Abstract
With aging, intact parathyroid hormone (iPTH) increases. It plays a crucial role in left ventricular hypertrophy (LVH). Also, 25-hydroxy vitamin D (Vit-D) and iPTH have been observed to be determinants of muscle wasting known as sarcopenia. Fetuin A (FetA), a systemic calcification inhibitor, involves in the development of diastolic heart failure. Hence, we hypothesized that the interplay among FetA, Vit-D and iPTH may contribute to sarcopenic LVH among the elders. We analyzed a database from the Tianliao Old People study with 541 elders (≥65 years) in a Taiwan’s suburban community. After excluding patients with renal function impairment, 120/449 (26.7%) patients were diagnosed with sarcopenia. Sarcopenic patients had lower serum Vit-D levels but higher FetA as well as iPTH. Notably, sarcopenic patients with LVH had significantly lower FetA and higher iPTH levels. In multivariate logistic regression analysis, only the increase in iPTH was independently associated with sarcopenic LVH (Odds ratio: 1.05; confidence interval: 1.03–1.08, p = 0.005). Using iPTH >52.3 ng/l as a cutoff point, the sensitivity and specificity was 66% and 84%, respectively. In conclusion, FetA, Vit-D, and iPTH levels were all associated with sarcopenia in this geriatric population. Among them, iPTH specifically indicates patients with sarcopenic LVH.
With aging, the incidence of sarcopenia, an involuntary reduction in fatty-free muscle mass, and cardiac hypertrophy increases1,2,3,4. A growing number of studies have reported a continuous loss of myocytes subsequent to reactive hypertrophy of the remaining cells in age-related cardiac changes, or cells filled with fibrotic, adipose tissue in the extracellular matrix4,5. Although age-related cardiac changes have been well described in humans and rats, only a few studies have determined whether sarcopenia occurs in cardiac muscle5,6,7,8. Notably, the balance between vitamin D (Vit-D) and parathyroid hormone (PTH) has been considered a key regulator of muscle strength9. In a longitudinal aging study, low Vit-D and high PTH concentrations were concluded to be determinants of sarcopenia10. Increased PTH-induced cardiac hypercontractility subsequently causes reactive cardiac hypertrophy11. Fetuin-A (FetA) is a calcification inhibitor and is involved in insulin resistance12,13,14,15,16. It was a potential regulator of cardiovascular disease, and also recently reported to be a main factor in adjusting body composition remodeling in the geriatric population17. Also, FetA- and Vit-D receptor- knockout mice had significant ventricular hypertrophy and diastolic dysfunction18.
We previously reported a high concentration of FetA was associated with left ventricular dysfunction in participants with sarcopenia19. However, whether there is any interplay between these mineral-modification factors according to the development of heart failure in sarcopenic populations remains indeterminate. Herein, we aimed to study FetA, Vit-D, and PTH concentrations in the elderly (≥65 years old) with or without sarcopenia and left ventricular hypertrophy (LVH).
Results
Clinical and echocardiographic characteristics of participants with and without sarcopenia
One hundred twenty (26.7%) of the 449 participants were diagnosed with sarcopenia (Sarc+). Sarc+ participants were significantly (all p = 0.001) older, were more likely to be female, and had smaller waist circumferences, lower BMIs, and lower mean blood pressure (BP) (Table 1). Echocardiography showed preserved E/E′. Generally, their serologic profiles were similar, except for lower serum Vit-D concentrations (43.7 ± 11.5 vs. 41.0 ± 10.8 ng/ml, p = 0.04) but higher FetA (621.1 ± 140.7 vs. 697.3 ± 179.6 μg/dl, p < 0.001) and PTH (44.1 ± 28.6 vs. 52.1 ± 29.1 ng/l, p = 0.01) concentrations. None had specific heart failure symptoms. LVH+ participants (75/449, 16.7%) had larger waist circumferences, higher systolic blood pressure (SBP), and higher serum PTH concentrations (Supplementary Table 1). Their serum calcium, phosphate, Vit-D, and FetA concentrations were not significantly different from those of LVH− participants.
