Abstract
Background Displacement of distal radius fractures has been previously described in the literature; however, little is known about fracture displacement following splint or cast removal at the initial clinic visit following reduction and immobilization.
Purpose The purpose of this study was to evaluate risk factors for fracture displacement following splint or cast removal and physical examination in the acute postinjury period.
Methods All patients with a closed distal radius fracture who presented to our orthopedic hand clinic within 3 weeks of injury were prospectively enrolled in our study. Standard wrist radiographs were obtained prior to splint or cast removal. A second wrist series was obtained following physical exam and application of immobilization at the end of the clinic visit. Radiographic parameters for displacement were measured by two independent reviewers and included dorsal angulation, radial inclination, articular step-off, radial height, and ulnar variance. Displacement was assessed using predefined, radiographic criteria for displacement.
Results A total of 64 consecutive patients were enrolled over a period of 12 weeks. Of these, 37.5% were classified as operative according to American Academy of Orthopaedic Surgeons guidelines and 37.5% met LaFontaine instability criteria. For each fracture, none of the five measurements exceeded the predefined clinically or statistically significant criteria for displacement.
Conclusion Splint removal in the acute postinjury period did not result in distal radius fracture displacement. Clinicians should feel comfortable removing splints and examining underlying soft tissue in the acute setting for patients with distal radius fractures after closed reduction.
Level of Evidence Level II, prospective comparative study
Keywords: displacement, distal radius, fracture, management
Distal radius fractures account for 20% of all fractures seen in the emergency room, representing 3% of upper extremity injuries.1 2 Fracture incidence displays a bimodal age distribution as a result of high-energy trauma in younger patients and low-energy falls in the elderly.3 American Academy of Orthopaedic Surgeons (AAOS) guidelines recommend operative fixation for fractures that have any of the following factors on their postreduction radiograph: dorsal angulation >10 degrees, radial shortening > 3 mm, or intra-articular displacement > 2 mm.4 However, the majority of distal radius fractures are managed nonoperatively with closed reduction and cast immobilization.3
Several studies have evaluated variables associated with fracture stability, as fractures may re-displace (secondary displacement) after initial reduction.2 5 6 7 8 While risk factors for secondary displacement have been identified, there is no consensus on which of these factors are significant.2 5 7 9 10 While prior studies have evaluated secondary displacement following closed reduction, none have evaluated acute fracture displacement following temporary removal of immobilization during clinical examination at the initial clinic visit. This is important, as some surgeons may forgo discontinuation of immobilization at the initial clinic visit to avoid secondary displacement.
The purpose of this prospective study was to determine if distal radius fractures treated nonoperatively would significantly displace after splint or cast removal and physical examination within the first 3 weeks of injury. In addition, we sought to identify specific risk factors for secondary displacement after splint discontinuation and examination in the clinical setting. Assessing fracture stability in the acute postinjury period may guide treatment principles and improve our ability to better manage patients with distal radius fractures.
Methods
After obtaining institutional review board approval, closed fractures of the distal aspect of the radius (AO/OTA 23-A2 through 23-C3) that presented to our orthopedic hand clinic within 3 weeks of injury were prospectively enrolled. Patients were excluded if they refused to participate in the study, sustained any concomitant injuries to the ipsilateral upper extremity (metacarpal, ulna, proximal radius, humerus, etc.), sustained the injury greater than 3 weeks prior presentation to clinic, or underwent previous open reduction and internal fixation of the fracture. Our exclusion of fractures presenting greater than 3 weeks after injury was based on prior studies examining secondary displacement.2 11
Prior to the clinic visit, all patients were first evaluated in the emergency department by our orthopedic staff, and were placed in either a sugar-tong splint or short-arm cast with or without closed reduction. Standard posterior-anterior, lateral, and oblique wrist radiographs were obtained in clinic prior to removal of the splint or cast. The cast or splint was then removed at the initial clinic visit and a standard hand and soft tissue exam was performed by a physician. The physical exam consisted of a skin exam, palpating for tenderness, and concluded with a neurovascular exam. Range of motion and strength were not assessed at the clinic visit, since the fractures were in the acute period. Elbow and shoulder range of motion were also assessed, but not recorded as this was not the focus of our study. Each physical examination was conducted by at least one orthopedic surgeon. As our institution is a teaching hospital, residents and fellows were involved in the care of these patients. However, any physical examination conducted by a resident was confirmed by a board-certified orthopedic surgeon. Following examination, a short-arm cast or a custom thermoplastic splint was reapplied and radiographs were repeated. Pre- and post-examination radiographs were then compared with evaluate for fracture displacement.
