Abstract
Background: Fractures of the proximal pole of the scaphoid can be difficult to heal because of its limited vascular supply. Furthermore, nonunion with avascular necrosis and secondary fragmentation makes surgical reconstruction a challenging procedure. Method: We describe a technique and report the outcome of a proximal hamate autograft to treat a proximal pole scaphoid nonunion with avascular necrosis. Results: At 3.5 years post reconstruction, the patient remains asymptomatic with union of his scaphoid reconstruction without any evidence of scapholunate instability. Conclusion: Proximal hamate autograft is a useful technique for addressing proximal pole scaphoid nonunions with avascular necrosis.
Keywords: proximal scaphoid pole fracture, nonunion, avascularity, ipsilateral proximal hamate autograft
Introduction
Fractures of the proximal pole of the scaphoid can be difficult to heal because of its limited vascular supply.8 Nonunion with or without avascular necrosis (AVN) is a known complication of such fractures with secondary fragmentation of the proximal pole that may in turn render the ability to surgically correct this problem very challenging.17 Techniques utilizing vascularized15,18 and nonvascularized bone grafts,3 rib autografts,14,18 and free osteochondral grafts4 have been described with varying success and associated donor site morbidities. One of the limitations of these techniques is how to reconstruct the scapholunate ligament. Given this, we report the use of the proximal pole of the hamate with its associated ligament to reconstruct a fragmented proximal pole nonunion as well as repair of the dorsal scapholunate ligament.
Case Presentation and Surgical Technique
An 18-year-old right-hand dominant male was seen with a symptomatic proximal scaphoid fracture. He had previously undergone open reduction and internal fixation elsewhere, 12 months prior. Despite using a splint and a bone stimulator, he continued to have pain and weakness in his left wrist for which he sought another opinion.
Examination revealed a well-healed surgical scar on the dorsum of the left wrist. The patient had significant tenderness to palpation over the radial aspect of the wrist. There was no tenderness over the radiolunate, mid-carpal, and distal radioulnar joints. Range of motion (ROM) was limited on the left wrist with a flexion-extension arc of 30°. Radiographs showed evidence of a proximal third scaphoid nonunion with an intramedullary screw in situ. The remnant of the proximal pole appeared small and sclerotic (Figure 1). A computed tomography (CT) scan confirmed proximal scaphoid nonunion with a fragmented proximal pole that was deemed unsalvageable (Figure 2). There were no signs of degenerative joint disease.
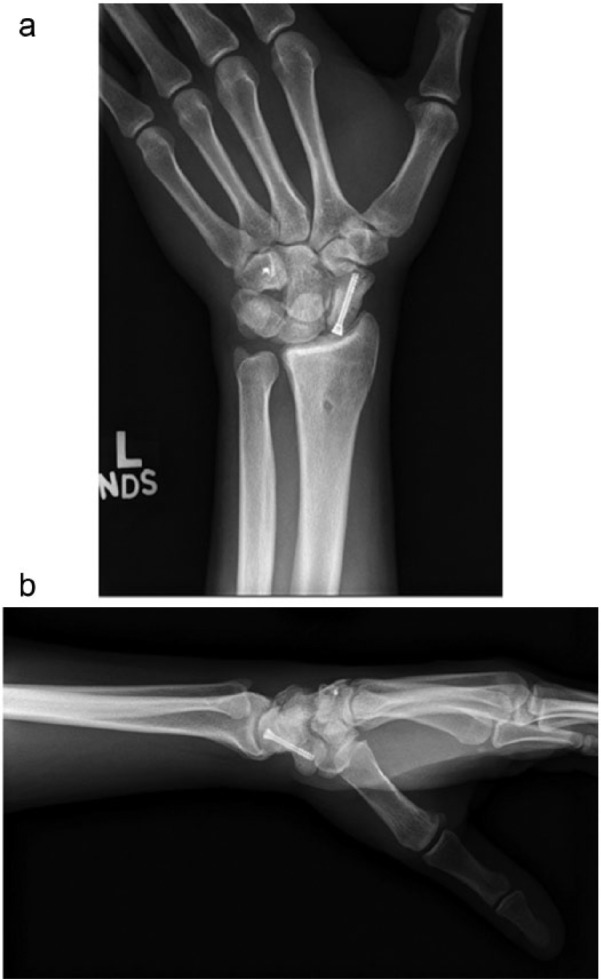
Figure 1.

