Abstract
Chronic histiocytic intervillositis (CHI) is a rare placental lesion associated with adverse obstetric outcomes and high recurrence rate. We report a case of six consecutive pregnancies in one woman, where CHI was detected following an intrauterine death in the fifth pregnancy, after being missed in four earlier losses. The successful sixth pregnancy was treated with a combination of immunosuppressive and antithrombotic agents. While low-molecular-weight heparin (LMWH) and aspirin had been shown to improve pregnancy outcome in recurrent pregnancy loss, there was limited evidence of improved outcome in CHI. It has been suggested that CHI may result from a maternal immunological process and there have been a few reports of the use of corticosteroids because of this possibility, though without convincing evidence of efficacy. We too tried a corticosteroid, in combination with LMWH and aspirin. Comparative histopathological analysis of the placentae supported post-treatment effectiveness of our intervention strategy.
Background
Chronic histiocytic intervillositis (CHI), also known as chronic intervillositis, massive perivillous histiocytosis, massive chronic intervillositis or chronic intervillositis of unknown aetiology1–4 is a placental lesion associated with high fetal morbidity and mortality.
CHI was first described as a separate pathological entity in 19872 and clinicopathologically appears to overlap in some cases with villitis of unknown aetiology,5 6 although definitive criteria for the diagnosis of CHI have not been established. CHI can only be diagnosed following pathological examination of the placenta as peripheral blood tests such as alkaline phosphatase while often raised are non-specific.7
The incidence of CHI may vary with gestational age. The incidence in spontaneous first trimester miscarriages with normal karyotype has been reported at a higher incidence of up to 4.4%8 compared with 0.6% in second and third trimester placentae.3
The case reports published so far revealed a high recurrence rate in subsequent pregnancies, varying between 67 to 100%1 2 6 9 and high rates of perinatal mortality1 6 7 9 and growth restriction.1 10 In one study, only 18% of pregnancies reached 37 weeks gestation.1
As many of the reported recurrent pregnancies are lost at an early stage, or not examined pathologically, it has not been conclusively established that CHI is the exclusive lesion associated with these adverse outcomes. We report herein a case of six successive pregnancies in one woman with histological review of the placenta in the four pregnancies to progress beyond 10 weeks gestation. We also report for the first time, the pathological findings of the sixth (most recent) pregnancy which, post-treatment, resulted in a live birth.
Case presentation
We present the case of a 31-year-old with recurrent pregnancy loss and a medical history of pituitary microprolactinoma with secondary galactorrhoea, which was managed by regular consultation with an endocrinologist. She had been prescribed cabergoline 0.25 mg once daily to manage the galactorrhoea, which also regulated her menstrual cycle. Her medical history, prior to all pregnancies, included hypochromic microcytic anaemia (iron-deficiency), mild asthma and eczema. She was not taking cabergoline at the time of conception or during pregnancy. A high-grade smear had been treated by cervical transformation zone excision biopsy before she had become pregnant.
This woman was diagnosed with CHI following the loss of her fifth pregnancy at 27 weeks gestation, which had been complicated by mild preeclampsia and severe intrauterine fetal growth restriction. Preeclampsia was suspected when our patient presented with a raised blood pressure of 145/92 mm Hg (compared to 110/72 mm Hg at booking), and was found to have a raised urinary protein-creatinine ratio of 69. At the time, the rest of her blood tests; including liver function tests, urea, creatinine and electrolytes, and full blood count; were all normal apart from a mildly elevated alkaline phosphatase at 219. Estimated fetal size from ultrasound was not considered compatible with survival and after extensive monitoring intrauterine demise was detected at 27 weeks gestation and labour was induced. The couple agreed to proceed to postmortem examination and cytogenetic testing. The female fetus was growth restricted (<5th personalised growth centile) weighing 345 g and had no chromosomal or anatomical anomaly. CHI was diagnosed in the placenta.
Additional investigations including thrombophilia, infectious and autoimmune screens were all normal, with the exception of an elevated antinuclear antibody titre of 160 (fine speckled pattern). Lupus anticoagulant and anticardiolipin antibodies specifically, were undetectable.
Her obstetrics history is summarised in table 1 below.
Table 1.