Table 1. Clinical and echocardiographic characteristics: comparison between Sarc− and Sarc+ groups.
| Without Sarcopenia (Sarc−) | With Sarcopenia (Sarc+) | p | |
|---|---|---|---|
| (329/449, 73.3%) | (120/449, 26.7%) | ||
| Age (years) | 75.20 ± 5.8 | 80.00 ± 6.1 | <0.001 |
| Male (%) | 190.00 (57.7) | 33 (27.5) | <0.001 |
| Waist circumference (cm) | 88.40 ± 9.7 | 78.70 ± 9 | <0.001 |
| BMI (kg/m2) | 25.10 ± 3.8 | 21.40 ± 2.9 | <0.001 |
| SBP (mmHg) | 135.70 ± 20.9 | 127.40 ± 19.9 | 0.002 |
| DBP (mmHg) | 77.60 ± 11.9 | 72.70 ± 10.9 | 0.001 |
| Medical History (%) | |||
| Previous stroke | 19 (5.7) | 4 (3.3) | 0.90 |
| CAD | 36 (10.9) | 8 (6.6) | 0.85 |
| Arrhythmia | 10 (3) | 3 (2.5) | 0.33 |
| Cancer | 9 (2.7) | 6 (5) | 0.65 |
| Serology profiles | |||
| eGFR | 83.20 ± 16.2 | 71.00 ± 8.9 | 0.53 |
| HbA1c (%) | 6.10 ± 0.9 | 6.10 ± 1.2 | 0.92 |
| TG (mg/dl) | 130.40 ± 80.1 | 118.50 ± 61.3 | 0.24 |
| Cholesterol (mg/dl) | 201.80 ± 36.8 | 204.90 ± 34.9 | 0.51 |
| Calcium (mg/dl) | 9.10 ± 0.4 | 9.10 ± 0.4 | 0.61 |
| Phosphate (mg/dl) | 3.50 ± 0.5 | 3.60 ± 0.4 | 0.36 |
| FetA (μg/dl) | 621.10 ± 140.7 | 697.30 ± 179.6 | <0.001 |
| Vit-D (ng/ml) | 43.70 ± 11.5 | 40.90 ± 10.8 | 0.02 |
| PTH (ng/l) | 44.10 ± 28.6 | 52.10 ± 29.1 | 0.01 |
| Echocardiographic parameters | |||
| LVMI (g/M2) | 82.10 ± 19.9 | 77.10 ± 16.8 | 0.34 |
| LVEF (%) | 71.30 ± 6.4 | 70.00 ± 4.7 | 0.34 |
| E/A | 0.70 ± 0.2 | 0.70 ± 0.3 | 0.69 |
| E′ (m/s) | 0.08 ± 0.02 | 0.08 ± 0.02 | 0.61 |
| E/E′ | 7.60 ± 2.1 | 9.20 ± 4.4 | 0.002 |
| Diastolic dysfunction | 50 (15.2) | 18 (15) | 0.06 |
Data are expressed as n (%) or mean ± standard error. BMI = body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure; eGFR = estimated glomerular filtration rate; CAD = coronary artery disease; HbA1C = glycated hemoglobin; TG = triglyceride; FetA = Fetuin A; Vit-D = 25-hydroxy vitamin D; PTH = parathyroid hormone; LVMI = left ventricular mass index; LVEF = left ventricular ejection fraction; E/A = transmitral valve E to A velocity ratio; E/E′ = mitral early filling velocity to early diastolic mitral annular velocity ratio.
In this case control study, 10 (8.3%) of the 120 Sarc+ participants were also LVH+ (Table 2). Significantly (p < 0.001) more participants diagnosed as Sarc+ LVH+ were male and had relatively lower SBP than did Sarc+ LVH− participants, their prevalence of stroke, coronary artery disease (CAD), and arrhythmia was not significantly different. Notably, Sarc+ LVH+ participants had significantly lower FetA concentrations (696.9 ± 171.9 vs. 547.6 ± 142.6 μg/dl, p < 0.03) but significantly higher PTH concentrations (44.7 ± 17.6 vs. 63.7 ± 17.9 ng/l, p = 0.007) no significant differences in Vit-D, calcium, or phosphate concentrations. Echocardiography showed significantly higher LVMI and a lower E/E′ in the Sarc+ LVH+ subgroup. The incidence of diastolic dysfunction (impaired relaxation [E′ < 0.08 m/s] and high left ventricular end-diastolic pressure [E/E′ > 8]) was significantly higher in the Sarc+ LVH+ subgroup than in the other subgroups.
