Abstract
With few exceptions (e.g., Lesch-Nyhan syndrome), the specific nature of self-injury in relation to identified genetic syndromes associated with mental retardation is poorly understood. In the present study we surveyed the families of 62 persons with Prader-Willi syndrome to determine the prevalence, topographies, and specific body locations of self-injurious behavior. Self-injury was reported for 81% of the participants. Skin-picking was the most prevalent form, with the front of the legs and head being disproportionately targeted as preferred self-injury body sites. Individuals with the 15q11-q13 deletion injured significantly more body sites than did individuals with maternal disomy 15. Results are discussed in relation to previous self-injury body site findings and implications for the relevance of syndrome-specific behavioral phenotypes.
Prader-Willi syndrome, first described by Prader, Labhart, and Willi (1956), is caused by a deletion in the 15q11-q13 region of chromosome 15 and is associated with infantile hypotonia, hyperphagia, hypogonadism, food-seeking and perseveration, marked obesity, and mild to moderate mental retardation (Butler, Meaney, & Palmer, 1986; Butler, Levine, Le, Hall, & Cassidy, 1995; Cassidy, 1997; Dykens, Hodapp, Walsh, & Nash, 1992). The majority of Prader-Willi syndrome cases are caused by a paternal deletion of chromosome 15, but approximately one third of individuals have a maternal disomy 15, in which case both chromosome 15s come from the mother. Although Prader-Willi syndrome is known best for its association with food foraging, hoarding, and morbid obesity, a number of other significant aberrant behaviors are common among children and adults with Prader-Willi syndrome, including temper tantrums, emotional dysregulation, mood lability, anxiety, obsessions and compulsions, and self-injurious behavior—SIB (Cassidy et al., 1997; Dykens & Cassidy, 1996; Dykens, Hodapp, Walsh, & Nash, 1997).
Self-injurious behavior among persons with mental retardation, autism, and related developmental disabilities ranges from 5% to 60%, depending on the methods used and the populations sampled. Current prevalence estimates for adults with mental retardation suggest that approximately 1 person in 5 living in a residential treatment facility engages in some form of self-injury (Thompson & Gray, 1994). Serious health problems are posed by persistent self-injury, including blindness associated with eye-poking, subdural hemorrhage from forceful head-banging, infections from self-inflicted skin-picking, and anorectal disease resulting from rectal picking and digging (Bhargava, Putnam, Kocoshis, Rowe, & Hanchett, 1996; Hellings & Warnock, 1994). Self-injurious behaviors are among the most clinically problematic behavioral consequences associated with Prader-Willi syndrome. In previous studies, investigators reported SIB (most notably skin-picking) to be a prevalent behavioral problem for 69% of a sample of adolescents with Prader-Willi syndrome (Whitman & Accardo, 1987) and in 81% of a sample of adults with Prader-Willi syndrome (Thornton & Dawson, 1990).
The etiology and pathophysiological mechanisms of SIB are poorly understood. The primary pharmacological approaches for treating self-injury in persons with mental retardation and related developmental disabilities are aimed at the dopaminergic system (i.e., neuroleptics), the serotonergic system (i.e., 5-HTP precursors, serotonin reuptake inhibitors), or the endogenous opioid peptide system (i.e., opiate antagonists). Pharmacological treatments for SIB among persons with Prader-Willi syndrome have appeared promising but problematic because of methodological weaknesses. Hellings and Warnock (1994) reported positive responses to the SSRI fluoxetine for three people with Prader-Willi syndrome, two of whom presented with severe skin-picking. Benjamin and Buot-Smith (1993) evaluated a combination of fluoxetine and naltrexone for a 9-year-old boy with Prader-Willi syndrome and documented improvements in both weight control and skin-picking. All reported studies, however, were open label, single-case reports. The variability in response to pharmacological treatment for SIB in general and in Prader-Willi syndrome suggests an incomplete understanding of the mechanisms regulating self-injury. Our purpose in this study was to examine in more detail the SIB of persons with Prader-Willi syndrome by describing the specific forms and body locations of self-injury sites.