Obstetric history
| Pregnancy number (year) | Maternal age | Pregnancy result and gestation | Comments | Placenta |
|---|---|---|---|---|
| 1 (2003) | 24 | Spontaneous miscarriage, 10 weeks | Expectant management | Not examined |
| 2 (2004) | 25 | Termination of pregnancy, first trimester | Expectant management | Not examined |
| 3 (2010) | 31 | Spontaneous miscarriage, 11 weeks | Surgically managed with dilation and curettage (D&C) | Initially reported as unremarkable. On review, the estimated involvement of the maternal space by macrophages was ∼50% |
| 4 (2011) | 32 | Intrauterine fetal demise (IUFD), 20 weeks | Medical management with misoprostol. Spontaneous passage of fetus but required D&C for the placenta | Initially reported as unremarkable. On review, the estimated involvement of the maternal space by macrophages was ∼40% |
| 5 (2012) | 33 | IUFD at 27 weeks of a female fetus weighing 345 g | Developed mild preeclampsia with severe fetal intrauterine growth restriction. Undergone induction of labour following IUFD | The placenta weighed 154 g and measured 120×90 mm by 20 mm in thickness. The cord was centrally inserted and non-coiled. Microscopically intervillous histiocytosis was associated with abundant perivillous fibrin deposition, and immature second trimester villi. The estimated involvement of the maternal space by macrophages was ∼30% |
| 6 (2013) | 34 | Healthy baby boy weighting 2200 g, with Apgars of 9 and 10 at 1 and 5 min respectively, delivered by elective caesarean section at 34 weeks | Managed with prednisone, enoxaparin, calcium and aspirin. Close monitoring with regular growth scans. Baby's growth plateaued between 32–34 weeks | Placenta reported as unremarkable, although pathologist unaware of previous diagnosis. On review, the estimated involvement of the maternal space by macrophages was minimal at ∼5%. The placenta weighed 348 g |
At diagnosis of CHI, the patient and obstetrician performed a literature search and together established contacts with experts via the CHI facebook page. Treatments options were discussed and their availability in New Zealand and safety were reviewed. In consult with a fetomaternal specialist from the University of Auckland, Dr Katie Groom, a management plan was put in place.
The mother provided signed informed consent and ethical approval was obtained from the NZ Health and Disabilities Multiregional Ethics and Lower Regional South Ethics Committees (LRS/09/09/038). Retrospective pregnancy placental samples were extracted, with patient permission, from case files. The placentae from the third, fourth, fifth and sixth pregnancies (11 weeks, 20 weeks, 27 weeks and 34 weeks gestation respectively) were available for review.
Treatment
The pregnancy was closely followed from conception with regular antenatal clinic reviews and fortnightly ultrasound scans. Medical management comprised of CHI targeted treatment including: prednisone 20 mg oral once daily from conception to 20 weeks, and then in decreasing dose to 28 weeks, and enoxaparin (low-molecular-weight heparin, LMWH) 40 mg subcutaneously once daily from 6 weeks. Aspirin (salicylic acid) 100 mg oral once daily was given for both the history of preeclampsia and as a CHI targeted treatment. She was also given calcium 1.2 g oral once daily due to her history of preeclampsia, and was taking Ferrotab (200 mg ferrous fumarate) once daily for her iron-deficient anaemia. She was also given monthly vitamin D from 12 weeks, and was taking folic acid 5 mg once daily and two tablets of an over-the-counter vitamin preparation per day for the duration of the pregnancy for her general health.
This sixth pregnancy was complicated by the development of a constant frontal headache early in the second trimester. An MRI showed mild increase in size of the pituitary microprolactinoma, as expected in pregnancy, but was thought to be an unlikely cause of her headache. On further investigations, a diagnosis of idiopathic intracranial hypertension was excluded with normal lumbar puncture performed at 18 weeks, however, this did relieve the headache.
Progress and outcomes
Progress was satisfactory and growth scans, performed fortnightly from week 18, were reassuring to 33 weeks gestation. At the 33-week scan growth had slowed with the fetus lying at<10th customised growth centile. The middle cerebral artery Doppler was at the upper range of normal (peak systolic velocity 59 cm/s), and the ductus venosus trace and the umbilical artery Doppler were normal. There was little growth of the abdominal circumference since the previous scan 2 weeks earlier, when it was tracking normally along the 50th centile. In view of the prior obstetric history and in consultation with the paediatric team, the decision was made to proceed to caesarean section at 34 weeks with the delivery of a live male infant weighing 2195 g. A course of two intramuscular betamethasone doses 11.4 mg 24 hours apart was completed prior to the caesarean section.
Neonatal details
A male baby was born at the gestational age of 34 weeks and 2 days weighing 2195 g with Apgar scores of 9 at 1 min and 10 at 5 min. He was admitted to the neonatal intensive care unit due to prematurity and, while there, was noted to have mild respiratory distress that required a short course of intravenous antibiotics. No respiratory support was required.
