Abstract
Objectives
Decreased renal function is associated with increased cardiovascular risk. Our study was planned to verify the association of decreased renal function and subclinical coronary atherosclerosis in postmenopausal women.
Methods
We performed a retrospective review of 251 Korean postmenopausal women who visited the health promotion center for a routine health checkup. Estimated glomerular filtration rate (eGFR) was used to show renal function, which was estimated by calculated using the Cockcroft-Gault (CG) and the modification of diet in renal disease (MDRD) formulas. Coronary atherosclerosis was assessed by 64-row multidetector computed tomography.
Results
Women with reduced eGFR (< 60 mL/minute/1.73 m2) had significantly higher brachial-ankle pulse wave velocity (baPWV) than women with normal eGFR (≥ 60 mL/minute/1.73 m2). The eGFR was negatively correlated with baPWV (r = -0.352, P < 0.001), significantly. The eGFR was lower in women with coronary atherosclerosis than in normal control women, markedly. Reduced eGFR was significantly associated with the presence of coronary atherosclerosis (odds ratio [OR] = 7.528, 95% confidence interval [CI] = 2.728-20.772, P < 0.001).
Conclusions
Decreased eGFR was closely associated with increased arterial stiffness and coronary atherosclerosis in postmenopausal women. Evaluating subclinical atherosclerosis by screening the renal function in postmenopausal women may be helpful screening high risk group and considering starting menopausal hormone therapy before atherosclerosis development.
Keywords: Coronary artery disease, Kidney function tests, Postmenopause, Vascular stiffness
Introduction
In postmenopausal women, cardiovascular disease (CVD) is major reason of morbidity and mortality.1 In the past, menopausal hormonal therapy (MHT) had been regarded to have effect of preventing CVD, but several randomized controlled trials (RCTs) have shown that MHT does not reduce or slow the progression of established CVD.2,3,4,5 Nowadays MHT is not recommended for the primary and secondary prevention of CVD.
Unlike RCTs, most observational studies support potential benefits of MHT in reducing risk of CVD. Furthermore, reanalysis of RCT showed that starting MHT closer to menopause tended to reduce the risk of CVD compared with starting MHT distant from menopause, which suggests determining start point of MHT could be important.6 However, when the endothelium is involved with atherosclerosis already, it is too late for estrogen to exert a beneficial effect.7 Therefore, risk assessment of atherosclerosis among postmenopausal women is important to enhance primary prevention of CVD and to minimize adverse effects of MHT.
CVD is common in patients with chronic kidney disease regardless of age and stage of kidney disease. There is now evidence that decreased renal function (estimated glomerular filtration rate [eGFR] < 60 mL/minute/1.73 m2) is associated with cardiovascular events in general populations as well as high-risk groups.8 Therefore, screening for early kidney function impairment assessed by glomerular filtration rate (GFR) may help to detect patients at increased cardiovascular risks. Previous our study showed that postmenopausal women with decreased renal function are more likely to have increased arterial stiffness which reflects the severity of vascular damage.9 In addition, arterial stiffness measured by brachial-ankle pulse wave velocity (baPWV) had high predictive values for coronary atherosclerosis in postmenopausal women.10 These results suggest that assessing renal function using eGFR can be an economical and convenient method for assessment of cardiovascular risks in postmenopausal women.
However, it has not been evaluated whether renal function assessed by eGFR may reflect cardiovascular risk in postmenopausal women. The purpose of the current study is to investigate the association of decreased renal function with subclinical coronary atherosclerosis in postmenopausal women.
Materials and Methods
1. Participants
We performed a retrospective review of postmenopausal women who visited the health promotion center in Gangnam Severance Hospital, Seoul, South Korea, for a routine checkup from January 2007 to December 2009. Lifestyle, past histories and current medication were checked as same as our previous study, as well as the physical examination.11 We included postmenopausal women over 45 years old who underwent blood analysis, baPWV, and 64-row multidetector computed tomography (64-MDCT) as parts of the routine checkup. Menopause was defined as the absence of menstrual periods for 12 months and was confirmed by a serum follicle stimulating hormone (FSH) levels > 30 mIU/mL. Participants with CVD such as myocardial infarction or ischemic stroke were excluded. A total of 251 participants who met these criteria were finally included in the study.
