Abstract
Descemet's membrane detachment (DMD) though uncommon in the present day scenario of advancing surgical techniques is a significant complication that requires prompt diagnosis and management. A middle-aged man presented to our hospital with poor gain of vision following cataract surgery. There was significant corneal oedema with DMD which was confirmed on anterior segment optical coherence tomography. We describe a modified continuous intraoperative-guided approach for the management of DMD in cases with oedematous hazy corneas. The aim of this technique is to allow early reattachment of Descemet's membrane in chronic cases where fluid pockets prevent reattachment of the posterior layer of cornea. Our technique involves the use of full thickness stromal vent incisions in the paracentral cornea along with intracameral isoexpansile concentration of gas for the successful settlement of the detached Descemet's membrane.
Background
Descemet's membrane detachment (DMD) is a well-recognised complication of cataract surgery and other intraocular surgeries. The detachment of the Descemet's-endothelial complex from the stroma leads to endothelial pump failure resulting in corneal oedema.1 While small, subclinical detachments may go undetected as they resolve spontaneously, larger untreated DMDs cause severe bullous keratopathy. Prompt recognition in the immediate postoperative period and optimal management ensures good functional and anatomical outcome.
On slit lamp biomicroscopy, DMD appears as a translucent membrane in the anterior chamber separated from the posterior stroma. The overlying corneal oedema may preclude visualisation of DMD at times, which warrants a high index of suspicion in such cases when the postoperative corneal oedema is nonresolving in nature. Newer surgical tools such as anterior segment optical coherence tomography (ASOCT) now enable early recognition of DMD in oedematous postoperative corneas. The need for management and the type of procedure employed depend on the extent of the detachment, the type and the effect it has on the visual function of the individual. Various methods to manage a DMD have been described in the literature depending on the clinical evaluation and assessment.2–4 We describe here an improvised surgical technique where a case of postcataract surgery DMD with corneal oedema was managed successfully by pneumodescemetopexy (with intracameral isoexpansile perfluoropropane gas) under the guidance of intraoperative optical coherence tomography (iOCT) aided with corneal stromal vent incisions.
Case presentation
A 53-year-old man presented to our Cornea Clinic services with a history of decrease in visual acuity OD since one and half months. The patient gave a history of phaecoemulsification in the right eye 6 weeks back in a private hospital at his native place with no improvement in the best-corrected visual acuity postsurgery. He also gave a history of air injection in the eye 2 days postsurgery, with no further improvement, following which he was referred to a higher centre for further management.
On detailed ophthalmic evaluation at our centre, the patient had a best-corrected visual acuity (BCVA) OD 1/60, projection of rays being accurate in all quadrants; OS 6/9. On slit-lamp biomicroscopy of the right eye (OD), there was conjunctival congestion, with diffuse limbus to limbus stromal and epithelial oedema and few bullae in the temporal third of the cornea (figure 1). The pupil was circular, regular, with brisk direct and consensual reflex to light. The patient was pseudophakic. A detailed fundus evaluation was not possible, and B-scan revealed an anechoic posterior chamber. The left eye (OS) had immature senile cataract with nuclear sclerosis grade II and a healthy fundus.
Figure 1.