He also had mild jaundice with initially trending up bilirubin levels, and was treated with phototherapy for 48 hours. There was also initial hypoglycaemia and hypothermia which was quickly corrected and he remained stable until discharge 13 days later. By discharge, full breast feeding was well established.
Investigations: pathological examination procedures
For the index placenta, a trained examiner assessed the fresh refrigerated placentae (within 24 hours of delivery) by standard pathological technique. Eight standard sections were dissected per placenta and consisted of transmural placental sections within 50 mm of the umbilical insertion. H&E stained sections were prepared according to standard procedures, and examined by a perinatal pathologist. The other placentae had been examined histopathologically following formalin fixation, within 24 hours of delivery. Miscarriage products had been submitted for routine histopathological processing.
Clinicopathological features
The first two pregnancies over 10 weeks (third and fourth pregnancy) showed intervillous histiocytes (macrophages) among abundant perivillous fibrin, haemorrhage and acute inflammation on review. The histiocytic inflammation was either not noticed or considered typical for products of conception. On review the intervillous histiocytes and perivillous fibrin were regarded as pathological. Neither of the diagnostic reports by general pathologists mentioned histiocyte presence. Review of the 20 weeks placenta (fourth pregnancy), also reported by general diagnostic histopathology did not mention abundant intervillous histiocytes.
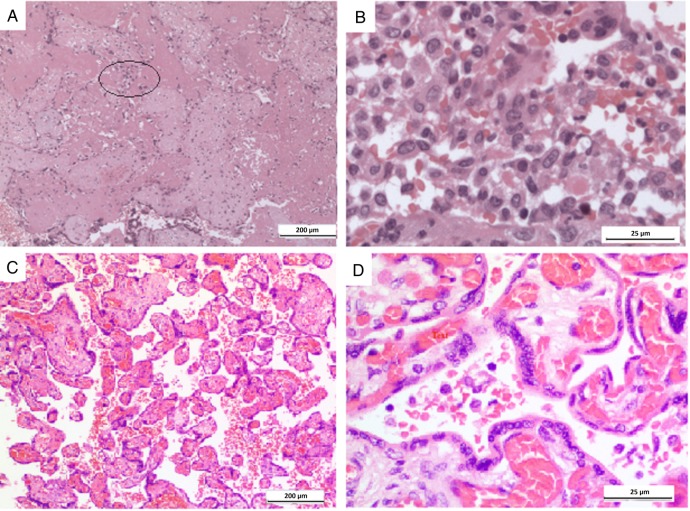
The 27-week intrauterine fetal demise (fifth pregnancy) placenta demonstrated abundant intervillous histiocytes and perivillous fibrin (figure 1A, B). The villous capillaries also demonstrated increased numbers of nucleated red cells. Maternal serology was negative for cytomegalovirus, toxoplasmosis, rubella and herpes and no viral inclusions (eg, parvovirus or herpes) were found in the fetal tissue samples. In the placenta from the treated liveborn pregnancy, the sixth pregnancy, placental perivillous fibrin was almost absent and intervillous histiocytes were much less frequent (figure 1C, D). The placenta was also submitted for routine diagnostic histopathology, and the few histiocytes present (5%) were not noticed by the reporting pathologist who was not aware of the previous postmortem diagnosis. Placental transections were supplemented on clinicopathological review, by a further four sections to ensure that the placenta was rigorously sampled, to confirm the low level of histiocyte infiltration (∼5%) following treatment.
Figure 1.
Placentae histopathology. (A) Low power view of fifth pregnancy placenta with scattered histiocytes (encircled) and abundant fibrin deposition. (B) Higher power view of the fifth pregnancy placenta with numerous histiocytes. (C) No intervillous fibrin and few scattered histiocytes in treated sixth pregnancy placenta. (D) Only a few patches of intervillous histiocytes were present in the treated sixth pregnancy placenta.
Discussion
The diagnosis of CHI is restricted to a postnatal histopathological analysis. It is based on the presence of extensive maternal histiocytes (macrophages) within the intervillous space.1 11 12 Although no consensus exists on the diagnostic criteria,10 a CHI score based on the relationship between the extent of the histological lesions and the severity of the clinical outcome has been published,6 demonstrating a correlation between high scores and worse pregnancy outcomes.
Interestingly, a clinical history of atopic conditions, namely asthma and eczema, reported in our patient, but not autoimmune disease, is in keeping with Boyd and Redline study1 in which 52% of women had history of autoimmune disease (defined as organ specific autoantibodies, antiphospholipid antibody syndrome and sarcoidosis), asthma, or drug allergy.