Method
Subjects and Settings
In collaboration with the Prader-Willi Syndrome Association and the newsletter Prader-Willi Perspectives, we conducted a self-injury survey by both mailing and distributing questionnaires to parents and guardians of children with Prader-Willi syndrome at regional, national, and international meetings. The questionnaires solicited information regarding individual medical and psychiatric histories, the social conditions associated with forms of self-injury, and a self-injury grid booklet (described later) to indicate where on the body their son or daughter self-injured. In total, 62 families from 20 states and one Canadian province completed questionnaires. Overall, 61% of the individuals with Prader-Willi syndrome were female and 39% were male. The mean age was 18 years (range = 3 to 44). Degree of mental retardation as reported by the parent or guardian ranged from mild to moderate. Twelve percent of respondents reported their child as having seizure activity, but only 1% were receiving medications specific for seizure disorders at the time of the survey. Sixty-one percent of the individuals with Prader-Willi syndrome were reported as having 15q11-q13 deletion, 18% as having maternal disomy 15, and 21% as unknown.
Self-injury grid general procedures
Parents and/or guardians were asked to indicate where on the body their son/daughter directed their self-injury. A self-injury grid booklet included an instructional cover sheet, examples of completed grids, and a series of figures of human body areas with overlapping grids forming squares covering the body’s surface. Respondents were instructed to shade in squares on the grids that corresponded to any known self-injury site. The grids consisted of 14 figures containing the outline of parts of the human body with a superimposed grid on each figure. Two diagrams were of the entire head (front & back), four were of the arms (front and back, left and right), two were of the palms of the hands (right and left), two were of the back of the hands (right and left), two were of the torso (front and back), and two were of the legs and feet (front and back). The body surface was divided into squares representing approximately 1.2 × 1.2 cm of the surface area of the trunk, torso, and arms; approximately 2.3 × 2.0 cm of surface area on the legs; approximately 1.5 × 1.5 cm of surface area on the head; and 0.55 × 0.55 cm surface area on the hands. Respondents were instructed to shade in the squares on the grid to indicate the exact body location where their son or daughter self-injured.
Self-injury comparison group
Between-group comparisons were made with a school-age sample of persons with mental retardation, autism, and related developmental disabilities. This sample consisted of 29 students receiving special education services who self-injured at least once per day (additional data for this sample are reported in Symons & Thompson, 1997). The majority of the sample were males (76%), who, on average, were 15 years old (range = 7 to 22) with severe or profound mental retardation (59%). Although teachers, not parents, completed the grid in the comparison group, the identical grid and instructions were used.
Results
Body site-specific data were reported for 62 persons with Prader-Willi syndrome. Of these, 12 persons were reported not to injure any sites (i.e., 50 of the 62 individuals with Prader-Willi syndrome injured at least one specific site). Overall, parents and guardians identified 869 self-injury body sites for 50 individuals with Prader-Willi syndrome and SIB described in this study. Eighty-one percent reported that their son or daughter had a history of some form of self-injury or current problems with self-injury. The most prevalent form of self-injury was skin-picking (82%), followed by nose-picking (28%). Other forms of self-injury reported included hand-biting (17%), head-banging (14%), hair-pulling (9%), and rectal-picking (6%). One individual was reported to engage in pica and was not included in subsequent analyses.
The location of self-injury body sites were described first according to their general distribution on the body and second in relation to results from a previous study of self-injury body sites among people with other forms of mental retardation. Self-injury body sites were distributed unevenly across the body’s surface area. The legs were the most prevalent body-site for self-injurious skin-picking, followed by the head and arms. Forty-four percent of all self-injury sites were located on the legs, 42% of all sites on the head, and 39% were located on the arms.