Smoking history was divided into two categories: current and past or never smoker. Alcohol intake was divided into drinker and nondrinker. Hormone therapy (HT) use was divided into two categories: current or ever and never users. Physical activity was divided into active and inactive exerciser. Active exerciser was defined as someone who exercised three or more times per week for over 30 minutes. The study was reviewed and approved by the institutional review board of Severance Hospital, Yonsei University College of Medicine.
2. Blood analysis
After a 12-hour overnight fast, participants' blood samples were collected through an antecubital vein. Fasting plasma glucose, total cholesterol, triglyceride, high-density lipoprotein (HDL)-cholesterol, low-density lipoprotein (LDL)-cholesterol, and creatinine were measured using a 7600-110 Chemistry Auto analyzer (Hitachi, Tokyo, Japan).
3. Renal function
The GFR (mL/minute/1.73 m2) was estimated according to the Cockcroft-Gault (CG) formula and the modification of diet in renal disease (MDRD) formula as follows:
CG = ([140 - age] × body weight [kg] × 0.85)/(serum creatinine [mg/dL] × 72), adjusted for body surface area by 1.73 m2/body surface area
MDRD = 186 × serum creatinine (mg/dL)-1.154 × age- 0.203 × 0.742.
Decreased renal function was diagnosed with eGFR less than 60 mL/minute.
4. baPWV measurement
