ref. |
| High strain | 303 | 207 | 14 | 6.7 | 96 | 23 | 24.0 | 2.3 (1.0 – 5.1) |
| Active job | 277 | 181 | 13 | 7.1 | 96 | 17 | 17.7 | 1.5 (0.7 – 3.6) |
| Passive Job | 480 | 349 | 20 | 5.7 | 131 | 28 | 21.2 | 1.9 (0.9 – 4.2) |
| C | HADS-A≤10 | HADS-A>10 | ||||||
| Chi2=2.0 (NS) | Chi2=1.8 (NS) | |||||||
| Low strain | 240 | 215 | 9 | 4.2 | 25 | 7 | 28.0 | |
| High strain | 303 | 270 | 23 | 8.5 | 33 | 14 | 42.2 | |
| Active job | 277 | 227 | 11 | 4.8 | 50 | 19 | 38.0 | |
| Passive Job | 480 | 433 | 30 | 6.9 | 47 | 18 | 38.8 | |
| D | HADS-D≤10 | HADS-D>10 | ||||||
| Chi2=1.0 (NS) | Chi2=Low sample | |||||||
| Low strain | 240 | 232 | 8 | 9.1 | 8 | 0 | 0.0 | |
| High strain | 303 | 286 | 33 | 10.8 | 17 | 4 | 23.5 | |
| Active job | 277 | 260 | 25 | 10.0 | 17 | 5 | 29.0 | |
| Passive Job | 480 | 466 | 46 | 9.9 | 14 | 2 | 14.3 | |
Values are occurrence or odds ratio with 95% Confidence interval (OR 95% CI). Total is the number of subject for each job strain catégorie. Sub total is the number of subject for (A) no-insomniac and insomniac, (B) ESS ≤10 and ESS ≥10, (C) HAD-A ≤10 or >10, (D) HADS-D ≤10 and >10. *is p<0.05. ESS, Epworth sleepiness scale; HADS, Hospital anxiety (A) and depression (D) scale.
Correlation analysis between quantitative variables
Using the Pearson coefficient between quantitative variables, we show numerous significant correlations between job strain (job demand and job control), burnout (the three dimensions), the difference between weekend and week sleep time, sleepiness, anxiety and depression parameters (table 5). The highest strain of the relation (Pearson coefficient >0.4) was for anxiety and depression with emotional exhaustion.
Table 5.
Pearson coefficient between quantitative variables
| HST | Diff.ST | ESS | HADS-A | HADS-D | Job demand | Job control | EE | DP | PA | Social support |
|---|---|---|---|---|---|---|---|---|---|---|
| HST | 0.36** | −0.09 | −0.20** | −0.25** | 0.11* | 0.11* | −0.13* | −0.11* | 0.10* | −0.32** |
| Diff.ST | – | −0.01 | 0.15** | 0.09 | −0.08 | −0.12 | 0.13 | 0.08 | −0.14* | 0.17* |
| ESS | – | – | 0.32** | 0.35** | 0.22** | 0.01 | 0.38** | 0.21** | −0.03 | −0.21** |
| HADS-A | – | – | 0.50** | 0.16* | −0.06 | 0.52** | 0.30** | −0.09 | −0.04 | |
| HADS-D | – | – | – | 0.20** | −0.16** | 0.54** | 0.41** | −0.16** | −0.18* | |
| Job demand | – | – | – | – | 0.14* | 0.43** | 0.20** | 0.20** | −0.35** | |
| Job control | – | – | – | – | – | −0.19** | −0.12* | 0.35** | −0.02 | |
| EE | – | – | – | – | – | – | 0.49** | −0.09 | −0.24* | |
| DP | – | – | – | – | – | – | – | −0.09 | −0.09 | |
| PA | – | – | – | – | – | – | – | – | −0.11 |
Values are: Pearson coefficient. *p<0.01; **p<0.001. Bold values are Pearson coefficient >0.4.
HST, habitual sleep time; Diff.ST, Difference between week and weekend sleep time; ESS, Epworth sleepiness scale; HADS-A, (anxiety); HADS-D (depression); EE: emotional exhaustion; DP, depersonalisation; PA, personal accomplishment.