For leg-directed self-injury, 62% of sites were located on the front of the legs whereas 25% of sites were located on the back of the legs. Of the head-directed self-injury, 63% of sites were located on the front and 21% were located on the rear of the head. For arm-directed self-injury, 54% of sites were located on the front and 24% were located on the rear of the arms. Finally, for hand-directed self-injury, 56% of sites were located on the back of the hands with only 5% located on the palms.
In general, self-injury sites were disproportionately located on the legs, head, and arms of reported individuals with Prader-Willi syndrome. There were also notable areas toward which a high proportion of reported self-injury was localized to very specific body areas. These body areas included the nasal/oral area of the front of the head and the shin areas of the front of the legs. Specifically, of head-directed self-injury, 12% was located on the nose/mouth area and of the leg-directed self-injury, 22% was located on the shin area. Alternatively, of individuals who had head-directed SIB, 41% injured their nasal/oral areas. Similarly, of individuals who had leg-directed SIB, 67% injured their shin area.
Within-group analyses were conducted to examine the relation between age, gender, and the number of body sites self-injured. There was a significant correlation between age and the number of sites injured, r = .389, p = .002, medium effect, for the entire sample, N = 62. There was a significant correlation between age and the number of sites injured for the group of individuals with either uniparental disomy or deletion, r = .336, p = .019, medium effect, N = 49. For individuals with only deletions, there was a significant correlation between age and the number of sites injured, r = .336, p = .018, medium effect, N = 38. For individuals with uniparental disomy, there was no significant correlation between age and the number of sites injured, r = .246, p = .47, N = 11. There was no effect for gender on the number of sites injured. The mean number of sites injured by 24 males was 8.2 (standard deviation [SD]=7.6) = and by 37 females, 12.1 (SD = 1.8), p = .13. Information on IQ was available for less than half the sample, making it untenable to examine that variable.
Additional analyses were conducted to evaluate the possibility of Prader-Willi syndrome subtype differences in relation to self-injury. The total number of self-injury body sites was calculated for each person, and the distribution of that variable compared between genetic subtypes via a nonparametric procedure. There was a significant difference between the 15q11-q13 deletion and the maternal disomy group, Mann-Whitney U = 122.5, p < .05, suggesting that individuals with a 15q11-q13 deletion injure more sites than do those with maternal disomy.
We compared a number of demographic variables between the 50 persons with Prader-Willi syndrome who self-injured and the 12 who did not. Continuous variables were analyzed using Mann-Whitney U and t tests, and categorical variables were analyzed via Fisher’s Exact. There were no differences between the groups for age (Ms = 18.9 [SD = 9.5] vs. 14.4 [SD = 8.2]), t = −1.49, p = .14, for Prader-Willi syndrome with SIB versus no SIB, respectively) or for gender (Ms = 32 out of 50 [64%] females vs. 5 of 11 males [46%], Fisher’s Exact p =.32, for Prader-Willi syndrome with SIB vs. no SIB, respectively). We note that gender was not known for one person in the no-SIB group. Because IQ data were available for only 24 out of the 50 persons with Prader-Willi syndrome and SIB and 4 of the 12 persons with Prader-Willi syndrome and no SIB, we were unable to properly and validly evaluate differences.
Finally, comparisons were made with a previous sample of school-age children and adolescents with mental retardation and self-injury (cf. Symons & Thompson, 1997). Differences were evident in terms of both the forms and locations of SIBs. Among the school-age students with mental retardation, the most common forms of self-injury were biting, banging, and hitting, whereas pinching and picking were most common among individuals with Prader-Willi syndrome. Although the individuals with and without Prader-Willi syndrome and mental retardation appeared to injure comparable numbers of body sites overall, they injured very different sites. Comparisons of self-injury body sites were made between the two groups using a cutoff score of 15% or more (i.e., if 15% or more of individuals injured a given area it was considered a salient site for additional evaluation). Only 4 of 44 salient areas were common to both groups (3 areas on the back of the hands and the front of the left leg) (see Figure 1). The remaining distributions showed that individuals without Prader-Willi syndrome directed more self-injury toward their head than did the individuals with Prader-Willi syndrome, whereas the Prader-Willi syndrome sample’s SIB tended to be distributed widely across more body areas, including discrete finger, arm, and leg areas (see Table 1; bold entries represent those toward which 15% or more of individuals self-injured).