PWV was measured using the automatic waveform analyzer (BP-203RPE; Colin Co., Komaki, Japan) in accordance with a previously described method.10 The inter-operator and intra-operator variation were less than 5.0% of coefficient. The mean values for the right and left baPWV were used for statistical analyses.
5. Coronary artery assessment
Cardiac MDCT was done using a 64-MDCT scanner (Philips Brilliance 64; Philips Medical System, Best, the Netherlands). The method of performance for the MDCT was in accordance with a previous described method.10 Coronary atherosclerosis was defined as any size of calcified or noncalcified atherosclerotic plaque with or without luminal narrowing.12
6. Statistical analysis
All the statistical analyses carried out by using the SPSS 18.0 software package. (SPSS Inc., Chicago, IL, USA). Student's t-test was applied to compare the general characteristics of participants between two groups. Univariate and multivariate regression analysis were done to find the independent parameters in the presence of decreased renal function. Logistic regression analysis was done to assess the independent influence of renal function on detection of coronary atherosclerosis. A P value less than 0.05 was considered to be statistically significant.
Results
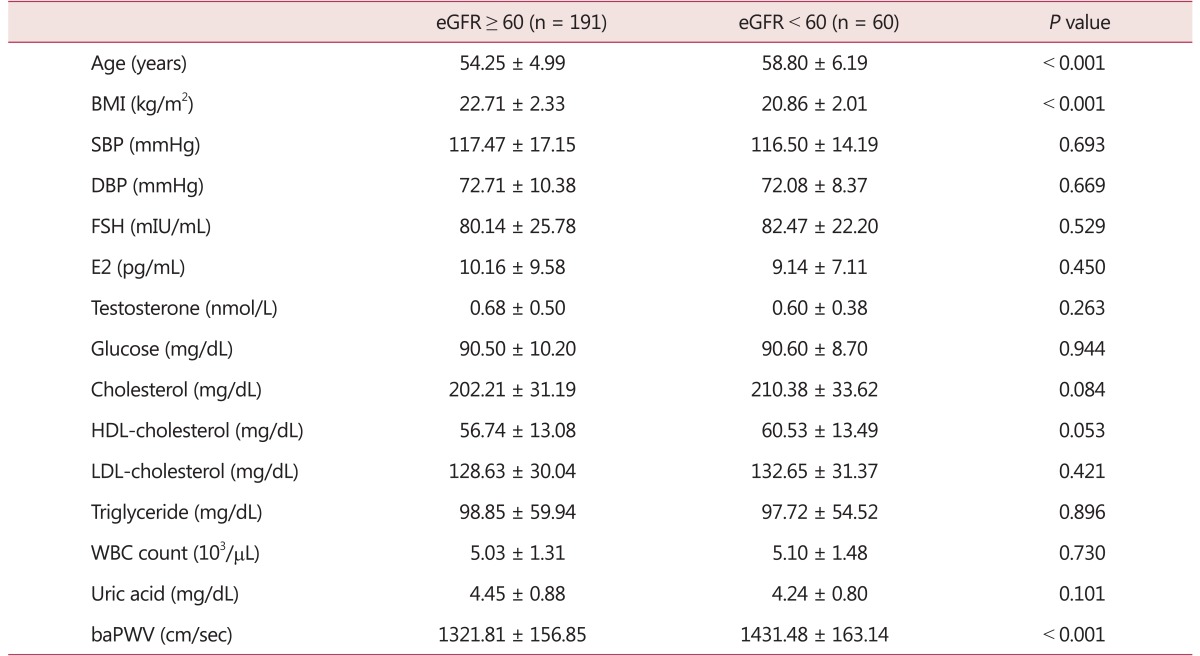
