Abstract
Objectives
The purpose of this study was to evaluate the quality of life (QOL) in postmenopausal members and non-members of the elderly support association in Borujen city, Iran.
Methods
This study was a cross-sectional descriptive study being applied to the participants were postmenopausal women of over 55 years. Thus, 40 postmenopausal members of the elderly support association of Borujen city and 40 non-members were randomly selected. The 36 item short-form health survey (SF-36), with the 4 psychological, social, physical-movement, and environmental domains, was completed. Data were analyzed using SPSS software.
Results
The mean total score of QOL of member of the association was significantly greater than non-members. Student's t-test showed a significant relationship between QOL and membership of the association (P < 0.05). One-way analysis of variance (ANOVA) showed that the mean QOL of postmenopausal women, according to membership and marital status (P < 0.01), housing (P < 0.01), and underlying disease (P < 0.01), was statistically significant.
Conclusions
According to the results, supportive measures, such as increasing the participation of the elderly in public life through proper preparations to join them and membership in peer groups such as support associations and non-governmental organizations (NGOs) can be greatly effective in improving QOL. The results showed that the QOL of the participants was at a moderate level and membership in support associations for the elderly was effected on the QOL in postmenopausal women. Moreover, considering the importance of the elderly in the community.
Keywords: Aged, Community networks, Postmenopause, Quality of life, Women's health
Introduction
One of the greatest challenges facing society in this century, aging population with a growing elderly population along with industrialization, an increase in the number of working-women, a decreasing fertility rate, and an extended human life span with improvements in medicine.1 Today, health systems plan their most important programs based on family health. Women are the center of family health and are the main role model for the next generation of teaching and promoting healthy living. Although men and women have similar health issues, women are confronted with specific issues arising from their physiological conditions.2 One of these issues is the menopausal transition during which women experience additional problems due to the reduction in estrogen. Menopause is part of the critical phases of a woman's life, which characterizes the transition from fertility to infertility. Menopause is inevitable and goes back to the early history of human creation. Its occurrence in women has been associated with different cultural, economic, and religious attitudes.3,4 According to the World Health Organization (WHO), menopause is the actual cessation of menstruation for at least 12 months due to loss of ovarian follicular activity. Menopause is held between the ages of 40 and 60 years and on average at the age of 51 years. With increased longevity, women spend about one third of their life in the postmenopausal period.5 Menopause is followed by endocrine, physical, and mental disorders and can last for several years. Although these symptoms and problems are numerous, no one experiences all of them. However, it is estimated that 75% of postmenopausal women experience severe symptoms, some of which cause extreme discomfort and life disruption.3,6 With aging and the incidence of menopause, changes will occur in various aspects of women's health, including genital symptoms (dryness, burning, and irritation), and sexual symptoms (lack of lubrication, discomfort or pain, and impaired function, but also urinary symptoms (urgency, dysuria, and recurrent urinary tract infections) and a variety of diseases.7 However, due to these changes, the elderly are vulnerable to damage and reduced quality of life (QOL), and require attention, respect, and an intensive care model.8
Through measuring QOL, we can obtain a more realistic portrayal of individuals' emotions and areas of difficulty in understanding their needs and distribution of health care. Therefore, the effectiveness of this approach, as an ultimate purpose of all preventive interventions and health promotion, should be considered.9 Research findings show that 58% of the elderly aged over 65 years need help to carry out their daily activities and have a lower QOL, because menopause affects all aspects of health and increased symptoms it threatens the QOL.10,11 In describing QOL, it can be said that it is composed of both objective and subjective indicators. The subjective indicator of QOL is the feeling of satisfaction or pleasure which is the result of perception and evaluation of one's life. Though in this feeling, cognitive aspects are further discussed, it is the emotional aspect of QOL which is mainly considered.12 Similar situations are the environmental variables that affect the QOL, including issues like the welfare state, economic, political, cultural, environmental factors, and etcetera. Modification of life model and consideration of QOL can to some extent increase the efficiency and independence of the elderly and help them in controlling and treating of complications of aging and menopause.13 Changes in life style and inclination to healthy living are possible with appropriate nutrition, exercise, stress reduction, decreased fat and salt intake, avoidance of self-medication, fruits and vegetable consumption, blood pressure control, and increased daily water consumption.10 Modifying life style and attention to quality very much it can increase the efficiency and independence of older people and put them in control of multiple effects of aging and help its different treatment.14 Menopausal women experience more extreme symptoms during this period usually have lower QOL improve the QOL using alternative and preventive measures, effective role in the management of women has menopause period.15 The number of elderly training and physiotherapy associations and centers is increasing across the country. Moreover, their main aim is to strengthen the abilities and independence of the elderly, and thus, to increase their vitality. Numerous studies have been conducted on the QOL of the elderly, but rarely on the factors affecting their QOL. Therefore, this study aimed to assess QOL in postmenopausal women, both members and non-members of the elderly support association.
