Abstract
Objective
The best treatment for moderately displaced radial head fractures (Mason type II) still remains controversial. In cases of isolated fractures, there is no evidence that a fragment displacement of ≥ 2 mm gives poor results in conservatively treated fractures.
Patients and methods
We retrospectively reviewed 52 patients (31M, 21F) affected by an isolated Mason type II fracture, treated with a long arm cast for two weeks between 2008 and 2013. All patients had practiced sports before being injured. They were all either bicyclists, or baseball, boxers, basketball, rugby, tennis or football players. The mean follow-up was 36 months. Elbow and forearm range of motion were measured. The Mayo Elbow Performance Score, the Broberg and Morrey rating system and the Disabilities of the Arm, Shoulder and Hand Score (DASH score) were analyzed. Follow-up radiographs were examined for evidence of consolidation, late displacement, early arthritis and non-unions.
Results
Flexion was slightly impaired in the injured limb when compared to the uninjured limb (137°± 6° versus 139°±5°) as were extension (–3°±6° versus 1°±4°, p < 0.05), supination (86°±6° versus 88°±3°), pronation (87°±4° versus 88°±6°) and valgus deviation (10°±4° versus 8°±3°, p < 0.05). 40 patients had no elbow complaints; 9 patients experienced occasional pain, 2 a mild instability of the elbow, and 4 a mild loss of grip strength. The DASH score was excellent in 48 patients (92.31%). In only 6 cases (11.53%) degenerative changes were greater in formerly injured elbows than in uninjured elbows. All patients returned to their previous sports activities.
Conclusions
Isolated Mason type II fractures can have a good or excellent mid-term functional outcome even when treated conservatively.
Keywords: Elbow, Fractures, Athletes, Mason, Nonsurgical treatment
Introduction
Radial head fractures are common, accounting for approximately one-third of all elbow fractures, with an estimated incidence of 2.5 to 2.9 per 10.000 people per year (1–3). They generally occur after a fall on the outstretched arm. They may be isolated or associated with more complex injuries such as fractures of the olecranon or coronoid process, elbow dislocation, ligament rupture, vascular injuries or nerve injuries (4, 5).
Several classifications (6–10) have been introduced to describe radial head fractures, nearly all derived from the classification proposed by Mason in 1954 (6). A Mason type I fracture is a fissure or marginal sector fracture without displacement. Type II fractures are articular fractures involving a part of the head with displacement. Comminuted articular fractures involving the whole head of the radius are Mason type III fractures. Broberg and Morrey (8) modified Mason’s classification, quantifying displacement of 2 mm or greater as articular step-off or gap, and indicating that fracture fragments representing less than 30% of the articular surface should not be considered type II.
It is generally agreed that type I fractures can be successfully treated non operatively with early mobilization (11–15). For Mason type III fractures potential treatment modalities include open reduction and internal fixation, radial head excision, or radial head replacement (16–19). The best treatment of type II fractures having no association with other fractures or ligament injuries (known as isolated fractures) is still debated. Historically, the treatment of choice for Mason Type II fractures was radial head excision after failure of conservative treatment (20, 21). In recent years, the improvement of surgical techniques (new instrumentation and implants) has made open reduction and internal fixation (ORIF) increasingly popular (22, 23). However mid and long-term follow-up have demonstrated that nonsurgical treatment can provide a good or excellent functional outcome in the vast majority of cases (24, 25).
Aim
The aim of this retrospective study was to evaluate the clinical and radiographic mid-term outcomes of a cohort of athletes with an isolated Mason type II radial head fracture conservatively treated, and to evaluate their return to sports activities.
Patients and methods
A retrospective chart review was performed on athletes who were diagnosed a radial head fracture during the period between 2006 and 2012.
The following inclusion criteria were established: 1) Mason type II fractures (2–5 mm of displacement), as shown on anteroposterior and lateral radiographs of the elbow taken at the time of injury and before treatment; 2) isolated fractures; 3) nonsurgical treatment; 4) all patients were involved in sports activities at different levels. Exclusion criteria were: Mason type II fractures associated with other elbow fractures (coronoid apophysis, olecranon, lateral and medial epicondyle), elbow dislocation, ligament injuries, vascular injuries or nerve injuries.
