Abstract
Objective:
The aim of this study is to evaluate the effect of slice thickness on the visibility of inferior alveolar canal (IAC) in cone-beam computed tomography (CBCT) images.
Materials and Methods:
CBCT images of thirty patients (15 male and 15 female) with an age range between 40–50 years old were used. Cross-sectional images were obtained with 0.5, 1, and 2 mm slice thickness and 2 mm interval. Two oral radiologists with at least 5 years' of experience observed all of the 90 images and rated the images based on the visibility of IAC in a 4-score classification (highly visible, visible, nearly visible, nearly invisible). Friedman test was used for the comparison of visibility of IAC in different slice thicknesses. To do the above test, the average of the scores of two examiners was calculated. A P. value below 0.05 was considered significant.
Results:
Visibility of IAC in different slice thicknesses of both raters showed no significant difference (P = 0.20).
Conclusion:
Within the limitations of this study the slice thickness has no effect on visibility of IAC in cross-sectional images. Future studies on other multiplanar images are recommended.
Key Words: Cone beam computed tomography, cross, inferior alveolar nerve, section
INTRODUCTION
Successful dental surgery needs complete information about regional anatomy. Some of the surgical procedures including insertion of dental implants, mandibular third molar surgery, osteotomy, and other surgeries close to inferior alveolar canal (IAC) require assessment of IAC to prevent injuries to neurovascular bundles.[1] Mandibular canal is one of the most important anatomic structure due to its content and risk of damage during surgery. This is more critical in atrophic ridges in premolar and molar area. In conventional radiographic images, IAC could be seen as a radiolucent line with two thin cortical borders. In some osteoporotic mandibles detection of IAC may be difficult due to its lack of well-defined cortical boundaries. Panoramic is a widely used technique for tracing IAC and estimating its position in vertical dimension.[2,3] In the late 1990s, cone-beam computed tomography (CBCT) was introduced to dentistry which provided more sharpness.[2] Linear measurements in CBCT are accurate enough for implant surgery.[3,4] CBCT images are useful for evaluating IAC and its position three-dimensionally, considering tooth roots, and alveolar crest. Furthermore, abnormal mandibular canals like branched canals can be identified by CBCT. This technology facilitates the evaluation of IAC due to its cross-sectional images which overcome the weak points of conventional images.[5] Various parameters influence the characteristics of CBCT image, such as field of view, slice interval, and tube current. One of the parameters which may affect the visibility of anatomic structures like IAC is the slice thickness. There is a common belief in multi-detector computed tomography (MDCT) that thin slices make better images.[6] It is known that thinner slices provide less partial volume averaging and better image quality with more detailed visibility.[7] The aim of this study is to evaluate the effect of slice thickness on visibility of IAC in CBCT images.
MATERIALS AND METHODS
We used CBCT archive in the Oral and Maxillofacial Department of Radiology, Tehran University of Medical Sciences, Tehran, Iran. CBCT images of 30 patients (15 male and 15 female) with age range between 40 and 60 years old were used. Imaging was performed by Alphard VEGA (Asahi Roentgen, Japan). Peak kilovoltage and mA was 80 and 4, respectively for all samples. The images were processed using Neo 3D software Version 2.01 (Asahi Roentgen, Japan) and cross-sectional images were prepared by 0.5, 1, and 2 mm slice thicknesses and 2 mm interval. Default thickness of cross-sectional images in the software was 1 mm, and we selected half and double thicknesses of default. All of the 90 images were coded and saved in joint photographic experts format [Figures 1–3]. Two oral radiologists with at least 5 years of experience observed images randomly and blindly using 19˝ LCD monitor (Samsung, SyncMaster P23700). They rated the images based on the visibility of IAC in a 4-score classification (highly visible, visible, nearly visible, nearly invisible). For the second time, all images were rated 10 days later with different codes.
