Abstract
IMPORTANCE
Patients with stroke often have a decline in blood pressure after thrombolysis. Neurologic improvement could result from recanalization or better collateral flow despite persistent occlusion. We hypothesized that neurologic improvement with concurrent decline in blood pressure may be a clinical sign of recanalization after intravenous tissue plasminogen activator.
OBSERVATIONS
Patients treated with intravenous tissue plasminogen activator at Suburban Hospital, Bethesda, Maryland, and MedStar Washington Hospital Center, Washington, DC, from 1999 to 2009 were included in the study if they had pretreatment and 24-hour magnetic resonance angiographic scans, National Institutes of Health Stroke Scale scores at those times, and proximal middle cerebral artery occlusion demonstrated prior to treatment. The recanalization status on 24-hour magnetic resonance angiography was classified as none, partial, or complete. Seventeen patients met study criteria. On 24-hour magnetic resonance angiography, 3 patients had no recanalization, 8 had partial recanalization, and 6 had complete recanalization. At 24 hours after thrombolysis, neurologic improvement with concurrent decline in systolic blood pressure of 20 mm Hg or greater was seen in 4 patients with partial recanalization, 4 patients with complete recanalization, and none of the patients with no recanalization.
CONCLUSIONS AND RELEVANCE
Neurologic improvement with concurrent decline in systolic blood pressure of 20 mm Hg or greater after intravenous tissue plasminogen activator may be a clinical sign of recanalization. This observation needs confirmation in a larger cohort.
Patients with stroke usually have some spontaneous decline in blood pressure (BP) after the vascular event and after thrombolysis. The decrease in BP may be secondary to atrial fibrillation with rapid ventricular response1,2; improvement in symptoms, such as nausea or headache; medication effects; or systemic bleeding secondary to tissue plasminogen activator (tPA). There are reports describing decreases in BP following intravenous (IV) or intra-arterial recanalization procedures.3,4 The goal of tPA is to achieve recanalization and restore blood flow to the ischemic brain, resulting in neurologic improvement. However, in some patients, neurologic improvement might result from improved collateral flow despite persistent occlusion. Based on our clinical observation that a patient who had recanalized after IV tPA had neurologic improvement associated with a decline in systolic BP (SBP) of approximately 30 mm Hg, we hypothesized that the combination of these findings might be a clinical sign of recanalization after IV tPA.
Methods
Patients
The Lesion Evolution of Stroke Ischemia On Neuroimaging5 registry includes patients with ischemic stroke evaluated at Suburban Hospital, Bethesda, Maryland, and MedStar Washington Hospital Center, Washington, DC, between August 1999 and October 2009. Patients from the registry were included in our study if they were treated with standard IV tPA, had a National Institutes of Health Stroke Scale (NIHSS) score and magnetic resonance angiography (MRA) done before and 24 hours after IV tPA treatment, and had an M1 middle cerebral artery (MCA) occlusion on pretreatment MRA. Patients were excluded if they had a pretreatment SBP of less than 120 mm Hg, required treatment with pressors, had M2 or tandem internal carotid artery (ICA)/M1 occlusion, or the medical record was not available to abstract BP measurements. We restricted the study to only M1 occlusion to keep the study sample uniform; minimize bias; and avoid having subgroups with M1, M2, and ICA occlusions. We assumed that the patients with M2 occlusion may not have very high BP or NIHSS score at presentation compared with those with M1 occlusion; therefore, evaluating for BP and NIHSS score changes might not be useful in this group. Patients with ICA occlusion or tandem ICA/M1 occlusion are less likely to recanalize with IV tPA; therefore, this group could introduce bias when evaluating for BP and NIHSS score changes with recanalization status after IV tPA. Office of Human Subjects Research exemptions and institutional review board approvals from the National Institute of Neurological Disorders and Stroke, Bethesda, Maryland; Suburban Hospital, Bethesda, Maryland; and Medstar Health Research Institute, Washington, DC, were obtained for use of clinical and research data.
