Abstract
Background: Closed reduction with percutaneous Kirschner wires (K-wires) is the most minimally invasive surgical option for stabilizing phalanx fractures. This study examines the effect of K-wire placement on proximal interphalangeal (PIP) joint motion. Methods: PIP joint flexion was measured in the digits of 4 fresh-frozen cadaver hands after placing a suture loop through the flexor tendons and placing tension on the flexors via a mechanical scale. The load necessary to flex the PIP joint to 90° or to maximum flexion was recorded. The load was removed and K-wires were inserted in 3 locations about the metacarpophalangeal joint (MPJ): through the extensor tendon and across the MPJ, adjacent to the extensor tendon insertion site and across the MPJ, and through the sagittal band and into the base of the proximal phalanx (P1). The load on the tendons was reapplied, and angles of PIP joint flexion were recorded for each of the 3 conditions. Results: The mean angle of PIP joint flexion prior to K-wire insertion was 87°, and the mean load applied was 241 g. The angles of flexion were 53° when the K-wire was placed through the extensor tendon, 70° when the K-wire was placed adjacent to the tendon, and 75° when the K-wire was placed into the base of P1 by going through the sagittal band, midway between the volar plate and the extensor tendon. Conclusions: K-wires placed remote from the extensor tendon create less of an immediate tether to PIP joint flexion than those placed through or adjacent to the extensor tendon.
Keywords: proximal phalanx fracture, proximal interphalangeal joint motion, Kirschner wires fixation, extensor tendon, joint stiffness
Introduction
The surgical management of extra-articular fractures at the base of the proximal phalanx (P1) includes percutaneous pinning with Kirschner wires (K-wires), screw fixation, and plate fixation.4,7-13 Closed reduction with percutaneous K-wires of phalanx fractures is a minimally invasive technique that is quick, avoids soft tissue stripping about the fracture, and allows early mobilization.4,7,9,13 Early proximal interphalangeal (PIP) joint motion following fracture fixation minimizes tendon adhesions and joint contractures, improving ultimate motion.1,2,6
In this study, we examine the effect of K-wire placement on PIP joint motion. We hypothesize that K-wires placed remote from the extensor tendon will create less of a tether to PIP joint motion than those placed through or adjacent to the extensor tendon.
Materials and Methods
We used 4 fresh-frozen cadaver hand specimens, 2 male and 2 female. Each hand was dissected at the proximal amputated end in the mid forearm to isolate the individual flexor tendons corresponding with each finger. The proximal end of the flexor digitorum profundus tendon was prepared with a suture loop for a spring-loaded 0.9 kg hanging scale, graduated in 14.2-g increments (Accu-weigh Model T-2; McMaster Carr, Aurora, OH). The hand was placed onto a custom-designed testing mount. A hook attached to the scale was attached to the tendons via the suture loop and pulled until the PIP joint flexed to 90° (Figure 1). The load necessary to effect 90° of flexion or maximum flexion was recorded. Each trial was performed twice. On one hand, only 3 of 4 digits were available for testing; therefore, results were analyzed only for digits II to IV on all 4 hands.
Figure 1.

The testing construct with a cadaveric hand in the custom mount.
Note. An intramedullary Kirschner wire has been placed in the P1. Weight is applied to the flexor tendons using the spring-loaded hanging scale attached via a suture loop. The degree of flexion at the PIP joint is measured with a goniometer. PIP, proximal interphalangeal.
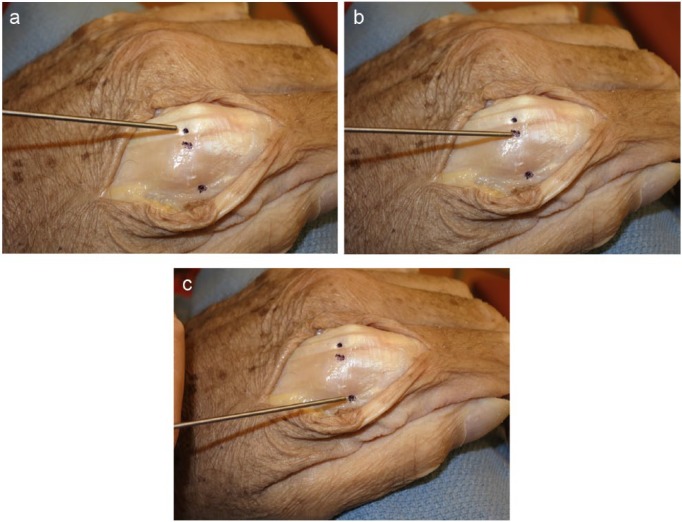
Incisions were then made over the metacarpophalangeal joints (MPJs) of the second through fourth digits, exposing the extensor tendon. The position of the MPJs in all the cases was controlled to be the same at 90° of flexion. Three sites were used for the insertion of a 0.035 inch K-wire into the medullary canal of the P1 (Figure 2).The first K-wire insertion was placed at a dorsal midline site, through the metacarpal head into the base of the P1, piercing the extensor tendon. The second insertion site was through the metacarpal head adjacent to the extensor tendon. The third K-wire was placed into the base of the P1 at the midaxial line, through the sagittal band, but remote from the fibers responsible for extending the PIP joint.