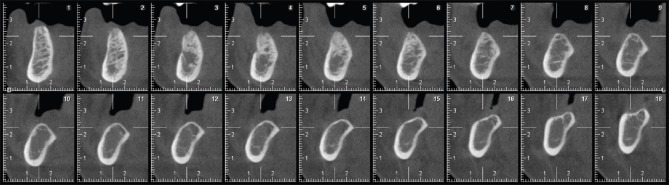
Figure 1.
Cross sectional image, 0.5 mm thickness.
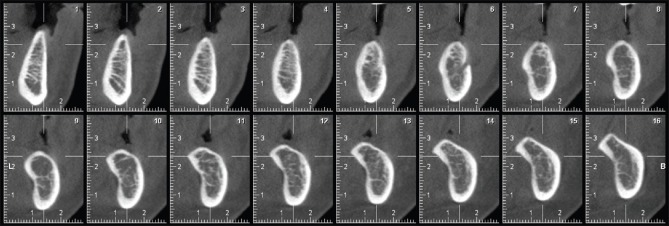
Figure 3.
Cross sectional image, 2 mm thickness.
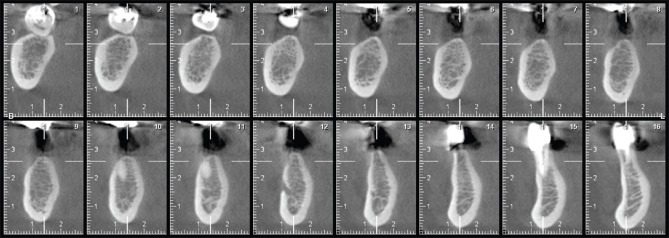
Figure 2.
Cross sectional image,1 mm thickness.
Intraclass correlation coefficient (ICC with two-way random model and absolute agreement type) was performed to evaluate inter- and intra-observer agreement. We found favorable agreement considering the resulted ICC [Tables 1–3].
Table 1.
Inter-observer reliability in different slice thickness
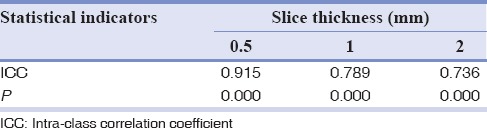
Table 3.
Intra-observer reliability in different slice thickness (Observer 2)

Table 2.
Intra-observer reliability in different slice thickness (Observer 1)

Statistical analysis
SPSS for Windows Version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY, USA) was used. Friedman test was used for the comparison of visibility of IAC as an ordinal variable in different slice thicknesses. To do the above test, the average of the scores of two raters was calculated. A P value below 0.05 was considered significant.
RESULTS
Visibility of IAC in different slice thicknesses of both raters had no significant difference (P = 0.20) [Table 4].
Table 4.
Visibility of inferior alveolar canal in different slice thickness
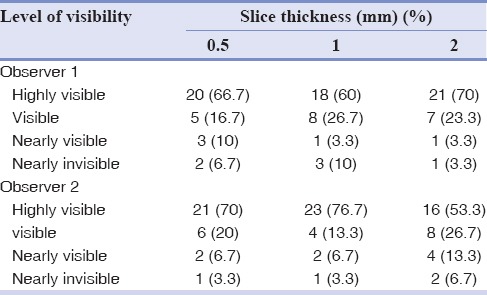
Our result demonstrates that 53.3% of images in females were highly visible, compared with 80% of images in males. Samples were not adequate to compare males and females.
DISCUSSION
Image quality is a subjective interpretation of visual data and does not have an exact definition. An image should have enough information to obtain a clinical decision. The aim of our study was to evaluate the effect of slice thickness of CBCT images on the visibility of IAC. IAC is one of the most important anatomical structure of mandible due to its content, including inferior alveolar nerve, artery, and vein. It is critical to consider the location and variations of IAC, especially in atrophic ridges before implant installation.[8]
CBCT machine provides perfect images with low dose and cost, compared to MDCT.[9] There is a wide variety of specification of CBCT machines which are used with different acceptable images and exposure doses.[10] One of the parameters which can be altered in CBCT to affect the image quality is slice thickness.[11] There have been few researches about the efficacy of slice thickness of CBCT and its effect on visibility of anatomical structure.
