Abstract
Superficial angiomyxomas (SAMs) are rare benign cutaneous tumors that involve the subcutaneous layer. They are commonly located in the trunk, lower limbs and head or neck of women of reproductive age. SAMs in the vulva of postmenopausal women are especially rare case. Herein, we report a vulvar SAM in a postmenopausal 60-year-old woman. The patient presented with a palpable cutaneous mass in the right labium majora that had appeared 3 months earlier. The mass was slow growing and approximately 5 cm in size and resembled a soft tissue malignancy. It appeared as a well-defined multilocular cystic mass in magnetic resonance images. The preoperative diagnosis was a benign cystic lesion such as an epidermoid cyst. Grossly, the completely excised mass was 6 × 5 cm in size and well circumscribed with a multilocular outer surface, a yellowish-gray gelatinous cut surface, and a smooth rubbery inner surface. Histologic review revealed that the mass contained small to moderate amount of cellular angiomyxoid nodules and bland-looking spindle-shaped to ovoid cells without atypia. Neutrophil infiltration, which is a diagnostic feature of SAMs, was observed. Immunohistochemistry showed expression of CD34, but not of estrogen receptors, progesterone receptors, or desmin in the SAM. The patient has been followed up for 12 months without recurrence.
Keywords: Myxoma, Postmenopause, Soft tissue neoplasms, Vulvar neoplasms
Introduction
Carney et al.1 first described the histology of superficial myxoid tumors in 1986.2,3 Recently established as discrete soft tissue tumor entities, superficial angiomyxomas (SAMs) occur cutaneously in numerous regions of the body, particularly the head and neck region, the trunk and the genital area.4 To date, 15 cases of SAMs, with diameters of 1 to 4 cm and including some in the vulva, have been reported. SAMs occur most frequently in premenopausal reproductive women 11 to 39 years of age; only one case of an SAM in vulva of a postmenopausal woman has been reported.4,5 Herein, we describe a second such case and discuss the histologic, cytologic, and immunohistochemical (IHC) features that distinguish SAMs from aggressive angiomyxomas (AAMs).
Case Report
A 60-year-old woman presented with a 3-month history of a slowly growing vulvar mass between the pubic bone and right labium majora. It was about 5 cm in size, oval-shaped, soft, mobile, non-tender, palpable on the right labium majora, and covered with normal-colored skin. The patient did not have any hyperpigmentation or nodules in other areas of the skin or any significant medical history of hypertension or dyslipidemia. The treatment history included laparoscopic bilateral salpingo-oophorectomy and a Cesarean section. Laboratory parameters, including thyroid levels, were within the normal range.
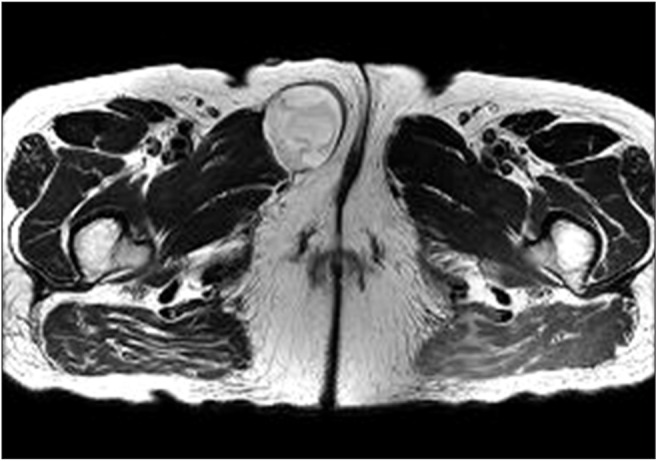
Magnetic resonance imaging performed to characterize the revealed well-defined tumor margins and inner homogenous signal intensity. On a T2-weighted image, the mass was loculated by a non-enhanced septum and had a high cystic signal (Fig. 1). No abnormal enhancement and no invasion of the mass into the surrounding tissue were found on the enhanced image. This well-defined multilocular cystic mass suggested a benign cystic lesion, such as an epidermoid cyst, which was the preoperative diagnosis. The mass was completely excised. Grossly, it was 6 × 5 cm in size and well circumscribed. Its outer surface was multilocular, cut surface was yellowish-gray and gelatinous and inner surface was smooth and rubbery. No ulcerative or erosive lesions were found on the overlying skin. A surgical specimen was stained with hematoxylin and eosin, fixed in 10% neutral buffered formalin, and embedded in paraffin.