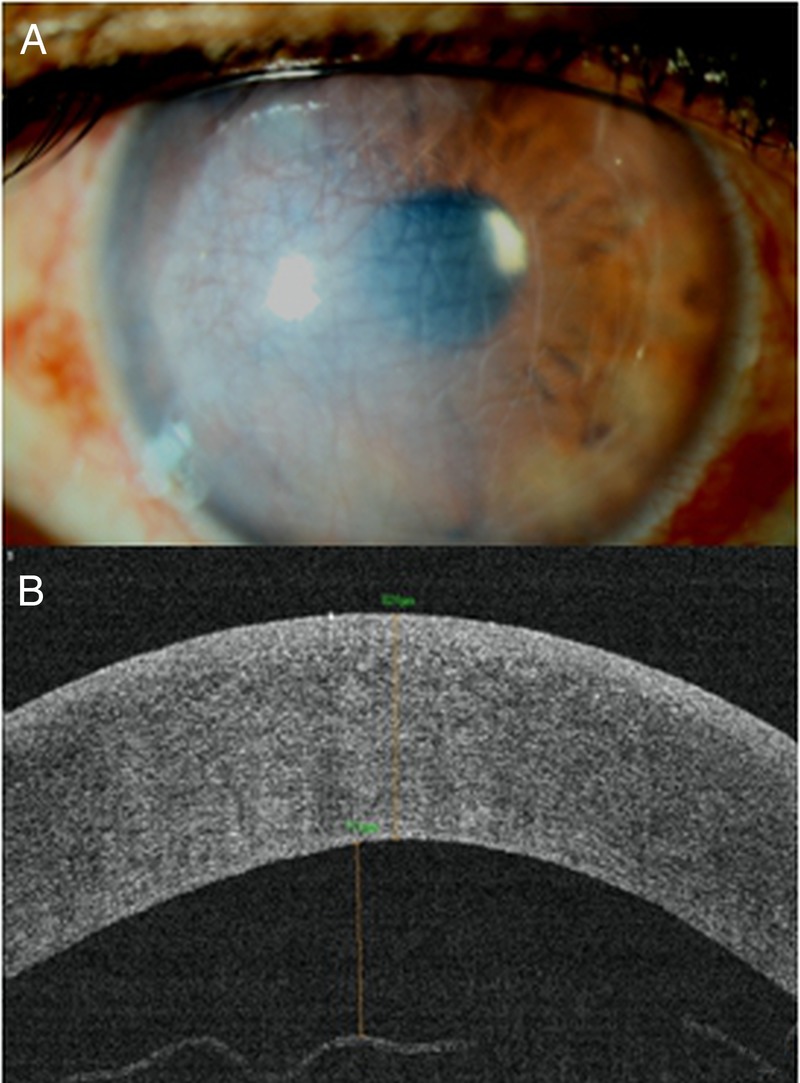
(A) Slit lamp biomicroscopy clinical photograph of the right eye showing diffuse corneal oedema. (B) Anterior segment OCT picture which confirms a detached Descemet's membrane with an increased thickness of the cornea representing oedema.
Investigations
An ultrasonic pachymetry was performed, and OD central corneal thickness was 820 μm and OS was 466 μm. The central corneal thickness on ASOCT was 824 μm with the maximum height of DMD noted to be 711 μm (extending from 6’o clock–12’o clock position) (figure 1). The endothelial cell count of the affected eye could not be captured on a specular microscope but was 2052 cells/mm2 in the fellow eye.
Treatment
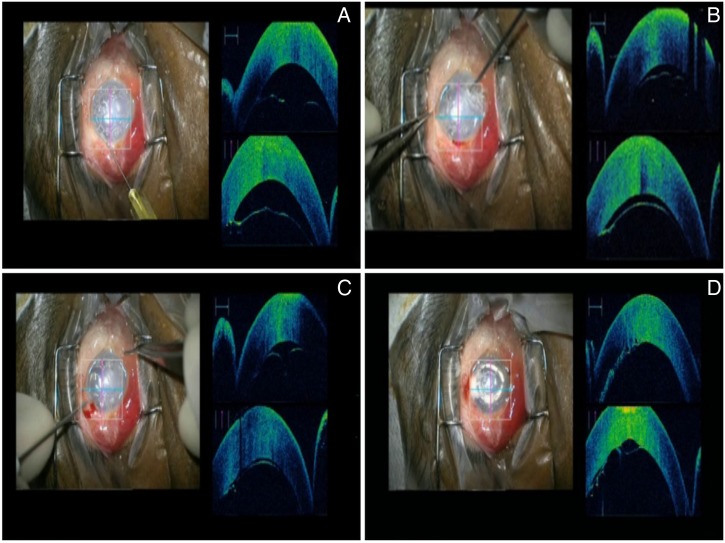
In view of subtotal DMD of more than 6 weeks duration and a failed intervention with intracameral air injection for DMD settlement that had been performed elsewhere, the patient was planned for an immediate surgical intervention under peribulbar block with the guidance of an iOCT microscope (OPMI LUMERA 700 and RESCAN 700; Carl Zeiss, Meditec, Germany). The eye was cleaned and draped under strict aseptic precautions. Anterior chamber paracentesis was carried out using a 30 gauge needle (figure 2) between 9 and 10 o'clock position. Pneumodescemetopexy was carried out by injecting an isoexpansile concentration of perfluoropropane gas (14%) into the anterior chamber using a 30 G needle under the guidance of an iOCT microscope. The iOCT images showed persistent detachment following the pneumodescemetopexy (figure 2) due to fluid collection between the stroma and the detached DM. Hence a full thickness stromal paracentral vent incisions concentric to the limbus was made using a 20 gauge microvitreoretinal blade under iOCT microscope guidance at the inferonasal quadrant to allow efflux of the fluid trapped between the detached Descemet's membrane and the host corneal stroma. An instantaneous decrease in the height of the detached membrane was noted intraoperatively with fluid remaining in the other quadrants. Hence three more paracentral full thickness stromal vent incisions were made to allow fluid efflux and facilitate the settlement of the refractory DMD. Near total settlement of the DMD was achieved. Further intracameral isoexpansile gas (14% perfluoropropane) was injected to ensure a complete fill