Table 1 shows general characteristics of decreased renal function group and normal renal function group. Age and baPWV were significantly higher in decreased renal function group than in normal renal function group. Body mass index (BMI) was significantly higher in normal renal function group than in decreased renal function group (Table 1).
Table 1. Baseline characteristics of the study population stratified according to estimated glomerular filtration rate values.
eGFR: estimated glomerular filtration rate, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, FSH: follicle stimulating hormone, E2: estradiol, HDL: high density lipoprotein, LDL: low density lipoprotein, WBC: white blood cells, baPWV: brachial-ankle pulse wave velocity
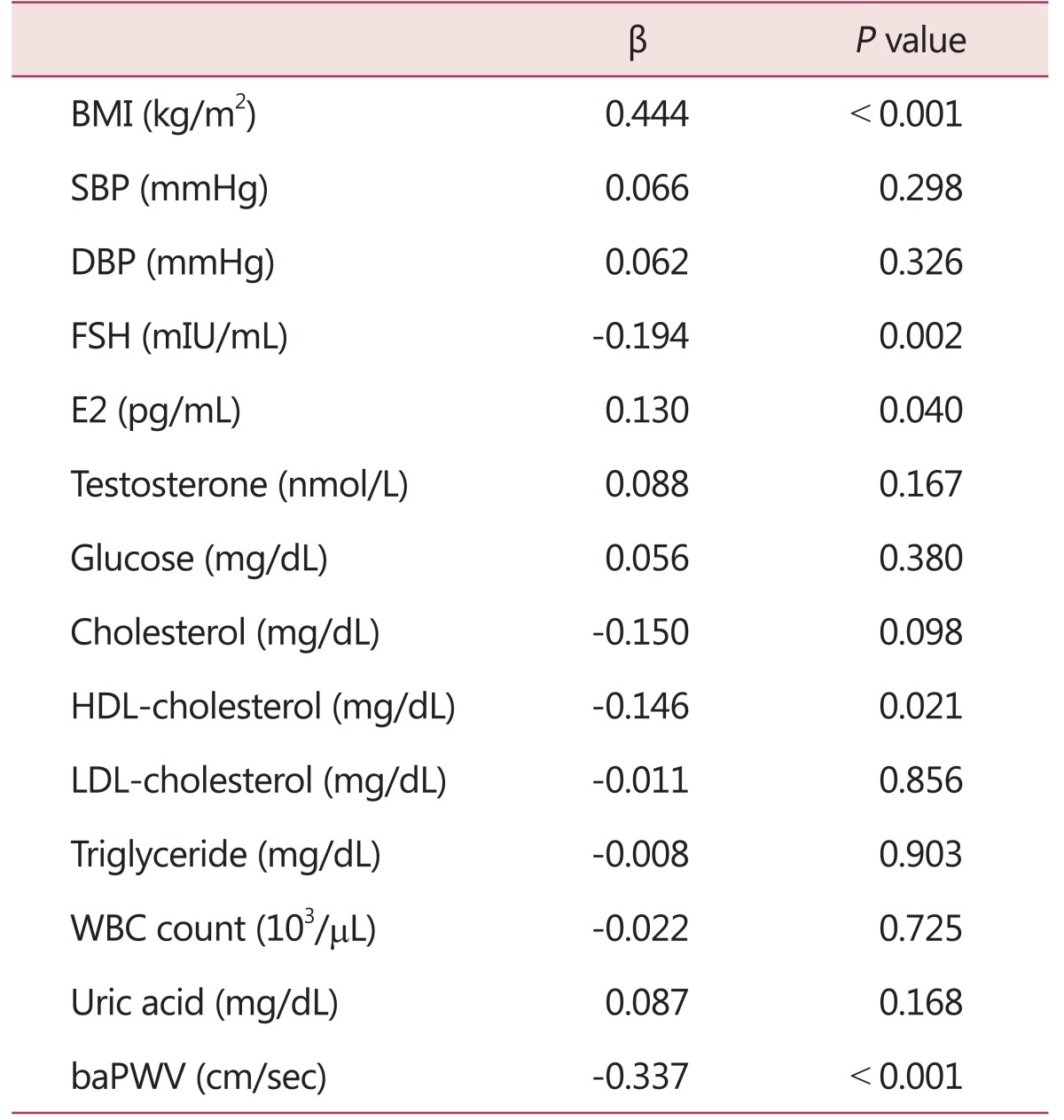
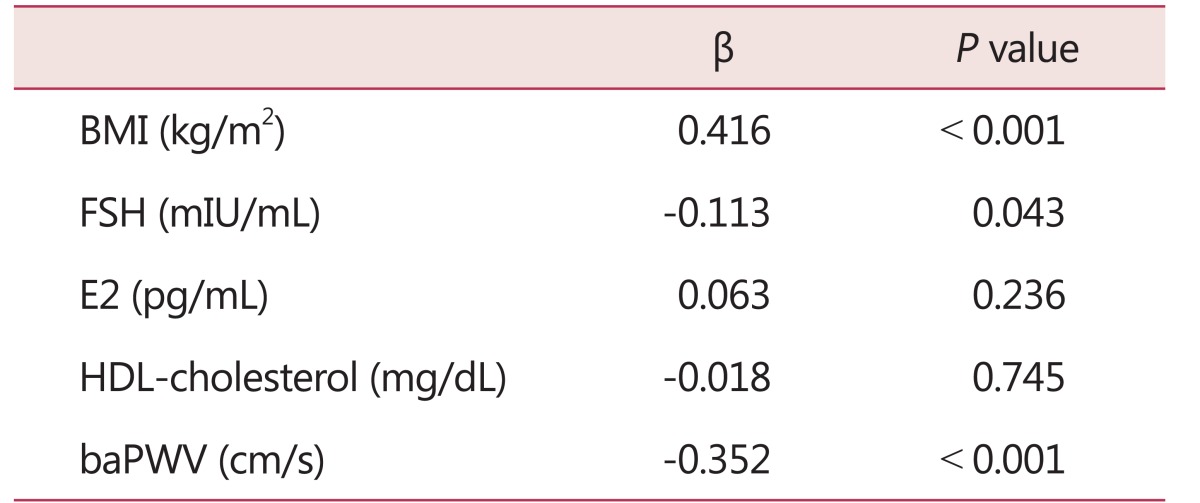
Univariate regression analysis revealed that the eGFR was significantly positively associated with BMI (β = 0.444, P < 0.001) and E2 (β = 0.130, P = 0.040), and negatively associated with FSH (β = -0.194, P = 0.002), HDL-cholesterol (β = -0.146, P = 0.021) and baPWV (β = -0.337, P < 0.001) (Table 2). Association between eGFR and baPWV is persisted in normal renal function group, but not in decreased renal function group (Fig. 1). Multivariate regression analysis revealed that the eGFR was significantly positively associated with BMI (β = 0.416, P < 0.001), and negatively associated with FSH (β = -0.113, P = 0.043) and baPWV (β = -0.352,P < 0.001) (Table 3).
