Highlights
-
•
Migration of a biliary stent can cause life-threatening complications.
-
•
When a stent migration occurs, in case of complications, surgical removal is the only treatment option.
-
•
Among the complications associated with stent migration, intestinal bleeding, obstruction and perforation are of outmost importance.
Keywords: Stent migration, Biliary stents, Intestinal perforation, Hartmann’s procedure
Abstract
Introduction
Biliary stent migration (proximal or distal) occurs in 6% of all cases. The majority of these migrating stents are passing through the intestine, without causing any complications. Usually when a stent migration occurs, endoscopic retrieval is the proper treatment option, except in case of complications when surgical removal is the only treatment option. This report presents a case of a biliary stent which migrated and caused a sigmoid colon perforation.
Presentation of case
A 75 years old female patient presented to the emergency department with diffuse abdominal pain, nausea and vomiting. Clinical examination showed distended abdomen and signs of peritoneal irritation.
CT scan of the abdomen revealed free gas and fluid in the left iliac fossa, as well as a foreign body penetrating the sigmoid colon. Emergency laparotomy was performed. A plastic stent was found perforating the sigmoid colon through a diverticulum. The rest of the sigmoid colon was intact presenting only uncomplicated diverticula. Hartmann’s operation was performed, involving the diseased segment, together with part of the descending colon due to profound diverticulosis. Patient’s post-surgical course was uneventful and was discharged on postoperative day 10.
Discussion
Migration of a biliary stent can cause life-threatening complications such as perforation of the intestine and peritonitis. The migration of the stent from the biliary tree may be mostly asymptomatic except in cases of intestinal perforation that immediate surgery is the proper treatment option. On the other hand, even in cases of benign lesions of the bile duct, the stent should be removed immediately after dislocation in order to reduce the risk of secondary complications such as obstruction, infection or perforation.
Conclusion
In cases of non-complicated stent migration endoscopic retrieval is the indicated treatment. In patients who suffer serious complications due to stent dislocation, emergency surgery may be the proper treatment option.
1. Introduction
Endoscopic biliary stents can be used for management of a variety of pancreatic, biliary and hepatic benign diseases or malignancies such as choledocholithiasis, biliary leaks, pancreatitis, pancreatic and biliary carcinomas [1]. Currently two types of stents are being widely used. Plastic stents, which are less expensive, easier to remove or replace, appearing a higher risk of being clogged by debris or dislodged in the gastrointestinal tract and metallic stents which are more expensive, non-replaceable with minor risk of clogging or dislocation [1], [2], [3].
Fortunately, distal stent migration is a rare complication, which occurs in 6% of all cases [4], [5], [6] most commonly affected the duodenum [5], [6], whereas small bowel and colon are rarely affected [7], [8], [9]. It has been shown that in order to reduce the risk of migration, a stent should be placed adjacent to the sphincter of Oddi [10].
Migration is more common in patients with benign than malignant diseases of the biliary tree [11], [12], [13]. Benign stenosis due to inflammation may contribute to stent migration. After regression of the local inflammatory reaction, a stent can easily move within the biliary tree. Among the complications associated with stent migration, intestinal bleeding, obstruction and perforation are of outmost importance [11], [12]. In cases of intestinal perforation, the stent should be immediately removed; otherwise it may lead to peritonitis and potential formation of intra-abdominal or retroperitoneal abscess. Furthermore, pelvic abscesses, colovesical or colocutaneous fistulas and necrotizing fasciitis due to perforation of the colon may also occur [14], [15], [16]. According to the literature, perforation of the colon appears more frequently by plastic stents [17], [18]. This case report study has been reported in line with the SCARE criteria [19] and presents a rare case of sigmoid colon perforation, due to plastic biliary stent migration.
2. Case report
A 75 years old female patient presented to the emergency department with diffuse abdominal pain, distended abdomen, nausea and vomiting. Clinical examination revealed tenderness over the left iliac fossa and supra pubic region and signs of peritonitis. White blood cells and C − reactive protein were abnormally elevated. She underwent an open cholecystectomy for empyema 2 months earlier, which was immediately followed by ERCP due to post-operative obstructive jaundice. During ERCP, a small plastic stent was placed into the common bile duct (CBD), after removal of CBD sludge. During the surgical procedure, the stent was dislocated and a larger stent was inserted into the CBD. ERCP was repeated a month later and the stent was successfully removed from the CBD, however no endoscopic or radiological tests were performed in order to locate and retrieve the first one. Post-ERCP and before her admission to the ER department, patient was completely asymptomatic.