of the anterior chamber which was maintained for 10 min. The gas was then released in a controlled manner, and a gas fill of approximately two-thirds of the anterior chamber was maintained. Sufficient tamponade was ensured to allow adequate attachment of the Descemet's membrane. A small area of residual detachment was noted to persist in the central region (figure 2D). A soft bandage contact lens was placed on the cornea. Strict supine position was advised postoperatively for 24 hours to ensure the attachment of Descemet's membrane postoperatively. The patient was maintained on postoperative regimen of topical antibiotic drops, antiglaucoma agents, steroid formulations and hyperosmotic drops.
Figure 2.
The intraoperative ASOCT-guided surgical procedure. (A) Anterior chamber paracentesis using a 30 G needle followed by intracameral injection of isoexpansile perfluoropropane gas. (B and C) Vent incisions are made in the paracentral cornea using a 20 gauge microvitreoretinal blade allowing release of fluid. (D) Intraoperative settled Descemet's membrane with residual small detachment.
Outcome and follow-up
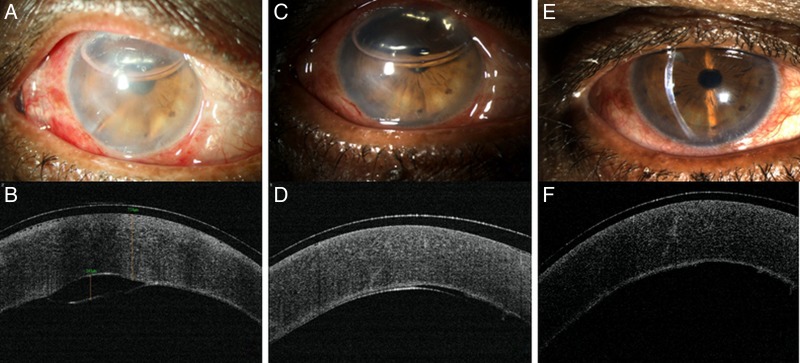
On the first postoperative day, the visual acuity of the patient was recorded to be 6/60 using Snellen's chart, and an intraocular pressure of 14 mm Hg by non-contact tonometry; a gas bubble was seen in the anterior chamber with a small area of DMD (figure 3A). On day 3, the vision further improved to 6/24, with an intraocular pressure of 12 mm Hg and an attached DM confirmed on anterior segment OCT imaging (figure 3B). The vision further improved to 6/12 on day 14 with an attached Descemet's membrane and minimal anterior chamber reaction (figure 3C). Confocal microscopy revealed an endothelial count of 640 cells/mm2 in the operated eye.
Figure 3.
(A) Postoperative day 1 slit lamp biomicroscopy clinical photograph showing a decrease of corneal oedema with a gas bubble filling two-third of the anterior chamber. (B) Anterior segment OCT on first postoperative day showing a small residual DMD. (C and D) Slit lamp biomicroscopy picture on postoperative day 3 shows a clearer cornea with a completely attached Descemet's membrane as confirmed on ASOCT. (E and F) Slit lamp biomicroscopy picture on postoperative day 14 shows a clear cornea with resolved oedema and attached Descemet's membrane.