Figure 2.
Three different insertion points of the K-wires. (a) The first K-wire insertion was placed at a dorsal midline site, through the metacarpal head into the base of the P1, piercing the extensor tendon. (b) The second insertion site was through the metacarpal head adjacent to the extensor tendon. (c) The third K-wire was placed into the base of the P1 at the midaxial line, through the sagittal band, but remote from the fibers responsible for extending the PIP joint.
Note. PIP, proximal interphalangeal.
In the cadaver specimens, the absence of swelling and the minimal subcutaneous fat made it easy to reproducibly place the K-wires in all the digits without fluoroscopy control. K-wire placement was designed to simply enter the base of the P1. This was performed by controlling the amount of K-wire that was inserted into the bones. It insured that it would be impossible for the K-wire to encroach on the PIP joint. The hand was placed back on the mount, and the scale was hung from the suture loop affixed to the free end of the flexor tendon. The previously determined weight required to produce 90° of flexion at the PIP joint in the noninstrumented digit was applied, and the angle of flexion was measured using a goniometer (Figure 1). The second to fourth digits on each of the 4 hands were tested in this manner in the first trial, followed by removal of the K-wire. Each digit was then tested again in the same manner for a total of 2 trials per each of the 3 K-wire locations within each digit. The degrees of flexion following K-wires insertion were recorded.
Results
Before K-wire placement, the average angle of PIP joint flexion in response to a load applied to the flexor tendons was 87° (SD = 7°). The mean load applied to the flexor tendons was 241 g, with a range of 141.7 to 368.5 g (SD = 90.7). Hand 4 demonstrated the greatest degree of preinstrumented stiffness, with all 4 digits flexing less than 90°. The flexor tendons of hand 4 were pulled to maximal flexion, ranging from 75° to 88° (Table 1). Table 2 summarizes the mean angles of PIP joint flexion for the 3 K-wire fixation conditions.
Table 1.
The Load Applied to the Finger Flexor Tendons to Achieve Maximum PIP Joint Flexion; the Maximum Degree of PIP Joint Flexion With Indicated Load Applied in Each Finger According to the K-wire Placement.
| Hand | Digit | Load applied (g) | Midline tendon (degrees of PIPJ flexion) | Lateral to tendon (degrees of PIPJ flexion) | Midaxial phalanx (degrees of PIPJ flexion) |
|---|---|---|---|---|---|
| Hand 1 | II | 368.5 | 48 | 63 | 90 |
| III | 340.2 | 53 | 90 | 90 | |
| IV | 198.4 | 50 | 55 | 98 | |
| Hand 2 | II | 255.1 | 48 | 65 | 27 |
| III | 311.8 | 80 | 88 | 50 | |
| IV | 226.8 | 95 | 100 | 53 | |
| Hand 3 | II | 340.2 | 50 | 59 | 82 |
| III | 170.1 | 26 | 48 | 75 | |
| IV | 198.4 | 34 | 68 | 82 | |
| Hand 4 | II | 226.8 | 53 | 62 | 72 |
| III | 198.4 | 53 | 67 | 82 | |
| IV | 226.8 | 59 | 79 | 84 |
Note. PIP, proximal interphalangeal; PIPJ, proximal interphalangeal joint.
Table 2.
Mean, Standard Deviation, and Loss of Flexion for Each K-wire Fixation Site in Degrees.
| Mean | SD | Loss of flexion | |
|---|---|---|---|
| Fixation site through the extensor tendon | 54 | 22 | 34 |
| Fixation site adjacent to the extensor tendon | 70 | 18 | 17 |
| Fixation site through the sagittal band at the midaxial line | 74 | 20 | 12 |
The data were analyzed by 2-factor analysis of variance for the condition and digit tested. A significant difference was found between the 3 conditions of K-wire placement (P = .0002), whereas the finger tested resulted in no significant difference in findings (P = .37). A repeated measures analysis found no significant interaction between the digit tested and the condition (P = .46).
