Abstract
Pityriasis versicolor is one of the most frequent epidermal mycotic infections in the world, but its atrophic variant is rarely described. The aetiology of the atrophy is still unknown, and two main hypotheses have been formulated, one suggesting a correlation with long-term use of topical steroids and the other a delayed type hypersensitivity to epicutaneous antigens derived from components of the fungus. Atrophic pityriasis versicolor is a benign disease, but needs to be distinguished from other more severe skin diseases manifesting with cutaneous atrophy. The diagnosis can be easily confirmed by direct microscopic observation of the scales soaked in 15% potassium hydroxide, which reveals the typical ‘spaghetti and meatball’ appearance, or by a skin biopsy in doubtful cases. Here, we describe a case of extensive atrophic pityriasis versicolor occurring in a woman affected by Sjögren's syndrome which completely resolved after topical antifungal treatment.
Background
Pityriasis versicolor is a widespread chronic-relapsing mycosis caused by the Malassezia species, a lipophilic yeast that, under normal conditions, is part of the physiological flora of the skin surface. Many factors may favour proliferation of the yeast and its transition into a pathogen: hormonal changes, increases in sebum secretions, hyperidrosis, congenital/acquired immunodepression and endocrine disorders.1 2 Predilection sites for pityriasis versicolor are the upper trunk, back, chest, shoulders and upper arms. In rare cases, the groins and thighs are involved. The disease typically starts with brownish-red, macular, oval and round, coalescing, flat, non-pruritic lesions of various sizes, in which discrete bran-like scaling may be evoked by tangential scraping.3 The lesions of pityriasis versicolor can be rarely accompanied by skin atrophy and in order to describe this variant, Crowson and Magro coined the term ‘atrophying pityriasis versicolor’.4 To the best of our knowledge, <20 cases have been reported since then. We report a case of atrophic pityriasis versicolor occurring in a woman affected by Sjögren's syndrome with a review of the literature.
Case presentation
A 42-year-old woman presented with hundreds of faintly erythematous scaly roundish asymptomatic patches varying in diameter from 0.5 to 1 cm, diffuse all over the back from the shoulders to the lumbar area and on both sides of the neck (figure1A, B). The patches presented a depressed appearance and a slight atrophy could be appreciated by palpation. The first patches appeared 2 months before on the neck and gradually increased in number.
Figure 1.
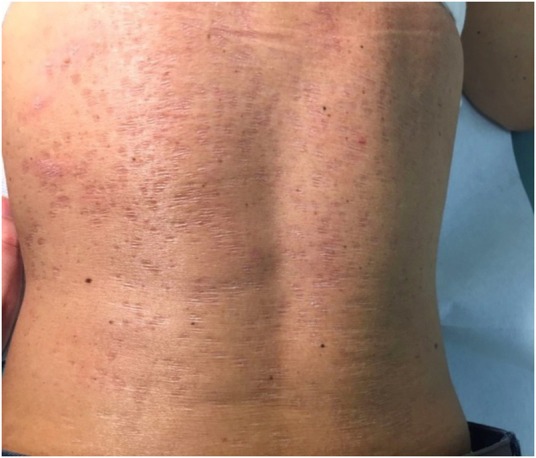
Erythematous roundish patches varying in diameter from 0.5 to 1 cm on the back of a 42-year-old woman (A). Close-up view of the patient's skin under tangential lighting shows mild scaling and atrophy (B).
The patient had been affected by Sjögren's syndrome with a severe musculoskeletal involvement (polyarticular arthritis) for 20 years requiring systemic corticosteroids since the beginning of the disease. She also was affected by Hashimoto's thyroiditis treated with levothyroxine. She denied the use of topical steroids. When the patient was referred to us, mycological examination of the lesions was performed to verify the clinical hypothesis of atrophic pityriasis versicolor.
Investigations
For direct microscopic observation, the scales were soaked in 15% potassium hydroxide (KOH) and microscopic evaluation revealed both hyphae and spores creating the ‘spaghetti and meatball’ appearance (figure 2), consequently the diagnosis of tinea versicolor was confirmed.
Figure 2.
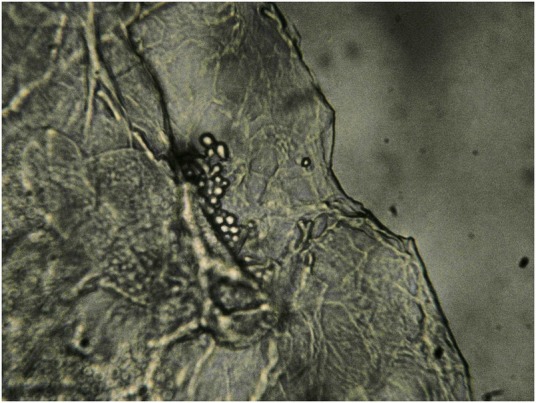
Microscopic examination of scales soaked in 10–15% potassium hydroxide (KOH). Hyphae are visible and grown into strands within clumps of keratinocytes. Thick-walled spores occur in grapelike clumps. Individual spores and short stubby hyphae float in the clear areas between clumps of keratinocytes. This combination is commonly referred to as ‘spaghetti and meatballs’.