Table 2. Clinical and echocardiographic characteristics: comparison between Without Sarcopenia and Without Left Ventricular Hypertrophy (Sarc− LVH−), Without Sarcopenia and With Left Ventricular Hypertrophy (Sarc− LVH+), With Sarcopenia and Without Left Ventricular Hypertrophy (Sarc+ LVH−), With Sarcopenia and With Left Ventricular Hypertrophy (Sarc+ LVH+) groups.
| Without Sarcopenia (Sarc−) |
With Sarcopenia (Sarc+) |
F | p | |||
|---|---|---|---|---|---|---|
| (329/449, 73.3%) |
(120/449, 26.7%) |
|||||
| Sarc− LVH− | Sarc− LVH+ | Sarc+ LVH− | Sarc+ LVH+ | |||
| (n = 272, 60.57%) | (n = 57, 12.69%) | (n = 110, 24.49%) | (n = 10, 2.2%) | |||
| Age (years) | 75.80 ± 5.9 | 77.70 ± 6.1a | 80.20 ± 6.1a | 77.50 ± 7.7 | 6.3 | <0.001 |
| Male (%) | 158 (58) | 37 (64.9) | 24 (21.8)a,b | 4 (40)a,b | <0.001 | |
| WC (cm) | 87.90 ± 9.6 | 91.95 ± 8.49 | 78.81 ± 9.22a,b | 78.80 ± 1.83a,b | 15.7 | <0.001 |
| BMI (kg/m2) | 24.40 ± 4 | 25.82 ± 2.9 | 21.50 ± 3a | 20.00 ± 0.1a,b | 11.5 | <0.001 |
| SBP (mmHg) | 133.90 ± 19.4 | 143.90 ± 23.2 | 128.20 ± 19.9a | 120.00 ± 14.1a,b | 4.6 | 0.001 |
| DBP (mmHg) | 76.90 ± 11.7 | 80.40 ± 14.1 | 78.90 ± 10.6 | 80.50 ± 9.2a | 3.9 | 0.004 |
| Previous stroke | 16 (5.8) | 3 (5.2) | 3 (2.7) | 1 (10) | 0.33 | |
| CAD | 28 (10.3) | 8 (14) | 6 (5.4) | 2 (20) | 0.06 | |
| Arrhythmia | 9 (3.2) | 1 (1.7) | 2 (1.8) | 1 (10) | 0.08 | |
| Cancer | 5 (1.8) | 4 (7) | 5 (4.5) | 1 (10) | 0.34 | |
| GFR | 80.50 ± 12.5 | 83.90 ± 11.3 | 78.20 ± 8.9 | 75.10 ± 9.8 | 3.2 | 0.21 |
| HbA1c (%) | 6.02 ± 0.9 | 5.95 ± 0.58 | 6.10 ± 1.2 | 6.40 ± 0.9 | 1.3 | 0.282 |
| TG (mg/dl) | 119.20 ± 76.5 | 109.30 ± 51.1 | 120.00 ± 61.9 | 95.00 ± 46.7 | 0.3 | 0.902 |
| Cholesterol (mg/dl) | 195.10 ± 35.3 | 193.80 ± 30.3 | 206.00 ± 34.6 | 158.00 ± 28.3 | 2.1 | 0.082 |
| Cholesterol (mg/dl) | 9.10 ± 0.3 | 8.80 ± 0.6 | 8.90 ± 0.3 | 8.80 ± 0.5 | 0.8 | 0.15 |
| Phosphate (mg/dl) | 3.40 ± 0.8 | 3.70 ± 1.7 | 3.50 ± 0.5 | 3.60 ± 0.8 | 0.7 | 0.51 |
| FetA (μg/dl) | 613.60 ± 136.7 | 602.10 ± 88.6 | 696.90 ± 171.9 | 547.60 ± 142.5a,b,c | 2.8 | 0.026 |
| Vit-D (ng/ml) | 48.30 ± 10.4 | 47.20 ± 9.8 | 40.20 ± 10.8 | 40.30 ± 6.2 | 5.4 | 0.08 |
| PTH (ng/l) | 38.40 ± 12.7 | 38.30 ± 14.9 | 44.70 ± 17.6 | 63.70 ± 17.9a,b | 3.6 | 0.007 |
| LVMI (g/M2) | 75.30 ± 13.9 | 113.50 ± 11.9a | 75.10 ± 12.1 | 103.60 ± 1.5a,c | 58.1 | <0.001 |
| LVEF (%) | 71.30 ± 6.2 | 71.10 ± 6.6 | 69.90 ± 4.9 | 70.50 ± 0.7 | 0.2 | 0.924 |
| E/A | 0.70 ± 0.2 | 0.70 ± 0.2 | 0.70 ± 0.2 | 0.70 ± 0.2 | 7.3 | 0.1 |
| E′ (m/s) | 0.08 ± 0.01 | 0.08 ± 0.02 | 0.09 ± 0.01 | 0.06 ± 0.02 | 2.1 | 0.089 |
| E/E′ | 7.50 ± 2 | 7.90 ± 2.3 | 7.80 ± 1.3 | 9.60 ± 1.6 | 3.4 | 0.08 |
| Diastolic dysfunction | 29 (10.7) | 21 (36.8) | 8 (7.2) | 10 (100)a,b,c | 8.9 | 0.001 |
Data are n (%) or mean ± standard error. Abbreviations presented in Table 1.