Out of 72 patients that met the inclusion criteria, 52 patients (31 males, 21 females) were enrolled in the study. Twenty patients were not enrolled in the study because of inability to be contacted or refusal to be included.
Demographic data were recorded. The mean age at the time of fracture was 28.1 years ± 7.5 (range 13 to 48). The dominant limb was affected in 33 patients, whereas the non dominant limb was affected in 19 patients. There were 4 bicyclists (7.69%), 3 baseball players (5.77%), 7 boxers (13.46%), 6 basket players (11.54%), 3 rugby players (5.77%), 23 tennis players (44.23%), 6 football players (11.54%).
The fracture was caused by a low energy trauma (defined as a fall or a direct impact) in 37 patients whereas 15 patients had a high energy trauma (defined as a motor-vehicle accident or a fall from > 2 m).
A long arm cast with the elbow 90° flexed and the forearm in neutral rotation was applied to all patients for two weeks. Immobilization was followed by rehabilitation including both passive and active movements of the elbow, of the forearm and of the wrist in all patients.
Patients were clinically and radiographically followed-up at a mean time of 36 months from injury (range 24 to 60 months).
Clinical evaluation was carried out by two different authors and the mean of each parameter was recorded in order to minimize intraobserver bias. Flexion and extension of the elbow, pronation and supination of the forearm and valgus deviation were measured with a standard full-circle goniometer. Collateral ligament stability was evaluated by the application of valgus and varus stresses. The uninjured contralateral limb was used as control. Data regarding the injured and uninjured arm of the same individual were assessed for statistical significance by use of the Student t-test with a level of significance set at p <0.05.
Clinical results were also evaluated using three different rating systems. Elbow pain at rest and on loading, range of motion, strength, stability and functional assessment were examined using the Mayo Elbow Performance Score and the Broberg and Morrey rating system. Subjective satisfaction and activities of daily living were evaluated with the Disabilities of the Arm, Shoulder and Hand Score (DASH score) with 0 reflecting no disability and 100 reflecting major disability. Grip strength was also evaluated.
Radiographic evaluation included antero-posterior and latero-lateral projections. X-Ray images were classified according to the Mason system modified by Broberg and Morrey. Measurement of bone displacement and percentage of radial head surface involved were recorded. Evidence of consolidation, late displacement, early arthritis and nonunions were recorded.
We also evaluated the time required to return to the pre-traumatic sports activity.
Results
Range of motion was slightly impaired in the injured elbows as when compared to the uninjured elbows (Table 1). The mean arc of motion in elbow flexion was 137°±6° on the injured side and 139°±5° on the uninjured side (p 0.11). The mean arc of motion in elbow extension was –3°±6° on the injured side and 1°±4° on the uninjured side (p 0.001). The mean arc of motion in forearm supination was 86°±6° on the injured side and 88°±3° on the uninjured side (p 0.06). The mean arc of motion in forearm pronation was 87°±4° on the injured side and 88°±6° on the uninjured side (p 0.38). Elbow valgus deviation was 10°±4° on the injured side and 8±3° on the uninjured side (p 0.01).
Table 1.
OBJECTIVE MEASUREMENTS FOR 52 PATIENTS WITH A MASON TYPE II FRACTURE TREATED NON-SURGICALLY.
| Injured elbows | Uninjured elbows | P | |
|---|---|---|---|
| Elbow flexion | 137°±6° | 139°±5° | 0.11 |
| Elbow extension | −3°±6° | 1°±4° | 0.001 |
| Forearm supination | 86°±6° | 88°±3° | 0.06 |
| Forearm pronation | 87°±4° | 88°±6° | 0.38 |
| Elbow valgus deviation | 10°±4° | 8°±3° | 0.01 |
| Grip strength (kp/cm2) | 0.7±0.4 | 0.8±0.3 | 0.21 |
Forty patients (72.92%) had no elbow complaints, while nine patients (17.30%) experienced occasional pain with loading or at rest. The mean visual analogic scale for these patients was 2.2 (range 1 to 4). In four of these cases, the dominant limb was involved. All these patients were involved in high functional demand sports activities.