Treatment
The patient was treated with daily application of topical ketoconazole 2% cream over a 6-week period. After this period, the skin lesions and the atrophy completely resolved (figure 3).
Figure 3.

Complete resolution of both scaly patches and atrophy after topical therapy with ketoconazole.
Outcome and follow-up
There was no recurrence of the disease after 3 months of follow-up.
Discussion
De Graciansky and Mery reported the first case of pityriasis versicolor associated with skin atrophy in 1971.5 Since then, this finding has been rarely described.4 6–9 The mechanism of cutaneous atrophy in atrophic pityriasis versicolor is not well understood. So far, two hypotheses have been proposed to explain skin atrophy. The first hypothesis suggests a pathogenetic role of long-term use of topical steroids in the patients affected.10–12 The authors suggested that atrophy induced by topical steroids, entirely confined to the pityriasis versicolor lesions, was due to the reduction in cutaneous barrier functions at sites of infection. The structural properties of the outer two-thirds of the horny layer are altered in pityriasis versicolor,13 and this may be responsible for the increased penetration of topical steroid and consequent atrophic dermal changes through the inhibition of collagen synthesis and reduction of the mitotic activity of keratinocytes. Therefore, the atrophy might have occurred only in the pityriasis versicolor lesions, although topical steroids were applied to the whole body of the affected patients.6 In our patient we cannot exclude a role of the systemic treatment with corticosteroids. Crowson and Magro conducted clinical and histological studies in 12 patients with atrophic pityriasis versicolor, but only one of these had been treated with topical steroids for a long time before diagnosis.4 The second hypothesis, suggested by these authors, is that the atrophy seen clinically and histologically in all of their patients may reflect a delayed type hypersensitivity to epicutaneous antigens derived from components of the pityriasis versicolor throughout the release by T helper lymphocytes of cytokines such as interleukin-1β and tumour necrosis factor α. These mediators could be responsible for the epidermal atrophy by provoking the apoptosis and impaired proliferation of keratinocytes and/or stimulating the histiocytes to release elastase that leads to elastolysis perturbing the collagen metabolism.
Atrophic pityriasis versicolor needs to be distinguished from other more severe skin diseases manifesting with cutaneous atrophy such as anetoderma, atrophoderma of Pasini and Pierini, mid-dermal elastolysis, confetti like macular atrophy, morphea, parapsoriasis and mycosis fungoides. Differential diagnoses especially with anetoderma, a rare elastolytic disorder characterised by circumscribed areas of flaccid skin due to the loss of elastic tissue in the superficial dermis, may be difficult because the clinical manifestations are very similar; however, anetoderma is associated with histological evidence of dermal loss and elastic tissue loss.14 Primary anetoderma (PA) is frequently observed in patients with autoimmune diseases, especially with antiphospholipid antibodies with or without antiphospholipid syndrome and in patients with systemic lupus erythematosus.15 Moreover, there are isolated reports of PA and autoimmune diseases like primary hypothyroidism, Graves’ disease, Addison's disease, Sjögren's syndrome, alopecia areata, vitiligo and multiple sclerosis.16 The evolution towards conspicuous atrophy, the irreversibility of skin lesions and the lack of therapeutic success are also typical of primary anetoderma. In our patient, the atrophic areas showed a complete regression after antimycotic therapy, so the diagnosis of anetoderma was definitively excluded. On the basis of typical clinical findings as the concurrent presence of scales and a positive KOH test; however, a differential diagnosis can be made in case of unclear presentation. Extensive biopsies and histological examinations might not be required in cases that are clinically and microscopically unequivocal.9 However, in doubtful cases, biopsy provides histological confirmation of the presence of the yeast in the horny layer and it may document reduction in number and fragmentation of elastic fibres, especially in long-standing forms.14 In this condition, following treatment of Malassezia the atrophy usually resolves,7 therefore some authors suggest the term of ‘pseudoatrophy’ to indicate its reversible character.8 12
Moon et al8 performed skin biopsies on the lesions before and after treatment and on perilesional normal skin of an affected man to investigate more accurately the mechanism of skin atrophy, and on the basis of their histopathological findings they suggested that atrophy observed in atrophic pityriasis versicolor may be more likely associated with alterations in dermis rather than epidermal changes. These dermal alterations seem to be related to defect of elastic fibres but not to changes or loss of collagen. As a matter of fact, focal fragmented or decreased elastic fibres were found only on lesional skin before treatment compared with the other two specimens.
