Abstract
Cryptococcus neoformans is the most frequent cause of fungal meningitis in humans. Cryptococcus affects people of all ages and has a worldwide distribution. It is the fourth most common infection in AIDS (CD4 counts <100/mm3). Cases also occur in patients with other forms of immunosuppression and in apparently immunocompetent individuals. Chronic high-dose steroid may precipitate such an immunocompromised state and thus create susceptibility to fungal infections. In our case, we describe a 14-year-old boy who was on steroids for tubercular meningitis for a period of 8 weeks after which he developed cryptococcal meningitis. Attention is drawn to the increasing number of reported cases of this disease which have been associated with steroid therapy and this possibility should be remembered when investigating patients with tubercular meningitis especially if they are being treated with steroids.
Background
Cryptococcus neoformans is an opportunistic infection. It is the fourth most common infection in AIDS with CD4 counts<100/mm3 1 but has also been seen in patients on prolonged corticosteroids which account for about 1/3rd cases without HIV. High-steroid dose can decrease migration and inhibit chemotaxis of neutrophils, inhibit phagocytosis, intracellular killing and decrease production of proinflammatory cytokines.1 We are reporting a case of cryptococcal meningitis in a HIV seronegative 14-year-old boy who was being treated on steroids for tubercular meningitis.
Case presentation
A 14-year-old boy (weight 39 kgs) presented with low grade fever, headache, cough with expectoration and dizziness for 20 days. There was history of one episode of generalised tonic–clonic seizure. There was no history of anorexia, weight loss or focal neurological deficit. There was no history of seizure and family history were unremarkable. On examination, he was conscious, oriented, moderately built and nourished. Patient was afebrile and haemodynamically stable. Respiratory examination showed decreased air entry in the left lower zone with an associated dull percussion note. The patient's neck was rigid on neurological examination but with negative Kernig's sign; however, rest of the systemic examination was normal.
Investigations
On laboratory investigations, complete haemogram, liver function tests, kidney function tests were within normal range. Sputum for acid-fast bacilli (AFB) was negative. HIV test by ELISA technique and repeated twice was negative; CD3 and CD4 counts were normal.
Chest X-ray showed left-sided pleural effusion. MRI of Brain was normal. Ultrasound scan of the abdomen was normal. Sputum microscopy for AFB was negative (two samples).
Pleural fluid analysis demonstrated total of 80 cells/mL, 64 lymphocytes and 12 neutrophils, protein of 4.7 gm/dL, sugar of 62 mg/dL and adenosine deaminase of 4.1 μ/L. Pleural fluid Gram stain and culture were negative. Pleural fluid tuberculosis PCR was negative.
A cerebrospinal fluid (CSF) examination was carried out which revealed 20 cells/mL of which 16 were lymphocytes and 4 neutrophils, protein of 159 gm/dL, and sugar of 73 mg/dL. The Gram stain, culture, AFB stain, India ink and cryptococcal antigen were negative in CSF. The CSF TB-PCR of the patient came out to be positive for Mycobacterium tuberculosis. The remaining CSF was sent for mycobacterium culture analysis.
A provisional diagnosis of disseminated tuberculosis (pulmonary and meningeal) was made and the patient was started on antitubercular therapy (ATT) category II that is, 2 months of intensive phase comprising of isoniazid, rifampicin, ethambutol, streptomycin and pyrazinamide followed by continuation phase with isoniazid and rifampicin for 7 months thereafter, dexamethasone and sodium valproate.
He was discharged after 7 days of hospital stay. He again presented to the emergency room after 35 days of discharge with symptoms of fever, headache and vomiting for 7 days with a new episode of seizure along with sudden onset weakness on right side and altered sensorium. On reviewing the history, it was found that patient was not taking ATT (did not follow-up at directly observed treatment, short-course centre) following discharge from hospital but was taking dexamethasone and sodium valproate.
On neurological examination, he had altered sensorium with a Glasgow Coma Scale score(GCS) of 9/15. Power in right half of the body was 2/5 and right plantar was extensor. Rest of the systemic examination was unremarkable.
Löwenstein-Jensen medium (LJ) culture which was sent during first admission was positive for M. tuberculosis and drug sensitivity test performed by the conventional method sent at the time of the first admission showed resistance to Isoniazid.
A repeat CSF was carried out which showed no cells, protein 38 mg/dL and sugar of 61 mg/dL. CSF cryptococcal antigen and India ink were negative.