Table 2. Univariate regression analysis for estimated glomerular filtration rate.
BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, FSH: follicle stimulating hormone, E2: estradiol, HDL: high density lipoprotein, LDL: low density lipoprotein, WBC: white blood cells, baPWV: brachial-ankle pulse wave velocity
Fig. 1. Simple correlation between brachial-ankle pulse wave velocity and estimated glomerular filtration rate (eGFR) according to eGFR values.
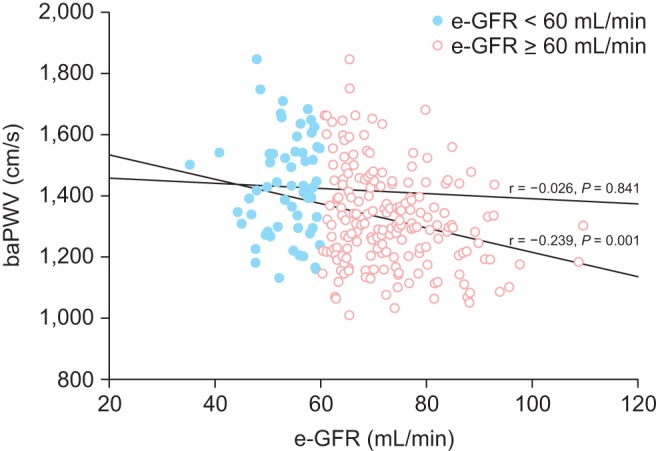
Table 3. Multivariate regression analysis for estimated glomerular filtration rate.
BMI: body mass index, FSH: follicle stimulating hormone, E2: estradiol, HDL: high density lipoprotein, baPWV: brachial-ankle pulse wave velocity
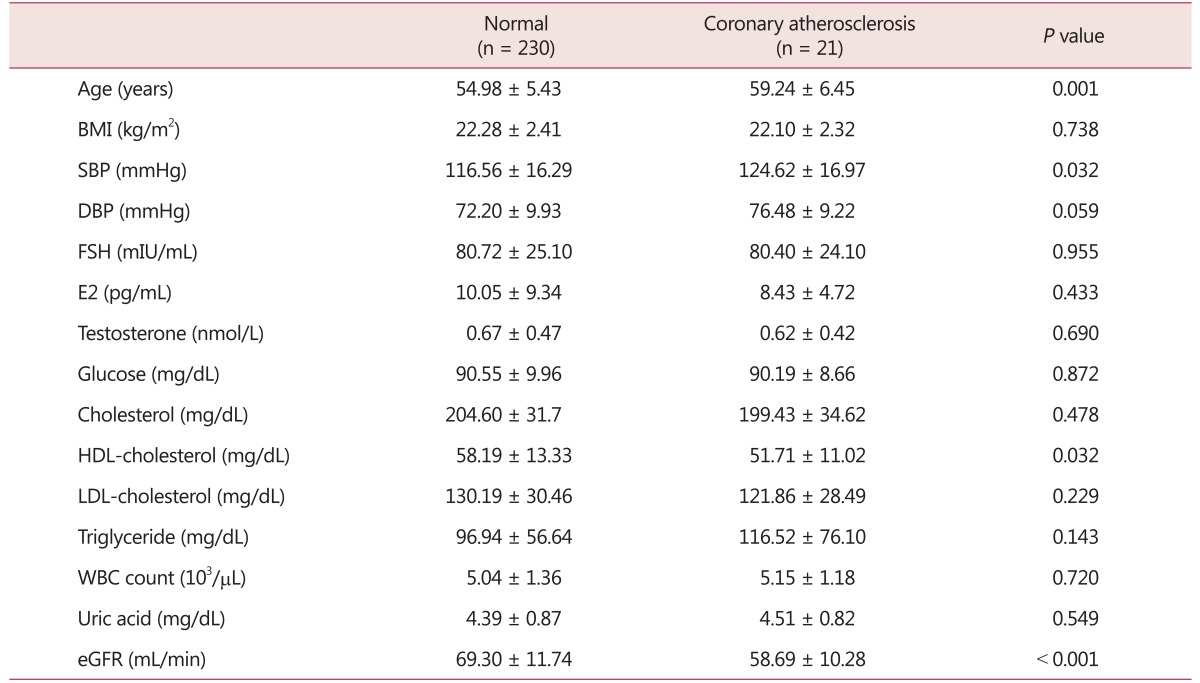
Table 4 shows general characteristics of atherosclerosis group and control group. Age and systolic blood pressure (SBP) were significantly higher in women with coronary atherosclerosis than in normal control women. HDL-cholesterol and eGFR were significantly lower in women with coronary atherosclerosis than in normal control women (Table 4).