Learning points.
Pityriasis versicolor is a widespread epidermal mycotic infection, but this atrophic variant is rarely described in the literature.
Atrophic pityriasis versicolor is a benign disease, but needs to be distinguished from other more severe skin diseases showing cutaneous atrophy.
The diagnosis is based on the typical clinical findings and the positive potassium hydroxide test, but histological examination might be required in case of unclear presentation.
Footnotes
Twitter: Follow Elena Marinello @elena_51@libero.it
Contributors: EM made substantial contribution to acquisition of clinical data and drafting the manuscript. SP made substantial contribution to interpretation of clinical data. MA made substantial contribution to acquisition of clinical data and drafting the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schwartz RA. Superficial fungal infections. Lancet 2004;364:1173–82. 10.1016/S0140-6736(04)17107-9 [DOI] [PubMed] [Google Scholar]
- 2.Belloni-Fortina A, Piaserico S, Bordignon M et al. Skin cancer and other cutaneous disorders in liver transplant recipients. Acta Derm Venereol 2012;92:411–15. 10.2340/00015555-1316 [DOI] [PubMed] [Google Scholar]
- 3.Nenoff P, Krüger C, Schaller J et al. Mycology—an update part 2: dermatomycoses: clinical picture and diagnostics. J Dtsch Dermatol Ges 2014;12:749–77. 10.1111/ddg.12420 [DOI] [PubMed] [Google Scholar]
- 4.Crowson AN, Magro CM. Atrophying tinea versicolor: a clinical and histological study of 12 patients. Int J Dermatol 2003;42:928–32. 10.1111/j.1365-4632.2003.02110.x [DOI] [PubMed] [Google Scholar]
- 5.De Graciansky P, Mery F. Atrophie sur pityriasis versicolor apres corticotherapie locale prolongee. Bull Soc Fr Dermatol Syphiligr 1971;78:295. [Google Scholar]
- 6.Yang YS, Shin MK, Haw CR. Atrophying pityriasis versicolor: is this a new variant of pityriasis versicolor? Ann Dermatol 2010;22:456–9. 10.5021/ad.2010.22.4.456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cullingham K, Hull PR. Atrophying pityriasis versicolor. CMAJ 2014;186:776 10.1503/cmaj.131846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moon SY, Lee WJ, Lee SJ et al. Pityriasis versicolor atrophicans: is it true atrophy or pseudoatrophy?. J Cutan Pathol 2016;43:187–9. 10.1111/cup.12596 [DOI] [PubMed] [Google Scholar]
- 9.Haiduk J, Treudler R, Ziemer M. Atrophying tinea versicolor with epidermal atrophy. J Dtsch Dermatol Ges 2016;14:740–3. 10.1111/ddg.12894 [DOI] [PubMed] [Google Scholar]
- 10.Tatnall FM, Rycroft RJ. Pityriasis versicolor with cutaneous atrophy induced by topical steroid application. Clin Exp Dermatol 1985;10:258–61. 10.1111/j.1365-2230.1985.tb00567.x [DOI] [PubMed] [Google Scholar]
- 11.Wagner G, Lubach D. [Pityriasis versicolor pseudoatrophicans. A case description]. Z Hautkr 1987;62:321–4. [PubMed] [Google Scholar]
- 12.Mazuecos Blanca J, García-Bravo B, Moreno Giménez JC et al. Pseudoatrophic pityriasis versicolor. Med Cutan Ibero Lat Am 1990;18:101–3. [PubMed] [Google Scholar]
- 13.Tosti A, Villardita S, Fazzini ML. The parasitic colonization of the horny layer in tinea versicolor. J Invest Dermatol 1972;59:233–7. 10.1111/1523-1747.ep12627257 [DOI] [PubMed] [Google Scholar]
- 14.Romano C, Maritati E, Ghilardi A et al. A case of pityriasis versicolor atrophicans. Mycoses 2005;48:439–41. 10.1111/j.1439-0507.2005.01160.x [DOI] [PubMed] [Google Scholar]
- 15.El Moussaoui N, Ramli I, El Amraoui M et al. Primary anetoderma revealing autoimmune disease. Ann Dermatol Venereol 2015;142:716–18. 10.1016/j.annder.2015.06.019 [DOI] [PubMed] [Google Scholar]
- 16.Al Buainain H, Allam M. Anetoderma: is it a sign of autoimmunity? Case Rep Dermatol 2009;1:100–4. 10.1159/000265699 [DOI] [PMC free article] [PubMed] [Google Scholar]