Outcomes
Neurologic improvement was defined as improvement of 4 or more points on the NIHSS or an NIHSS score of 0 at 24 hours after IV tPA. The BP decline was calculated as the difference between the emergency department triage pre-tPA BP and the average of the last 3 hourly readings preceding the 24-hour MRA. Three investigators blinded to clinical data determined recanalization on 24-hour MRA. No recanalization was defined as persistent complete MCA occlusion. Complete recanalization was defined as complete M1 recanalization and reperfusion of the MCA territory on 24-hour MRA without any visible distal M2/3 cutoff by clot migration. Those patients with vascular imaging findings between none and complete recanalization were grouped as partial recanalization. We did not evaluate for markers of collateralization in our study.
Mattle et al4 found that patients recanalized by intraarterial procedures had a decrease in mean SBP of 17.3 mm Hg. Therefore, we evaluated for the association of (1) decline in SBP of 20 mm Hg or greater, (2) neurologic improvement, and (3) neurologic improvement with a decline in SBP of 20 mm Hg or greater, with the recanalization status at 24-hour post-IV thrombolysis.
Results
Seventeen patients met the study criteria as described in the Figure. Table 1 shows the demographic, clinical, and recanalization variables of the patients with and without neurologic improvement; 13 were women, 13 were white, and 10 had atrial fibrillation. The mean (SD) age of the patients was 76 (13) years and the median baseline NIHSS score was 15. At 24 hours after IV tPA, 3 patients had no recanalization, 8 had partial recanalization, and 6 had complete recanalization.
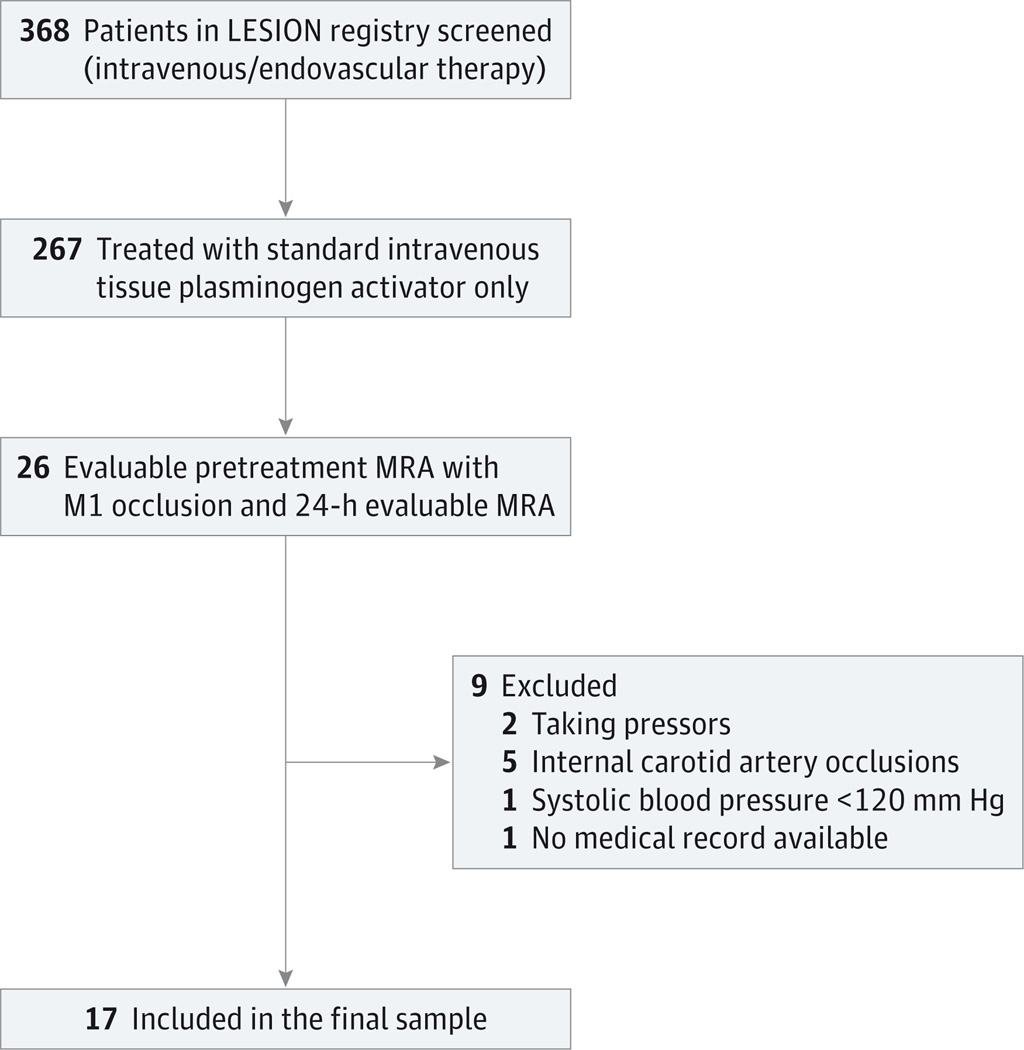
Figure. Study Sample From the Lesion Evolution of Stroke Ischemia On Neuroimaging (LESION) Registry.