A radiograph of the left wrist taken at the initial presentation showing evidence of a sclerotic un-united proximal scaphoid pole with a compression screw in situ.
Figure 2.
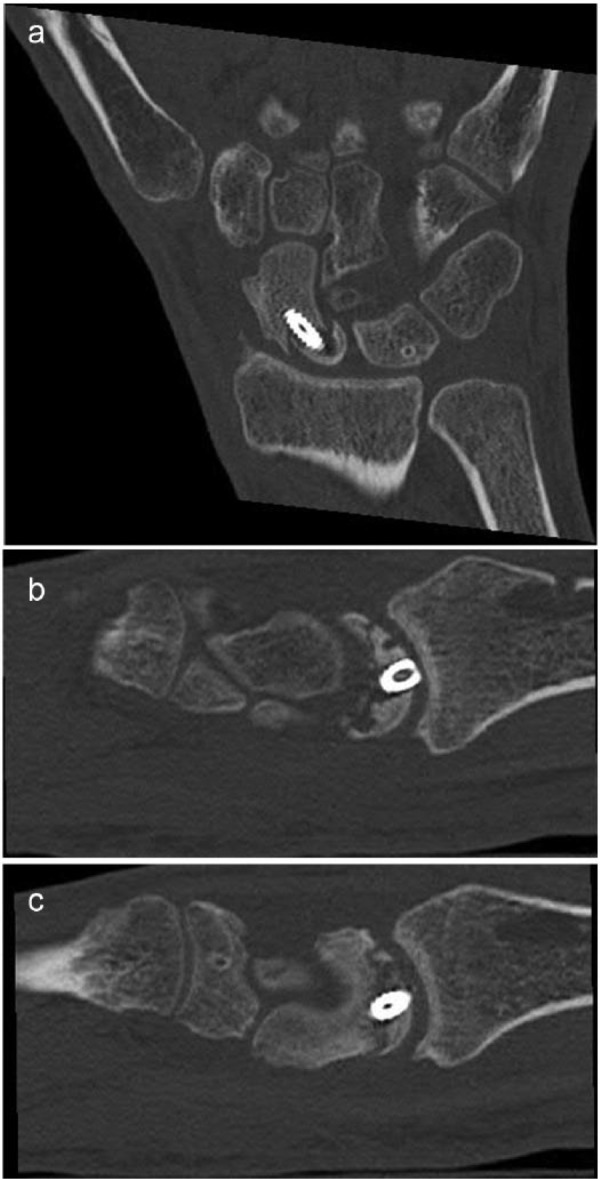
Preoperative CT scan images: (a) coronal view and (b and c) sagittal views of the left wrist showing fragmentation of the proximal pole of the scaphoid.
Note. CT, computed tomography.
Given the patient’s symptoms and young age, we decided to proceed with surgical reconstruction of the proximal scaphoid using the proximal hamate.
Surgical Technique
Under regional anesthesia and tourniquet control, the dorsal wrist was accessed using a ligament sparing capsulotomy.1 The proximal scaphoid was fragmented and necrotic. The cartilage over the scaphoid fossa and the radiolunate articulation appeared intact without any signs of arthritis. The tourniquet was deflated, the scaphoid screw removed, and the necrotic bone excised with an osteotome until punctate bleeding was noted from the remaining scaphoid. The length of the scaphoid defect measured 10 mm long, 10 mm wide, and 10 mm deep.
Attention was then directed to harvesting the proximal hamate. An osteotomy was made 10 mm distal to its proximal tip to ensure that the size of the proximal pole of the hamate mirrored the scaphoid defect (Figure 3). In doing so, care was taken to protect the volar capitohamate ligament by placing a retractor between the triquetrum and hamate and ensuring the osteotome remained within the hamate during the osteotomy and did not deviate radially toward the capitohamate articulation that could inadvertently injure the ligament. The excised proximal hamate was then turned 180° (Figure 4) so that the capitohamate articular surface became the articular surface with the lunate. The graft was trimmed and reduced to the scaphoid by a temporary Kirschner wire. At this stage, the graft was inspected to ensure it matched the scaphoid, scapholunate, and scaphocapitate joints, and the scaphoid facet of the distal radius (Figure 5). Once deemed to be a suitable match, a derotation Kirschner wire was placed followed by compression screw fixation.
Figure 3.