Figure 1.
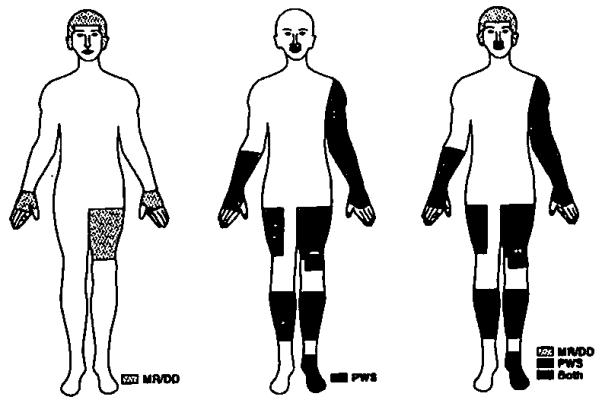
Distribution of self-injury sites overlapping between individuals with Prader-Willi syndrome and school-age children and adolescents with mental retardation with daily self-injury. Body sites towards which 15% or more of these individuals directed their self-injury are pictured. In total, only four areas overlapped between the two groups.
Table 1.
Individuals With and Without Prader-Willi Syndrome (in %) Injuring Specific Body Areas
| Body area/location | PWS | MR/DD |
|---|---|---|
| Head front | ||
| Lower nose/upper lip | 19.4 | 1.3 |
| Mouth | 12.9 | 6.9 |
| Chin | 12.9 | 0 |
| Middle of forehead | 11.2 | 24.1 |
| Forehead | 9.7 | 17.2 |
| Left side of forehead | 9.7 | 24.1 |
| Right cheek | 8.1 | 6.9 |
| Right eye | 6.5 | 6.9 |
| Right ear | 6.5 | 17.2 |
| Left cheek | 6.5 | 3.4 |
| Right side of forehead | 4.8 | 31.0 |
| Left eye | 4.8 | 6.9 |
| Left temple | 4.8 | 17.2 |
| Right temple | 3.2 | 17.2 |
| Nose | 3.2 | 0 |
| Left ear | 1.6 | 17.2 |
| Head back | ||
| Back of head | 12.9 | 17.2 |
| Top of head-balance | 8.1 | 6.9 |
| Top of head | 6.5 | 3.4 |
| Back of neck | 3.2 | 6.9 |
| Back of left ear | 1.6 | 6.9 |
| Back of right ear | 1.6 | 6.9 |
| Arms front | ||
| Left front wrist area/lower middle arm | 22.6 | 3.4 |
| Right front wrist area/lower middle arm | 21.1 | 6.9 |
| Right middle arm front-balance | 17.7 | 3.4 |
| Left upper arm front | 16.1 | 0 |
| Left hand front | 16.1 | 0 |
| Right middle of arm front | 14.5 | 6.9 |
| Left middle arm front-balance | 14.5 | 0 |
| Right upper arm front | 12.9 | 0 |
| Right tips of fingers front | 12.9 | 0 |
| Left tips of fingers front | 12.9 | 0 |
| Right hand front | 11.3 | 10.3 |
| Left middle center of arm front | 6.5 | 0 |
| Left middle of outer arm front | 6.5 | 0 |
| Right inner middle arm front | 3.2 | 0 |
| Arms back | ||
| Right middle arm rear | 17.7 | 6.9 |
| Left middle of arm rear | 14.5 | 6.9 |
| Right wrist rear | 8.1 | 6.9 |
| Right hand rear | 8.1 | 3.4 |
| Left wrist rear | 6.5 | 3.4 |
| Left hand rear | 6.5 | 3.4 |
| Left upper/shoulder arm rear | 4.8 | 0 |
| Left upper arm rear | 3.2 | 0 |
| Right upper arm rear | 3.2 | 0 |
| Right upper/shoulder arm rear | 3.2 | 0 |
| Hands front | ||
| Right palm | 3.2 | 24.1 |
| Left palm | 3.2 | 6.9 |
| Left pointer palm | 1.6 | 3.4 |
| Right thumb palm | 0 | 1.3 |
| Right pointer palm | 0 | 20.1 |
| Right index palm | 0 | 3.4 |
| Right small finger palm | 0 | 1.3 |
| Left thumb palm | 0 | 6.9 |
| Left upper thumb palm | 0 | 6.9 |
| Left middle thumb palm | 0 | 6.9 |