aP < 0.05, compared with Sarc− LVH−.
bP < 0.05, compared with Sarc− LVH+.
cp < 0.05, compared with values of Sarc− LVH+.
There were more Sarc+ and Sarc+ LVH+ female participants in the fourth quartile of PTH (concentration > 51.82 ng/l) (Supplementary Table 2). Likewise, there were significantly more Sarc+ LVH+ female participants in the first quartile of Vit-D (Supplementary Table 3).
The diagnostic effect of PTH on Sarc+ LVH+ participants
In the multivariate logistic regression, female gender, a lower BMI, and a lower Vit-D concentration were significantly correlated with sarcopenia (Supplementary Table 4), but only a higher PTH concentration significantly predicted that a participant was Sarc+ LVH+ (odds ratio: 1.05, 95% CI: 1.03–1.08, p < 0.005) (Table 3).
Table 3. Univariate and multivariate regression analyses to identify participants with sarcopenic left ventricular hypertrophy (Sarc+ LVH+).
| Univariate Analysis |
Multivariate Analysis |
|||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (years) | 1.07 (1.01–1.14) | 0.02 | ||
| Male (%) | 0.85 (0.37–1.96) | 0.7 | ||
| FetA (μg/dl) | 1.02 (1.00–1.08) | 0.01 | 1.01 (0.999–1.020) | 0.06 |
| PTH (ng/l) | 1.80 (1.2–2.7) | <0.001 | 1.05 (1.03–1.08) | <0.001 |
| LVMI (g/M2) | 1.56 (1.08–1.84) | 0.01 | 1.01 (0.85–1.32) | 0.12 |
Data are expressed as n (%) or mean ± standard error. OR = odds ratio; CI = confidence interval; FetA = Fetuin A; PTH = parathyroid hormone; LVMI = left ventricular mass index.
The area under the ROC curve was 0.75 for Sarc+ LVH+ compared with 0.7 for LVMI and 0.67 for age (Fig. 1). The ROC curve, using PTH > 52.3 ng/l as a cutoff point, showed a sensitivity of 66% and a specificity of 84% for a Sarc+ LVH+ diagnosis.
Figure 1. The areas under the ROC curves for the predictor of sarcopenic left ventricular hypertrophy were 0.7 for left ventricular mass index (LVMI), 0.67 for age and 0.75 for parathyroid hormone (PTH).

Discussion
The present study’s three main findings are: (1) sarcopenia and cardiac hypertrophy were not rare in the geriatric population; (2) PTH was significantly associated with Sarc+ LVH+, independently of hypertension and serum calcium and phosphate concentrations; (3) PTH >52.3 ng/l is a biomarker that indicates Sarc+ LVH+.