Table 4. Baseline characteristics of normal women and women with coronary atherosclerosis.
BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, FSH: follicle stimulating hormone, E2: estradiol, HDL: high density lipoprotein, LDL: low density lipoprotein, WBC: white blood cells, eGFR: estimated glomerular filtration rate
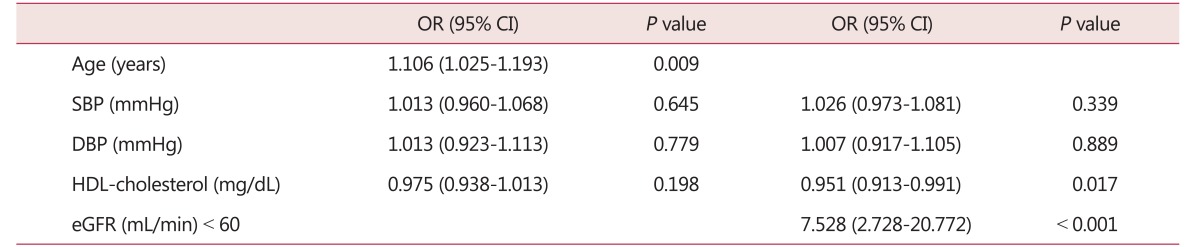
Logistic regression analysis was performed to evaluate the independence influence of decreased renal function on coronary atherosclerosis. Age was significantly associated with the presence of coronary atherosclerosis (odds ratio [OR] = 1.106, 95% confidence interval [CI] = 1.025-1.193, P = 0.009). When the eGFR was considered, HDL-cholesterol (OR = 0.951, 95% CI = 0.913-0.991, P = 0.017) and reduced eGFR (OR = 7.528, 95% CI = 2.728-20.772, P < 0.001) was significantly associated with the presence of coronary atherosclerosis (Table 5).
Table 5. Effects of various factors on coronary atherosclerosis as evaluated in a multiple logistic regression model.
OR: odds ratio, CI: confidence interval, SBP: systolic blood pressure, DBP: diastolic blood pressure, HDL: high density lipoprotein, eGFR: estimated glomerular filtration rate
Discussion
We evaluated the relationship between decreased renal function and risk of coronary atherosclerosis in healthy postmenopausal women. Our study demonstrated that decreased eGFR is associated with increased baPWV and increased risk of coronary atherosclerosis. This fact was confirmed through evaluating with 64-MDCT to check coronary atherosclerosis.