Materials and Methods
This study was a cross-sectional study on postmenopausal women aged 55 and older carried out in Borujen City Iran in 2014. Thus, 40 postmenopausal women attending the training and rehabilitation center Behbood of Borujen City and 40 postmenopausal women non-members of the association were randomly selected for this study. All study subjects expressed their willingness to participate in the study during an explanation meeting. Inclusion criteria included being over 55 years of age, lack of dementia, lack of any disability, being a resident of Borujen city, and receiving regular follow-up care of the treatment center.
Data collection tool used in the present study was the QOL questionnaire 36 item short-form health survey (SF-36). The original version of this questionnaire was released in 1988 and the final version was released in 1990. Currently, the SF-36 questionnaire, due to be short and comprehensive, is the most widely used tool for measuring QOL in the world. It consists of statements in the form of physical functioning subscales, physical role, body pain, general health, vitality, social functioning, emotional role, psychological health, and one statement on change in health status.16,17
To respond to questions from the 5 point Likert scale, ranging from excellent to poor, was used. The maximum score for each section or subscale was 100 and the minimum was 0. High scores indicate better health status and lower scores indicate poorer health status. The mean score of QOL dimensions was 50, and scores higher and lower than 50 indicated high and l ow performances, respectively. Numerous studies performed in different countries have confirmed the validity and reliability of the SF-36 questionnaire. In the study of Montazeri et al.18, the reliability and internal consistency of this questionnaire was assessed using statistical analysis. This analysis showed that, except the vitality scale (a = 0.65), the scales of the inventory were in the minimum range of the standard reliability coefficients, ranging from 0.77 to 0.9.18 Therefore, to determine the internal consistency and reliability of the questionnaire, the Cronbach's alpha coefficient was used (r = 0.83). To