| Left upper pointer palm | 0 | 10.3 |
| Left middle pointer palm | 0 | 3.4 |
| Left small finger palm | 0 | 3.4 |
| Hands back | ||
| Right back pointer nail area | 24.2 | 6.9 |
| Left back index area | 22.6 | 3.4 |
| Right back thumb nail area | 21.1 | 3.4 |
| Right back index nail area | 21.1 | 0 |
| Right back ring nail area | 21.1 | 3.4 |
| Left back thumb nail area | 21.1 | 0 |
| Left back ring nail area | 21.1 | 0 |
| Left back small finger nail area | 21.1 | 3.4 |
| Right back small finger nail area | 19.4 | 3.4 |
| Left back pointer nail area | 19.4 | 3.4 |
| Right middle back of hand | 16.1 | 37.9 |
| Left back of hand-balance | 14.5 | 17.2 |
| Left middle back of hand | 14.5 | 24.1 |
| Right back of hand-balance | 12.9 | 34.5 |
| Right index back | 8.1 | 0 |
| Left back of pointer finger–balance | 8.1 | 17.2 |
| Left thumb back | 6.5 | 20.7 |
| Left index back | 6.5 | 0 |
| Right pointer back | 4.8 | 6.9 |
| Right back middle of index | 3.2 | 10.3 |
| Left ring back | 3.2 | 0 |
| Right thumb back | 1.6 | 6.9 |
| Right back of upper thumb | 0 | 48.3 |
| Right back upper part of pointer | 0 | 10.3 |
| Right back of middle pointer | 0 | 17.2 |
| Right small finger back | 0 | 3.4 |
| Torso front | ||
| Upper torso front | 11.3 | 0 |
| Upper middle/chest torso front | 8.1 | 0 |
| Lower torso front | 4.8 | 0 |
| Torso back | ||
| Upper torso back | 11.3 | 0 |
| Upper torso right shoulder back | 6.5 | 0 |
| Lower torso back | 6.5 | 0 |
| Upper torso left shoulder back | 4.8 | 0 |
| Legs front | ||
| Right shin front | 32.3 | 3.4 |
| Right upper middle leg front | 14.5 | 6.9 |
| Left middle leg front | 14.5 | 17.2 |
| Left center knee front | 14.5 | 0 |
| Left shin front | 14.5 | 0 |
| Left foot front | 14.5 | 0 |
| Right foot front | 12.9 | 0 |
| Left shin front-balance | 12.9 | 0 |
| Right shin front-balance | 11.3 | 0 |
| Right lower outer shin front | 9.7 | 0 |
| Pelvis front | 8.1 | 6.9 |
| Right middle leg front | 4.8 | 10.3 |
| Left inner knee front | 4.8 | 0 |
| Right inner knee front | 3.2 | 0 |
| Right center knee front | 3.2 | 0 |
| Right middle leg front-balance | 1.6 | 13.8 |
| Right lower middle leg front | 1.6 | 0 |
| Legs back | ||
| Left calf back | 12.9 | 0 |
| Right calf back | 12.9 | 0 |
| Gluteus maximus back | 4.8 | 0 |
| Left middle leg back | 3.2 | 3.4 |
| Right middle leg back | 3.2 | 0 |
| Left foot back | 1.6 | 0 |
| Right foot back | 1.6 | 0 |
Note. PWS = Prader-Willi syndrome, MR/DD = mental retardation/developmental disabilities. Bold face indicates those areas toward which 15% or more of individuals self-injured.