A total of 368 patients were screened in the LESION database and 17 patients met the study criteria. MRA indicates magnetic resonance angiography.
Table 1.
Demographic, Clinical, and Recanalization Variables of Patients With NI (Patients 1–12) and Without NI (Patients 13–17)
| Patient No./ Sex/Age, y |
NIHSS Scorea | Pre-tPA BP, mm Hg |
24-h Post-tPA BP, mm Hgb |
BP Treatmentc |
Decline in SBP ≥20 mm Hg |
NI + Decline in SBP ≥20 mm Hg |
Recanalization 24-h MRA |
|
|---|---|---|---|---|---|---|---|---|
| Pre-tPA | At 24 h |
|||||||
| 1/F/81 | 1 | 0 | 160/59 | 145/63 | No | No | No | Complete |
| 2/M/65 | 5 | 0 | 126/88 | 122/86 | No | No | No | Complete |
| 3/F/84 | 25 | 17 | 135/82 | 158/89 | No | No | No | None |
| 4/F/63 | 9 | 3 | 127/74 | 125/83 | No | No | No | None |
| 5/M/67 | 11 | 2 | 151/77 | 112/61 | No | Yes | Yes | Partial |
| 6/F/83 | 15 | 10 | 162/84 | 136/65 | Yes | Yes | Yes | Partial |
| 7/F/47 | 6 | 0 | 144/96 | 124/73 | No | Yes | Yes | Partial |
| 8/F/83 | 8 | 0 | 172/78 | 131/60 | No | Yes | Yes | Complete |
| 9/F/83 | 24 | 14 | 144/87 | 108/66 | No | Yes | Yes | Partial |
| 10/F/92 | 23 | 14 | 165/82 | 125/77 | No | Yes | Yes | Complete |
| 11/F/88 | 21 | 10 | 211/147 | 149/92 | Yes | Yes | Yes | Complete |
| 12/F/83 | 27 | 12 | 172/81 | 148/78 | No | Yes | Yes | Complete |
| 13/F/79 | 4 | 7 | 159/93 | 143/78 | No | No | No | Partial |
| 14/M/54 | 17 | 14 | 145/84 | 127/69 | Yes | No | No | Partial |
| 15/M/74 | 13 | 20 | 153/74 | 160/70 | No | No | No | Partial |
| 16/F/94 | 20 | 25 | 173/85 | 147/65 | No | Yes | No | Partial |
| 17/F/74 | 26 | 23 | 150/115 | 119/52 | Yes | Yes | No | None |
Abbreviations: BP, blood pressure; F, female; M, male; MRA, magnetic resonance angiography; NI, neurologic improvement; NIHSS, National Institutes of Health Stroke Scale; SBP, systolic blood pressure; tPA, tissue plasminogen activator.