Two patients perceived a mild instability of the elbow, without disabling consequences. Loss of grip strength of less than 20% in the injured limb was observed in 4 patients. The mean grip strength was 0.7±0.4 on the injured side and 0.8±0.3 (p 0.21).
According to this evidence, the Mayo Elbow Performance Score was excellent in 42 patients (80.77%), good in 8 patients (15.38%) and fair in 2 patients (3.85%) (Table 2).
Table 2.
MAYO ELBOW PERFORMANCE SCORE.
| Results | N° of patients | % of patients | Mean score (range) |
|---|---|---|---|
| Excellent | 42 | 80.77 | 98.5 (90–100) |
| Good | 8 | 15.38 | 80.5 (75–85) |
| Fair | 2 | 3.85 | 67.5 (65–70) |
| Poor | 0 | 0 | - |
The Broberg and Morrey rating system was excellent in 40 patients (76.92%), good in 9 patients (17.31%) and fair in 3 patients (5.77%) (Table 3).
Table 3.
BROBERG AND MORREY RATING SYSTEM.
| Results | N° of patients | % of patients | Mean score (range) |
|---|---|---|---|
| Excellent | 40 | 76.92 | 98 (95–100) |
| Good | 9 | 17.31 | 86 (83–91) |
| Fair | 3 | 5.77 | 71.5 (64–77) |
| Poor | 0 | 0 | - |
Patients started resuming their daily activities immediately after the two weeks of immobilization. The Disabilities of the Arm, Shoulder and Hand Score (DASH) was excellent in 48 patients (92.31%) and good in 4 patients (7.69%) (Table 4).
Table 4.
DISABILITIES OF THE ARM, SHOULDER AND HAND SCORE.
| Results | N° of patients | % of patients | Mean score (range) |
|---|---|---|---|
| Excellent | 48 | 92.31 | 10.6 (0–22) |
| Good | 4 | 7.69 | 33.4 (27–46) |
| Fair | 0 | 0 | - |
| Poor | 0 | 0 | - |
Radiographic evaluation did not reveal any late displacement. All fractures healed at an average time of 3 weeks (Figures 1, 2) and no cases of delayed consolidation or nonunion were observed. In only 6 cases (11.53%) degenerative changes (sclerosis of subchondral bone with osteophytes and a joint-space reduction of > 1mm) were greater in formerly injured elbows than in uninjured elbows.
Figure 1.
A) Anteroposterior X-ray of a 42 years old woman who experienced a direct trauma on her left elbow, reporting an isolated Mason type II radial head fracture. B) Lateral X-ray confirms Mason type II fracture after injury. C) Anteroposterior X-ray showing fracture healing 1 year after injury. The patient has a full range of motion. Both the subjective (DASH) and objective (Morrey and Broberg score) scores are excellent.
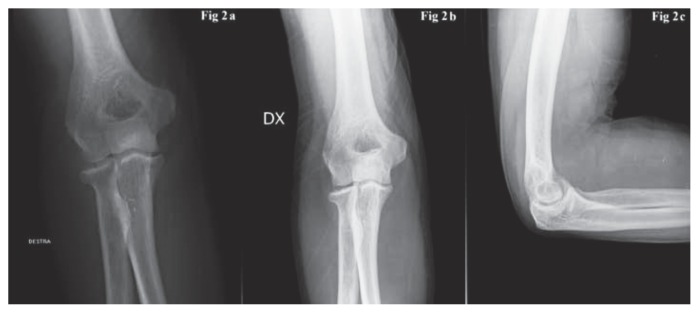
Figure 2.
A) Anteroposterior X-ray of a 48 years old woman who fell while walking, suffering an isolated Mason type II radial head fracture. B) Lateral X-ray confirms the radial head fracture after injury. C) Anteroposterior X-ray showing fracture healing 2 years after injury. The patient has a full range of motion and has returned to her daily activities.