Discussion
This study was designed to describe in more detail the specific forms and body locations of SIB by people with Prader-Willi syndrome. In total, over 800 self-injury body sites were reported. Skin-picking was the most common form of self-injury and the legs and head were the most likely body locations. Males and females were equally likely to self-injure. Older individuals were more likely to injure more areas of their body. Finally, individuals with paternal deletions were more likely to self-injure than individuals with maternal disomy.
In a previous study describing self-injury body locations among a sample of school-age children with mental retardation and related developmental disabilities of unknown or heterogeneous etiologies, Symons and Thompson (1997) reported an uneven distribution of self-injury body locations. In that sample, however, the majority of SIB sites were located on the front of the head and specific areas on the back of the hands. Using independent teacher reports to describe the distribution of self-injury body sites, a total of 115 self-injury sites were identified, with approximately 80% of the sites located on a very small percentage of the body’s surface (primarily the head, hands, and wrists, although other areas such as the upper arms, chest, abdomen, and thighs were presumably equally accessible but were rarely targeted as SIB sites). Of these 115 self-injury sites, 56% were located on the hands and 25% were located on the head. Moreover, the most frequent forms of self-injury were head-hitting, head-banging, and self-biting.
In contrast, the sample of people with Prader-Willi syndrome directed the majority of their self-injury toward the legs followed by the head. The most common self-injury form was skin-picking and nose-picking, with hand-biting and head-banging reported for only a small percentage of respondents. Although the group comparisons were conducted post hoc and were not a priori matched, the differences in SIB between the two groups are noteworthy. The two groups did not differ in the overall amount of self-injury, but they did differ clearly on the form (banging/hitting/biting versus picking for Prader-Willi syndrome) and overall distribution of self-injury sites (primarily head/hands versus legs, head, and a wide distribution on the body for individuals with Prader-Willi syndrome). Given that our comparison sample consisted of more individuals with severe or profound intellectual impairments than did our Prader-Willi syndrome sample, an explanation for this finding might be that severity of intellectual impairment could account for the differences in SIB form and distribution. Additional research designed accordingly is needed to resolve that possibility. One final point worth considering concerns skin-picking location and the issue of visibility. Thus, some individuals may pick areas of the body that are not easily or clearly visible, whereas our self-injury grid method may be more sensitive to readily visible body areas. This possibility deserves further attention in future studies among individuals with skin-picking problems in Prader-Willi syndrome and other disabilities.
Several limitations of this study should be noted. Because we conducted a survey covering numerous states and one province, we were unable to measure directly the reliability of the reported SIB body locations. In the previous study, relying on teacher- collected self-injury grid data, Symons and Thompson (1997) reported 80% agreement of the self-injury locations between trained independent observers and teaching staff. Although it is impossible to know for certain, it seems unlikely the self-injury locations were Significantly misrepresented or inaccurately reported by caregivers in this study. These are the persons most familiar with the individuals with Prader-Willi syndrome and their history of SIB. Because of the design of the survey, it was impossible to know the extent to which the parents/guardians were emphasizing current forms and body locations of self-injury as opposed to forms and locations of past self-injury. In addition, because of the mixed methodology (mail outs and distribution at conferences), we were not able to establish exact response rates nor identify sampling biases; therefore, caution is appropriate when considering how representative this sample may be of individuals with Prader-Willi syndrome and their families. Finally, although there is no reason to doubt that each individual had Prader-Willi syndrome, we did not verify the reliability of parental/guardian reports of the specific genetic status. In a recent comparison of phenotypes between deletion and maternal disomy cases, however, Cassidy et al. (1997) reported that those individuals with maternal disomy were less likely to exhibit skin-picking behaviors when compared with individuals with deletion 15q11-q13. Individuals were subtyped using molecular techniques. Our results, which were based on parental report of genetic status, also indicate that individuals with maternal disomy are less likely to self-injure (i.e., the deletion group injured more body sites than did the disomy group).