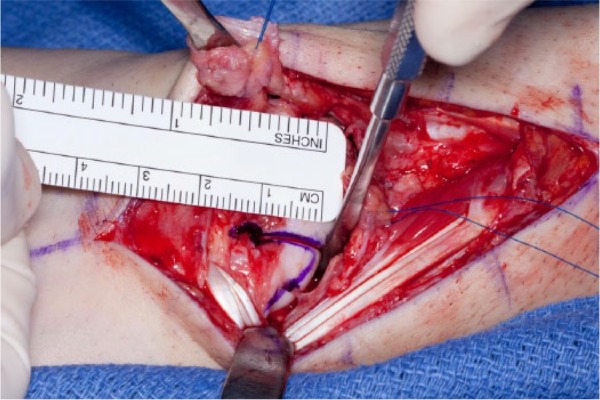
An intraoperative photograph showing the left hamate bone with osteotomy performed on the proximal 10 mm.
Figure 4.
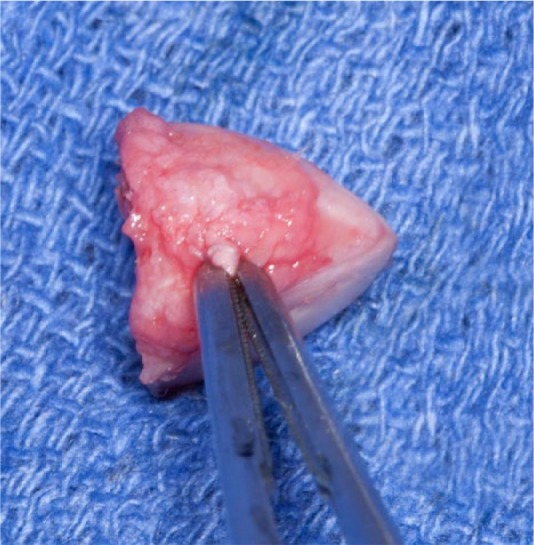
An intraoperative photograph showing the harvested proximal hamate autograft bone with the volar capitohamate ligament that was utilized for reconstructing the dorsal scapholunate ligament.
Figure 5.
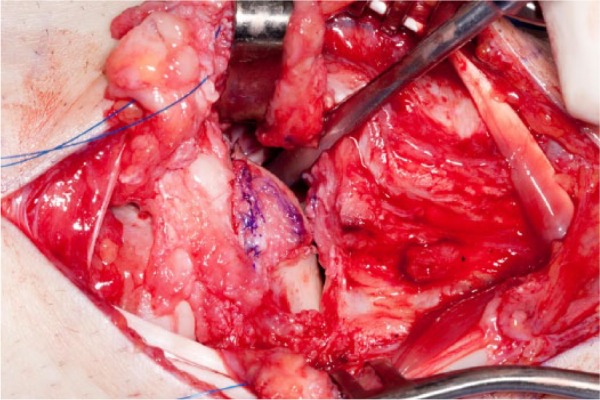
An intraoperative photograph demonstrating the hamate autograft after opposed to the scaphoid.
Attention was next directed to stabilization of the scapholunate joint. The lunate was maintained in neutral alignment using a Kirschner wire placed through the capitolunate joint. With the scapholunate joint reduced, the volar capitohamate ligament on the proximal pole of the hamate, which now lies dorsal, was repaired to the remnant of the scapholunate ligament on the lunate with a 2-0 nonabsorbable suture. Fluoroscopic imaging demonstrated satisfactory anatomical reduction of the scaphoid and scapholunate interval (Figure 6). The scapholunate repair was then augmented with a distally based strip of the dorsal intercarpal ligament. The dorsal capsule and extensor retinaculum were then closed. The patient was immobilized in a thumb spica splint for 2 weeks and then a thumb spica cast for 2 months until union was confirmed via a CT scan (Figure 7). The capitolunate pin was removed, and the patient made a satisfactory postoperative recovery. At 3.5 years postreconstruction, the patient was asymptomatic and working as a carpenter without any sequelae. On examination, his wrist ROM was 60° of flexion, 60° of extension, and full forearm rotation. His grip strength was 110 kg on the left compared with 120 kg on the right side. His Mayo wrist score was 90 points that interprets to an excellent functional outcome. He was nontender over the scaphoid and scapholunate ligament with a negative Watson shift test. Radiographs showed a well-healed scaphoid with maintenance of scapholunate alignment (Figure 8).
Figure 6.