No patient needed a delayed treatment due to an un-satisfactory primary outcome. No correlation was found between severity of displacement and clinical outcome.
All patients returned to their previous sports activities. The interval of time between cast removal and return to pre-traumatic sports activity level took place at an average of 48.4 days ±8.7: in particular, after 35 days in 8 patients (15.38%; 6 football players and 2 bicyclists); after 40 days in 8 patients (15.38%; 3 baseball players, 3 rugby players and 2 basket players); after 45 days in 7 patients (13.48%; 3 tennis players, 2 basket players and 2 bicyclists); after 50 days in 9 patients (17.31%; 7 tennis players, 2 basket players); after 55 days in 12 patients (23.07%; 10 tennis players and 2 boxers); after 60 days in 8 patients (15.38%; 3 tennis players and 5 boxers) (Table 5).
Table 5.
TIME TO RETURN TO SPORT.
| Time to return to same level of sport activities (in days) | % of patients | Kind of sport |
|---|---|---|
| 35 | 15.38 | 6 football players and 2 bicyclists |
| 40 | 15.38 | 3 baseball players, 3 rugby players and 2 basket players |
| 45 | 13.48 | 3 tennis players, 2 basket players and 2 bicyclist |
| 50 | 17.31 | 7 tennis players, 2 basket players |
| 55 | 23.07 | 10 tennis players and 2 boxer |
| 60 | 15.38 | 3 tennis players and 5 boxers |
Discussion and conclusion
In the 1970s, the treatment of choice for Mason type II fractures was radial head excision if conservative treatment was not successful or possible (26). In 1979 (27) and then in 1988 (28) Morrey et al. demonstrated that the radial head contributes to the valgus, varus and posterolateral rotatory stability of the elbow and acts as an axial stabilizer of the forearm; because of these biomechanical studies and along with significant improvement in surgical techniques and instrumentation, open reduction and internal fixation has become the preferred treatment for Mason type II fractures. At present, a fracture fragment displacement of ≥ 2 mm is usually used as a criterion for operative treatment (29); as a matter of fact, different parameters should be taken into account when planning the best treatment to perform (30, 31): type of fracture, displacement, fragment stability, magnitude of articular involvement, and presence of associated complex injuries. In the case of a stable and isolated Mason type II fracture, mid- and long-term follow up studies have demonstrated that nonsurgical treatment can provide good or excellent functional outcome in the vast majority of cases (32, 33, 34, 35).
Bakalim et al. (32), in a study on 59 patients with Mason type II fractures, reported good outcome for 80% of patients at a mean of 9 years after the injury.
More recently, Akesson et al. (33), in a study on 49 patients managed nonsurgically, reported a favorable outcome with 40 patients (82%) having no elbow complaints and 9 patients experiencing minor impaired function.
A prospective study performed by Duckworth et al. (34) in 2011 favors nonsurgical management of Mason type II radial head fractures, with excellent/good results obtained in 96% of cases.
A systematic review of the literature performed by Furey et al. (35) in 2013 did not show a significant difference between conservatively treated radial head fractures with greater than 2 mm of displacement or those with less than 2 mm of displacement in terms of patient-reported or clinical outcomes.
The results of our descriptive study support the effectiveness of nonsurgical treatment in the therapeutic management of athletes in isolated Mason type II radial head fractures. The slightly restricted range of motion in the injured elbow compared to the uninjured elbow appeared to be of mild clinical relevance. No statistically significant differences between the injured and uninjured arm was found in terms of elbow flexion, forearm supination and pronation, and grip strength. Only elbow extension and valgus deviation were statistically significant, even though no patient reported complaints in regard to this parameter. Almost 80% of patients reported an excellent outcome at the Mayo Elbow Performance Scoring scale and at the Broberg and Morrey rating system scale, whereas more than 90% of patients had an excellent result according to the Dash Score. Interestingly, the higher value rate of excellent results detected with the subjective score (DASH) in comparison to the objective scale (Morrey and Broberg) might suggest that a slight residual functional restriction could be not perceived by patients as a disability.