gather the data, first the demographic characteristics questionnaire including age, education level, occupation, income, marital status, accommodation, underlying disease, and the effects of menopause was completed. Subsequently, the QOL questionnaire (SF-36), consisting of eight elements, of physical functioning, role functioning, body pain, general health, life and vitality, social functioning, emotional functioning, and mental health in the four psychological, social, physical movement, and environmental domains, was completed through interviews and collected. Data were analyzed using SPSS software (version 16; SPSS Inc., Chicago, IL, USA), one-way analysis of variance (ANOVA), t-test, and Pearson correlation coefficient.
Results
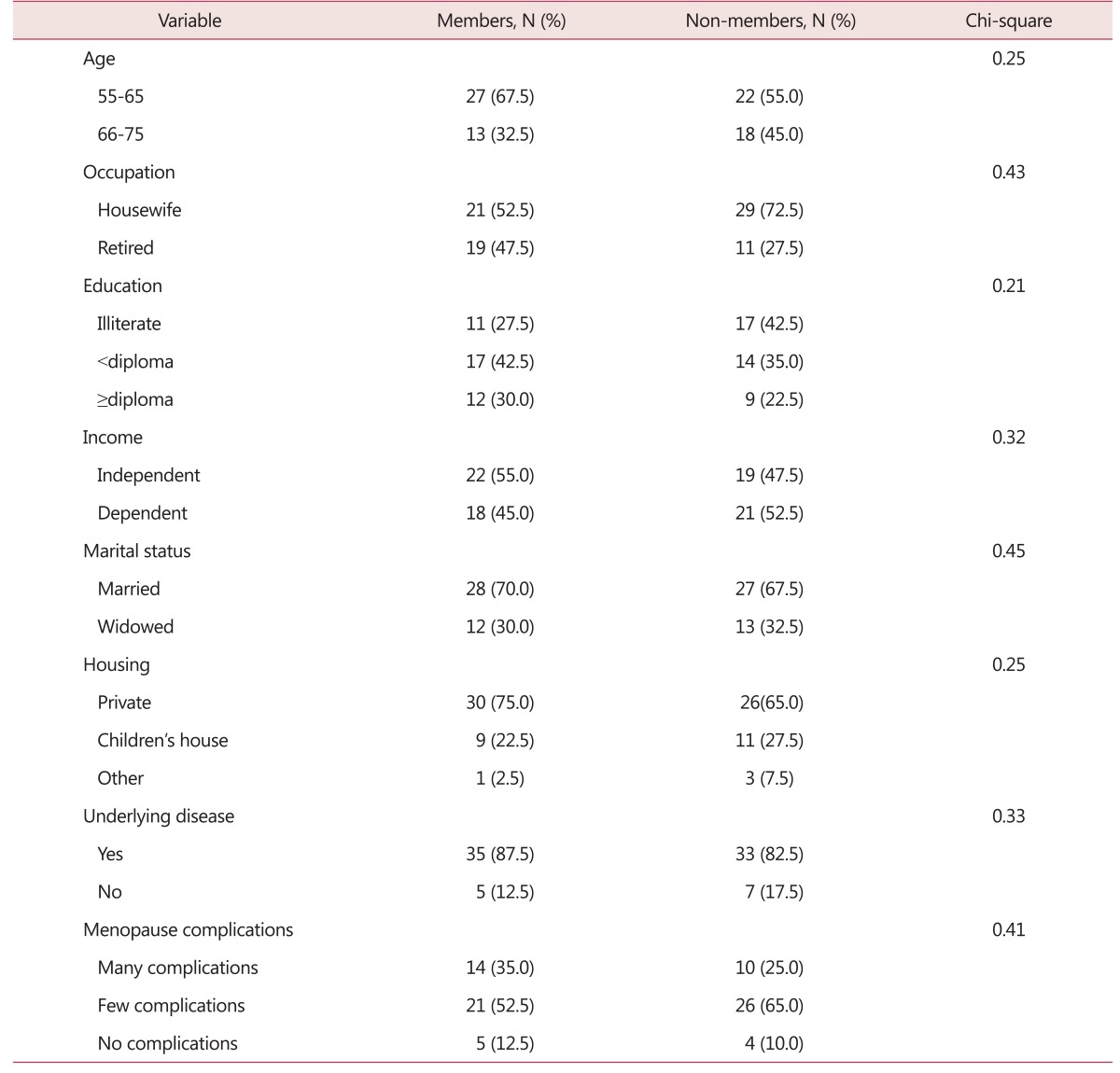
According to the study results, the mean age of the participants was 57.70 ± 0.5 years. Moreover, 52.5% of the members of the association and 72.5% of the non-members were housewives. Regarding the education level, 42.5% of members had diploma and 42.5% of non-members were illiterate. In both groups, the majority of women was living in a private household. Chi-square and Mann-Whitney test showed no statistically significant differences between members and non-members, with regard to age, occupation, education, income, marital status, accommodation, underlying disease, and menopausal symptoms (P > 0.05). Therefore, these variables were the same in both groups. Additional information about the status of the subjects is shown in Table 1.
Table 1. Comparison of the demographic variables of menopausal women, members and non-members of the elderly association.
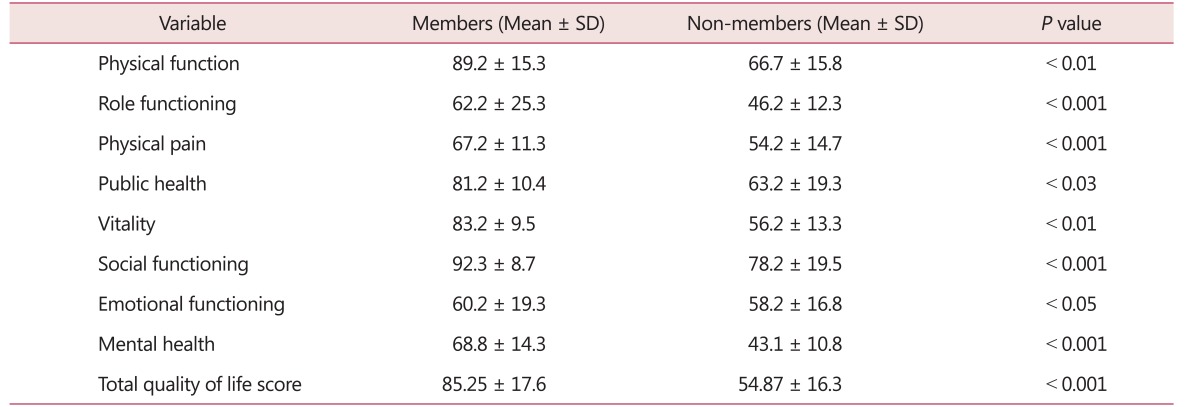
In terms of the QOL dimensions and subscales, findings indicated that the mean total score of QOL of the group of members was higher than that of the non-members group (85.25 ± 17.16). Student's t-test showed a significant relationship between mean QOL score and membership of the association (P < 0.05). The highest mean score and standard deviation were that of the social functioning of the members of the association (92.3 ± 8.7) and the lowest mean (43.1 ± 10.8) was related to the mental health of the non-members (Table 2).