Aging is a major cause of congestive heart failure5,6. Clinically, 40–50% percent of patients with symptomatic heart failure have preserved systolic function, which is called “diastolic dysfunction”5,8. People with diastolic heart failure tend to be older and have sarcopenia, chronic heart failure, and cardiac hypertrophy8. Physiologically, diastolic dysfunction occurs when a rigid ventricle fails to properly fill7,8. Importantly, the survival of participants with diastolic dysfunction is similar to that of patients with systolic dysfunction5. The importance of investigating diastolic heart failure has recently been emphasized. One study20 reported that in Vit-D receptor-knockout mice, suppressing the pro-hypertrophic calcineurin pathway led to cardiac hypertrophy20, and another21 reported that PTH activates the protein kinase C of cardiomyocytes and induces hypertrophic growth. PTH treatment, though being shown to improve cardiac function after myocardial infarction by increasing neovascularization and cell survival, also increases fibrosis, which accelerates decompensated heart failure22. Notably, the combination of lower Vit-D and higher PTH concentrations appears to be independently associated with sudden cardiac death in older adults without overt cardiovascular disease23. FetA, although valued as a negative acute-phase protein, has anti-inflammatory characteristics and protects patients with renal failure from cardiovascular events. Emerging evidence indicated its dark sides in insulin resistance, myocardial infarction and ischemic stroke24,25. Despite causing cardiac hypertrophy and diastolic dysfunction in FetA-knockout mice18, the actual role of FetA in the development of heart failure remains uncertain.
Other studies3,4 have hypothesized several mechanisms for sarcopenia. Some hypothesize sarcopenic obesity: the notion that adipose tissue replaces lost myocytes3. A recent study17 showed that higher FetA concentrations were associated with the accumulation of visceral fat tissue in well-functioning, community-living older people, which corresponds to the spirit of sarcopenic obesity. Vit-D directly affected various aspects of muscle function, including myofibrillar protein degradation and impaired calcium transmission in the mitochondria26. One study27 reported that a Vit-D deficiency in the elderly causes secondary hyperparathyroidism. The coexistence of low Vit-D and high PTH has been a determinant of muscle strength loss in the elderly10.
In our previous study of the TOP population19, the Sarc+ group tended to have a higher concentration of FetA, which was associated with poor heart function. More recently, we documented28 that the hearts of the elderly were stiffer than those of younger people. In a mouse model that investigated cardiac sarcopenia7, senescent mice showed both intracellular lipid accumulation and a decrease in glycogen storage. In humans, many mechanisms have been proposed for the aging process, including mitochondrial function changes, senescence adaption, and telomerase shortening29,30. Quantitative studies7,31 have shown that a continuous loss of myocytes is accompanied by reactive hypertrophy of the remaining cells, or that the extracellular matrix is filled with fibrotic, adipose tissue. The adaptation of the left ventricle is a complex process of hormonal, structural, and hemodynamic factors, and most serological markers changed with aging7,31. In the present study, we analyzed the related mineralizing serological markers—FetA, Vit-D, and PTH—in elderly Sarc+ LVH+, Sarc+ LVH−, Sarc− LVH+, and Sarc− LVH− participants. To prevent the disturbance of the calcium and phosphate balance in participants with impaired renal function, we focused only on participants with preserved renal function. Consequently, in addition to low Vit-D concentrations in Sarc+ participants, we discovered the specific association between PTH and Sarc+ LVH+ participants independently of hypertension and of calcium or phosphate concentration.
Our study has some limitations. First, only 120 of our 449 (26.7%) participants presented as Sarc+ LVH+, and the statistical findings might be over-fitted. Second, cardiac dysfunction and hypertrophy were defined based on echocardiography, and none of participants diagnosed with these diseases presented with clinical symptoms. Third, through this case control study, identifying the causal relationship between iPTH and diastolic dysfunction faces difficulty. More studies in the future to correlate the echocardiographic findings to clinical symptoms are required.
Conclusion
The mineralizing markers FetA, Vit-D, and PTH were all associated with sarcopenia in our participants. PTH identified Sarc+ LVH+ participants. However, more investigation and longitudinal follow-ups are required to verify the clinical effects of Sarc+ LVH+.
Methods
Study Population
Tianliao Township is a suburban community of Kaohsiung City, Taiwan. Nearly a quarter (23.7%) of its 31,000 residents are >65 years old. The Tianliao Old People (TOP) study19 has continuously been conducted for the elders since 2009 in order to develop better community-oriented primary-care services. Based on the 2010 census, there were 1,033 elderly men in Tianliao. In July 2010, we used the whole community sampling method for an epidemiological survey. After excluding 269 empty houses, 21 deaths, and 62 non-ambulatory residents, only 681 residents were eligible. The response rate was 60.8% and the statistical power was 0.80. After residents with left ventricular systolic dysfunction (left ventricular ejection fraction <50%) and renal function impairment (estimated glomerular filtration rate [eGFR] <60 mL/min per 1.73 m2, based on the Kidney Disease: Improving Global Outcomes (KDIGO) recommendation <http://kdigo.org/home/>), and residents taking calcium, PTH, or Vit-D supplements had been excluded, 541 residents were enrolled. Based on the medical history reported by each participant, medical information about strokes, coronary artery disease, arrhythmia, and cancer was recorded. Anthropometric (e.g., body mass index [BMI]) and duplicate waist circumference measurements were done on bare skin midway between the lower rib margin and the iliac crest at the end of normal expiration. Each participant signed an informed consent before they were examined. This study was approved by the Institutional Review Board of National Cheng Kung University Hospital (IRB: ER-99-111) and all methods were performed in accordance with our local guidelines and clinical regulations.