However, percentages of favorable functional outcomes reported in literature after open reduction and internal fixation are high as well (36–39). Nevertheless, in many of these studies, authors include different types of fractures (Mason types 2, 3, 4) and this makes hardly ever possible to deduce the results of isolated Mason type 2 fractures. Ring et al. (36) described good or excellent results in 93% of their patients. Meyer-Marcotty (37) also had 90% good or excellent results in their serie. Zarattini et al. (38) reported excellent or good functional outcome in 35 patients (97.1%). The results of our study are in line with those described in literature after ORIF.
Nonsurgical treatment of Mason type II fractures has the advantage of preserving normal kinematics of the elbow and avoiding complications that can frequently after surgery (36, 38, 39). Radial head resection can result in lateral elbow instability with chronic strain of the medial collateral ligament, proximal migration of the radius with subluxation of the distal radioulnar joint, attenuation of the interosseous membrane, and ulnar neuropathy (40–42). Conversely, patients treated nonsurgically have good clinical outcome with a low rate of complications. In our series, only 9 patients complained occasional pain, 2 patients perceived a mild instability of the elbow and 4 patients reported a loss of grip strength of less than 20%. To our knowledge, these complications can be related to osteoarthritis secondary to the fracture. This paper shows the effectiveness of conservative treatment of Mason II fractures in athletes with high functional demand, allowing return to sports at previous levels of activity in all patients. We therefore believe that an immobilization for 2 weeks in this type of fracture does not lead to permanent rigidity of the elbow, but allows an optimal recovery of the ROM after removal of the brace. This observational study is based on single-center retrospective research. It specifically describes the results of nonsurgical treatment of stable and isolated Mason type II fractures with preserved elbow and forearm motion at first examination after injury. We only included moderately displaced radial head fractures, whereas other studies have included more displaced fractures, comminuted fractures, and radial neck fractures. The main limits of the present study are represented by the lack of randomization and the absence of a comparative group of patients treated operatively. Because of this, it is difficult to draw any definite conclusion regarding the treatment of choice of isolated Mason type II fractures.
This retrospective study suggests that displacement from 2 to 5 mm in Mason type II radial head fractures is not necessarily an indication for surgical fixation in isolated fractures of the radial head. Results of this study clearly show how a conservative treatment may provide good or excellent clinic outcome.
References
- 1.Kaas L, van Riet RP, Vroemen JPAM, Eygendaal D. The epidemiology of radial head fractures. J Shoulder Elbow Surg. 2010;19:520–523. doi: 10.1016/j.jse.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 2.Duckworth AD, Clement ND, Jenkins PJ, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of radial head and neck fractures. J Hand Surg Am. 2012;37:112–119. doi: 10.1016/j.jhsa.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 3.Kaas L, Struijs PA, Ring D, van Dijk CN, Eygendaal D. Treatment of Mason type II radial head fractures without associated fractures or elbow dislocation: a systematic review. J Hand Surg Am. 2012;37:1416–1421. doi: 10.1016/j.jhsa.2012.03.042. [DOI] [PubMed] [Google Scholar]
- 4.van Riet RP, Morrey BF, O’Driscoll SW, Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clin Orthop Relat Res. 2005;441:351–355. doi: 10.1097/01.blo.0000180606.30981.78. [DOI] [PubMed] [Google Scholar]