NI defined as improvement in NIHSS score of 4 or more points or NIHSS score of 0 at 24 hours post-tPA treatment.
Average of the last 3 hourly readings of BP prior to 24-hour MRA.
Treatment with intravenous antihypertensives in the first 24 hours per tPA monitoring protocol.
The association of neurologic improvement, decline in SBP of 20 mm Hg or greater, or both with the MCA recanalization status on 24-hour MRA after IV tPA is shown in Table 2. All 6 patients with complete recanalization and 4 with partial recanalization had neurologic improvement but there were 2 patients with no recanalization who also had neurologic improvement. Four patients with complete recanalization and 5 with partial recanalization had a decline in SBP of 20 mm Hg or greater. One patient with no recanalization also had a decline in SBP of 20 mm Hg or greater. Neurologic improvement with a concurrent decline in SBP of 20 mm Hg or greater was not observed in any patient who did not have recanalization at 24 hours post-IV tPA. Four patients with complete recanalization and 4 with partial recanalization had combined neurologic improvement, with a decline in SBP of 20 mm Hg or greater.
Table 2.
Association of Neurologic Improvement, Decline in SBP of 20 mm Hg or Greater, or Both With Recanalization Status on 24-Hour MRA
| Variable | Recanalization Status | ||
|---|---|---|---|
| None (n = 3) |
Partial (n = 8) |
Complete (n = 6) |
|
| Neurologic improvement | 2 | 4 | 6 |
| SBP decline ≥20 mm Hg | 1 | 5 | 4 |
| Neurologic improvement and SBP decline ≥20 mm Hg |
0 | 4 | 4 |
Abbreviations: MRA, magnetic resonance angiography; SBP, systolic blood pressure.
Discussion
We found that neurologic improvement by 4 or more points on the NIHSS or an NIHSS score of 0 at 24 hours after IV tPA with a concurrent decline in SBP of 20 mm Hg or greater was more likely to be associated with recanalization after thrombolysis. If confirmed by larger studies, this clinical correlation could be useful in the management of patients with acute ischemic stroke. Patients who have recanalized may not need aggressive treatment with IV fluids or rarely pressors for management of declining blood pressure after stroke. Avoiding these therapies could be particularly valuable for those with congestive heart failure. In patients considered for bridging IV tPA with endovascular interventions, repeat vessel imaging could be considered prior to the procedure if there is neurologic improvement associated with a decrease in SBP of 20 mm Hg or greater because this finding might suggest recanalization.
Not all patients with neurologic improvement had recanalization. Improvement may have been due to good collateral flow from higher BP.6 In our series, 2 patients (patients 3 and 4; Table 1) had neurologic improvement without recanalization; neither had a decline in SBP of 20 mm Hg or greater. Four patients received 1 dose of IV antihypertensive medication, either labetalol hydrochloride or hydralazine hydrochloride, in the first 24 hours per tPA monitoring protocol. None of the patients received any oral antihypertensive medications during the first 24 hours after tPA.
The association of recanalization, decline in BP, and neurologic improvement may not be as useful in patients with lower NIHSS scores or pre-tPA SBP at baseline. Whereas the 4 patients (patients 8, 10, 11, and 12; Table 1) who had complete recanalization and demonstrated neurologic improvement with concurrent decline in SBP of 20 mm Hg or greater at 24 hours after IV t-PA had higher NIHSS scores at baseline (scores of 8, 23, 21, and 27 respectively), the 2 patients (patients 1 and 2; Table 1) who completely recanalized but did not have a decline in SBP of 20 mm Hg or greater had lower NIHSS scores at baseline (scores of 1 and 5, respectively). Patient 2 also had lower pre-tPA SBP of 126 mm Hg.