Laboratory Methods
After the participants had fasted for at least 8 hours, peripheral blood samples were collected and centrifuged at 3,000 rpm for 15 minutes at 4 °C. The samples were frozen and sent to a central laboratory for analysis. Serum PTH, Vit-D, and FetA were determined using an ELISA assay (Biovendor Laboratory Medicine, Brno, Czech Republic). The minimum detectable concentrations of PTH, Vit-D, and FetA were 0.2, 0.8, and 9.38 ng/ml, respectively.
Definition of Sarcopenia
To define sarcopenia in this study, we measured skeletal muscle mass (SMM) using a bioelectrical impedance analyzer (BioScan 920; Maltron, Rayleigh, Essex, UK), a convenient, noninvasive, and radioisotope-free tool with an operating frequency of 50 kHz at 800 mA. Participants were supine on a non-conductive surface with their arms abducted away from their trunk and their legs slightly separated for 5 minutes. Four electrodes and cables were attached to their right hand and ankle. When the measurements stabilized, the analyzer displayed resistance directly and immediately. SMM was calculated using the BIA equation (described elsewhere)2:
 |
 |
The associated units were: height in cm; resistance in ohms (Ω); gender (51 men, 50 women); and age in years. Absolute SMM was converted to an SMI by dividing it by height in square meters (SMM/Ht m2). Based on the literature1,2,19, the normal range of the SMI was defined as >7.23 for men and >5.67 for women.
Sarcopenia was defined based on the 2010 criteria of the European Working Group on Sarcopenia in Older People (EWGSOP)2 as presenting 3 of the following components: (1) loss of muscle mass: an SMI of ≥2 standard deviations (SDs) less than the normal gender-specific mean. In the studied population, an SMI <7.23 in men and <5.67 in women meant being assigned to the sarcopenic group; (2) low muscle strength: the maximal weight of hand-grasping <30 pounds in men and <20 pounds in women; (3) low physical performance: a maximal walking speed <0.8 m/s.
Echocardiography
Standard echocardiography was done (Vivid I; GE Vingmed Ultrasound AS, Horten, Norway) using a 3.5-MHz multiphase-array probe, based on the recommendations of the American Society of Echocardiography32. The chamber dimensions, left ventricular (LV) mass, LV ejection fraction (LVEF), and left ventricular mass index (LVMI) were all determined using 2D and 3D M-mode methods.
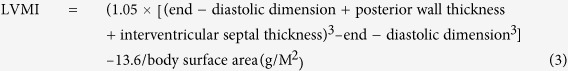 |
LVMIs >102 g/M2 in men and >88 g/M2 in women were defined as cardiac hypertrophy. Transmitral Doppler flow velocity was obtained from an apical four-chamber view, and peak early mitral inflow velocity (E), peak atrial velocity (A), and the E/A ratio were recorded. Early mitral inflow velocity and early annular diastolic velocity (E′) were also measured to estimate the LV end-diastolic pressure (E/E′). Both the medial and lateral early annular diastolic velocity values were measured to determine the mean value. Echocardiographic diastolic dysfunction was defined as the coexistence of impaired relaxation (E′ < 0.08 m/s [determined using tissue Doppler]) and elevated mean LV end-diastolic pressure (E/E′ > 8)23. To distinguish them from the population with preserved LV systolic function, participants with an LVEF <50% were defined as having an impaired LV systolic function (or left ventricular dysfunction [LVD])24. The systolic and diastolic function of each echocardiographic image was analyzed in triplicate by experienced cardiologists. Based on the criteria of sarcopenia and of LVH, participants were assigned to sarcopeniaPositive LVHNegative (Sarc+-LVH−), Sarc−-LVH+, Sarc−-LVH−, and Sarc+-LVH+ groups.