- 5.van Riet RP, Morrey BF. Documentation of associated injuries occurring with radial head fracture. Clin Orthop Relat Res. 2008;466:130–134. doi: 10.1007/s11999-007-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mason ML. Some observation on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–132. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 7.Johnston GW. A follow up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J. 1962;31:51–56. [PMC free article] [PubMed] [Google Scholar]
- 8.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fractures. J Bone Joint Surg. 1986;68A:669–674. [PubMed] [Google Scholar]
- 9.Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10. doi: 10.5435/00124635-199701000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Sheps DM, Kiefer KR, Boorman RS, Donaghy J, Lalani A, Walker R, Hildebrand KA. The interobserver reliability of classification systems for radial head fractures: the Hotchkiss modification of the Mason classification and the AO classification systems. Can J Surg. 2009;52:277–282. [PMC free article] [PubMed] [Google Scholar]
- 11.van Riet RP, van Glabbeek F, Morrey BF. Radial head fracture: general consideration, conservative treatment and open reduction and internal fixation. In: Morrey B, Sanchez-Sotelo J, editors. The elbow and its disorders. 4th ed. Philadelphia: Saunders; 2009. pp. 359–381. [Google Scholar]
- 12.Struijis PA, Smit G, Steller EP. Radial head fractures: effectiveness of conservative treatment versus surgical intervention. A systematic review. Arch Orthop Trauma Surg. 2007;127:125–130. doi: 10.1007/s00402-006-0240-4. [DOI] [PubMed] [Google Scholar]
- 13.Herbertsson P, Josefsson PO, Hasserius R, Karlsson C, Besjakov J, Karlsson MK. Displaced Mason type I fractures of the radial head and neck in adults: a fifteen- to thirty-year follow-up study. J Shoulder Elbow Surg. 2005;14:73–77. doi: 10.1016/j.jse.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Rosenblatt Y, Athwal GS, Faber KJ. Current recommendations for the treatment of radial head fractures. Orthop Clin North Am. 2008;39:173–185. vi. doi: 10.1016/j.ocl.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Pike JM, Athwal GS, Faber KJ, King GJ. Radial head fractures an update. J Hand Surg Am. 2009;34:557–565. doi: 10.1016/j.jhsa.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 16.Faldini C, Nanni M, Leonetti D, Capra P, Bonomo M, Persiani V, Galante C, Giannini S. Early radial head excision for displaced and comminuted radial head fractures: considerations and concerns at long-term follow-up. J Orthop Trauma. 2012;26:236–240. doi: 10.1097/BOT.0b013e318220af4f. [DOI] [PubMed] [Google Scholar]
- 17.Janssen RP, Vegter J. Resection of the radial head after Mason type III fractures of the elbow: follow up at 16 to 30 years. J Bone Joint Surg Br. 1998;80:231–233. doi: 10.1302/0301-620x.80b2.8255. [DOI] [PubMed] [Google Scholar]
- 18.Ikeda M, Sugiyama K, Kang C, Takagaki T, Oka Y. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am. 2005;87:76–84. doi: 10.2106/JBJS.C.01323. [DOI] [PubMed] [Google Scholar]
- 19.Grewal R, MacDermid JC, Faber KJ, Drosdowech DS, King GJ. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty. Study of outcomes. J Bone Joint Surg Am. 2006;88:2192–2200. doi: 10.2106/JBJS.E.00962. [DOI] [PubMed] [Google Scholar]
- 20.Radin EL, Riseborough EJ. Fractures of the radial head. A review of eighty-eight cases and analysis of the indications for excision of the radial head and non-operative treatment. J Bone Joint Surg Am. 1966;48:1055–1064. [PubMed] [Google Scholar]
- 21.Coleman DA, Blair WF, Shurr D. Resection of the radial head for fracture of the radial head, long-term follow up for seventeen cases. J Bone Joint Surg Am. 1987;69:385–392. [PubMed] [Google Scholar]
- 22.King GJ, Evans DC, Kellarn JF. Open reduction and internal fixation of radial head fractures. J Orthop Trauma. 1991;5:21–28. doi: 10.1097/00005131-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Esser RD, Davis S, Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma. 1995;9:318–323. doi: 10.1097/00005131-199509040-00008. [DOI] [PubMed] [Google Scholar]
