Abstract
Cephalic tetanus is defined as a combination of trismus and paralysis of one or more cranial nerves. Since it is a rare cause of facial nerve palsy, it is often overlooked as a differential diagnosis. We present the case of a 75-year-old man admitted to our emergency department with left facial nerve palsy, left ptosis and dysphagia 2 weeks after a head laceration. Soon after admission, he was orally intubated because of massive aspiration. A delayed diagnosis of cephalic tetanus was reached only when he was extubated and trismus and risus sardonicus were identified in addition to facial nerve palsy. The patient was re-intubated and successfully extubated on day 20 postadmission. In orally intubated patients, trismus and risus sardonicus may be overlooked, and although rare, cephalic tetanus should be considered to be a differential diagnosis of facial nerve palsy.
Background
Facial nerve palsy has various aetiologies.1 2 Cephalic tetanus is defined as a combination of trismus and paralysis of one or more cranial nerves.3 Although the facial nerve is involved in most cases of cephalic tetanus, cephalic tetanus is rarely considered to be a cause of facial nerve palsy. Here we report a case of delayed diagnosis of cephalic tetanus in which facial nerve palsy was present on admission but the identification of trismus was difficult because of oral intubation.
Case presentation
A 75-year-old man fell off a fence and suffered from a scalp laceration, which required suturing. He experienced left ptosis 2 days after the injury and left facial palsy and dysphagia 13 days after the injury. He presented to our emergency department 15 days after the injury. A physical examination revealed stiffness in the neck, left peripheral facial nerve palsy and left ptosis but no limb muscle weakness or depressed deep tendon reflexes.
Investigations
Results of complete blood count and biochemical analysis were within normal limits.
Brain CT and MRI showed no abnormal findings. His cerebrospinal fluid examination revealed no white cell count and normal levels of protein (49 mg/dL) and glucose (106 mg/dL).
Differential diagnosis
The most important differential diagnoses in a patient with facial nerve palsy are stroke and encephalitis/meningitis. Imaging and cerebrospinal tests ruled out these entities.
A diagnosis of Bell's palsy was considered, but ptosis and dysphagia are not its typical presentations.
Although the patient lacked limb muscle weakness, Guillain-Barré syndrome was suspected as it can cause paralysis of the facial and bulbar muscles.
Treatment
Soon after admission, the patient experienced massive aspiration and was orally intubated. Muscle relaxants were not required to open the patient's mouth for the intubation procedure. Guillain-Barré syndrome was suspected and intravenous immunoglobulin treatment was administered; however, this did not result in the improvement of symptoms.
The patient was extubated 24 days after the injury, at which point, he could not open his mouth to more than the width of a finger. He also experienced risus sardonicus resulting from facial muscle spasms, which led to a diagnosis of cephalic tetanus (figure 1). A culture from his head wound identified Gram-positive bacilli consistent with Clostridium tetani (figure 2). The patient was re-intubated because of severe dysphagia, and penicillin G and human tetanus immunoglobulin were administered.
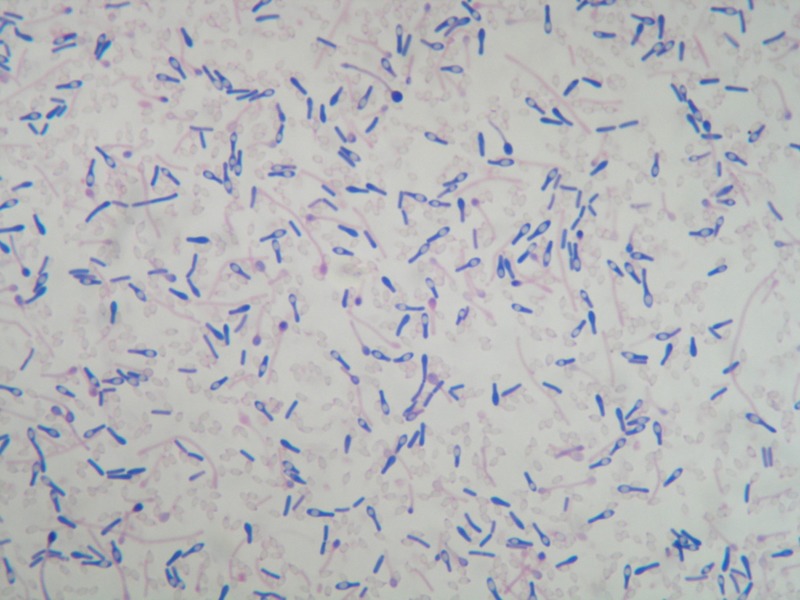
Figure 1.