Statistical Analysis
Data management and statistical analyses were done using SPSS 18.0. Continuous variables with a normal distribution are expressed as means ± standard deviation (SD). Other continuous variables with a non-normal distribution are expressed as means ± standard error (SE). Continuous variables were compared using Student’s t test for normally distributed values. To validate the association between sarcopenia and heart function, we separated the participants based on whether they had sarcopenia, LVH, or both. Group differences were analyzed using analysis of variance (ANOVA). Significant differences verified using a Tukey post hoc test in analysis were entered into multivariate analysis. Odds ratios (ORs) and 95% confidence intervals (CIs) were assessed using logistic regression. Statistical tests were 2-sided; significance was set at p < 0.05. Receiver operating characteristic (ROC) curve analysis was used to determine the optimal cutoff values of PTH in participants with and without sarcopenic cardiomyopathy. The best cutoff value was defined as the point with the highest sum of sensitivity and specificity.
Additional Information
How to cite this article: Chang, W.-T. et al. Serum vitamin D, intact parathyroid hormone, and Fetuin A concentrations were associated with geriatric sarcopenia and cardiac hypertrophy. Sci. Rep. 7, 40996; doi: 10.1038/srep40996 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
This research was supported from grants of Ministry of Science and Technology, Taiwan (MOST 103-2628-B-006-002-MY4; 105-2314-B-006-057-MY3) and grant from National Cheng Kung University Hospital (2012-2015, P.Y.L.). The investigator (P.Y.L.) was granted by “A Landmark Project to Promote Innovation & Competitiveness of Clinical Trials by the Excellent Clinical Trial and Research Center in National Cheng Kung University Hospital, Ministry of Health and Welfare, Taiwan”.
Footnotes
Author Contributions Study concept and design, W.C. and P.L. Acquisition of data, W.C., C.W. and P.L. Analysis and interpretation of data, W.C., W.T. and P.L. Drafting of the manuscript, W.C. and P.L. Statistical analysis, W.C. and P.L. Administrative, technical, or material support, W.C., H.L., C.P., Y.J., W.T., C.W., C.C. and P.L. Study supervision, P.L.
References
- Patel H. P. et al. Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People (EWGSOP) definition: Findings from the Hertfordshire Cohort Study. Age Ageing. 42, 378–84 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Jentoft A. J. et al. Sarcopenia: European consensus on definition and diagnosis: Report of the EuropeanWorking Group on Sarcopenia in Older People. Age Ageing. 39, 412–23 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauley J. A. An Overview of Sarcopenic Obesity. J Clin Densitom. 18, 499–505 (2015). [DOI] [PubMed] [Google Scholar]
- Anker M. S., von Haehling S., Springer J., Banach M. & Anker S. D. Highlights of the mechanistic and therapeutic cachexia and sarcopenia research 2010 to 2012 and their relevance for cardiology. Int J Cardiol. 162, 73–6 (2013). [DOI] [PubMed] [Google Scholar]
- Zile M. R. & Brutsaert D. L. New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation. 105, 1387–93 (2002). [DOI] [PubMed] [Google Scholar]
- Chin S. O. et al. Sarcopenia is independently associated with cardiovascular disease in older Korean adults: the Korea National Health and Nutrition Examination Survey (KNHANES) from 2009. PLOS One. 8, e60119 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J. et al. Age-related cardiac muscle sarcopenia: Combining experimental and mathematical modeling to identify mechanisms. Exp Gerontol. 43, 296–306 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fülster S. et al. Muscle wasting in participants with chronic heart failure: Results from the studies investigating co-morbidities aggravating heart failure (SICA-HF). Eur Heart J. 34, 512–9 (2013). [DOI] [PubMed] [Google Scholar]
- Houston D. K. et al. Association between vitamin D status and physical performance: The InCHIANTI study. J Gerontol A Biol Sci Med Sci. 62, 440–6 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser M., Deeg D. J. & Lips P. Low vitamin D and high parathyroid hormone concentrations as determinants of loss of muscle strength and muscle mass (sarcopenia): The Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 88, 5766–72 (2003). [DOI] [PubMed] [Google Scholar]