- 24.Khalfayan EE, Culp RW, Alexander AH. Mason type II radial head fractures: operative versus nonoperative treatment. J Orthop Trauma. 1992;6:283–289. doi: 10.1097/00005131-199209000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Herbertsson P, Josefsson PO, Hasserius R, Karlsson C, Besjakov J, Karlsson M. Uncomplicated Mason type II and III fractures of the radial head and neck in adults. A long-term follow-up study. J Bone Joint Surg Am. 2004;86-A:569–574. doi: 10.2106/00004623-200403000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Duckworth AD, McQueen MM, Ring D. Fractures of the radial head. Bone Joint J. 2013;95-B(2):151–159. doi: 10.1302/0301-620X.95B2.29877. [DOI] [PubMed] [Google Scholar]
- 27.Morrey BF, Chao EY, Hui FC. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am. 1979;61:63–68. [PubMed] [Google Scholar]
- 28.Morrey BF, An KN, Stormont TJ. Force transmission through the radial head. J Bone Joint Surg Am. 1988;70:250–256. [PubMed] [Google Scholar]
- 29.Druschel M, Palmer G, Baratz ME, Miller MC. Mason II fractures with three millimeters displacement require reduction. Presented at the American Society of Biomechanics 2010 Conference; August 18–21, 2010; Providence, RI. [Google Scholar]
- 30.Ruchelsman DE, Christoforou D, Jupiter JB. Fractures of the radial head and neck. J Bone Joint Surg. 2013;95:469–478. doi: 10.2106/JBJS.J.01989. [DOI] [PubMed] [Google Scholar]
- 31.Yoon A, Athwal GS, Faber KJ, King GJ. Radial head fractures. J Hand Surg Am. 2012;37:2626–2634. doi: 10.1016/j.jhsa.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Bakalim G. Fractures of radial head and their treatment. Acta Orthop Scand. 1970;41:320–31. doi: 10.3109/17453677008991518. [DOI] [PubMed] [Google Scholar]
- 33.Akesson T, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg. 2006;88A:1909–1014. doi: 10.2106/JBJS.E.01052. [DOI] [PubMed] [Google Scholar]
- 34.Duckworth AD, Watson BS, Will EM, Petrisor BA, Walmsley PJ, Court-Brown CM, McQueen MM. Radial head and neck fractures: functional results and predictors of outcome. J Trauma. 2011;71:643–648. doi: 10.1097/TA.0b013e3181f8fa5f. [DOI] [PubMed] [Google Scholar]
- 35.Furey MJ, Sheps DM, White NJ, Hildebrand KA. A retrospective cohort study of displaced segmental radial head fractures: is 2 mm of articular displacement an indication for surgery? J Shoulder and Elbow Surg. 2013;22:636–641. doi: 10.1016/j.jse.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 36.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Meyer-Marcotty MV, Lahoda LU, Hahn MP, Muhr G. Differential therapy for radial head fractures: critical analysis of the results from 53 patients. Unfallchirurg. 2002;105:532–539. doi: 10.1007/s00113-001-0380-5. [DOI] [PubMed] [Google Scholar]
- 38.Zarattini G, Galli S, Marchese M, Di Mascio L, Pazzaglia UE. The surgical treatment of isolated Mason type II fractures of the radial head in adults: comparison between radial head resection and open reduction and internal fixation. J Orthop Trauma. 2012;26:229–235. doi: 10.1097/BOT.0b013e318220a227. [DOI] [PubMed] [Google Scholar]
- 39.Smith GR, Hotchkiss RN. Radial head and neck fractures: anatomic guidelines for proper placement of internal fixation. J Shoulder Elbow Surg. 1996;5:113–117. doi: 10.1016/s1058-2746(96)80005-x. [DOI] [PubMed] [Google Scholar]
- 40.Mikic ZD, Vukadinovic SM. Late results in fractures of the radial head treated by excision. Clin Orthop Relat Res. 1983;181:220–228. [PubMed] [Google Scholar]
- 41.Stephen IB. Excision of the radial head for closed fractures. Acta Orthop Scand. 1981;52:409–412. doi: 10.3109/17453678109050121. [DOI] [PubMed] [Google Scholar]
- 42.Postacchini F, Morace GB. Radial head fractures treated by resection. Long term results. Ital J Orthop Traumatol. 1992;18:323–330. [PubMed] [Google Scholar]