CVD is the number one health risk to women which is caused by age, genetic influences, hypertension, diabetes, obesity and smoking.13 Along with these risk factors, menopause causes women to face many physical as well as psychosocial problems.14 To mitigate these postmenopausal symptoms, estrogen therapy could be an option in postmenopausal women, and previous study has reported that serum estradiol level might be associated with the degree of calcification of coronary artery in postmenopausal women.15 Besides estrogen therapy, renal function is also alleged to affect on cardiovascular system. Over the last few years, measurements of renal function, increase in urine albumin excretion, are known to be powerful prognostic values for CVD.16 While the exact pathophysiological mechanisms in associations of renal disease and CVD have not been completely clarified, changes in intrarenal hemodynamics secondary to an increased systemic blood pressure load may be tangled with increased capillary leakiness at the glomerular level, reflecting on endothelial or atherosclerotic process.17
Many others have shown a positive association between decreased renal function and atherosclerosis previously.18,19,20 CVD is known to be one of the Atherosclerosis was evaluated in variable ways, such as examining the presence of plaque, peripheral arterial disease, baPWV, and left ventricular mass index. Above these studies, one study has presented decreased eGFR is significantly associated subclinical atherosclerosis.19 Similarly, another cross-sectional study also has presented mild impairment of renal function might increase arterial stiffness.21 Our results show common interrelationship with these previous studies, especially about relationship among decrease renal function and arterial stiffness, atherosclerosis. Whereas these previous studies were targeted on broadly over 50 years old people including the healthy and sick, our study focused on healthy postmenopausal women only. This makes strength on our study, which shows positive correlation between decreased renal function and atherosclerotic risk not in high risk group but in healthy postmenopausal women group for the first time. Also we have strength on that this is the first study of arterial stiffness and atherosclerosis to be co-analyzed. Additionally we suggest CG equation more sensitive in acquiring eGFR than MDRD equation, especially in Koreans. We analyzed renal function in both calculations, decreased eGFR calculated by MDRD equation also showed positive relationship with atherosclerosis. But we had limitation of data because most of eGFR by MDRD was higher and over 60 mL/minute/1.73 m2, leading analysis hardly done. To give an account of it, MDRD equation has been different according to race. On the basis of this difference, for example, modified MDRD equation is used in Japan and China. And as known generally, eGFR by MDRD equation inaccurately correlates specially in those who have normal renal function.
In practice, there are some limitations in this study. First, it has a limitation coming from the nature of retrospective study. Although several putative mechanisms were mentioned, we could not demonstrate the causal relationship between renal function and atherosclerosis. Appropriate long-term follow-up and prospective study is needed to investigate the effects of decreased renal function on development of atherosclerosis in postmenopausal women. Second, the relatively small number of participants impeded our efforts to arrive at a valid conclusion about the association between renal function and atherosclerosis. Lastly, eGFR by CG or MDRD has error compared to GFR measured by collecting 24 hour urine. In recent years, cystatin C is becoming more widely available and provides improved estimates of kidney function. Therefore, a newer kidney function marker would be required for future clinical practice.
Age and/or menopausal period is strongly associated with vascular damage (stage of atherosclerosis), and that also has been strongly accepted widely, therefore initiating MHT before vascular damage may be important factor in reducing CVD. Developing screening tool of subclinical atherosclerosis should be taken into account importantly to determine starting MHT before vascular damage development. To our knowledge, eGFR is a simple, cheap and convenient screening tool not only filtering high risk group of CVD, but also detecting atherosclerosis which could help to determine initiating MHT in postmenopausal women.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.von der Recke P, Hansen MA, Hassager C. The association between low bone mass at the menopause and cardiovascular mortality. Am J Med. 1999;106:273–278. doi: 10.1016/s0002-9343(99)00028-5. [DOI] [PubMed] [Google Scholar]