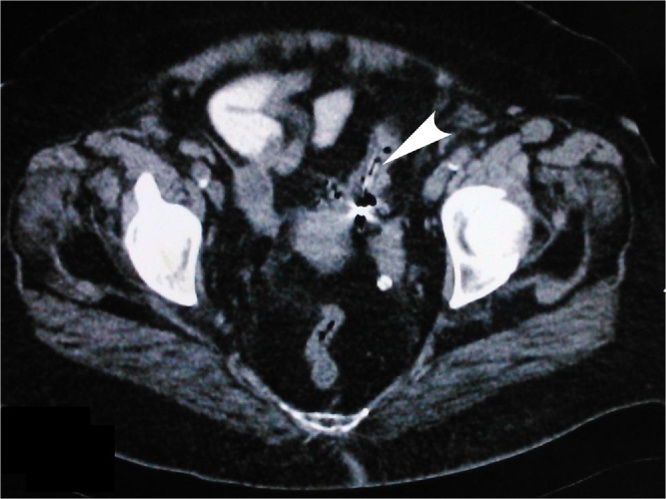
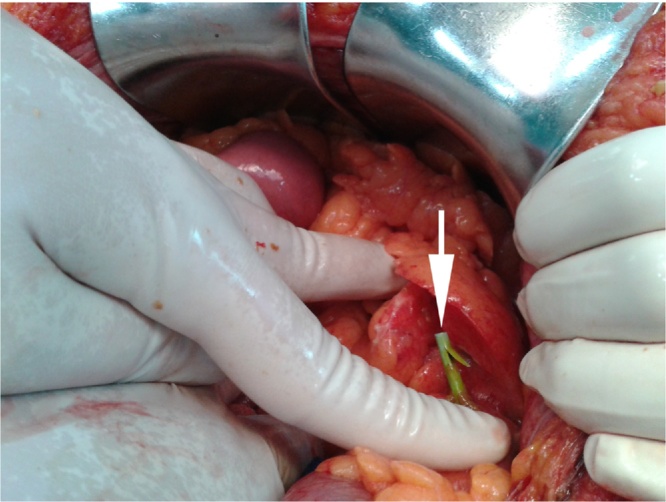
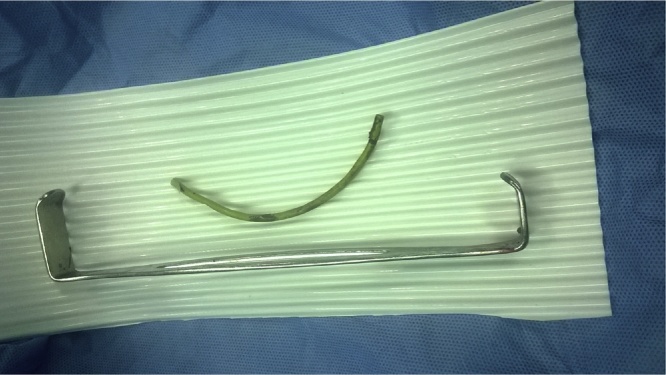
After clinical evaluation in the emergency department, abdominal CT scan analysis revealed free gas in the abdomen, free fluid in left iliac fossa and lesser pelvis and a foreign body penetrating the mid-sigmoid colon (Fig. 1). Emergency laparotomy was performed and a green plastic stent was found perforating the sigmoid colon through a diverticulum (Fig. 2, Fig. 3). Hartmann’s operation was performed by resection of the perforated sigmoid colon and part of the descending colon which revealed severe diverticulosis. Patient had an uneventful post-operative period and was discharged on 10th postoperative day. Approximately 6 months later patient was proceed in elective reoperation and bowel continuity was successfully established.
Fig. 1.
CT scan of the abdomen revealed free gas in the abdomen, free fluid in left iliac fossa and foreign body (arrowhead) penetrating at the sigmoid colon.
Fig. 2.
A green stent (arrow) was found penetrating the sigmoid colon.
Fig. 3.
The green plastic stent that was found perforating the sigmoid colon through a diverticulum.
3. Discussion
Introduction of endoscopic biliary stents is a common and useful procedure which contributes to decompression of the biliary system. In cases of long-term treatment, stent migration can cause complications which can lead to life-threatening situations and sometimes diagnosis can be difficult due to absence of typical symptoms. To date, a small number of works are available concerning sigmoid perforation from a biliary stent [15], [20], [21], [22], [23], [24], [25], [26], [27], [28]. In most cases, the patient had concurrent diverticulosis or abdominal adhesions, which increase the risk for colonic perforation [7], [25]. When stent migration is suspected, an endoscopic retrieval is highly indicated, whilst in case of evident perforation, laparotomy should be performed.