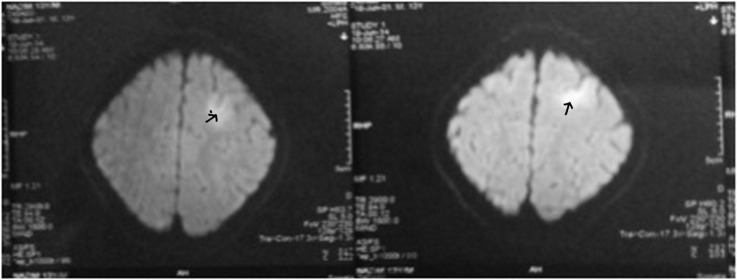
MRI brain this time was suggestive of late subacute infarct in left frontoparietal region with early hydrocephalus (figure 1). As the patient had been non-compliant, he was resumed on category II ATT and kept under observation.
Figure 1.
MRI of the brain (at first presentation): s/o late subacute infarct in left front—parietal region with early hydrocephalus.
One week later, he had an episode of sudden onset of loss of consciousness. He regained consciousness after 3–4 hours. CSF was repeated again which showed total leucocyte count of 20 cells/mL, 18 lymphocytes and 2 neutrophils. Protein of 274 gm/dL, sugar of 70 mg/dL, CSF Cartridge-Based Nucleic Acid Amplification (CB-NAAT) test to look for resistance against isoniazid and rifampicin was negative. However, CSF cryptococcal antigen by latex agglutination and India ink were positive this time.
MRI of the brain showed enhancing nodular lesion seen in left frontal region likely cryptococcoma with areas of restricted diffusion seen in bilateral basal ganglia likely due to ischaemic insult (figure 2).
Figure 2.
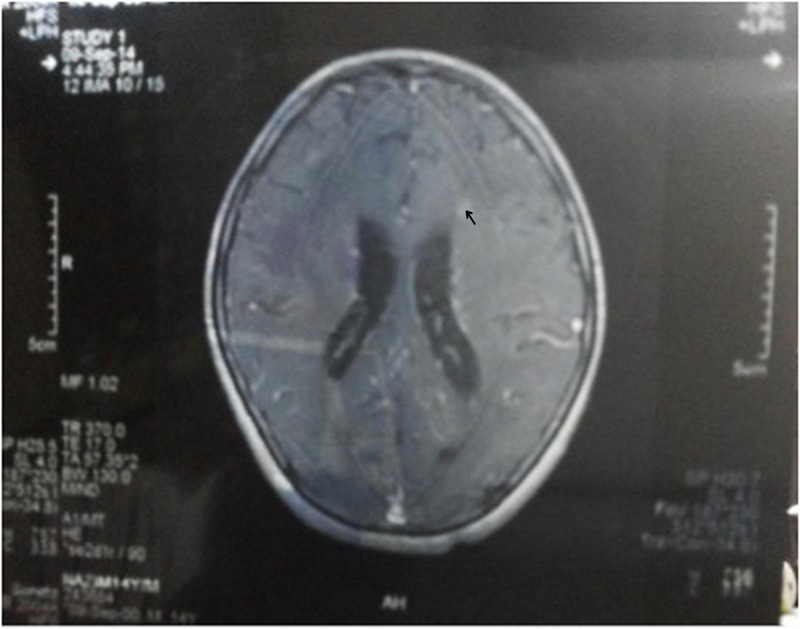
MRI of the brain (after 8 weeks of steroids): enhancing nodular lesion seen in left frontal region likely cryptococcoma.
Differential diagnosis
At the time of the first admission, a provisional diagnosis of disseminated tuberculosis was made, while awaiting the report of LJ medium culture.
However, during the second presentation, apart from the issue of non-compliance, a possibility of multidrug-resistant tuberculosis was kept in mind.
Treatment
First admission: Category II ATT was given that is, isoniazid (200 mg), rifampicin(450 mg), ethambutol(800 mg), pyrazinamide(1000 mg) and streptomycin(0.75 g) along with dexamethasone 4 mg four times a day. The patient was discharged a week later on these drugs along with valproate (400 mg two times a day), tapered dose of dexamethasone (3 mg four times a day) and cerebral decongestants.
Second admission: Category II ATT was restarted along with dexamethasone 2 mg for times a day. Dexamethasone was decreased to 1 mg four times a day after 1 week and then stopped after 1 week. Amphotericin (28 mg once daily) was given for 6 weeks followed by fluconazole (400 mg once daily) with serial renal function test monitoring. Dexamethasone was continued for 2 weeks after starting amphotericin.