These findings may have implications for future treatment studies of self-injurious skin-picking. In pharmacological treatment reports for other forms of SIB, investigators have noted form-dependent responses. Specifically, response to naltrexone hydrochloride varies as a function of self-injury form or body location (Herman et al., 1987; Symons, Fox, & Thompson, 1998; Thompson, Hackenberg, Cerutti, Baker, & Axtell, 1994). Herman et al. found that individuals whose self-injury was head- and face-directed responded positively to naltrexone but those exhibiting self-biting did not. Thompson et al. noted that both head-banging and intense self-biting were reliably reduced by naltrexone treatment, but other forms and body locations were unaffected (scratching, thrusting fingers in the nose). Skin-picking by people with Prader-Willi syndrome is not a likely candidate for naltrexone treatment because the self-injury forms and body site distribution overlaps minimally with that of individuals with mental retardation and autism who are known to be naltrexone responders (e.g., Sandman, Hetrick, Taylor, & Chicz-DeMet, 1997; Thompson et al., 1994). The fact that people with Prader-Willi syndrome have many features in common with people who have obsessive compulsive disorder (Dykens, Leckman, & Cassidy, 1996; Roof et al., 1998) suggests that skin-picking may be more appropriately viewed as a component of compulsive behavior and may be responsive to medications specifically effective in treating such conditions (e.g., selective serotonin reuptake inhibitors).
Finally, two points can be made in relation to issues of syndrome-specific behavioral phenotypes (Dykens, 1995). First, it appears that relative to a sample of individuals with mental retardation and self-injury but without Prader-Willi syndrome, persons with Prader-Willi syndrome are more likely to skin pick. Second, persons with maternal disomy appear to be less likely to manifest self-injury (cf. Cassidy et al., 1997). Studies designed to further analyze between-group differences in genetic subtypes of Prader-Willi syndrome may shed light on different mechanisms regulating skin-picking with implications for differential diagnosis and treatment.
Acknowledgments
Support for this research was provided, in part, by Public Health Service (PHS) Grant No. HD30329 from the National Institute of Child Health and Human Development (NICHD) to Vanderbilt University and PHS Grant No. HD35682 from NICHD to University of North Carolina at Chapel Hill. We gratefully acknowledge the anonymous reviewers for their insight on a number of important issues. Requests for reprints can be sent to Frank Symons, FPG Child Development Center, UNC at Chapel Hill, CD# 8180 105 Smith Level Rd., Chapel Hill, NC 27599.
Contributor Information
F. J. Symons, University of North Carolina at Chapel Hill
M. G. Butler, Children’s Mercy Hospital (Kansas City, Missouri)
M. D. Sanders, Vanderbilt University
I. D. Feurer, Vanderbilt University
T. Thompson, Vanderbilt University
References
- Benjamin E, Buot-Smith T. Naltrexone and fluoxetine in Prader-Wil1i syndrome. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:870–873. doi: 10.1097/00004583-199307000-00025. [DOI] [PubMed] [Google Scholar]
- Bhargava SA, Putnam PE, Kocoshis SA, Rowe M, Hanchett JM. Rectal bleeding in Prader-Willi syndrome. Pediatrics. 1996;97:265–267. [PubMed] [Google Scholar]