In our study, there was no significant difference between visibility of IAC in different slice thicknesses and any attempt to change slice thickness did not cause better visualization of IAC in cross-sectional images.
Any change in slice thickness either increasing or decreasing may affect subject's contrast and visibility. In the present research, the subject contrast of IAC was not affected by the thickness of cross-sectional images. It may be due to the favorable contrast in well-corticated IACs so that good visibility of IAC was not influenced by slice thickness. On the other hand, ill-defined IAC has low contrast and may be mistaken with surrounding bone marrow space, to an extent that altering the thickness is of no benefit to its visibility.
There are some other researches with different methods which concluded positive effect of slice thickness. Sezgin et al. evaluated the effect of slice thickness on volumetric calculation of CBCT, showing that estimated volumes of intrabony lesions did not change with different slice thicknesses.[12] Jia et al. studied the effect of slice thickness of CBCT on the precision of image-guided radiotherapy. They showed that slice thickness has no significant effect on positioning precision.[13]
Similar research was done in MDCT with different methods and results. Mühler et al. studied the accuracy and reliability of age estimation, using clavicular epiphyseal plate in forensic medicine. In their study, the best result was obtained with slice thickness of 1 mm.[14] Dogan evaluated the effect of heart rate and slice thickness on volumetric analysis of CT images of cardiac phantom and concluded that slice thickness of 2 and 8 mm have the same diagnostic value.[15] Guggenbuhl et al. studied microstructure of tibia in CT and concluded that increasing the slice thickness will result in lower accuracy of tissue analysis parameters.[16] In another research, Rubinstein et al. noticed that the diagnostic accuracy of fractures in odontoid process will increase with 1 mm section thickness.[17] Jung et al. studied the multiplanar reformation using 1.25, 2.5, 3.75, and 5 mm slice thicknesses for quantitative measurement in CT and demonstrated that thinner slice thicknesses result in better image quality.[18] Sirin studied diagnostic accuracy of reconstructed CBCT images, using different slice thicknesses, in detection of simulated mandibular condylar fracture. They concluded that the diagnosis will be more accurate using slice thickness of 0.2 and 1 mm, compared to 2 and 3 mm.[19]
CONCLUSION
Our study showed that slice thickness has no effect on visibility of IAC in cross-sectional images. Tracing ill-defined IACs can be achieved by other multiplanar images, such as panoramic or axial view; also nerve tracing tools in software's used for CBCT might be useful. Further studies with different methodology may be useful to achieve more results.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
REFERENCES
- 1.Denio D, Torabinejad M, Bakland LK. Anatomical relationship of the mandibular canal to its surrounding structures in mature mandibles. J Endod. 1992;18:161–5. doi: 10.1016/S0099-2399(06)81411-1. [DOI] [PubMed] [Google Scholar]
- 2.Panmekiate S, Apinhasmit W, Petersson A. Effect of electric potential and current on mandibular linear measurements in cone beam CT. Dentomaxillofac Radiol. 2012;41:578–82. doi: 10.1259/dmfr/51664704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: A cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:e420–5. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang X, Lambrichts I, Sun Y, Denis K, Hassan B, Li L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and Multi-Slice CT (MSCT).Part II: On 3D model accuracy. Eur J Radiol. 2010;75:270–4. doi: 10.1016/j.ejrad.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Asaumi R, Kawai T, Sato I, Yoshida S, Yosue T. Three-dimensional observations of the incisive canal and the surrounding bone using cone-beam computed tomography. Oral Radiol. 2010;26:20–8. [Google Scholar]
