Abstract
Hepatitis C virus (HCV) infection has also been associated with many extrahepatic manifestations including the development of B-cell non-Hodgkin's lymphoma (NHL). Primary pancreatic lymphoma is very rare and comprises 2.2% of NHL and 4.9% of all pancreatic malignancies. Our patient was a woman with a history of infection with HCV found to have a mass in the head of the pancreas. Biopsy of the mass revealed a high-grade B-cell lymphoma consistent with Burkitt's lymphoma. Our case reflects a need to initiate antiviral therapy for all patients infected with HCV even in early stages of fibrosis to prevent cirrhosis and other extrahepatic manifestations of infection with HCV.
Background
Chronic infection with hepatitis C virus (HCV) has been shown to progress to cirrhosis in 20% of cases. HCV, a single-stranded positive-sense RNA virus, can replicate in peripheral blood mononuclear cells resulting in the development of lymphoproliferative disorders. Chronic HCV infection has been associated with many extrahepatic manifestations including the development of B-cell non-Hodgkin's lymphoma (NHL). Primary pancreatic lymphoma is very rare and comprises 2.2% of NHL and 4.9% of all pancreatic malignancies.1 We report a patient with early stage HCV infection who developed and died of complications from a primary pancreatic lymphoma.
Case presentation
The patient was a woman with a history of infection with HCV, who presented with jaundice and dyspepsia. She had a history of hepatitis C-genotype 1b awaiting interferon-free therapy. Her liver biopsy was consistent with grade 1 inflammation and stage 1–2 fibrosis. Her HCV viral load was 3 962 429 IU/mL.
She presented with abdominal distension, nausea, pruritus and jaundice. On physical examination, she had scleral icterus and a palpable abdominal mass. US scan of the abdomen revealed a hypoechoic mass (figure 1). CT of the abdomen revealed a large solid mass in the head of the pancreas extending to or involving the hilum of the liver. The mass measured 7.5×4.9×12.7 cm (figures 2 and 3). Her laboratory tests showed T. Bili 10.0 mg/dL, D. Bili 5.8 mg/dL, alkaline phosphatase (ALP) 160 U/L, aspartate transaminase (AST) 216 U/L, alanine transaminase (ALT) 166 U/L, alpha-fetoprotein (AFP) 2.1 IU/mL, carcinoembryonic antigen (CEA) 1.0 ng/mL and cancer antigen (CA) 19–9 46 U/mL. After a failed endoscopic retrograde cholangiopancreatography (ERCP), the patient underwent placement of internal and external biliary drains by the interventional radiologist. A core biopsy of the mass through ERCP revealed a high-grade B-cell lymphoma consistent with Burkitt's lymphoma with cells positive for CD20, CD10 and Bcl-6. Ki-67 was displayed with a proliferation index >95%. The morphological and immunohistochemical features are diagnostic for a high-grade B-cell lymphoma and most consistent with Burkitt's lymphoma. The patient underwent two cycles of chemotherapy with rituximab and EPOCH. Unfortunately, her disease process was complicated by tumour lysis syndrome, ascites, delirium, anasarca and pneumonia, and the patient expired.
Figure 1.

Abdominal US image showing a hypoechoic mass measuring 2.6×1.9×2.8 cm in the pancreas.
Figure 2.

CT abdomen showing a periportal solid 7.5×4.9×12.7 cm mass obstructing the central hepatic ducts, encasing the main portal vein and multiple smaller venous branches.
Figure 3.