After the results of drug sensitivity, since the primary drugs showed resistance to isoniazid, tablet levofloxacin 500 mg once a day was added while rest of the antitubercular drug regimen (isoniazid (200 mg), rifampicin(450 mg), ethambutol (800 mg), pyrazinamide(1000 mg) and streptomycin(0.75 g)) continued on account of monoresistance not classifying as multidrug-resistant tuberculosis.
Outcome and follow-up
The sensorium of the patient showed slight improvement. His GCS score improved to 11/15 with spontaneous eye opening and moving the left side of the body. However, his strength did not recover on the right side and feeding was continued using a Ryles tube. There was no new episode of seizure or focal neurological deficit. The patient was lost to follow-up after 6 months from the date of discharge.
Discussion
Cryptococcosis is an important infectious disease globally with meningitis being the most common clinical presentation accounting for over 1 million cases and 600 000 deaths per year.2 HIV infection is the main risk factor, accounting for 95% of cases in middle-income and low-income countries and 80% of cases in high-income countries.3 The other risk factors include transplant recipients, patients with acute leukaemias or lymphomas, on imunnosuppressive therapy and steroid use. Meningitis in immunocompetent host is usually attributed to Cryptococcus gattii while that in immunocompromised is mostly by C.neoformans.4 Diagnosis of cryptococcal meningitis can be reliably performed by serum cryptococcal latex agglutination titre which has a sensitivity of 87% in HIV-negative while CSF latex agglutination assay is 95% sensitive. India ink preparation has a sensitivity of 50% in HIV negative and >90% in HIV positive.4 Another case report which compared four different methods of detecting cryptococcal antigen in serum and CSF besides latex agglutination with comparable sensitivities and specifities.5 However, CSF culture remains the gold standard. Although cryptococcal meningitis is more commonly seen in immunocompromised host there have been cases reports of its association with steroid use being given for another illness in immunocompetent.
In another Indian case report, a 13-year-old girl developed cryptococcal meningitis after taking prednisolone (4.5 mg/kg body weight/day) for a year for autoimmune haemolytic anaemia.6 In our case the patient was on steroids for 8 weeks following a diagnosis of tubercular meningitis after which he was readmitted and found to be having cryptococcal meningitis. It was thought to be a result of steroid treatment as the patient had no other risk factors except for his recent steroid use and on initial investigation there was no evidence of Cryptococcus found in CSF examination or MRI of the brain. Also there was nothing to suggest in history, examination and laboratory investigations of an underlying haematological malignancy. Both crytococcosis and tubercular meningitis are more commonly found in immunocompromised. Their coexistence, if at all is more common in immunocompromised. Cryptococcal meningitis is rare in immunocompetent patients. Their association with tuberculosis in an immunocompetent host and by far association with steroids as seen in our case should alert the physician to possible immunosuppression due to steroids and to think of an unusual pathogen.
Learning points.
When patient continues to show partial response or develops further neurological complications despite on therapy for tuberculosis, possibility of dual infection may be considered.
Chronic high-dose steroid may precipitate an immunocompromised state and thus create susceptibility to fungal infections.
Footnotes
Contributors: AN compiled and wrote the article. She received beneficial input from MKD, AM and AS into improving this case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Klein NC, Go CHU, Cunha BA. Infections associated with steroid use. Infect Dis Clin North Am 2001;15:423–32. 10.1016/S0891-5520(05)70154-9 [DOI] [PubMed] [Google Scholar]
- 2.Park BJ, Wannemuehler KA, Marston BJ et al. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009;23:525–30. 10.1097/QAD.0b013e328322ffac [DOI] [PubMed] [Google Scholar]
- 3.Solan DJ, Pariss V. Cryptococcal meningitis: epidemiology and therapeutic options. Clin Epidemiol 2014;6:169–82. 10.2147/CLEP.S38850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanes B, Hanes M, Juliana F et al. Crptococcal meningitis in an immunocompetent patient: a case report. Am Med J 2013;4:100–4. 10.3844/amjsp.2013.100.104 [DOI] [Google Scholar]
- 5.Binnicker MJ, Jespersen DJ, Bestrom JE et al. Comparison of four assays for the detection of cryptococcal antigen. Clin Vaccine Immunol 2012;19:1988–90. 10.1128/CVI.00446-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumari PR, Shahapur PR, Rao PS. Corticosteroid induced cryptococcus meningitis. Ind J Med Microbiol 2005;23:207–8. 10.4103/0255-0857.16603 [DOI] [PubMed] [Google Scholar]