- 6.Richards PJ. Cervical spine clearance: A review. Injury. 2005;36:248–69. doi: 10.1016/j.injury.2004.07.027. [DOI] [PubMed] [Google Scholar]
- 7.Whyms BJ, Vorperian HK, Gentry LR, Schimek EM, Bersu ET, Chung MK. The effect of computed tomographic scanner parameters and 3-dimensional volume rendering techniques on the accuracy of linear, angular, and volumetric measurements of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:682–91. doi: 10.1016/j.oooo.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feifel H, Riediger D, Gustorf-Aeckerle R. High resolution computed tomography of the inferior alveolar and lingual nerves. Neuroradiology. 1994;36:236–8. doi: 10.1007/BF00588141. [DOI] [PubMed] [Google Scholar]
- 9.Scarfe WC. Imaging of maxillofacial trauma: Evolutions and emerging revolutions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(2 Suppl):S75–96. doi: 10.1016/j.tripleo.2005.05.057. [DOI] [PubMed] [Google Scholar]
- 10.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int J Oral Maxillofac Surg. 2009;38:609–25. doi: 10.1016/j.ijom.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 11.Hassan B, Couto Souza P, Jacobs R, de Azambuja Berti S, van der Stelt P. Influence of scanning and reconstruction parameters on quality of three-dimensional surface models of the dental arches from cone beam computed tomography. Clin Oral Investig. 2010;14:303–10. doi: 10.1007/s00784-009-0291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sezgin OS, Kayipmaz S, Sahin B. The effect of slice thickness on the assessment of bone defect volumes by the Cavalieri principle using cone beam computed tomography. J Digit Imaging. 2013;26:115–8. doi: 10.1007/s10278-012-9480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jia MX, Zhang X, Li N, Han CB. Impact of different CBCT imaging monitor units, reconstruction slice thicknesses, and planning CT slice thicknesses on the positioning accuracy of a MV-CBCT system in head-and-neck patients. J Appl Clin Med Phys. 2012;13:3766. doi: 10.1120/jacmp.v13i5.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mühler M, Schulz R, Schmidt S, Schmeling A, Reisinger W. The influence of slice thickness on assessment of clavicle ossification in forensic age diagnostics. Int J Legal Med. 2006;120:15–7. doi: 10.1007/s00414-005-0010-9. [DOI] [PubMed] [Google Scholar]
- 15.Dogan H, Veldkamp WJ, Dibbets-Schneider P, Spijkerboer AM, Mertens BJ, Kroft LJ, et al. Effects of heart rate, filling and slice thickness on the accuracy of left ventricular volume measurements in a dynamic cardiac phantom using ECG-gated MDCT. Br J Radiol. 2008;81:577–82. doi: 10.1259/bjr/92798700. [DOI] [PubMed] [Google Scholar]
- 16.Guggenbuhl P, Chappard D, Garreau M, Bansard JY, Chales G, Rolland Y. Reproducibility of CT-based bone texture parameters of cancellous calf bone samples: Influence of slice thickness. Eur J Radiol. 2008;67:514–20. doi: 10.1016/j.ejrad.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Rubinstein D, Escott EJ, Mestek MF. Computed tomographic scans of minimally displaced type II odontoid fractures. J Trauma. 1996;40:204–10. doi: 10.1097/00005373-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Jung H, Kim HJ, Kim DO, Hong SI, Jeong HK, Kim KD, et al. Quantitative analysis of three-dimensional rendered imaging of the human skull acquired from multi-detector row computed tomography. J Digit Imaging. 2002;15:232–9. doi: 10.1007/s10278-002-0031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sirin Y, Guven K, Horasan S, Sencan S, Bakir B, Barut O, et al. The influence of secondary reconstruction slice thickness on NewTom 3G cone beam computed tomography-based radiological interpretation of sheep mandibular condyle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:638–47. doi: 10.1016/j.tripleo.2010.05.053. [DOI] [PubMed] [Google Scholar]