- Butler MG, Levine GJ, Le JY, Hall BD, Cassidy SB. Photoanthropometric study of craniofacial traits of individuals with Prader-Willi syndrome. American Journal of Medical Genetics. 1995;58:38–45. doi: 10.1002/ajmg.1320580109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Meaney FJ, Palmer CG. Clinical and cytogenetic survey of 39 individuals with Prader-Labhart-Willi syndrome. American Journal of Medical Genetics. 1986;23:793–809. doi: 10.1002/ajmg.1320230307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy SB. Prader-Willi syndrome. Journal of Medical Genetics. 1997;34:917–923. doi: 10.1136/jmg.34.11.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy SB, Forsythe M, Heeger S, Nicholls RD, Schork N, Benn P, Schwartz S. Comparison of phenotype between patients with Prader-Willi syndrome due to deletion 15q and uniparental disomy 15. American Journal of Medical Genetics. 1997;68:433–444. [PubMed] [Google Scholar]
- Dykens EM. Measuring behavioral phenotypes: Provocations from the “new genetics.”. American Journal on Mental Retardation. 1995;99:522–532. [PubMed] [Google Scholar]
- Dykens EM, Cassidy SB. Prader-Willi syndrome: Genetic, behavioral, and treatment issues. Child and Adolescent Psychiatric Clinics of North America. 1996;5:913–927. [Google Scholar]
- Dykens EM, Hodapp RM, Walsh K, Nash LJ. Adaptive and maladaptive behavior in Prader-Willi syndrome. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:1131–1136. doi: 10.1097/00004583-199211000-00023. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Leckman JF, Cassidy SB. Obsessions and compulsions in Prader-Willi syndrome. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1996;37:995–1002. doi: 10.1111/j.1469-7610.1996.tb01496.x. [DOI] [PubMed] [Google Scholar]
- Hellings JA, Warnock JK. Self-injurious behavior and serotonin in Prader-Willi syndrome. Psychopharmacology Bulletin. 1994;30:245–325. [PubMed] [Google Scholar]
- Herman B,H, Hammock MK, Arthur-Smith A, Egan J, Chatoor I, Werner A, Zelnick N. Naltrexone decreases self-injurious behavior. Annals of Neurology. 1987;22:550–552. doi: 10.1002/ana.410220419. [DOI] [PubMed] [Google Scholar]
- Prader A, Labhart A, Willi H. En syndrom von adipositas, kieinwuchs, kryptorchismus und oligophrenic nach myato-mieartigem zustand in neugeborenalte. Schweizerische Medizinische Wochenschrift. 1956;86:1260–1261. [Google Scholar]
- Roof E, Stone W, Maclean W, Feurer ID, Thompson T, Butler MG. IQ and adaptive behavior differences in genetic subtypes of Prader-Willi syndrome. 1999 Manuscript submitted for publication. [Google Scholar]
- Sandman CA, Hetrick W, Taylor DV, Chicz-DeMet A. Dissociation of POMC peptides after self-injury predicts responses to centrally acting opiate blockers. American Journal on Mental Retardation. 1997;102:182–199. doi: 10.1352/0895-8017(1997)102<0182:DOPPAS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Symons FJ, Fox ND, Thompson T. Functional communication training and naltrexone treatment of self-injurious behavior: An experimental case report. Journal of Applied Research in Intellectual Disabilities. 1998;11:273–292. [Google Scholar]
- Symons FJ, Thompson T. Self-injurious behavior and body site preference. Journal of Intellectual Disability Research. 1997;41:456–468. doi: 10.1111/j.1365-2788.1997.tb00737.x. [DOI] [PubMed] [Google Scholar]
- Thompson T, Gray DB, editors. Destructive behavior in developmental disabilities: Diagnosis and treatment. Sage; Thousand Oaks, CA: 1994. [Google Scholar]
- Thompson T, Hackenberg T, Cerutti D, Baker D, Axtell S. Opioid antagonist effects on self-injury in adults with mental retardation: Response form and location as determinants of medication effects. American Journal on Mental Retardation. 1994;99:85–102. [PubMed] [Google Scholar]
- Thornton L, Dawson KP. Prader-Willi syndrome in New Zealand: A survey of 36 affected people. New Zealand Medical Journal. 1990;103:97–98. [PubMed] [Google Scholar]
- Whitman BY, Accardo P. Emotional symptoms in Prader-Willi syndrome adolescents. American Journal of Medical Genetics. 1987;28:897–905. doi: 10.1002/ajmg.1320280415. [DOI] [PubMed] [Google Scholar]