Conflict of interest
All authors declare no conflicts of interest
Funding
Our research had no funding.
Ethical approval
No ethics committee request was submitted.
Consent
Letter of consent was signed and obtained by the patient.
Author contribution
P. Siaperas, A. Ioannidis and I. Karanikas carried out the operation.
I. Drikos, A. Skarpas, A. Angelopoulos helped draft the manuscript.
A. Ioannidis, A. Skarpas collected all preoperative, perioperative and postoperative data.
Guarantor
Petros Siaperas.
Acknowledgement
We would like to thank the consultants of the Department of Surgery, at Sismanoglion General Hospital Athens, for kindly allowing the patient to be included in the study.
Contributor Information
Petros Siaperas, Email: petrossiap@yahoo.gr.
Argyrios Ioannidis, Email: agis.ioannidis@gmail.com.
Andreas Skarpas, Email: andrewskarpas@gmail.com.
Argiris Angelopoulos, Email: aargangel@gmail.com.
Ioannis Drikos, Email: johndrikos@yahoo.com.
Ioannis Karanikas, Email: ikaranikas@yahoo.gr.
References
- 1.Costamagna G., Pandolfi M., Mutignani M., Spada C., Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest. Endosc. 2001;54(2):162–168. doi: 10.1067/mge.2001.116876. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal N., Sharma B.C., Garg S., Kumar R., Sarin S.K. Endoscopic management of postoperative bile leaks. Hepatobiliary Biliary Pancreatic Dis. Int.: HBPD INT. 2006;5(2):273–277. [PubMed] [Google Scholar]
- 3.Levy M.J., Baron T.H., Gostout C.J., Petersen B.T., Farnell M.B. Palliation of malignant extrahepatic biliary obstruction with plastic versus expandable metal stents: An evidence-based approach. Clin. Gastroenterol. Hepatol. 2004;2(4):273–285. doi: 10.1016/s1542-3565(04)00055-2. [DOI] [PubMed] [Google Scholar]
- 4.Miller G., Yim D., Macari M., Harris M., Shamamian P. Retroperitoneal perforation of the duodenum from biliary stent erosion. Curr. Surg. 2005;62(5):512–515. doi: 10.1016/j.cursur.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Melita G., Curro G., Iapichino G., Princiotta S., Cucinotta E. Duodenal perforation secondary to biliary stent dislocation: a case report and review of the literature. Chir. Ital. 2005;57(3):385–388. [PubMed] [Google Scholar]
- 6.Basile A., Macri A., Lamberto S., Caloggero S., Versaci A., Famulari C. Duodenoscrotal fistula secondary to retroperitoneal migration of an endoscopically placed plastic biliary stent. Gastrointest. Endosc. 2003;57(1):136–138. doi: 10.1067/mge.2003.37. [DOI] [PubMed] [Google Scholar]
- 7.Diller R., Senninger N., Kautz G., Tubergen D. Stent migration necessitating surgical intervention. Surg. Endosc. 2003;17(11):1803–1807. doi: 10.1007/s00464-002-9163-5. [DOI] [PubMed] [Google Scholar]
- 8.Blake A.M., Monga N., Dunn E.M. Biliary stent causing colovaginal fistula: case report. JSLS: J. S. Laparoendoscopic Surg./Soc. Laparoendoscopic Surg. 2004;8(1):73–75. [PMC free article] [PubMed] [Google Scholar]
- 9.Klein U., Weiss F., Wittkugel O. [Migration of a biliary Tannenbaum stent with perforation of sigmoid diverticulum] RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2001;173(11):1057. doi: 10.1055/s-2001-18306. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen F.M., Lassen A.T., Schaffalitzky de Muckadell O.B. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest. Endosc. 1998;48(6):574–579. doi: 10.1016/s0016-5107(98)70038-0. [DOI] [PubMed] [Google Scholar]
- 11.Jendresen M.B., Svendsen L.B. Proximal displacement of biliary stent with distal perforation and impaction in the pancreas. Endoscopy. 2001;33(2):195. doi: 10.1055/s-2001-11920. [DOI] [PubMed] [Google Scholar]