A limitation of our study was the small sample size. We also did not evaluate the BP and NIHSS score changes in patients without MCA occlusion on pre-tPA treatment scan. However, this is a clinically relevant proof-of-concept, hypothesis-generating study. The decline in SBP of 20 mm Hg or greater was considered to reflect recanalization based on previous studies. These observations need to be confirmed with larger studies. Our future plan is to verify our findings in a larger cohort with inclusion of patients with and without MCA occlusion on pre-tPA treatment scan. The clinical sign to determine recanalization may not apply when BP changes are influenced by other conditions, such as atrial fibrillation with rapid ventricular response, systemic hemorrhage, and intubation, or when there is lower baseline pre-tPA NIHSS scores or SBP. Neurologic improvement with a concurrent decline in SBP indicates a high likelihood of recanalization but its absence does not necessarily indicate nonrecanalization.
Conclusions
Neurological improvement with a concurrent decline in SBP may be a useful clinical sign to determine recanalization.
Acknowledgments
Dr Adams reviews outcome events for clinical trials sponsored by Merck and serves on the data and safety monitoring board for a clinical study funded by Medtronic. He is a consultant to Pierre Fabre (France) and has funding from St Jude Medical. Dr Merino receives salary support from The BMJ for his role as US clinical research editor.
Funding/Support: This research was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Neurological Disorders and Stroke. Dr Adams has grant support from the National Institute of Neurological Disorders and Stroke.
Role of the Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We acknowledge and thank the National Institutes of Health Stroke Team; the staffs of Suburban Hospital, Bethesda, Maryland, and MedStar Washington Hospital Center, Washington, DC; and the patients for their valuable participation.
Footnotes
Author Contributions: Dr Nagaraja had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Nagaraja, Warach, Latour, Merino.
Acquisition, analysis, or interpretation of data: Nagaraja, Hsia, Adams, Auh, Latour, Merino.
Drafting of the manuscript: Nagaraja.
Critical revision of the manuscript for important intellectual content: Warach, Hsia, Adams, Auh, Latour, Merino.
Study supervision: Merino.
Conflict of Interest Disclosures No other disclosures were reported.
REFERENCES
- 1.Seet RC, Zhang Y, Rabinstein AA, Wijdicks EF. Risk factors and consequences of atrial fibrillation with rapid ventricular response in patients with ischemic stroke treated with intravenous thrombolysis. J Stroke Cerebrovasc Dis. 2013;22(2):161–165. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Wasmund SL, Li JM, Page RL, et al. Effect of atrial fibrillation and an irregular ventricular response on sympathetic nerve activity in human subjects. Circulation. 2003;107(15):2011–2015. doi: 10.1161/01.CIR.0000064900.76674.CC. [DOI] [PubMed] [Google Scholar]
- 3.Delgado-Mederos R, Ribo M, Rovira A, et al. Prognostic significance of blood pressure variability after thrombolysis in acute stroke. Neurology. 2008;71(8):552–558. doi: 10.1212/01.wnl.0000318294.36223.69. [DOI] [PubMed] [Google Scholar]
- 4.Mattle HP, Kappeler L, Arnold M, et al. Blood pressure and vessel recanalization in the first hours after ischemic stroke. Stroke. 2005;36(2):264–268. doi: 10.1161/01.STR.0000153052.59113.89. [DOI] [PubMed] [Google Scholar]
- 5.Freeman JW, Luby M, Merino JG, et al. Negative diffusion-weighted imaging after intravenous tissue-type plasminogen activator is rare and unlikely to indicate averted infarction. Stroke. 2013;44(6):1629–1634. doi: 10.1161/STROKEAHA.111.000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rordorf G, Cramer SC, Efird JT, Schwamm LH, Buonanno F, Koroshetz WJ. Pharmacological elevation of blood pressure in acute stroke: clinical effects and safety. Stroke. 1997;28(11):2133–2138. doi: 10.1161/01.str.28.11.2133. [DOI] [PubMed] [Google Scholar]