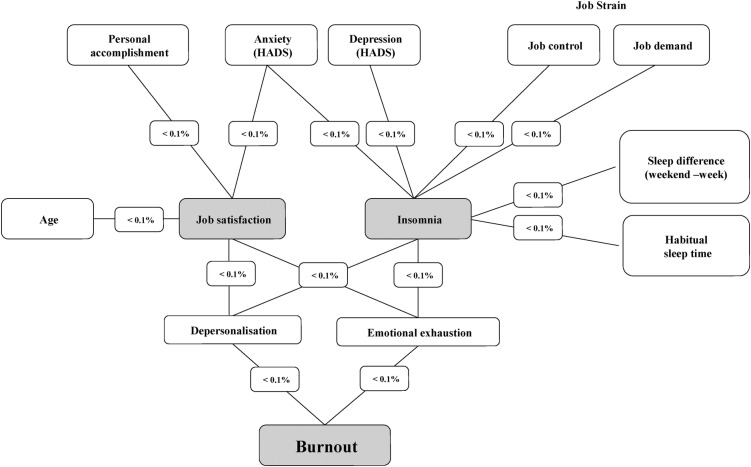
By analysing the paths between burnout, job strain and sleep parameters, a model with only p<0.001 significant path coefficients was produced (figure 1).
Figure 1.
Relationships model with significant coefficients (p<0.001) between job strain, sleep, job satisfaction, anxiety and burnout.
Discussion
Burnout is a stress phenomenon that shows the expected pattern of health correlates, such as headaches, gastrointestinal disorders, muscle tension, hypertension, cold/influenza episodes and sleep disturbances.3 Karasek's job demand–control–social support model predicts that workers with high-strain jobs, characterised by high demands in combination with little control and little social support in the workplace, are at high risk of disease.25 In addition, self-report studies suggest that individuals with high burnout levels exhibit poorer sleep quality,12 and persistent association between burnout and insomnia has been established.13 The main result of this study indicates that insomnia is strongly associated with EE and DP, the two burnout-related dimensions, while job strain represents a burnout risk factor only if coupled with insomnia. In other words, among this group of financial workers, insomnia can be considered as a relevant clinical marker for burnout.
Job strain and burnout
Among the study group, the prevalence of burnout is 10.2%, (9% moderate and 1.2% severe), with 78.3% of the participants having a moderate to high score of emotional exhaustion. The burnout participants were more exhausted and less efficient. Our results are similar to those previously described among medical students (10.2%),26 and lower than that reported on general practitioners (24.1%) or medical residents (14.4%).14 27
Our population is characterised by a high level of job strain (23.3%) concomitantly to high level of job satisfaction (93.3%). The proportion of job strain participants (23.3%) was higher than those observed in other studies.28 29 It was equivalent to those described in the first French national survey of a large population of 24 486 workers (around 20.0%),18 and in strictly rotating shift workers (23.3%).30 Our results are also close to those found among white-collar Finnish employees (17.5% of high job strain among men and 36.2% among women).4 In the Nyberg et al28 meta-analysis, 16.7% of job strain was evidenced on pooled data from eight studies comprising 47 000 men and women. In 2015, Agbenyikey et al29 have described 12.5% of high strain among 1429 participants from the Framingham Offspring cohort.
Regarding sociodemographic variables in our participants group, burnout was associated primarily with the female sex. This finding is confirmed by a previous study of intensivists presenting a high level of burnout,9 but differs from other studies that have associated the male sex with burnout in medical occupations.14 26 We also found association with age (ie, in the age range of 24–29 and 36–41years), marital status (higher when single) and physical activity level (higher when virtually sedentary).
So we found that high job strain was a predictive factor for burnout (OR=1.9, 95% CI 1.1 to 3.6), but this is no longer significant when the sleep parameters were examined. Low social support is a burnout predictive factor that is not present after adjustment with sociodemographic and sleep variables, while low job satisfaction is strongly predictive of burnout even after adjustment. These results can also be explained by the cut-off we used to define low job satisfaction (under 5 in a VAS from 0 to 10). However, financial workers usually have a high degree of professional requirement, so a low job satisfaction may indicate a negative affectivity which influences the relationship to stress and leads to low coping resources. Low score of job satisfaction can also be in correlation with DP symptoms which are mainly negative effects. These findings are relevant in regard to clinical assessments.