Intraoperative fluoroscopy showing the alignment of the reconstructed scaphoid with the compression screw and a scapholunate pin in situ.
Figure 7.

A postoperative 3-dimensional CT scan image of the left wrist taken at 2 months postoperatively demonstrates evidence of scaphoid fusion.
Note. CT, computed tomography.
Figure 8.
Postoperative (a) anteroposterior and (b) lateral radiographs of the left wrist taken at 3.5 years postoperatively show evidence of scaphoid fusion.
Discussion
Three percent of all scaphoid fractures develop AVN.10 A delay in diagnosis and treatment is a major risk factor for its development.15 Other proposed risk factors include a proximal location of the fracture site, fracture diastasis greater than 1 mm, and carpal malalignment.11
Many techniques have been described for the treatment of proximal pole scaphoid nonunions with AVN including the use of nonvascularized13,15 and vascularized5 bone grafts. Common donor sites for nonvascularized corticocancellous bone grafts are from the anterior iliac crest13 or the distal radius15 with success rates ranging from 36% to 89%.13,15 Many reports emphasized the challenge associated with scaphoid nonunion with established AVN, with reported radiographic healing as low as 53%.13 Vascularized bone grafts demonstrate a union rate ranging from 50% to 100%.3,19 Utilizing 1,2 intercompartmental supraretinacular artery,16 Chang et al reported a 50% healing rate in patients with proximal pole nonunions with AVN.5 Complications of vascularized and nonvascularized grafts range from graft extrusion to failure of fixation.3,5
A fragmented proximal pole fracture in the setting of AVN can be even more difficult to treat and fewer surgical options are available. In cases of small fragments, excision of the fragments and advancement of the scapholunate ligament to the remaining scaphoid bone may be a valid option given an intact scapholunate ligament.6 However, large proximal poles require reconstruction and replacement of the necrotic bone.
Proximal scaphoid rib graft arthroplasty has been proposed as a promising alternative and demonstrated favorable outcome.14,18 Sandow reported a successful outcome in all 47 patients treated with osteochondral grafts. All patients experienced improved wrist function with a median follow-up of 15 months.14 Despite this success, the rib graft harvest procedure carries risks such as pleural tears, pneumothorax, and other associated donor site morbidity.
Recently, techniques using a vascularized osteochondral flap harvested from the medial femoral trochlea have been described.4 Burger et al reported healing in 15 of their 16 patients and complete pain resolution in 12 of the 16 patients with an average follow-up period of 14 months. In this technique, the authors attempted to address the scapholunate stability issue by preserving the distal-most portions of the scapholunate ligament while excavating the diseased segment of the scaphoid. The mid-term and long-term outcomes associated with the technique in addition to the donor site morbidity remain unknown.
The technique we describe has the advantage of graft harvest from within the carpus and avoids the risks associated with the rib autograft procedure. In addition, the morphology of the proximal pole of the hamate is similar to that of the scaphoid and requires minimal contouring to fit the defect, and both bones are fully covered by cartilage. The technique also enables the volar ligament of the ipsilateral hamate to repair the dorsal scapholunate ligament. Berger et al demonstrated that the dorsal region of the scapholunate ligament is the most structurally and functionally important area of the scapholunate ligament.2 In a subsequent study, Gay et al investigated material and biomechanical properties of the common graft alternatives utilized for the reconstruction of the dorsal scapholunate ligament. Although the volar capitohamate ligament was not included in the study, the authors reported that the dorsal capitohamate ligament has the closest properties to the native dorsal scapholunate ligament.7 Ritt et al examined the capitohamate ligaments and noted that the volar ligament was stronger than the dorsal ligament (171 N compared with 133 N, respectively).12 These evidence support the rationale behind using the volar capitohamate ligament for the repair of the dorsal scapholunate utilized in the present technique.
Resection of the proximal hamate is well established for the treatment of hamate arthrosis lunotriquetral ligament tear.9 Harley and colleagues in biomechanical and long-term clinical outcome studies demonstrated no evidence of carpal instability or adverse carpal kinematics associated with the resection of the proximal hamate.9 As such, the bone stock of the proximal hamate may represent a potential area for grafting from within the carpus. Excision of the proximal pole of the hamate can destabilize the triquetrohamate articulation resulting in a dorsal intercalated segment instability pattern. The patient in this case did not develop this, as care was taken to protect the triquetrohamate ligament as well as the carpus secondary stabilizers.