Discussion
DMD is an entity which has been described as a complication following intraocular procedures5–7 such as cataract surgeries, trabeculectomy, cyclodialysis, surgical iridectomies6 and following deep anterior lamellar keratoplasties (DALK).8 The common causes for DMD during or following a cataract surgery include inappropriate incision construction in the anterior clear cornea, use of blunt blades for incision construction, excessive manipulation and instrumentation, intraoperative shallowing of anterior chamber, misdirection of cannulas while injecting intracameral drugs or viscoelastics and difficult IOL insertion.9 In the present case, the risk factor was probably related to prolonged duration of surgery as per the clinical history which suggests extensive manipulation and instrumentation as a potential cause of DMD. Even though recognised early, the DMD continued to persist after an initial air injection suggesting probably an incorrect plane of injection or presence of fluid trapped between the detached Descemet's membrane and the rest of the corneal layers.
The extent of the detachment may range from a small localised area to a visually significant large DMD which requires surgical management. The procedure of choice depends on the site and height of the detachment, the extent of involvement and the duration of DMD. The presence of adhesions with anterior segment structures and scrolled DMDs may further complicate the situation.
The need for surgical intervention arises in cases of large and persistent DMDs which fail to respond to conservative line of treatment. The main aim of the management is to prevent permanent corneal decompensation and stromal scarring thus reducing ocular morbidity.
The literature suggests surgical management of DMD using intracameral injection of 100% air2 or gases such as C3F8 and SF6.10 In long standing cases, transcorneal suturing has also been attempted to improve the chances of attachment.11 But less is discussed in the literature regarding the management of DMD after a failed pneumodescemetopexy. Datar et al12 have reported successful management of a single case of recurrent DMD with repeat descemetopexy with C3F8 gas injection. Jain et al13 conducted a multicentric trial in 13 eyes and suggested that repeat descemetopexy should be attempted in postcataract surgery DMD before planning for procedures such as keratoplasty. The most important reported cause for failure of descemetopexy is the entrapment of fluid in the supra-Descemet's space. Venting incisions14 15 have been reported to successfully drain this fluid, leading on to complete re-attachment of the detached Descemet's membrane. The use of modern tools such as ASOCT can help in overcoming the challenge of identifying a DMD in oedematous cornea where visualisation on slit lamp biomicroscopy alone is difficult. But with the advent of iOCT, the management of DMD has further been revolutionised. Intraoperative visualisation during surgery with iOCT allows for the identification of the correct plane for instrumentation and ensures membrane attachment intraoperatively.
The integration of OCT in the surgical ophthalmic microscope helps in on-table assessment of the ocular structures and thus saves time and improves the surgical efficiency and outcomes. It has been a useful tool for guiding anterior segment procedures such as cases of acute corneal hydrops managed with corneal stab incisions and intracameral air injection.16 Its use has been evaluated in lamellar procedures including Descemet's stripping automated endothelial keratoplasty to assess attachment of donor lenticule and the interface changes.17 18 As a result, the precision of the surgical procedure improves and better anatomical outcomes are ensured. The use of iOCT for intraoperative real-time imaging has been reported for the management of DMD in a post-DALK patient.19 Along with decreasing the operating time and the need for manipulation, it may result in better functional and visual outcomes as compared to conventional procedures without the aid of such advanced technology. It has also been utilised in other procedures such as corneal collagen cross linking20 21 and Laser in situ keratomileusis (LASIK).22 In today's era of ever improving technology, the iOCT integrated in the operating microscope has evolved as a handy tool which has been used in anterior and posterior segment surgeries.23–25 This becomes particularly important in cases where DMD is long standing and endothelial counts may already be compromised. A 20 gauge microvitreoretinal (MVR) surgical blade was used to create multiple stromal punctures to help drain the fluid pockets along with which an intracameral isoexpansile injection of perfluoropropane gas provided sufficient tamponade.