- 12.Liebich-Bartholain L., Kleinau U., Elsbernd H., Buchsel R. Biliary pneumonitis after proximal stent migration. Gastrointest. Endosc. 2001;54(3):382–384. doi: 10.1067/mge.2001.113646. [DOI] [PubMed] [Google Scholar]
- 13.Culp W.C., McCowan T.C., Lieberman R.P., Goertzen T.C., LeVeen R.F., Heffron T.G. Biliary strictures in liver transplant recipients: treatment with metal stents. Radiology. 1996;199(2):339–346. doi: 10.1148/radiology.199.2.8668775. [DOI] [PubMed] [Google Scholar]
- 14.Wilhelm A., Langer C., Zoeller G., Nustede R., Becker H. Complex colovesicular fistula: a severe complication caused by biliary stent migration. Gastrointest. Endosc. 2003;57(1):124–126. doi: 10.1067/mge.2003.71. [DOI] [PubMed] [Google Scholar]
- 15.Anderson E.M., Phillips-Hughes J., Chapman R. Sigmoid colonic perforation and pelvic abscess complicating biliary stent migration. Abdom. Imaging. 2007;32(3):317–319. doi: 10.1007/s00261-006-9067-2. [DOI] [PubMed] [Google Scholar]
- 16.Figueiras R.G., Echart M.O., Figueiras A.G., Gonzalez G.P. Colocutaneous fistula relating to the migration of a biliary stent. Eur. J. Gastroenterol. Hepatol. 2001;13(10):1251–1253. doi: 10.1097/00042737-200110000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Mistry B.M., Memon M.A., Silverman R., Burton F.R., Varma C.R., Solomon H., Garvin P.J. Small bowel perforation from a migrated biliary stent. Surg. Endosc. 2001;15(9):1043. doi: 10.1007/s004640041008. [DOI] [PubMed] [Google Scholar]
- 18.Mofidi R., Ahmed K., Mofidi A., Joyce W.P., Khan Z. Perforation of ileum: an unusual complication of distal biliary stent migration. Endoscopy. 2000;32(11):S67. [PubMed] [Google Scholar]
- 19.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S. Orgill DP and the SCARE Group. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Elliott M., Boland S. Sigmoid colon perforation following a migrated biliary stent. ANZ J. Surg. 2003;73(8):669–670. doi: 10.1046/j.1445-2197.2003.02698.x. [DOI] [PubMed] [Google Scholar]
- 21.Belyaev O., Muller C.A., Uhl W. Double sigmoid colon perforation by a migrated biliary stent. Acta Chir. Belg. 2008;108(1):125–126. [PubMed] [Google Scholar]
- 22.Konstantinidis C., Varsos P., Kympouris S., Volteas S. Migrated biliary plastic stent causing double sigmoid colon perforation. J. Surg. Case Rep. 2014;2014(12) doi: 10.1093/jscr/rju134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malgras B., Pierret C., Tourtier J.P., Olagui G., Nizou C., Duverger V. Double Sigmoid colon perforation due to migration of a biliary stent. J. Visc. Surg. 2011;148(5):e397–399. doi: 10.1016/j.jviscsurg.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 24.Chittleborough T.J., Mgaieth S., Kirkby B., Zakon J. Remove the migrated stent: sigmoid colon perforation from migrated biliary stent. ANZ J. Surg. 2014 doi: 10.1111/ans.12796. [DOI] [PubMed] [Google Scholar]
- 25.Mady R.F., Niaz O.S., Assal M.M. Migrated biliary stent causing perforation of sigmoid colon and pelvic abscess. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-206805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trovato C., Fiori G., Ravizza D., Tamayo D., Zampino M.G., Biffi R., Crosta C. Delayed colonic perforation after metal stent placement for malignant colorectal obstruction. Endoscopy. 2006;38(Suppl. 2):E96. doi: 10.1055/s-2006-944621. [DOI] [PubMed] [Google Scholar]
- 27.Lenzo N.P., Garas G. Biliary stent migration with colonic diverticular perforation. Gastrointest. Endosc. 1998;47(6):543–544. doi: 10.1016/s0016-5107(98)70262-7. [DOI] [PubMed] [Google Scholar]
- 28.Storkson R.H., Edwin B., Reiertsen O., Faerden A.E., Sortland O., Rosseland A.R. Gut perforation caused by biliary endoprosthesis. Endoscopy. 2000;32(1):87–89. doi: 10.1055/s-2000-87. [DOI] [PubMed] [Google Scholar]