From a treatment perspective, at the time we looked after this woman, very little had been published on effective interventions to improve pregnancy outcomes in the presence of CHI5 6 12 and comparative trials on different treatment regimens were lacking. LMWH with or without aspirin has been extensively investigated for its potential benefit in thrombophilic and non-thrombophilic women with prior recurrent pregnancy loss and other adverse outcomes (eg, fetal growth restriction, placental vasculopathy). Some trials suggest benefit in reducing recurrent early and late pregnancy loss,13 14 as well as reduction in adverse outcomes and placental vasculopathy.15 16 Conversely, a recent double-blinded randomised controlled study by Pasquier et al17 reported, in keeping with similarly well conducted studies, that LMWH did not improve live birth rates in non-thrombophilic women with previous consecutive recurrent miscarriage.18–20
A hypothesis regarding the origin of this pathological entity suggests a maternal immunological process,1 7 21 and is the reason for using corticosteroid treatment to improve pregnancy outcomes.3 5 6 12 21
Moreover, a recent multicentre prospective case series of subsequent pregnancy in 24 patients with previous CHI has since been published.21 In addition to describing the pregnancy outcomes, immunological findings and associated diseases in women with previous CHI, and factors associated with pregnancy loss, they also looked at different treatment regimens to improve outcomes. The comparison of different treatment regimens, including aspirin, LMWH, prednisone and hydroxychloroquine, failed to determine the most effective treatment in improving live birth rates. Nevertheless, they reported an increase in the number of live births from 32% to 67% in the treated pregnancies, albeit with a persistent 30% risk of preterm delivery despite different treatment strategies.21
In our reported case, the histopathological examination demonstrated that placentae from the unsuccessful pregnancies had similar intensities of intervillous histiocytic infiltration and fibrin deposition, and it is thus hypothesised that the treatment with LMWH and aspirin reduced both parameters in the successful pregnancy when compared with previous pregnancies (figure 1C, D).
In summary, we report a case of a successful pregnancy following treatment subsequent to a diagnosis of CHI. Although further studies are required to confirm the hypothesis and the efficacy of interventions, immunosuppressive and antithrombotic treatments show favourable results thus far.6 12 21
Concerning histopathological examination, awareness among reporting pathologists is important so that CHI is detected following the earliest pregnancy loss possible to allow for potentially effective intervention in a subsequent pregnancy. In this case, it was missed in two pregnancies before an intrauterine demise of a growth restricted fetus led to the diagnosis and the subsequent successful intervention and outcome.
Learning points.
Chronic histiocytic intervillositis (CHI) is a rare placental lesion associated with adverse obstetric outcomes including recurrent miscarriage, intrauterine growth restriction and death, and high recurrence rate in subsequent pregnancies.
Diagnosis can only be established postpartum by histopathological examination of the placenta and can be easily missed in the absence of strong suspicion and awareness of this entity.
Limited evidence suggests that early intervention with immunosuppressive and antithrombotic agents may improve outcome for pregnancies that follow a CHI pregnancy.
In all cases of fetal complications (eg, intrauterine fetal growth restriction, intrauterine fetal demise) placentae should preferably be examined by a perinatal pathologist.