A post hoc analysis of the condition type with Tukey’s honest significant difference test showed a significant difference (P < .05) between all conditions: P = .0033 for the difference in degree of flexion between the condition of inserting the pin through the tendon and inserting adjacent to the tendon, P = .00036 for the difference between inserting the pin through the midline tendon and inserting along the midaxial line, and P = .013 for the difference between inserting the pin adjacent to tendon and inserting along the midaxial line through the sagittal band.
Discussion
The treatment options for fractures of the phalanges include a variety of methods that depend on a number of factors. These factors include the type of fracture, patient demographics, and surgeon preference. Many fractures of the phalanges can be treated nonoperatively, but those that involve instability, shortening, rotational deformity, or marked angulation often benefit from operative management.
Liew et al9 found that the use of multiple intramedullary K-wires in metacarpal and phalangeal fractures provided adequate stability with good union, grip strength, and range of motion (ROM). A study by Elmaraghy et al4 on unstable P1 fractures treated with intramedullary K-wires reported PIP joint flexion contractures as the most common complication. The PIP joint flexion contractures occurred in 8 of 25 patients (32%) and averaged 18.1° of flexion.
Those fractures best suited for K-wire fixation include transverse and short oblique fractures of the P1 at the base or the shaft. Many studies, including those by Liew et al,9 Elmaraghy et al,4 and Hornbach and Cohen,7 have demonstrated the adequacy of K-wires in stabilizing proximal phalangeal fractures with the added benefits of allowing an early return to motion. Belsky et al3 reported the results on closed K-wires of P1 fractures in 100 consecutive patients. In that study, 61% had excellent results (defined as pain-free union, no skin problems, no angular or rotational deformity, PIP joint motion greater than 100°, and total active motion [TAM] greater than 215°), 29% had good results (pain-free union, apparent deformity that did not impair function, PIP motion greater than 80°, and TAM greater than 180°), and 10% had poor results.
Faruqui et al5 compared transarticular (across the MPJ) and extra-articular cross-pinning fixation for proximal third of P1 fractures. They found neither fixation method to be superior in terms of the measured parameters. The mean TAM for the transarticular group and cross-pinning group was 201° and 198°, respectively. PIP joint motion was notably affected; nearly half of the patients in each group had flexion loss greater than 20° (average, 27°) at the PIP joint. Nearly one-third of patients in both groups had fixed flexion contracture greater than 15° at the PIP joint.
Many authors have discussed the placement of K-wire insertion in the lateral aspect of the MPJ to avoid the extensor tendon, including Belsky et al, Clifford et al, and Elmaraghy et al, but none have studied the difference in outcome from varying the site of K-wire insertion in relation to the extensor tendon.
This study attempted to quantify the limitation in PIP joint flexion resulting from insertion of the intramedullary K-wire in 3 different locations in relation to the extensor tendon over the base of the P1. Insertion of the K-wire through the tendon resulted in a loss of 34° of flexion. K-wire insertion laterally adjacent to the extensor tendon resulted in a loss of 17° flexion. Finally, K-wire insertion at the midaxial line created, on average, only 12° of restriction to PIP joint flexion.
Stiffness is the most common complication resulting from internal fixation of phalangeal fractures. Although other factors such as rotational deformity, angular deformity, or flexion contractures may contribute to loss of active ROM (AROM), 1 major factor in the recovery of AROM is the degree of soft tissue tethering. Our results demonstrate that placement of the K-wire to avoid insertion through the extensor tendon will minimize the loss of AROM as represented by the degree of flexion achieved following intramedullary K-wire insertion.
As with all cadaveric studies, our results do not include in vivo recovery effects, such as scar tissue formation, soft tissue tethering, and callus formation that may affect the relative loss of flexion and overall motion about the PIP joint.
However, the study attempted to isolate the role of the site of K-wire insertion on the limitation of function without the effects of other factors and was able to do so in this study on cadaveric hands. It is our sense that in vivo pain, postoperative soft tissue swelling would magnify the effect of pins tethering the extensor that we saw in this experiment. Furthermore, the midaxial approach allows less invasion of the tendons executing motion of the PIP joint and therefore should be associated with less scar tissue formation postoperatively compared with excursion through the extensor tendon.