Sleep disorders and burnout
In our study, 16.8% of the participants were insomniac, which is higher than Armon et al13 study, who found 10% among 1356 healthy employees, and then Jansson-Fröjmark et al31 study who found 12.7% in a general population of employees individuals aged 20–60 years. In contrast, the prevalence of insomnia is higher in two recent studies—34.3% in nurses32 and a mean of 28.3% in civil servants.33 In white-collar employees, de Beer et al34 observed 17% ‘always’ or ‘often’ reporting sleep difficulties and 37% ‘sometimes’ reporting sleep difficulties. In addition, several sleep disorders were significantly different in participants with burnout (ie, presence of insomnia and the three types of troubles), non-restorative sleep, sleepiness, sleep duration (ie, higher than 9 hours) and sleep debt (ie, difference in night sleep duration between the week and the weekend from 1 hour to 4 hours). Insomnia symptoms, like trouble falling asleep, non-restorative sleep and early awakenings, have been reported in persons with high burnout scores in questionnaire studies.12 35 In the healthcare system, hospital physician burnout has been shown to be directly related to short sleeping time.36
We found that most of the sleep disorders remained risk factors of burnout even after adjustment with sociodemographic variables, and sleep duration lower than 6 hours per night became significant. Significant associations were also found between anxiety and burnout before and after sociodemographic adjustment. It was because higher levels of depressive and anxiety symptoms have consistently been associated with insomnia37 that we investigated the relationship between burnout and professional parameters after adjustment with sociodemographic and sleep parameters including anxiety. In a recent study of white-collar employees, de Beer et al34 observed that the treatment of depression decreases the risk of sleep disorders and burnout.
When we investigated the impact of job strain in burnout participants, we only found significant association with high strain in the persons suffering of insomnia In addition, burnout participants were not significantly different based on self-reported anxiety. Our results underlined that anxiety is an independent factor of burnout, as strengthened by the significant positive correlation found with EE and DP (r=0.52 and r=0.30, p<0.01 for the two).
In the results presented here on financial workers showing a high prevalence of job strain, sleep disturbances are closely related to burnout, which is in agreement with other cross-sectional studies.12 More recently, Portela et al32 showed that the inclusion of low social support combined with high demands and low job control led to increased odds for insomnia symptoms in a population of nurses. Prospective studies also enlightened a relationship between burnout and insomnia. Armon et al13 indicated that burnout and insomnia recursively predict each other's development and intensification over time. In contrast, Jansson-Fröjmark et al31 demonstrated that the link between burnout and insomnia was not bidirectional. These authors have conducted a longitudinal prospective study during 1 year in 1258 participants, and they observed that insomnia increases the risk for the persistence of EE (the core burnout dimension) by more than three times. Moreover, they showed that burnout was not related to future insomnia.
The strong relation between insomnia and burnout could be explained by a chronic hyperarousal that might be related to the accumulation of stress at work responsible for the disturbed emotion. However, it would be only possible to assess it by PSG (the gold standard in the objective assessment of sleep). Since insomnia and major depressive disorder are known to be associated with hyperarousal,38 and instability of rapid eye movement (REM) sleep,39 polysomnographic studies focused on hyperarousal and REM sleep in burnout participants could be useful.
Limitations
This study has several limitations. It was cross-sectional; therefore, it was not possible to analyse the causal relationships between the variables. A prospective study is required to demonstrate the causal relationship between insomnia to burnout and job strain in our population of white-collar financial employees.13 31 The timing of the snapshot is not guaranteed to be representative, as far as there are seasonal variations in the professional activity all along the year. As in many studies, our sleep data were based on self-reports. In the future, experimental research would be interesting to objectively investigate the inter-relationship between insomnia and burnout and the sleep characteristics (eg, fragmentation) using ultraminiaturised PSG as previously used by us.40
Conclusions
This study evidenced a moderate prevalence of burnout in financial workers who are under high job strain but with high job satisfaction. In this specific and not often studied working population, high job strain is significantly associated with burnout only in individuals with insomnia. Insomnia appears to be a strong clinical marker of burnout.
This findings suggest that (1) insomnia should be better targeted for prevention of mental health in the workplace, (2) it would be interesting to include the monitoring of sleep parameters in the detection and survey of burnout, particularly in high job strain workers and (3) participants with high scores of burnout and insomnia can define a subgroup at high risk of mental disorder. Future research on other professional groups such as physicians or the large group of medical occupations who are more prone to burnout prevalence should be conducted in order to detect, prevent or treat sleep disorders, particularly insomnia.
Acknowledgments
The authors would like to thank all the employees who agreed to participate in this study and Mrs Berot Stéphanie for administrative help for producing the data files necessary for these analyses. The study was conducted in close collaboration with Donnet J, Vaucouleur F, Gouache B, Balika Y, Demirer-Vivenot F and De Testa A.