Radiographic parameters were measured by two independent orthopedic surgeons and included the following variables: ulnar variance, volar tilt, intra-articular displacement, radial height, radial shortening, presence or absence of dorsal comminution, and concomitant ulnar styloid fracture.6 Volar tilt was measured on a lateral radiograph and was defined as the angle between a line perpendicular to the long axis of the radius and a second line passing through the dorsal and volar lips of the distal radius.7 Intra-articular displacement was defined as the greatest vertical distance between the two sides of an intra-articular fracture. Radial height was defined as the vertical difference between two lines drawn perpendicular to the radial shaft: one along the lunate facet and the second along the radial styloid tip. Ulnar variance was measured as the axial distance from the lunate facet of the radius to the carpal articular surface of the ulna styloid.
Measurement disparity between reviewers was defined as 2 degrees of dorsal angulation, 0.5 mm ulnar variance, or 0.5 mm radial height. Radiographic measurements were repeated if reviewer measurements differed by greater than these prespecified values. If any disparities persisted after repeat measurements, the two reviewers analyzed the images together and a consensus measurement was made between the two reviewers. LaFontaine criteria was used to evaluate fracture stability, where if three or more of the following criteria were met, the fracture pattern was considered to be unstable: dorsal angulation greater than 20 degrees, intra-articular comminution, radial shortening greater than 5 mm, age greater than 65 years, or concomitant ulnar styloid fracture. Demographic data was obtained, including age, gender, hand dominance, medical history, smoking history, and method of immobilization. Fractures were classified according to the AO/OTA fracture classification for distal radius fractures, which considers severity of fracture, extent of intra-articular involvement, and metaphyseal comminution.4 12 Postreduction radiographs were also evaluated to determine which patients met AAOS guideline recommendations for open reduction and internal fixation: dorsal angulation > 10 degrees, radial shortening > 3 mm, or intra-articular displacement > 2 mm.4
Clinically meaningful displacement was defined as: 5 degrees of dorsal angulation, 1 mm ulnar variance, 3 degrees radial inclination, and 2 mm radial shortening. These values were determined from prior studies.7 9 10 11 If the difference between pre- and post-splint removal and examination radiographs were greater than the predefined cutoffs, the fracture was considered to have displaced. Measurements were also assessed for statistically significant differences using a Wilcoxon signed-rank test. Using G*Power Statistical Analysis Software, an a priori power analysis with 80% power to detect a moderate effect size (0.4) between pre and postreduction radiographs (30% difference between two radiographs) required a minimum sample size of 54 patients.
Results
Sixty-five patients were recruited who met inclusion criteria between October 2014 and February 2015. One patient was excluded for a concomitant ulnar shaft fracture, resulting in 64 patients in the final analysis. The average age of the cohort was 48 years (range, 19–90) with 38 males (59%) and 26 females (41%). The mean time from initial injury to clinic evaluation was 12.5 days (range, 4–21 days), and 95% of fractures underwent closed reduction in our emergency department. Based on LaFontaine criteria, 37.5% of fractures met instability criteria (Table 1). In our cohort, 37.5% of fractures met AAOS criteria for operative fixation. AO/OTA type C fractures represented one-third of all included fractures (Fig. 1).