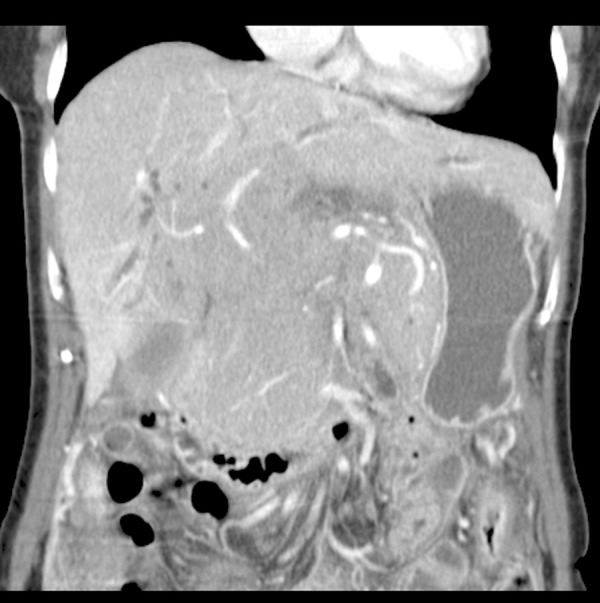
Coronal view of pancreatic mass in the abdomen.
Discussion
According to the analysis of the National Health and Nutrition Examination Survey (NHANES) database, it has been estimated that 2.7 million US residents suffer from chronic hepatitis C (CHC). CHC can progress to cirrhosis, hepatocellular carcinoma and various other extrahepatic diseases. In this case, our patient had early stage disease, F1–F2, and was awaiting interferon-free therapy because of the complications associated with interferon treatment. She developed a rare pancreatic lymphoma even before significant liver disease developed. She had a long-standing history of infection with HCV before development of her pancreatic lymphoma. This case discusses the importance of treatment at early stages of fibrosis in patients with hepatitis C in order to prevent lymphoma and other potential extrahepatic manifestations, such as diabetes, cryoglobulinemia, renal disease and, in this case, lymphoma.2 Our patient met the criteria for primary pancreatic lymphoma which includes no palpable superficial lymphadenopathy, no enlargement of mediastinal lymph nodes on chest radiograph, a normal leucocyte count and a pancreatic mass that predominates with grossly involved lymph nodes confined to the peripancreatic region and lack of hepatic or splenic involvement.3 4
There have been a few studies to suggest an association between HCV and pancreatic cancer. Takagi et al5 and Ghobakhlou et al1 also showed cases of patients with CHC who developed a pancreatic malignancy. One study by Huang et al showed that with 340 819 person-years in the HCV cohort, 34 pancreatic cancers were identified. The population-based cohort study demonstrated that the risk of pancreatic cancer was doubled in patients with HCV infection compared with the general Swedish population.6 The association between HCV infection and pancreatic cancer remains unclear, but prior evidence has shown that the pancreas is a remote location for hepatitis virus inhabitation and replication.7 It can be perceived that HCV serves as a biological agent that may indirectly contribute to inflammation-associated carcinogenesis in the pancreas. It has been postulated that HCV can induce an increase in growth factors and cytokines, which may affect various genes and promote cancer cell growth and proliferation.5
Primary pancreatic lymphoma tends to affect patients in the sixth decade of life and usually presents as a circumscribed, large solitary mass involving the pancreatic head.8 Signs and symptoms associated with primary pancreatic lymphoma include abdominal distension, a palpable mass, nausea, vomiting, diarrhoea, weight loss, haematemesis and ascites. It usually appears hypoechoic on endoscopic ultrasound scan and hypodense on CT. Treatment of choice for a primary pancreatic lymphoma is chemotherapy. Improved outcomes have been noted with aggressive combination chemotherapy regimens, which include rituximab.9
Recent extraordinary advances have been made in antiviral therapy for the treatment of HCV infection. Many times, patients are only treated if they have advanced liver disease, thereby restricting therapy to F3–F4 disease or even cirrhosis alone. Early treatment of patients with HCV is imperative as the efficacy of treatment declines with advancing stages of hepatic fibrosis or decompensated cirrhosis. In fact, patients with hepatocellular carcinoma or hepatic decompensation are less likely to benefit from antiviral therapy. Patients who are not treated early can progress to cirrhosis and decompensation of the liver which leads to complications such as ascites, variceal haemorrhage, hepatorenal syndrome, hepatopulmonary syndrome and encephalopathy. These complications all lead to an increased cost of hospitalisation. A recent study reported that patients with sustained virologic response after antiviral therapy had about a 2.45 times lower liver-related hospitalisations than those without maintained virologic response. Therefore, in order to decrease the burden of hospital costs, there should be efforts to screen high-risk populations and administer appropriate timely treatments.10
Learning points.