Footnotes
Contributors: AM, FS, DL and MC were involved in conception or design of the work. AM, FS, DGM, ME, JYD, DL and MC acquired, analysed and interpreted the data and manuscript redaction. All authors reviewed and approved the final manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The local hygiene and safety committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behav 1981;2:99–113. 10.1002/job.4030020205 [DOI] [Google Scholar]
- 2.Kim HJ, Shin KH, Umbreit WT. Hotel job burnout: the role of personality characteristics. Int J Hosp Manage 2007;26:421–34. 10.1016/j.ijhm.2006.03.006 [DOI] [Google Scholar]
- 3.Carod Artal FJ, Vazquez Cabrera C. Burnout syndrome in an international setting. In: Bahrer-Kohler S, ed.. Burnout for experts. NewYork: Prevention in the Context of Living and Working Springer Press, 2013:15–35. [Google Scholar]
- 4.Von Bonsdorff MB, Seitsamo J, von Bonsdorff ME et al. . Job strain among blue-collar and white-collar employees as a determinant of total mortality: a 28-year population-based follow-up. BMJ Open 2012;2:e000860 10.1136/bmjopen-2012-000860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imai H, Nakao H, Tsuchiya M et al. . Burnout and work environments of public health nurses involved in mental healthcare. Occup Environ Med 2004;61:764–8. 10.1136/oem.2003.009134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finney C, Stergiopoulos E, Hensel J et al. . Organizational stressors associated with job stress and burnout in correctional officers: a systematic review. BMC Public Health 2013;13:82 10.1186/147162458-13-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mojsa-Kaja J, Golonka K, Marek T. Job burnout and engagement among teachers—worklife areas and personality traits as predictors of relationships with work. Int J Occup Med Environ Health 2015;28:102–19. 10.13075/ijomeh.1896.00238 [DOI] [PubMed] [Google Scholar]
- 8.Grassi L, Magnani K. Psychiatric morbidity and burnout in the medical profession: an Italian study of general practitioners and hospital physicians. Psychother Psychosom 2000;69:329–34. doi:12416 [DOI] [PubMed] [Google Scholar]
- 9.Embriaco N, Azoulay E, Barrau K et al. . High level of burnout in intensivists prevalence and associated factors. Am J Respir Crit Care Med 2007;175:686–92. 10.1164/rccm.200608-1184OC [DOI] [PubMed] [Google Scholar]
- 10.Söderström M, Ekstedt M, Åkerstedt T et al. . Sleep and sleepiness in young individuals with high burnout scores. Sleep 2004;17:1369–77. [DOI] [PubMed] [Google Scholar]
- 11.Ekstedt M, Söderström M, Åkerstedt T et al. . Disturbed sleep and fatigue in occupational burnout. Scand J Work Environ Health 2006;32:121–31. [DOI] [PubMed] [Google Scholar]
- 12.Grossi G, Perski A, Evengård B et al. . Physiological correlates of burnout among women. J Psychosom Res 2003;55:309–16. 10.1016/S0022-3999(02)00633-5 [DOI] [PubMed] [Google Scholar]
- 13.Armon G, Shirom A, Shapira I et al. . On the nature of burnout-insomnia relationships: a prospective study of employed adults. J Psychosom Res 2008;65:5–12. 10.1016/j.jpsychores.2008.01.012 [DOI] [PubMed] [Google Scholar]
- 14.Galam E, Komly V, Le Tourneur A et al. . Burnout among French GPs in training: a cross-sectional study. Br J Gen Pract 2013;63:217–23. 10.3399/bjgp13X664270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vercambre MN, Brosselin P, Gilbert F et al. . Individual and contextual covariates of burnout: a cross-sectional nationwide study of French teachers. BMC Public Health 2009;9:333 10.1186/1471-2458-9-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd edn Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
- 17.Shanafelt TD, Bradley KA, Wipf JE et al. . Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67. 10.7326/0003-4819-136-5-200203050-00008 [DOI] [PubMed] [Google Scholar]
- 18.Niedhammer I, Chastang JF, Gendrey L et al. . Psychometric properties of the French version of Karasek's “Job Content Questionnaire” and its scales measuring psychological pressures, decisional latitude and social support: the results of the SUMER. Santé publique 2006;18:413–27. [DOI] [PubMed] [Google Scholar]