Footnotes
Contributors: HP was the O&G consultant caring for the patient and NAH was the pathologist. HP, NAH and LV participated equally in the preparation of this report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Boyd TK, Redline RW. Chronic histiocytic intervillositis: a placental lesion associated with recurrent reproductive loss. Hum Pathol 2000;31:1389–96. [PubMed] [Google Scholar]
- 2.Labarrere C, Mullen E. Fibrinoid and trophoblastic necrosis with massive chronic intervillositis: an extreme variant of villitis of unknown etiology. Am J Reprod Immunol Microbiol 1987;15:85–91. [DOI] [PubMed] [Google Scholar]
- 3.Doss BJ, Greene MF, Hill J et al. . Massive chronic intervillositis associated with recurrent abortions. Hum Pathol 1995;26:1245–51. [DOI] [PubMed] [Google Scholar]
- 4.Jacques SM, Qureshi F. Chronic intervillositis of the placenta. Arch Pathol Laboratory Med 1993;117:1032–5. [PubMed] [Google Scholar]
- 5.Rota C, Carles D, Schaeffer V et al. . Perinatal prognosis of pregnancies complicated by placental chronic intervillitis. J Gynecol Obstet Biol Reprod (Paris) 2006;35:711–19. [DOI] [PubMed] [Google Scholar]
- 6.Parant O, Capdet J, Kessler S et al. . Chronic intervillositis of unknown etiology (CIUE): relation between placental lesions and perinatal outcome. Eur J Obstet Gynecol Reprod Biol 2009;143:9–13. 10.1016/j.ejogrb.2008.06.012 [DOI] [PubMed] [Google Scholar]
- 7.Marchaudon V, Devisme L, Petit S et al. . Chronic histiocytic intervillositis of unknown etiology: clinical features in a consecutive series of 69 cases. Placenta 2011;32:140–5. 10.1016/j.placenta.2010.11.021 [DOI] [PubMed] [Google Scholar]
- 8.Redline RW, Zaragoza M, Hassold T. Prevalence of developmental and inflammatory lesions in nonmolar first-trimester spontaneous abortions. Human pathol 1999;30:93–100. [DOI] [PubMed] [Google Scholar]
- 9.Contro E, deSouza R, Bhide A. Chronic intervillositis of the placenta: a systematic review. Placenta 2010;31:1106–10. 10.1016/j.placenta.2010.10.005 [DOI] [PubMed] [Google Scholar]
- 10.Traeder J, Jonigk D, Feist H et al. . Pathological characteristics of a series of rare chronic histiocytic intervillositis of the placenta. Placenta 2010;31:1116–19. 10.1016/j.placenta.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 11.Labarrere C, Althabe O. Chronic villitis of unknown aetiology in recurrent intrauterine fetal growth retardation. Placenta 1987;8:167–73. [DOI] [PubMed] [Google Scholar]
- 12.Boog G, Le Vaillant C, Alnoukari F et al. . Combining corticosteroid and aspirin for the prevention of recurrent villitis or intervillositis of unknown etiology. J Gynecol Obstet Biol Reprod (Paris) 2006;35:396–404. [DOI] [PubMed] [Google Scholar]
- 13.Fawzy M, Shokeir T, El-Tatongy M et al. . Treatment options and pregnancy outcome in women with idiopathic recurrent miscarriage: a randomized placebo-controlled study. Arch Gynecol Obstet 2008;278:33–8. 10.1007/s00404-007-0527-x [DOI] [PubMed] [Google Scholar]
- 14.Gris JC, Mercier E, Quéré I et al. . Low-molecular-weight heparin versus low-dose aspirin in women with one fetal loss and a constitutional thrombophilic disorder. Blood 2004;103:3695–9. 10.1182/blood-2003-12-4250 [DOI] [PubMed] [Google Scholar]
- 15.Kupferminc M, Rimon E, Many A et al. . Low molecular weight heparin versus no treatment in women with previous severe pregnancy complications and placental findings without thrombophilia. Blood Coagul Fibrinolysis 2011;22:123–6. 10.1097/MBC.0b013e328343315c [DOI] [PubMed] [Google Scholar]
- 16.Kamda JH, Ghidini A, Pezzullo JC et al. . Prophylaxis with low molecular weight heparin for prevention of placenta-related recurrent adverse pregnancy outcomes International Blood Research & Reviews 2014;2:140–8. [Google Scholar]
- 17.Pasquier E, de Saint Martin L, Bohec C et al. . Enoxaparin for prevention of unexplained recurrent miscarriage: a multicenter randomized double-blind placebo-controlled trial. Blood 2015;125:2200–5. 10.1182/blood-2014-11-610857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaandorp SP, Goddijn M, van der Post JA et al. . Aspirin plus heparin or aspirin alone in women with recurrent miscarriage. N Engl J Med 2010;362:1586–96. 10.1056/NEJMoa1000641 [DOI] [PubMed] [Google Scholar]
- 19.Clark P, Walker ID, Langhorne P et al. . SPIN (Scottish Pregnancy Intervention) study: a multicenter, randomized controlled trial of low-molecular-weight heparin and low-dose aspirin in women with recurrent miscarriage. Blood 2010;115:4162–7. 10.1182/blood-2010-01-267252 [DOI] [PubMed] [Google Scholar]
- 20.Dolitzky M, Inbal A, Segal Y et al. . A randomized study of thromboprophylaxis in women with unexplained consecutive recurrent miscarriages. Fertil Steril 2006;86:362–6. 10.1016/j.fertnstert.2005.12.068 [DOI] [PubMed] [Google Scholar]
- 21.Mekinian A, Costedoat-Chalumeau N, Masseau A et al. . Chronic histiocytic intervillositis: outcome, associated diseases and treatment in a multicenter prospective study. Autoimmunity 2015;48:40–5. 10.3109/08916934.2014.939267 [DOI] [PubMed] [Google Scholar]