Table 1. Study population characteristics.
| Age (mean ± SD, range) | 47.95 ± 17.89 (19–90) y |
| Gender | 58.5% male, 41.5% female |
| Hand dominance | 86.1% right, 10.8% left, 3.1% unknown |
| Time from injury to exam | 12.5 ± 3.9 (4–21) d |
| Fracture stability based on LaFontaine criteria | 37.5% unstable |
| Meet AAOS guidelines for operative management | 37.5% |
| Percent closed reduction in the emergency department | 95.4% |
| Percent intra-articular extension | 58% |
| Percent concomitant ulnar-styloid fracture | 48% |
| Percent dorsal comminution | 50% |
| Percent shortening > 5 mm | 41% |
Abbreviations: AAOS, American Academy of Orthopedic Surgeons; SD, standard deviation.
Fig. 1.
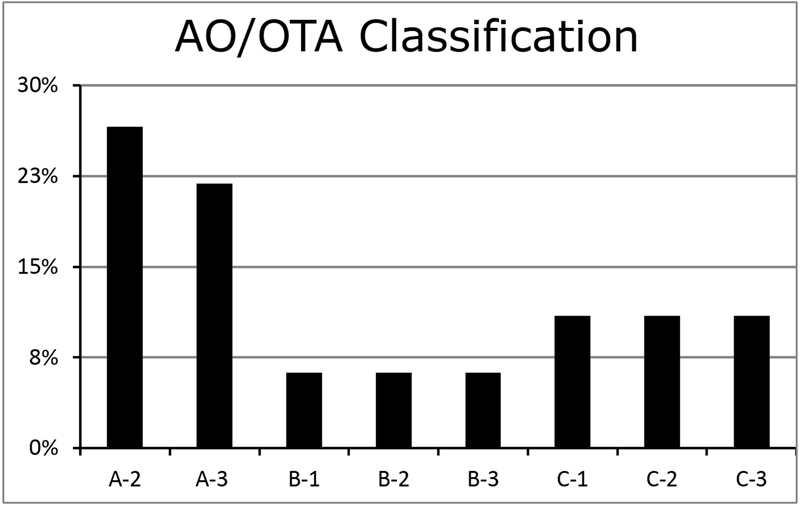
Distribution of fracture patterns among participants.
The mean palmar tilt, ulnar variance, and radial inclination of the fractures at initial evaluation in the emergency department were −8.5 ± 16.4 degrees, −2.2 ± 2.8 mm, and 20.4 ± 8.3 degrees, respectively (Fig. 2). The mean palmar tilt, ulnar variance, and radial inclination after splint application in the emergency department were −0.8 ± 7.3 degrees, 0.2 ± 1.9 mm, and 19.5 ± 5.9 degrees, respectively. The mean palmar tilt, ulnar variance, and radial inclination at time of splint removal in the clinic were 0.3 ± 10.1 degrees, −1.2 ± 2.0 mm, and 21.7 ± 7.6 degrees, respectively.
Fig. 2.
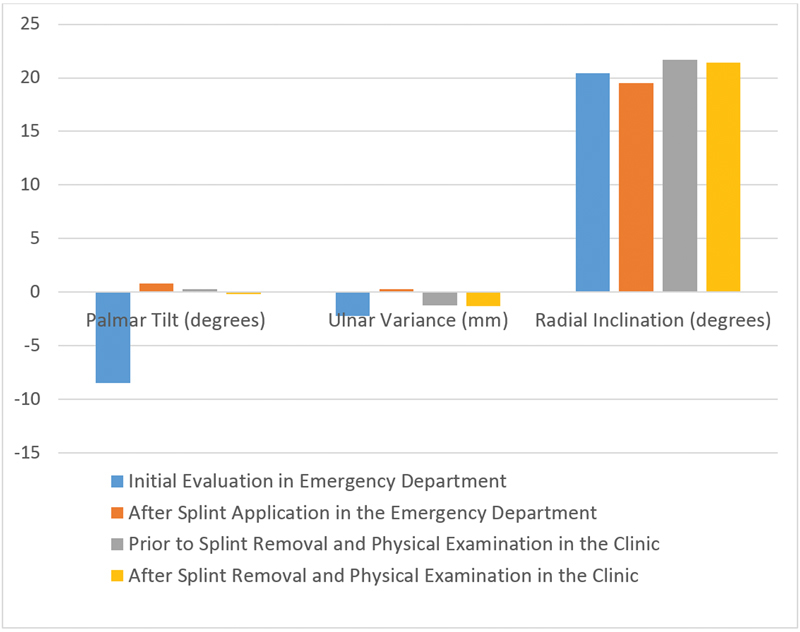
Mean values of radiographic parameters.