In hand 4, the degree of flexion prior to instrumentation was limited to an average of 78.5°, with a range of 75° to 88°. This preinstrumented limitation in motion likely represents natural variation in stiffness present in the PIP joint. Nonetheless, the overall pattern in the loss of motion resulting from intramedullary K-wire fixation was consistent with the study findings supporting the midaxial approach as the least functionally impairing, followed next by the K-wire insertion site adjacent to the tendon and finally the midline tendon excursion as the most limiting of PIP joint flexion.
Our study utilized 2 trials per K-wire insertion location. Although there was variability in postinstrumented degrees of flexion between some trials (the overall standard deviations are midline tendon, SD = 22; laterally adjacent to tendon, SD = 18; midaxial phalanx, SD = 20), the analyses of the data support a strong correlation between K-wire location and loss of flexion with a P value < .013 between all 3 conditions.
When retesting the same specimen with a sequential intervention, it is ideal to randomize the order in which the intervention is applied for each specimen. This is the weakness of our method.
Further investigation may involve studying the postoperative AROM in patients with P1 fractures treated with intramedullary K-wire fixation with K-wire insertion in the midline tendon compared with insertion through the midaxial aspect of the base of the P1 with limited dissection to ensure avoidance of excursion through the extensor tendon. This study would be able to take into account any differences in the effects of scar tissue formation, postoperative physical therapy, as well as other factors impacting on the recovery of function that were not considered in this study.
Acknowledgments
The authors would like to thank Joelle Tighe for assisting with the article and to Dr. John Fowler for assisting with the statistical analysis.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was appropriately secured, either via body donation registration, autopsy authorization, or consent provided by next of kin or legal representative.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Mark E. Baratz has received consultant fees and royalties from Integra LifeSciences and consultant fees from Elizur.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Qattan MM. Phalangeal neck fractures of the proximal phalanx of the fingers in adults. Injury. 2010;41(10):1084-1089. [DOI] [PubMed] [Google Scholar]
- 2. Al-Qattan MM, Al-Zaharani K. Open reduction and cerclage wire fixation for long oblique/spiral fractures of the proximal phalanx of the fingers. J Hand Surg Eur. 2008;33(2):170-173. [DOI] [PubMed] [Google Scholar]
- 3. Belsky MR, Eaton RG, Lane LB. Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am. 1984;9:725-729. [DOI] [PubMed] [Google Scholar]
- 4. Elmaraghy MW, Elmaraghy AW, Richards RS, Chinchalkar SJ, Turner R, Roth JH. Transmetacarpal intramedullary K-wire fixation of proximal phalangeal fractures. Ann Plast Surg. 1998;41:125-130. [DOI] [PubMed] [Google Scholar]
- 5. Faruqui S, Stern PJ, Kiefhaber TR. Percutaneous pinning of fractures in the proximal third of the proximal phalanx: complications and outcomes. J Hand Surg Am. 2012;37:1342-1348. [DOI] [PubMed] [Google Scholar]
- 6. Henry M. Soft tissue sleeve approach to open reduction and internal fixation of proximal phalangeal fractures. Tech Hand Up Extrem Surg. 2008;12(3):161-165. [DOI] [PubMed] [Google Scholar]
- 7. Hornbach EE, Cohen MS. Closed reduction and percutaneous pinning of fractures of the proximal phalanx. J Hand Surg Br. 2001;26(1):45-49. [DOI] [PubMed] [Google Scholar]
- 8. Kurzen P, Fusetti C, Bonaccio M, Nagy N. Complications after plate fixation of phalangeal fractures. J Trauma. 2006;60:841-843. [DOI] [PubMed] [Google Scholar]
- 9. Liew JH, Kuen CB, Ooi LC. Metacarpal and proximal phalangeal fractures—fixation with multiple intramedullary Kirschner wires. Hand Surg. 2000;5(2):125-130. [DOI] [PubMed] [Google Scholar]
- 10. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23:827-832. [DOI] [PubMed] [Google Scholar]
- 11. Pun WK, Chow SP, So YC, et al. Unstable phalangeal fractures: Treatment by A.O. Screw and plate fixation. J Hand Surg Am. 1991;16(1):113-117. [DOI] [PubMed] [Google Scholar]
- 12. Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res. 1987;214:59-65. [PubMed] [Google Scholar]
- 13. Vom Saal FH. Intramedullary fixation in fractures of the hand and fingers. J Bone Joint Surg Am. 1953;35:5-16. [PubMed] [Google Scholar]