- 19.Leger D, Guilleminault C, Dreyfus JP et al. . Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res 2000;9:35–42. 10.1046/j.1365-2869.2000.00178.x [DOI] [PubMed] [Google Scholar]
- 20.Metlaine A, Leger D, Choudat D. Socioeconomic impact of insomnia in working populations. Ind Health 2005;43:11–9. 10.2486/indhealth.43.11 [DOI] [PubMed] [Google Scholar]
- 21.Darien I, International Classification of sleep disorders. 3rd edn American Academy of Sleep Medicine, 2014. [Google Scholar]
- 22.Heit HA, Gourlay DL. DSM-V and the definitions: time to get it right. Pain Med 2009;10:784–6. 10.1111/j.1526-4637.2009.00654.x [DOI] [PubMed] [Google Scholar]
- 23.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 1992;15:376–81. [DOI] [PubMed] [Google Scholar]
- 24.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 25.Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. Basic Books, New York, 1992. [Google Scholar]
- 26.Costa EF, Santos SA, Santos AT et al. . Burnout syndrome and associated factors among medical students: a cross-sectional study. Clinics (Sao Paulo) 2012;67:573–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zis P, Anagnostopoulos F, Sykioti P. Burnout in medical residents: a study based on the job demands-resources model. Sci World J 2014;6:732–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nyberg ST, Fransson EI, Heikkilä K et al. , IPD-Work Consortium. Job strain and cardiovascular disease risk factors: meta-analysis of individual-participant data from 47,000 men and women. PLoS ONE 2013;8:e67323 10.1371/journal.pone.0067323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agbenyikey W, Karasek R, Cifuentes M et al. . Job strain and cognitive decline: a prospective study of the Framingham offspring cohort. Int J Occup Environ Med 2015;6:79–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Esquirol Y, Bongard V, Mabile L et al. . Shift work and metabolic syndrome: respective impacts of job strain, physical activity, and dietary rhythms. Chronobiol Int 2009;26:544–59. 10.1080/07420520902821176 [DOI] [PubMed] [Google Scholar]
- 31.Jonsson-Fröjmark M, Lindblom K. Is there a bidirectional link between insomnia and burnout ? A prospective study in the Swedish workforce. Int J Behav Med 2010;17:306–13. 10.1007/s12529-010-9107-8 [DOI] [PubMed] [Google Scholar]
- 32.Portela LF, Kröning Luna C, Rotenberg L et al. . Job strain and self-reported insomnia symptoms among nurses: what about the influence of emotional demands and social support? Biomed Res Int 2015;2015:820610 10.1155/2015/820610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saijo Y, Chiba S, Yoshioka E et al. . Synergistic interaction between job control and social support at work on depression, burnout, and insomnia among Japanese civil servants. Int Arch Occup Environ Health 2015;88:143–52. 10.1007/s00420-014-0945-6 [DOI] [PubMed] [Google Scholar]
- 34.de Beer LT, Pienaar J, Rothmann S Jr.. Job burnout's relationship with sleep difficulties in the presence of control variables: a self-report study. South African J Psychol 2014;44:454–66. [Google Scholar]
- 35.Melamed S, Ugarten U, Shirom A et al. . Chronic burnout, somatic arousal and elevated salivary cortisol levels. J Psychosom Res 1999. Jun; 46:591–8. 10.1016/S0022-3999(99)00007-0 [DOI] [PubMed] [Google Scholar]
- 36.Tokuda Y, Hayano K, Ozaki M et al. . The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis. Ind Health 2009;47:166–72. 10.2486/indhealth.47.166 [DOI] [PubMed] [Google Scholar]
- 37.Taylor DJ, Lichstein KL, Durrence HH et al. . Epidemiology of insomnia, depression, and anxiety. Sleep 2005;28:1457–64. [DOI] [PubMed] [Google Scholar]
- 38.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev 2010;14:9–15. 10.1016/j.smrv.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 39.Riemann D, Spiegelhalder K, Nissen C et al. . REM sleep instability—a new pathway for insomnia? Pharmacopsychiatry 2012;45:167–76. 10.1055/s-0031-1299721 [DOI] [PubMed] [Google Scholar]
- 40.Arnal PJ, Sauvet F, Leger D et al. . Benefits of sleep extension on sustained attention and sleep pressure before and during total sleep deprivation and recovery. Sleep 2015;38:1935–43. [DOI] [PMC free article] [PubMed] [Google Scholar]