- Saleh F. N., Schirmer H., Sundsfjord J. & Jorde R. Parathyroid hormone and left ventricular hypertrophy. Eur Heart J. 24, 2054–60 (2003). [DOI] [PubMed] [Google Scholar]
- Jiang Q., Dibra F., Lee M. D., Oldenburg R. & Uitto J. Overexpression of Fetuin-A counteracts ectopic mineralization in a mouse model of pseudoxanthoma elasticum (abcc6(−/−)). J Invest Dermatol. 130, 1288–96 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto J. et al. Accelerated growth plate mineralization and foreshortened proximal limb bones in fetuin-a knockout mice. PLOS ONE. 7, e47338 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal D. et al. Fetuin-A acts as an endogenous ligand of TLR4 to promote lipid-induced insulin resistance. Nat Med. 18, 1279–85 (2012). [DOI] [PubMed] [Google Scholar]
- Lorant D. P. et al. Fetuin-A concentrations are increased in participants with type 2 diabetes and peripheral arterial disease. Diabetes Care. 34, 156–61 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou H. Y., Wu H. T., Hung H. C., Yang Y. C., Wu J. S. & Chang C. J. Endoplasmic reticulum stress induces the expression of Fetuin-A to develop insulin resistance. Endocrinology. 153, 2974–84 (2012). [DOI] [PubMed] [Google Scholar]
- Ix J. H. et al. Health Aging and Body Composition Study. Fetuin-A and change in body composition in older persons. J Clin Endocrinol Metab 94, 4492–8 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merx M. W. et al. Myocardial stiffness, cardiac remodeling, and diastolic dysfunction in calcification-prone Fetuin-A-deficient mice. J Am Soc Nephrol. 16, 3357–64 (2005). [DOI] [PubMed] [Google Scholar]
- Chang W. T. et al. Fetuin-A as a predicator of sarcopenic left ventricular dysfunction. Sci Rep. 5, 12078 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S. et al. Cardiomyocyte-specific deletion of the vitamin D receptor gene results in cardiac hypertrophy. Circulation. 124, 1838–47 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlüter K. D. & Piper H. M. Cardiovascular actions of parathyroid hormone and parathyroid hormone-related peptide. Cardiovasc Res. 37, 34–41 (0998). [DOI] [PubMed] [Google Scholar]
- Cha H. et al. Parathyroid hormone accelerates decompensation following left ventricular hypertrophy. Exp Mol Med. 42, 61–8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deo R. et al. Vitamin D, parathyroid hormone, and sudden cardiac death: Results from the Cardiovascular Health Study. Hypertension. 58, 1021–8 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim P. et al. Usefulness of Fetuin-A and C-reactive protein concentrations for prediction of outcome in acute coronary syndromes. Am J Cardiol. 111, 31–7 (2013). [DOI] [PubMed] [Google Scholar]
- Weikert C. et al. Plasma Fetuin-A concentrations and the risk of myocardial infarction and ischemic stroke. Circulation. 118, 2555–62 (2008). [DOI] [PubMed] [Google Scholar]
- Sinha A., Hollingsworth K. G., Ball S. & Cheetham T. Improving the vitamin D status of vitamin D deficient adults is associated with improved mitochondrial oxidative function in skeletal muscle. J Clin Endocrinol Metab. 98, E509–13 (2013). [DOI] [PubMed] [Google Scholar]
- Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: Consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 22, 477–501 (2001). [DOI] [PubMed] [Google Scholar]
- Chang W. T., Chen J. S., Hung Y. K., Tsai W. C., Juang J. N. & Liu P. Y. Characterization of aging-associated cardiac diastolic dysfunction. PLOS ONE. 9, e97455 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai D. F., Chen T., Johnson S. C., Szeto H. & Rabinovitch P. S. Cardiac aging: From molecular mechanisms to significance in human health and disease. Antioxid Redox Signal. 15, 1492–1526 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosato M., Zamboni V., Ferrini A. & Cesari M. The aging process and potential interventions to extend life expectancy. Clin Interv Aging. 2, 401–12 (2007). [PMC free article] [PubMed] [Google Scholar]
- Anversa P., Hiler B., Ricci R., Guideri G. & Olivetti G. Myocyte cell loss and myocyte hypertrophy in the aging rat heart. J Am Coll Cardiol. 8, 1441–8 (1986). [DOI] [PubMed] [Google Scholar]
- Lang R. M. et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 18, 1440–63 (2005). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