Fig. 1. T2-weighted magnetic resonance image shows a relatively well-circumscribed mass with inner homogenous high signal intensity.
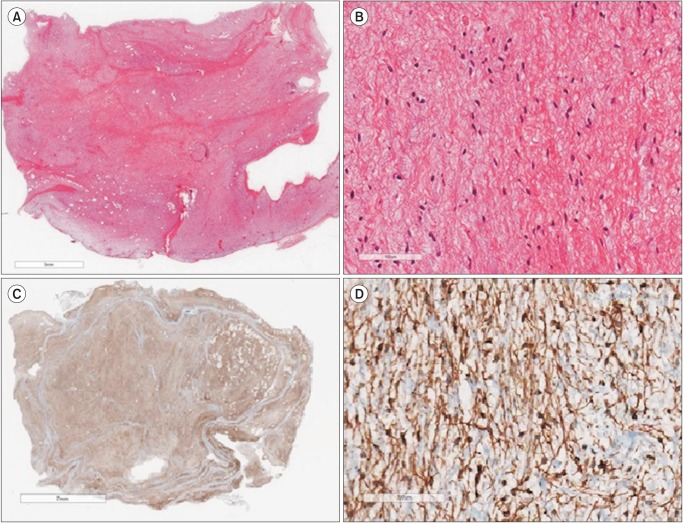
Microscopically, the tumor had sparse demarcated cellular angiomyxoid lobules and consisted of hypocellular myxoid tissue mixed with some adipose and collagenous tissue (Fig. 2A). The tumor cells had a small amount of cytoplasm, which contained collagenous strands. A histologic review revealed small to moderate amount of cellular angiomyxoid nodules.3 The mass was composed of bland-looking, spindle-shaped to ovoid cells without atypia, which is consistent with the histologic features of SAM in the absence of necrosis or ulceration (Fig. 2B). Grossly, no blood vessels were present. Immunochemistry revealed that the tumor cells expressed CD34 (Fig. 2C, 2D), but not estrogen receptors (ERs), progesterone receptors (PRs), desmin, or smooth muscle actin. No recurrence was observed during a 12-month follow-up.
Fig. 2. Histologic and imprint cytologic findings. (A) The mass consists of hypocellular myxoid tissue admixed with some adipose and collagenous tissue (hematoxylin and eosin [H & E] ×40). (B) The mass is composed of bland-looking, spindle to ovoid cells without cellular atypia, consistent with histologic features of superficial angiomyxoma (H & E ×200). (C, D) The tumor cells are immunoreactive for CD34 (C, H & E ×40; D, H & E ×200).
Discussion
SAMs are rare benign cutaneous tumors recognized as a specific type of soft tissue tumor. Since they lack distinctive features like fibroepithelial polyp,6 their diagnosis is difficult. Recently, SAMs have been clearly established as discrete soft tissue tumor entities.5 They can occur anywhere in the superficial tissue and are non-tender, slow growing masses.4 To date, 15 cases of SAMs, 1 to 4 cm in diameter and including some in the vulva, have been reported. The incidence of SAMs peaks in premenopausal reproductive women aged 11 to 39. Thus far, only one case of an SAM in a postmenopausal woman has been described, and that case is similar to the present case.2,4,5 Fetsch et al.4 reported 13 cases of SAMs in the genital area, all occurring before menopause. Although SAMs are benign, local recurrence with non-fatal consequences has been reported in cases of incomplete excision.4 Four of the 15 previously described SAMs showed a tendency towards local recurrence.4,5 The lesions should be removed with a clear resection margin.