Table 2. Comparison of the mean quality of life in postmenopausal women members and non-members of the elderly association.
SD: standard deviation
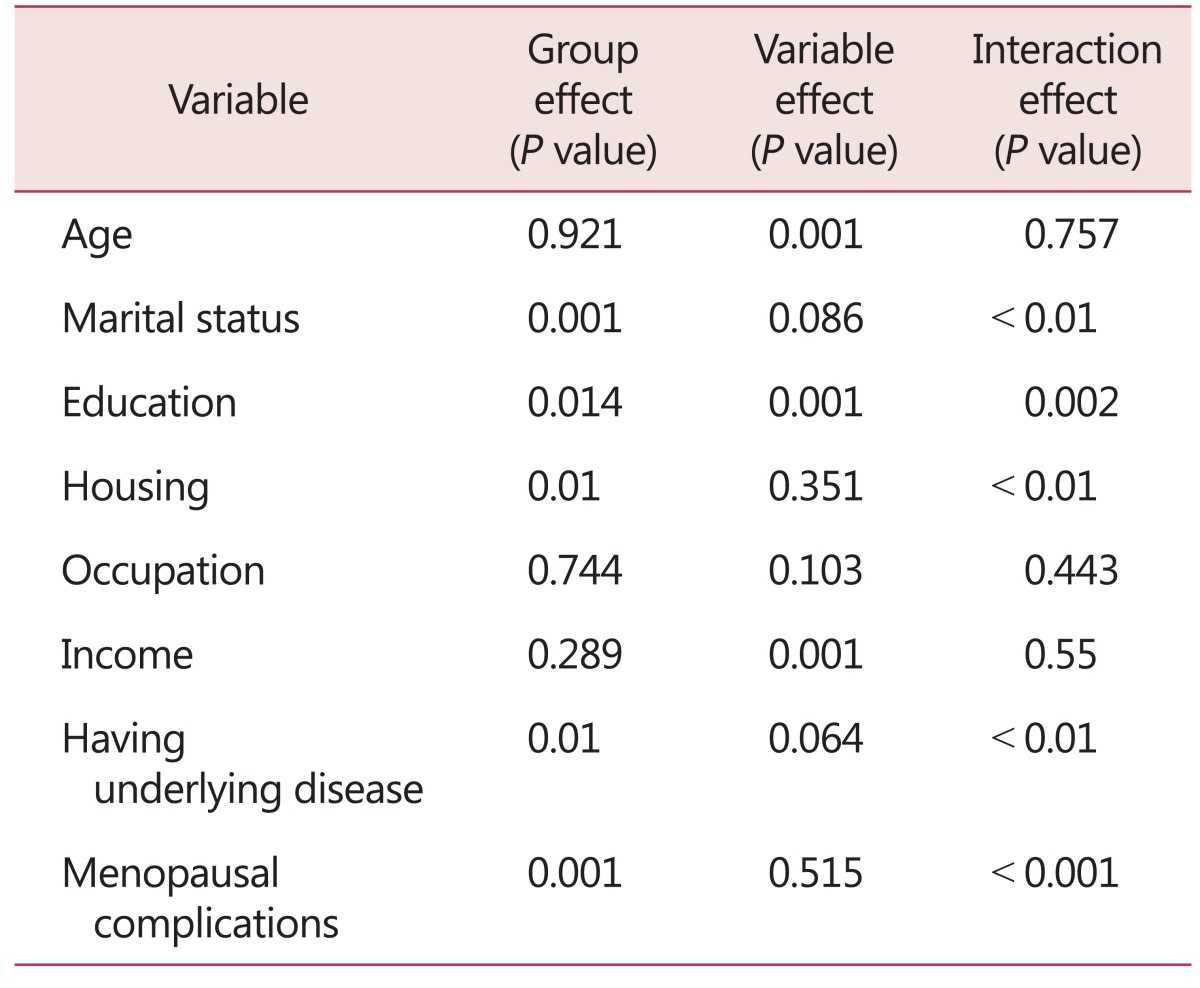
Two-way ANOVA results showed statistically significant differences in mean QOL of postmenopausal women, according to membership and marital status (P < 0.01), housing conditions (P < 0.01), underlying disease (P < 0.01), and menopause complications (P < 0.001) (Table 3).