The mean change in dorsal angulation, ulnar variance, articular step-off, and radial height between initial and post-visit radiographs was −0.2 degrees (standard deviation [SD], 1.74; range, −5–3; p = 0.53), −0.01 mm (SD,0.24; range, −1–0.6; p = 0.29), −0.01 mm (SD, 0.07; range, −0.5–0.2; p = 0.963), and −0.11 mm (SD, 0.28; range, −0.9–1; p = 0.85), respectively. Across all patients, none of the five radiographic measurements exceeded the predefined clinically significant criteria for displacement after splint removal (Fig. 3A, B). In addition, there were no statistically significant changes in dorsal angulation, ulnar variance, articular step-off, or radial height. Lastly, there was no association between fracture displacement and demographic variables, AO/OTA fracture type, fracture instability criteria, patient age, or injury-to-clinic interval.
Fig. 3.
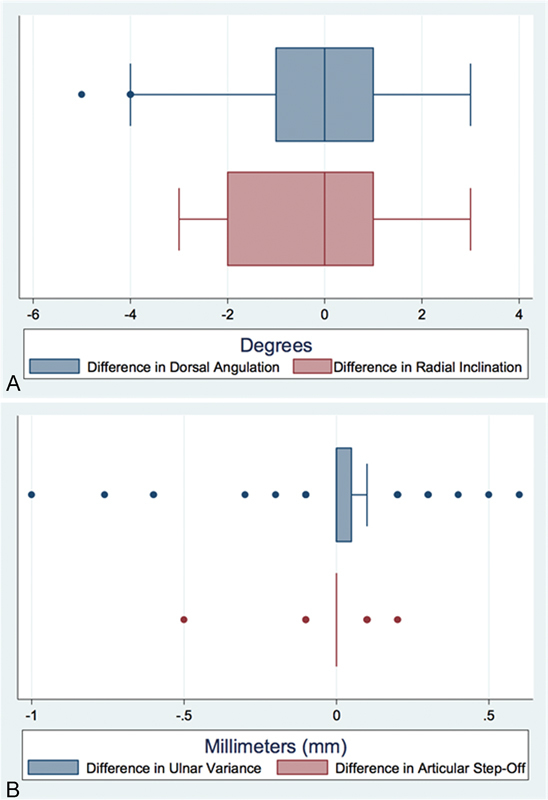
(A) Boxplot of difference in dorsal angulation and radial inclination; (B) Boxplot of difference in ulnar variance and articular step-off.
Discussion
Management of postreduction immobilization of distal radius fractures is variable and largely physician-dependent. Some surgeons may elect to continue the initial mode of immobilization at the first clinic visit to avoid displacing a well-reduced or potentially unstable fracture. However, splint immobilization is not without risk as soft tissue injury is still possible. Others elect to temporarily remove postreduction immobilization to permit physical examination of the affected extremity and transition to a short-arm cast. While prior studies have examined displacement over the course of weeks, ours is the first study to examine fracture stability with splint removal in the clinic.
The results of this study support safe removal of initial immobilization at the first clinic follow-up visit as no fracture showed evidence of clinically or statistically significant displacement following clinical examination and reapplication of a short-arm cast. This included those patients with unstable fracture patterns, advanced age, and short injury-to-clinic intervals. After classifying the fracture patterns using the AO/OTA system, our cohort had a wide distribution of fracture types. This included 37.5% of fractures that meet AAOS criteria for operative stabilization.12 Further, 37.5% of the patients met LaFontaine criteria for instability. Based on available data, these patients would be at greatest risk of secondary displacement in the acute postinjury period. However, none of these patients showed evidence of fracture displacement following splint removal and clinical examination. In addition, patient age, fracture pattern, and injury-to-clinic visit interval were not identified as risk factors for secondary displacement.