Our case reflects a patient whose survival may have been impacted had she been cured of her HCV infection. Although the patient only presented with stage 1-2 fibrosis, she nevertheless went on to develop an extrahepatic lymphoproliferative disorder that progressed to a rare pancreatic lymphoma.
Studies suggest that treatment of non-Hodgkin's lymphoma with antiviral therapy for HCV can lead to a regression of lymphoproliferative disease. Following successful antiviral therapy, HCV-infected persons with non-Hodgkin's lymphoma and other lymphoproliferative disorders can achieve complete or partial remission in up to 75% of cases.
Consequently, there is a need to initiate antiviral therapy for all HCV patients, even during the early stages of fibrosis, in order to prevent cirrhosis and other extrahepatic manifestations of HCV infection such as pancreatic Burkitt's lymphoma as seen in our patient. This underscores the importance of treating all patients with HCV regardless of the severity of liver fibrosis.
Footnotes
Contributors: VHB and TS wrote and revised the manuscript together. TS is the attending on the case.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ghobakhlou M, Mohammad Alizadeh AH, Naderi N et al. . A patient with chronic hepatitis C and a pancreatic mass in endoscopic ultrasound. Case Rep Gastroenterol 2012;6:387–93. 10.1159/000339693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tandon N, Balart LA, Laliberté F et al. . Impact of completing chronic hepatitis C (CHC) treatment on post-therapy healthcare cost. J Med Econ 2014;17:862–71. 10.3111/13696998.2014.964720 [DOI] [PubMed] [Google Scholar]
- 3.Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961;49:80–9. 10.1002/bjs.18004921319 [DOI] [PubMed] [Google Scholar]
- 4.Behrns KE, Sarr MG, Strickler JG. Pancreatic lymphoma: is it a surgical disease? Pancreas 1994;9:662–7. 10.1097/00006676-199409000-00019 [DOI] [PubMed] [Google Scholar]
- 5.Takagi K, Nishikawa S, Nagasaka A et al. . [Malignant lymphoma of the pancreas with chronic hepatitis C]. Nihon Shokakibyo Gakkai Zasshi 2004;101:1227–31. [PubMed] [Google Scholar]
- 6.Huang J, Magnusson M, Törner A et al. . Risk of pancreatic cancer among individuals with hepatitis C or hepatitis B virus infection: a nationwide study in Sweden. Br J Cancer 2013;109:2917–23. 10.1038/bjc.2013.689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hassan MM, Li D, El-Deeb AS et al. . Association between hepatitis B virus and pancreatic cancer. J Clin Oncol 2008;26:4557–62. 10.1200/JCO.2008.17.3526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khashab M, Mokadem M, DeWitt J et al. . Endoscopic ultrasound-guided fine-needle aspiration with or without flow cytometry for the diagnosis of primary pancreatic lymphoma—a case series. Endoscopy 2010;42:228–31. 10.1055/s-0029-1243859 [DOI] [PubMed] [Google Scholar]
- 9.Tuchek JM, De Jong SA, Pickleman J. Diagnosis, surgical intervention, and prognosis of primary pancreatic lymphoma. Am Surg 1993; 59:513–18. [PubMed] [Google Scholar]
- 10.Luo R, Greenberg A, Stone CD. Increasing volume but decreasing mortality of hospitalized hepatitis C patients in the United States, 2005 to 2011. J Clin Gastroenterol 2015;49:620–7. 10.1097/MCG.0000000000000216 [DOI] [PubMed] [Google Scholar]
- 11.Visco C, Finotto S. Hepatitis C virus and diffuse large B-cell lymphoma: pathogenesis, behavior and treatment. World J Gastroenterol 2014; 20:11054–61. 10.3748/wjg.v20.i32.11054 [DOI] [PMC free article] [PubMed] [Google Scholar]