Clinically, almost all vulvar SAMs are well-circumscribed, frequently extending to the subcutaneous fat and appearing as polypoid or papulonodular cutaneous lesions.7 Grossly they are soft, often elevated multilobular nodules. The cut surface is grey to white, translucent, and gelatinous with occasional hemorrhagic content.2
The pathogenesis of SAMs is not clear, although it is thought that SAMs arise from dysfunctional mesenchymal cells with genetic abnormalities.4 Vulvar SAMs are usually diagnosed by the pathologist, not by the clinician. Histopathologically, SAMs have small, prominent, thin-walled blood vessels, and stromal neutrophils are common.5 These features are important for diagnosis. The present case had sparse vascular structures and neutrophils. SAMs exhibit a vascular pattern with irregularities at the resection margin and a well-demarcated margin. They differ from AAMs because of their lower frequency of local recurrence.8 AAMs have about a 30% chance of recurrence, which is easily treatable via excision with a 1-cm margin. Most patients have only one AAM recurrence.9,10 About 150 cases of AAMs have been reported; although almost all had a favorable prognosis, two involved patients with a poor prognosis who ultimately succumbed to the cancer.11 Microscopically, AAMs have a vascular structure with a regular pattern and an infiltrative resection margin.12 IHC stains are helpful diagnostic tools. SAMs are usually negative for IHC markers other than vimentin and CD34.5 In this case, the tumor cells expressed CD34, but not ERs, PRs, or desmin. Unlike SAMs, AAMs are ER- and/or PR-positive.
SAMs are benign mesenchymal tumors that occur in women of reproductive age and in a wide variety of cutaneous locations. Postmenopausal cases of SAM are rare. AAMs can be distinguished from SAMs by their propensity for local recurrence and metastatic potential. Detailed histopathologic examination and IHC staining help to clarify the diagnosis.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Carney JA, Headington JT, Su WP. Cutaneous myxomas. A major component of the complex of myxomas, spotty pigmentation, and endocrine overactivity. Arch Dermatol. 1986;122:790–798. doi: 10.1001/archderm.122.7.790. [DOI] [PubMed] [Google Scholar]
- 2.Allen PW. Myxoma is not a single entity: a review of the concept of myxoma. Ann Diagn Pathol. 2000;4:99–123. doi: 10.1016/s1092-9134(00)90019-4. [DOI] [PubMed] [Google Scholar]
- 3.Allen PW, Dymock RB, MacCormac LB. Superficial angiomyxomas with and without epithelial components. Report of 30 tumors in 28 patients. Am J Surg Pathol. 1988;12:519–530. doi: 10.1097/00000478-198807000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Fetsch JF, Laskin WB, Tavassoli FA. Superficial angiomyxoma (cutaneous myxoma): a clinicopathologic study of 17 cases arising in the genital region. Int J Gynecol Pathol. 1997;16:325–334. doi: 10.1097/00004347-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Calonje E, Guerin D, McCormick D, Fletcher CD. Superficial angiomyxoma: clinicopathologic analysis of a series of distinctive but poorly recognized cutaneous tumors with tendency for recurrence. Am J Surg Pathol. 1999;23:910–917. doi: 10.1097/00000478-199908000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Kim TH, Lee HH, Chung SH, Hwang IC, Han HS. Fibroepithelial polyps on an unusual genital site during menopausal transition. J Korean Soc Menopause. 2011;17:110–113. [Google Scholar]
- 7.Nucci MR, Fletcher CD. Vulvovaginal soft tissue tumours: update and review. Histopathology. 2000;36:97–108. doi: 10.1046/j.1365-2559.2000.00865.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim HS, Kim GY, Lim SJ, Ki KD, Kim HC. Giant superficial angiomyxoma of the vulva: a case report and review of the literature. J Cutan Pathol. 2010;37:672–677. doi: 10.1111/j.1600-0560.2009.01333.x. [DOI] [PubMed] [Google Scholar]
- 9.Metin A, Nese CD, Nagihan C, Ender D. Aggressive angiomyxoma of the vulva: a case report and review of the literature. Aegean Pathol J. 2006;3:1–4. [Google Scholar]
- 10.Kura MM, Jindal SR, Khemani UN. Aggressive angiomyxoma of the vulva: An uncommon entity. Indian Dermatol Online J. 2012;3:128–130. doi: 10.4103/2229-5178.96712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blandamura S, Cruz J, Faure Vergara L, Machado Puerto I, Ninfo V. Aggressive angiomyxoma: a second case of metastasis with patient's death. Hum Pathol. 2003;34:1072–1074. doi: 10.1053/s0046-8177(03)00419-2. [DOI] [PubMed] [Google Scholar]
- 12.Fetsch JF, Laskin WB, Lefkowitz M, Kindblom LG, Meis-Kindblom JM. Aggressive angiomyxoma: a clinicopathologic study of 29 female patients. Cancer. 1996;78:79–90. doi: 10.1002/(SICI)1097-0142(19960701)78:1<79::AID-CNCR13>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]