- 2.Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 3.Clarke SC, Kelleher J, Lloyd-Jones H, Slack M, Schofiel PM. A study of hormone replacement therapy in postmenopausal women with ischaemic heart disease: the Papworth HRT atherosclerosis study. BJOG. 2002;109:1056–1062. doi: 10.1111/j.1471-0528.2002.01544.x. [DOI] [PubMed] [Google Scholar]
- 4.Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA. 1998;280:605–613. doi: 10.1001/jama.280.7.605. [DOI] [PubMed] [Google Scholar]
- 5.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 6.Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297:1465–1477. doi: 10.1001/jama.297.13.1465. [DOI] [PubMed] [Google Scholar]
- 7.Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science. 2005;308:1583–1587. doi: 10.1126/science.1112062. [DOI] [PubMed] [Google Scholar]
- 8.Kurth T, de Jong PE, Cook NR, Buring JE, Ridker PM. Kidney function and risk of cardiovascular disease and mortality in women: a prospective cohort study. BMJ. 2009;338:b2392. doi: 10.1136/bmj.b2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung YS, Hwang HJ, Yun BH, Chon SJ, Cho S, Choi YS, et al. Renal function is associated with bone mineral density and arterial stiffness in healthy postmenopausal women. Gynecol Obstet Invest. 2014;78:124–129. doi: 10.1159/000363746. [DOI] [PubMed] [Google Scholar]
- 10.Seo SK, Cho S, Kim HY, Choi YS, Park KH, Cho DJ, et al. Bone mineral density, arterial stiffness, and coronary atherosclerosis in healthy postmenopausal women. Menopause. 2009;16:937–943. doi: 10.1097/gme.0b013e3181a15552. [DOI] [PubMed] [Google Scholar]
- 11.Yun BH, Chon SJ, Lee YJ, Han EJ, Cho S, Choi YS, et al. Association of metabolic syndrome with coronary atherosclerosis in non-diabetic postmenopausal women. Climacteric. 2015;18:284–289. doi: 10.3109/13697137.2014.960384. [DOI] [PubMed] [Google Scholar]
- 12.Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004;109:14–17. doi: 10.1161/01.CIR.0000111517.69230.0F. [DOI] [PubMed] [Google Scholar]
- 13.Yi SS, Hwang E, Baek HK, Kim TH, Lee HH, Jun HS, et al. Application of bioactive natural materials-based products on five women's diseases. J Menopausal Med. 2015;21:121–125. doi: 10.6118/jmm.2015.21.3.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed K, Jahan P, Nadia I, Ahmed F, Abdullah Al E. Assessment of menopausal symptoms among early and late menopausal midlife Bangladeshi women and their impact on the quality of life. J Menopausal Med. 2016;22:39–46. doi: 10.6118/jmm.2016.22.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeon GH, Kim SH, Kim SR, Chae HD, Kim CH, Kang BM. The association between serum estradiol level and coronary artery calcification in postmenopausal women: a preliminary report. J Korean Soc Menopause. 2010;16:16–22. doi: 10.1097/gme.0b013e3181d76768. [DOI] [PubMed] [Google Scholar]
- 16.Viazzi F, Cappadona F, Pontremoli R. Microalbuminuria in primary hypertension: a guide to optimal patient management? J Nephrol. 2016;29:747–753. doi: 10.1007/s40620-016-0335-0. [DOI] [PubMed] [Google Scholar]
- 17.Pedrinelli R, Dell'Omo G, Di Bello V, Pontremoli R, Mariani M. Microalbuminuria, an integrated marker of cardiovascular risk in essential hypertension. J Hum Hypertens. 2002;16:79–89. doi: 10.1038/sj.jhh.1001316. [DOI] [PubMed] [Google Scholar]
- 18.Leoncini G, Viazzi F, Parodi D, Ratto E, Vettoretti S, Vaccaro V, et al. Mild renal dysfunction and cardiovascular risk in hypertensive patients. J Am Soc Nephrol. 2004;15(Suppl 1):S88–S90. doi: 10.1097/01.asn.0000093245.78097.cd. [DOI] [PubMed] [Google Scholar]
- 19.Choi SW, Kim HY, Lee YH, Ryu SY, Kweon SS, Rhee JA, et al. eGFR is associated with subclinical atherosclerosis independent of albuminuria: the Dong-gu Study. Atherosclerosis. 2010;212:661–667. doi: 10.1016/j.atherosclerosis.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 20.Astor BC, Arnett DK, Brown A, Coresh J. Association of kidney function and hemoglobin with left ventricular morphology among African Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2004;43:836–845. doi: 10.1053/j.ajkd.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 21.Miyatake N, Shikata K, Makino H, Numata T. Relation between the estimated glomerular filtration rate and pulse wave velocity in Japanese. Intern Med. 2010;49:1315–1320. doi: 10.2169/internalmedicine.49.3085. [DOI] [PubMed] [Google Scholar]