Table 3. Comparison of the two groups of postmenopausal women in terms of quality of life associated with demographic variables.
Discussion
The results showed that the mean age of menopause was 57.7 years. The average age of menopause differs in different countries and cultures. In the study of Nayak et al.19, the mean age of menopause was 50.3 years. In the study by Abdi and Solhi,20 a mean age of 48.25 years was reported. In a previous study, QOL of the elderly was at a moderate level. Since women spend one third of their lives in the postmenopausal period, preparing women from the beginning of middle-age ensures the success of the elderly health program.21 The mean overall QOL among married women with private households, income, no history of chronic disease, and reduced menopausal symptoms was much higher than others. Uguz et al.22, in their study, also confirmed this finding and showed that QOL is associated with these variables. Williams et al.23, stated that good economic conditions followed by the improvement of related items, such as having a private household, can make it easier to cope with the changes during menopause. This was in agreement with the findings of the current study. What is certain is that the QOL of people in this period, in addition to the complications of menopause, is influenced by physical, psychological, social, and economic factors.23 In this regard, the findings of studies by Argyriou et al.24, Alipur et al.25, and Heidari and Shahbazi,26 were consistent. The present study results were inconsistent with that of Krajewska-Ferishah et al.27 In their study, the QOL of women was higher. The reason for this difference may be differences in government support systems, living conditions, and lifestyles.27 Hamidizadeh et al.28, were able to increase the QOL of the elderly through moderate exercise training. In this study, noticeable increases were observed in physical functioning, general health, and social functioning.28 This was in accord with the present study results. The study by Alipur et al.25, investigated the role of social support in the QOL of the elderly and showed that the QOL in men was higher than women, and social, emotional, functional, and structural support had an important role in improving QOL. The results of the study by Dickson et al.29, showed that self-care programs, exercise, and work to increase the QOL.
Conclusion
If the elderly learn to spend the rest of their life in peace and comfort, they can better balance the factors that reduce their QOL. Improving QOL through relying on social assistance results in an active and productive aging. Considering the importance of the elderly in the community. It is of great importance that we empower them. Thus, the health and treatment burden that is imposed on the society will be decreased.
Acknowledgement
We thank all elderly participating in the research project.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Park S, Yang MJ, Ha SN, Lee JS. Effective anti-aging strategies in an era of super-aging. J Menopausal Med. 2014;20:85–89. doi: 10.6118/jmm.2014.20.3.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meeta, Digumarti L, Agarwal N, Vaze N, Shah R, Malik S. Clinical practice guidelines on menopause: An executive summary and recommendations. J Midlife Health. 2013;4:77–106. doi: 10.4103/0976-7800.115290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tandon VR, Mahajan A, Sharma S, Sharma A. Prevalence of cardiovascular risk factors in postmenopausal women: A rural study. J Midlife Health. 2010;1:26–29. doi: 10.4103/0976-7800.66993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruan X, Jin J, Hua L, Liu Y, Wang J, Liu S. The prevalence of metabolic syndrome in Chinese postmenopausal women and the optimum body composition indices to predict it. Menopause. 2010;17:566–570. doi: 10.1097/gme.0b013e3181c8f4e1. [DOI] [PubMed] [Google Scholar]
- 5.Lejsková M, Alušík S, Suchánek M, Zecová S, Pitha J. Menopause: clustering of metabolic syndrome components and population changes in insulin resistance. Climacteric. 2011;14:83–91. doi: 10.3109/13697131003692745. [DOI] [PubMed] [Google Scholar]