We describe an alternative form of treatment for the management of proximal pole scaphoid nonunions. These can be challenging fractures to treat, especially when they develop AVN and fragmentation. The technique offers a source of bone harvest from within the carpus and a solution to reconstruct the scapholunate ligament. Our patient experienced a favorable outcome and returned to his full spectrum of activities. Larger scale studies are warranted to further evaluate the effectiveness of the procedure.
Footnotes
Ethical Approval: As this is a case report, no IRB permission was needed.
Statement of Human and Animal Rights: Procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent: Informed consent for research purposes was obtained per institutional protocol.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(1):54-59. [DOI] [PubMed] [Google Scholar]
- 2. Berger RA, Imeada T, Berglund L, An KN. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg Am. 1999;24(5):953-962. [DOI] [PubMed] [Google Scholar]
- 3. Boyer MI, von Schroeder HP, Axelrod TS. Scaphoid nonunion with avascular necrosis of the proximal pole. Treatment with a vascularized bone graft from the dorsum of the distal radius. J Hand Surg Am. 1998;23(5):686-690. [DOI] [PubMed] [Google Scholar]
- 4. Burger HK, Windhofer C, Gaggl AJ, Higgins JP. Vascularized medial femoral trochlea osteocartilaginous flap reconstruction of proximal pole scaphoid nonunions. J Hand Surg Am. 2013;38(4):690-700. [DOI] [PubMed] [Google Scholar]
- 5. Chang MA, Bishop AT, Moran SL, Shin AY. The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg Am. 2006;31(3):387-396. [DOI] [PubMed] [Google Scholar]
- 6. Garcia-Elias M, Lluch A. Partial excision of scaphoid: is it ever indicated? Hand Clin. 2001;17(4):687-695. [PubMed] [Google Scholar]
- 7. Gay AM, Thoreson A, Berger RA. Biomechanical comparison of the hand-based transplant used in bone-tissue-bone scapho-lunate ligament reconstruction. Chir Main. 2014;33(1):23-28. [DOI] [PubMed] [Google Scholar]
- 8. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980;5(5):508-513. [DOI] [PubMed] [Google Scholar]
- 9. Harley BJ, Werner FW, Boles SD, Palmer AK. Arthroscopic resection of arthrosis of the proximal hamate: a clinical and biomechanical study. J Hand Surg Am. 2004;29(4):661-667. [DOI] [PubMed] [Google Scholar]
- 10. Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 5th ed. St. Louis, MO: Mosby; 2002. [Google Scholar]
- 11. Pao VS, Chang J. Scaphoid nonunion: diagnosis and treatment. Plast Reconstr Surg. 2003;112(6):1666-1676. [DOI] [PubMed] [Google Scholar]
- 12. Ritt MJ, Berger RA, Kauer JM. The gross and histologic anatomy of the ligaments of the capitohamate joint. J Hand Surg Am. 1996;21(6):1022-1028. [DOI] [PubMed] [Google Scholar]
- 13. Robbins RR, Ridge O, Carter PR. Iliac crest bone grafting and Herbert screw fixation of nonunions of the scaphoid with avascular proximal poles. J Hand Surg Am. 1995;20(5):818-831. [DOI] [PubMed] [Google Scholar]
- 14. Sandow MJ. Costo-osteochondral grafts in the wrist. Tech Hand Up Extrem Surg. 2001;5(3):165-172. [DOI] [PubMed] [Google Scholar]
- 15. Shah J, Jones WA. Factors affecting the outcome in 50 cases of scaphoid nonunion treated with Herbert screw fixation. J Hand Surg Am. 1998;23(5):680-685. [DOI] [PubMed] [Google Scholar]
- 16. Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg Am. 1995;20(6):902-914. [DOI] [PubMed] [Google Scholar]
- 17. Trumble TE. Avascular necrosis after scaphoid fracture: a correlation of magnetic resonance imaging and histology. J Hand Surg Am. 1990;15(4):557-564. [DOI] [PubMed] [Google Scholar]
- 18. Yao J, Read B, Hentz VR. The fragmented proximal pole scaphoid nonunion treated with rib autograft: case series and review of the literature. J Hand Surg Am. 2013;38(11):2188-2192. [DOI] [PubMed] [Google Scholar]
- 19. Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am. 1991;16(3):474-478. [DOI] [PubMed] [Google Scholar]