Trismus, risus sardonicus, weakness and difficulty in moving the left eyebrow were observed at the first extubation 24 days after injury.
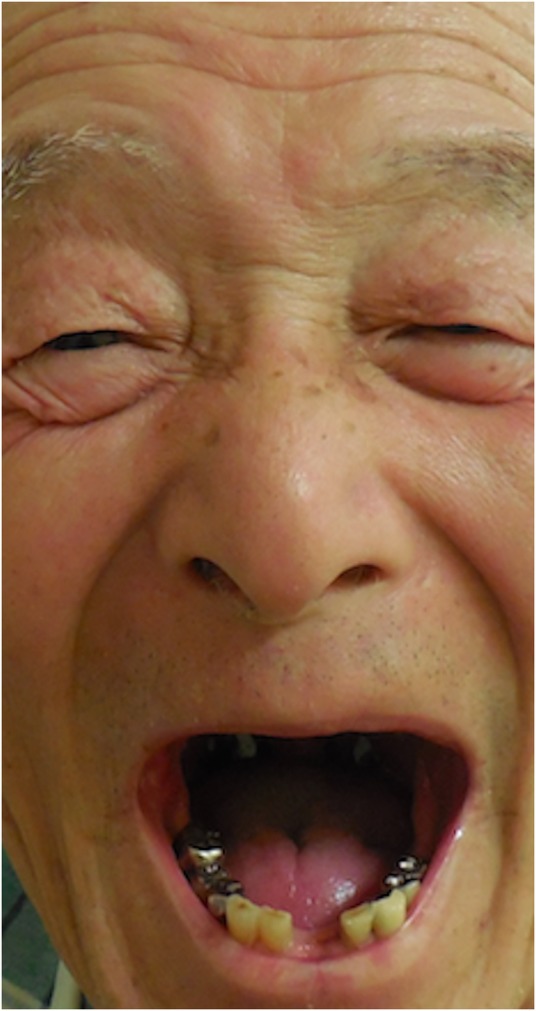
Figure 2.
Gram-positive bacilli with a drumstick or tennis racquet appearance, producing spherical terminal spores, obtained from the patient's head wound.
Outcome and follow-up
He was successfully extubated on day 35 and discharged on day 69 after the injury without any neurological sequela (figure 3).
Figure 3.
The patient at 66 days after injury, showing full resolution of symptoms.
Discussion
The delayed diagnosis of cephalic tetanus in this case suggests two important clinical issues.
First, although rare, cephalic tetanus should be prioritised and included in clinical guidelines as a differential diagnosis of facial nerve palsy. Cephalic tetanus is defined as a combination of trismus and paralysis of one or more cranial nerves and accounts for only 0.9–3.0% of all tetanus cases. The facial nerve is most commonly involved in cephalic tetanus.3 At present, a clinical practice guideline and a review article on Bell's palsy1 2 4 outline differential diagnoses of facial nerve palsy as diabetic neuropathy, facial nerve tumour, Guillain-Barré syndrome, leprosy, Lyme disease, multiple sclerosis, otitis media, polyarteritis nodosa, sarcoidosis, stroke and syphilis. Cephalic tetanus is not included in this list. In emergency department settings, it is important to immediately consider, and if appropriate, rule out stroke and encephalitis/meningitis in patients with facial nerve palsy. After ruling these out, cephalic tetanus is the diagnosis requiring the most urgent intervention because of its high-mortality risk. Two-thirds of cephalic tetanus cases develop generalised tetanus, with an overall mortality rate of 15–30%.
It is important to be aware that in the course of cephalic tetanus, trismus can occur before, concurrently with or after facial nerve palsy. Although trismus is known to appear before or concurrently with facial nerve palsy,5 there have been recent reports in which it has occurred after facial nerve palsy.6–8 Since trismus is a key symptom of cephalic tetanus, a delay in identifying trismus in a patient with facial nerve palsy may cause a delay in proper diagnosis.