The initial failure of Descemet's attachment following an intracameral air injection can be attributed to the fluid entrapment in the supra-Descemet's space. Thus, venting incision with gas tamponade using C3F8 was performed to treat DMD in our case. The advantage of C3F8 as a tamponade agent is the longer half-life which helps improve the success rate of re-attachment. Also, its safety has been evaluated in the literature previously ensuring no endothelial cell loss and intraocular pressure fluctuations.26 We conclude that though rare, DMD does result in significant ocular morbidity. The present case presented 6 weeks after cataract surgery with severe corneal oedema making the DM visualisation difficult. The use of iOCT aids the ability of surgeon in the management of complex situations such as this and helps in better management. Thus, we report the usefulness of continuous monitoring using iOCT in the management of recurrent or refractory DMD before going for other procedures such as suturing or keratoplasty.
Patient's perspective.
I did not gain vision after the first surgery performed for cataract and even after a repeat procedure in the same eye. So I was referred for further management to higher centre. After a procedure here which was described to me as a gas injection in the affected eye, I have noticed an improvement in the vision and decrease of pain.
Learning points.
Full thickness stromal vent incisions along with intracameral isoexpansile gas injection helps in reattachment of the Descemet's membrane in the cases of refractory Descemet's membrane detachment.
This technique under the guidance of an intraoperative optical coherence tomography is useful in long-standing cases where oedematous cornea hampers optimal visualisation.
Footnotes
Contributors: AS involved in acquisition of data, analysis and interpretation and drafting the article and final approval of the manuscript. MV involved in conception and design, drafting of the article, critical revision and final approval of the manuscript. SS involved in acquisition of data, analysis and interpretation, drafting and final approval of the manuscript. SD involved data analysis and interpretation, drafting and final approval of the manuscript. All authors agree to be accountable for the article and ensure that all questions regarding the accuracy and integrity of the article are investigated and resolved.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Marcon AS, Rapuano CJ, Jones MR et al. Descemet's membrane detachment after cataract surgery: management and outcome. Ophthalmology 2002;109:2325–30. [DOI] [PubMed] [Google Scholar]
- 2.Mackool RJ, Holtz SJ. Descemet membrane detachment. Arch Ophthalmol 1977;95:459–63. [DOI] [PubMed] [Google Scholar]
- 3.Assia EL, Levkovich-Verbin H, Blumenthal M. Management of Descemet's membrane detachment. J Cataract Refract Surg 1995;21:714–17. [DOI] [PubMed] [Google Scholar]
- 4.Jain R, Murthy SI, Basu S et al. Anatomic and visual outcomes of descemetopexy in post-cataract surgery Descemet's membrane detachment. Ophthalmology 2013;120:1366–72. 10.1016/j.ophtha.2012.12.043 [DOI] [PubMed] [Google Scholar]
- 5.Sugar HS. Prognosis in stripping of Descemet's membrane in cataract extraction. Am J Ophthalmol 1967;63:140–3. [DOI] [PubMed] [Google Scholar]
- 6.Donzis PB, Karcioglu ZA, Insler MS. Sodium hyaluronate (Healon®) in the surgical repair of Descemet's membrane detachment. Ophthalmic Surg 1986;17:735–7. [PubMed] [Google Scholar]
- 7.Ostberg A, Tornqvist G. Management of detachment of Descemet's membrane caused by injection of hyaluronic. Ophthalmic Surg 1989;20:885–6. [PubMed] [Google Scholar]
- 8.Hirano K, Kojima T, Nakamura M et al. Triple anterior chamber after full-thickness lamellar keratoplasty for lattice corneal dystrophy. Cornea 2001;20:530–3. [DOI] [PubMed] [Google Scholar]
- 9.Mannan R, Pruthi A, OmParkash R et al. Descemet membrane detachment during foldable intraocular lens implantation. Eye Contact Lens 2011;37:106–8. 10.1097/ICL.0b013e31820c6fe7 [DOI] [PubMed] [Google Scholar]