- 6.Pandey S, Srinivas M, Agashe S, Joshi J, Galvankar P, Prakasam CP, et al. Menopause and metabolic syndrome: A study of 498 urban women from western India. J Midlife Health. 2010;1:63–69. doi: 10.4103/0976-7800.76214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The recent review of the genitourinary syndrome of menopause. J Menopausal Med. 2015;21:65–71. doi: 10.6118/jmm.2015.21.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nikpour S, Haghani H. The effect of exercise on quality of life in postmenopausal women referred to the bone densitometry centers of Iran University of Medical Sciences. J Midlife Health. 2014;5:176–179. doi: 10.4103/0976-7800.145156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shariatpanahi SA, Hajikazemi E, Nikpour S, Fghanipour S, Hosseini AF. Effect of yoga exercises on quality of life of postmenopausal women. HealthMed. 2013;7:1266–1273. [Google Scholar]
- 10.Elavsky S. Physical activity, menopause, and quality of life: the role of affect and self-worth across time. Menopause. 2009;16:265–271. doi: 10.1097/gme.0b013e31818c0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heidari M, Borujeni MG, Naseh L. Comparison of self-efficacy and loneliness between community-dwelling & institutionalized older people. Salmand. 2016;11:142–151. [Google Scholar]
- 12.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karaçam Z, Seker SE. Factors associated with menopausal symptoms and their relationship with the quality of life among Turkish women. Maturitas. 2007;58:75–82. doi: 10.1016/j.maturitas.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Van Malderen L, Mets T, Gorus E. Interventions to enhance the Quality of Life of older people in residential long-term care: a systematic review. Ageing Res Rev. 2013;12:141–150. doi: 10.1016/j.arr.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Kwak EK, Park HS, Kang NM. Menopause knowledge, attitude, symptom and management among midlife employed women. J Menopausal Med. 2014;20:118–125. doi: 10.6118/jmm.2014.20.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darvishpour A, Abed Saiidi J, Delavar A, Saiidozakerin M. Tools for assessment of health and quality of life in older adults. J Shahid Beheshti Med Sci Uni. 2009;33:162–173. [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The short form health survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14:875–882. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 19.Nayak G, Kamath A, Kumar PN, Rao A. Effect of yoga therapy on physical and psychological quality of life of perimenopausal women in selected coastal areas of Karnataka, India. J Midlife Health. 2014;5:180–185. doi: 10.4103/0976-7800.145161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdi N, Solhi M. Quality of life in postmenopausal women in Tehran. Iran J Health Educ Health Promot. 2014;2:87–96. [Google Scholar]
- 21.Dvivedi J, Kaur H, Dvivedi S. Effect of 1 week '61-points relaxation training' on cold pressor test induced stress in premenstrual syndrome. Indian J Physiol Pharmacol. 2008;52:262–266. [PubMed] [Google Scholar]
- 22.Uguz F, Sahingoz M, Gezginc K, Ayhan MG. Quality of life in postmenopausal women: the impact of depressive and anxiety disorders. Int J Psychiatry Med. 2011;41:281–292. doi: 10.2190/PM.41.3.g. [DOI] [PubMed] [Google Scholar]
- 23.Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009;62:153–159. doi: 10.1016/j.maturitas.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Argyriou AA, Iconomou G, Ifanti AA, Karanasios P, Assimakopoulos K, Makridou A, et al. Religiosity and its relation to quality of life in primary caregivers of patients with multiple sclerosis: a case study in Greece. J Neurol. 2011;258:1114–1119. doi: 10.1007/s00415-010-5894-8. [DOI] [PubMed] [Google Scholar]
- 25.Alipur F, Sajjadi H, Foruzan A, Biglarian A. Role of social quiet on elder's quality of life. Soc Welfare Quart. 2010;4:147–165. [Google Scholar]
- 26.Heidari M, Shahbazi S. Effect of self-care training program on quality of life of elders. Iran J Nurs. 2012;25:1–8. [Google Scholar]
- 27.Krajewska-Ferishah K, Krajewska-Kułak E, Terlikowski S, Wiktor H, Van Damme-Ostapowicz K, Chadzopulu A, et al. Analysis of quality of life of women in menopause period in Poland, Greece, Belarus and Belgium using MRS Scale. A multicenter study. Adv Med Sci. 2010;55:191–195. doi: 10.2478/v10039-010-0042-3. [DOI] [PubMed] [Google Scholar]
- 28.Hamidizadeh S, Ahmadi F, Aslani Y, Eatemadifar SH. Assessment the effect of group exercise on quality of life in older adults. J Saddughy Uni Yazd. 2009;16:81–86. [Google Scholar]
- 29.Dickson VV, Howe A, Deal J, McCarthy MM. The relationship of work, self-care, and quality of life in a sample of older working adults with cardiovascular disease. Heart Lung. 2012;41:5–14. doi: 10.1016/j.hrtlng.2011.09.012. [DOI] [PubMed] [Google Scholar]