Second, clinicians may overlook trismus and risus sardonicus in orally intubated patients. A review of why trismus and risus sardonicus were not identified while the patient was intubated revealed that this was due to the partial concealment of the patient's face by the device used to secure the tracheal tube. After intubation, the tracheal tube is secured in place using a device such as an adhesive tape, a cloth tape or a specific commercial device. Our hospital uses an Anchor Fast Oral Endotracheal Tube Fastener (Hollister Incorporated, Libertyville, Illinois, USA) for patients requiring intubation longer than 2 days. This device has the advantage of reducing ventilator-associated pneumonia and oral pressure ulcers caused by oral intubation.9 10 However, it also partially conceals the patient's cheeks, nose and mouth. Thus, clinicians may not be able to see and identify symptoms such as trismus and risus sardonicus in orally intubated patients if such types of tracheal tube securing devices are used.
In conclusion, trismus and risus sardonicus are key symptoms of cephalic tetanus, but they may be overlooked in orally intubated patients. Cephalic tetanus is a rare but serious cause of facial nerve palsy and should be prioritised as a differential diagnosis of facial nerve palsy.
Learning points.
Cephalic tetanus is a combination of trismus and paralysis of one or more cranial nerves.
Although cephalic tetanus is an uncommon cause of facial nerve palsy, the facial nerve is most commonly involved in cephalic tetanus; therefore, cephalic tetanus should be included as a differential diagnosis of facial nerve palsy.
Physicians may overlook trismus and risus sardonicus in orally intubated patients.
Footnotes
Contributors: YK, KK and SO wrote and edited the manuscript. TT supervised the writing of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Baugh RF, Basura GJ, Ishii LE et al. . Clinical practice guideline: Bell's Palsy executive summary. Otolaryngol Head Neck Surg 2013;149:656–63. 10.1177/0194599813506835 [DOI] [PubMed] [Google Scholar]
- 2.Tiemstra JD, Khatkhate N. Bell's palsy: diagnosis and management. Am Fam Physician 2007;76:997–1002. [PubMed] [Google Scholar]
- 3.Jagoda A, Riggio S, Burguieres T. Cephalic tetanus: a case report and review of the literature. Am J Emerg Med 1988;6:128–30. 10.1016/0735-6757(88)90049-6 [DOI] [PubMed] [Google Scholar]
- 4.Murthy JM, Saxena AB. Bell's palsy: treatment guidelines. Ann Indian Acad Neurol 2011;14(Suppl 1):S70–2. 10.4103/0972-2327.83092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayo J, Berciano J. Cephalic tetanus presenting with Bell's palsy. J Neurol Neurosurg Psychiatr 1985;48:290 10.1136/jnnp.48.3.290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doshi A, Warrell C, Dahdaleh D et al. . Just a graze? Cephalic tetanus presenting as a stroke mimic. Pract Neurol 2014;14:39–41. 10.1136/practneurol-2013-000541 [DOI] [PubMed] [Google Scholar]
- 7.Seo DH, Cho DK, Kwon HC et al. . A case of cephalic tetanus with unilateral ptosis and facial palsy. Ann Rehabil Med 2012;36:167–70. 10.5535/arm.2012.36.1.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gleeson T, Etienne M. Cranial nerve VII palsy as the first sign of cephalic tetanus after an earthquake. Arch Neurol 2011;68:536–7. 10.1001/archneurol.2011.55 [DOI] [PubMed] [Google Scholar]
- 9.Zaratkiewicz S, Teegardin C, Whitney JD. Retrospective review of the reduction of oral pressure ulcers in mechanically ventilated patients: a change in practice. Crit Care Nurs Q 2012;35:247–54. 10.1097/CNQ.0b013e3182542de3 [DOI] [PubMed] [Google Scholar]
- 10.Garcia R, Jendresky L, Colbert L et al. . Reducing ventilator-associated pneumonia through advanced oral-dental care: a 48-month study. Am J Crit Care 2009;18:523–32. 10.4037/ajcc2009311 [DOI] [PubMed] [Google Scholar]