- 10.Kim T, Hasan SA. A new technique for repairing Descemet membrane detachments using intracameral gas injection. Arch Ophthalmol 2002;120:181183. [DOI] [PubMed] [Google Scholar]
- 11.Amaral CE, Palay DA. Technique for repair of Descemet's membrane detachment. Am J Ophthalmol 1999;127:88–90. [DOI] [PubMed] [Google Scholar]
- 12.Datar S, Kelkar A, Jain AK et al. Repeat Descemetopexy after Descemet's membrane detachment following phacoemulsification. Case Rep Ophthal 2014;5:203–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain R, Mohan N. Outcomes of repeat descemetopexy in post-cataract surgery Descemet membrane detachment. Am J Ophthalmol 2014;157:571–5.e1–2 10.1016/j.ajo.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 14.Ghaffariyeh A, Honarpisheh N, Chamacham T. Supra-Descemet's fluid drainage with simultaneous air injection: an alternative treatment for Descemet's membrane detachment. Middle East Afr J Ophthalmol 2011;18:189–91. 10.4103/0974-9233.80712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhatia HK, Gupta R. Delayed-on set Descemet membrane detachment after uneventful cataract surgery treated by corneal venting incision with air tamponade: a case report. BMC Ophthalmol 2016;16:35 10.1186/s12886-016-0212-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vajpayee RB, Maharana PK, Kaweri L et al. Intrastromal fluid drainage with air tamponade: anterior segment optical coherence tomography guided technique for management of acute cornealhy drops. Br J Ophthalmol 2013;97:834–6. [DOI] [PubMed] [Google Scholar]
- 17.Titiyal JS, Kaur M, Falera R et al. Evaluation of time to donor lenticule apposition using Intraoperative optical coherence tomography in Descemet stripping automated endothelial keratoplasty. Cornea 2016;35:477–81. 10.1097/ICO.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 18.Juthani VV, Goshe JM, Srivastava SK et al. The association between transient interface fluid on intraoperative OCT and textural interface opacity following DSAEK surgery in PIONEER study. Cornea 2014;33:887–92. 10.1097/ICO.0000000000000209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma N, Aron N, Kakkar P et al. Continuous intraoperative OCT guided management of post-deep anterior lamellar keratoplasty Descemet's membrane detachment. Saudi J Ophthalmol 2016;30:133–6. 10.1016/j.sjopt.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pahuja N, Shetty R, Jayadev C et al. Intraoperative optical coherence tomography using the RESCAN700; preliminary results in collagen crosslinking. Biomed Res Int 2015;2015:572698 10.1155/2015/572698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rechichi M, Mazzotta C, Daya S et al. Intraoperative OCT pachymetry in patients undergoing dextran-free riboflavin UVA accelerated corneal collagen crosslinking. Curr Eye Res 2016;41:1310–5. 10.3109/02713683.2015.1118130 [DOI] [PubMed] [Google Scholar]
- 22.Ye C, Yu M, Jhanji V. Stromalbed thickness measurement during laser in situ keratomileusis using intraoperative optical coherence tomography. Cornea 2015;34:387–91. 10.1097/ICO.0000000000000345 [DOI] [PubMed] [Google Scholar]
- 23.Ehlers JP, Tam T, Kaiser PK et al. Utility of intraoperative optical coherence tomography during vitrectomy surgery for vitreomacular traction syndrome. Retina (Philadelphia, Pa) 2014;34:1341–6. 10.1097/IAE.0000000000000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ehlers JP, Xu D, Kaiser PK et al. Intrasurgical dynamics of macular hole surgery: an assessment of surgery-induced ultrastructural alterations with intraoperative optical coherence tomography. Retina (Philadelphia, Pa) 2014;34:213–21. 10.1097/IAE.0b013e318297daf3 [DOI] [PubMed] [Google Scholar]
- 25.Scorcia V, Busin M, Lucisano A et al. Anterior segment optical coherence tomography-guided big-bubble technique. Ophthalmology 2013;120:471–6. 10.1016/j.ophtha.2012.08.041 [DOI] [PubMed] [Google Scholar]
- 26.Macsai MS, Gainer KM, Chisholm L. Repair of Descemet's membrane detachment with perfluoropropane (C3F8). Cornea 1998;17:129–34. [DOI] [PubMed] [Google Scholar]