There are two important implications of this study with relation to the currently available literature. First, previous reports on unstable distal radius fractures, as defined by LaFontaine et al, showed a high rate of secondary displacement in the first 4 weeks postinjury.5 Given that none of the unstable fracture patterns in the current study displaced, secondary displacement likely results from prolonged muscular deformation and gradual reduction in soft tissue edema, resulting in overly capacious splints. It is unlikely that short periods without immobilization result in fracture displacement, as evidenced by this study. Second, injury-to-clinic interval was not a risk factor for displacement. One potential explanation for this finding is that organized fracture hematoma, in addition to soft tissue and osseous stabilizing structures, helps maintain fracture stability. Fracture hematoma likely provides some stabilization in the first weeks after injury that prevents displacement even among unstable patterns in elderly patients.
Removal of immobilization in the initial clinic evaluation has advantages. For one, since fracture blisters often form within the 24 to 48 hour time interval, patients who present for initial evaluation in the emergency department before this time period may later develop significant soft tissue compromise that was not noted at initial presentation.13 This also includes soft tissue compromise from poorly molded or padded splints/casts, loosening of splints/casts as soft tissue swelling resolves, and evaluation of potentially open injuries that may have been missed or developed after fracture reduction. Thus, splint removal and examination may result in important changes in treatment. In addition, Halanski et al recommend periodic inspection of the underlying skin in ‘high-risk’ patients, including patients who are very young, developmentally delayed, spastic, or have sensory impairments in the affected extremity.14 Early evaluation of this at-risk group of patients may assist in preventing future morbidity. In the present study, a total of 10/65 (15%) of our patients met this definition, with 7/65 (10%) diabetics and 3/65 (5%) with some form of mental impairment. For this reason, we are underpowered to give specific conclusions regarding this at-risk group. Despite this, our institution elects to evaluate patients in the first clinic visit with the splint removed, and then transition to a short-arm cast or thermoplastic splint based on the condition of underlying soft tissue, general range of motion of hand, and patient comfort. The results of this study show that our immobilization algorithm provides the aforementioned benefits without associated risk. Even if a surgeon doesn't elect to remove all splints at the initial clinic visit, he should feel comfortable removing a splint without fear of displacement in patients whom he believes need an exam.
Prior studies have also identified the incidence of displacement following closed reduction. Bong et al found a 38.9% displacement rate following closed reduction with either a sugar tong or radial gutter splint at 1-week follow-up.11 Nesbitt et al found that 54% of their cohort had a loss of reduction at 4 weeks, with 63% of these patients losing reduction in the first week.2 Kumar et al found a statistically significant loss of alignment at 1 week postmanipulation, with no significant changes after this time point.15 Thus, while distal radius fractures are at risk of displacement following initial reduction, our results show that these fractures are stable over short periods without immobilization. This is likely because fracture hematoma, bony apposition, and soft tissue constraints act to resist deforming forces for a short time period.16 In addition, while not apparent radiographically, chondrogenesis in the first 7 to 10 days of fracture healing also contributes to fracture stability.17
While inconsistent in the literature, prior studies have identified risk factors for secondary displacement in distal radius fractures. Age has been shown to be associated with loss of reduction.2 5 6 9 18 Makhni et al found that, when sub-analyzing only patients who underwent closed reduction, increasing age became a larger risk factor for secondary displacement.9 Our study did not find increasing age as a risk factor for displacement, despite 95% of our cohort receiving a closed reduction at presentation. The degree of initial displacement at injury presentation is predictive of secondary displacement, with severe fracture displacement being correlated with worse long-term outcomes.6 7 8 19 Conversely, Farah et al did not find the degree of initial displacement to be a risk factor for secondary displacement.10 This study did not identify the degree of initial displacement at injury presentation to be a risk factor for secondary displacement during temporary discontinuation of immobilization.
Several studies have examined radiographic parameters as predictors of instability. Initially, Jenkins found radial shortening and a loss of radial height to be predictive of fracture redisplacement.20 Meanwhile, LaFontaine et al found that dorsal angulation, intra-articular comminution, and radial shortening were predictors of fracture instability.5 Mackenney et al agreed that radial shortening was a risk factor for instability, but did not find dorsal angulation to be a risk factor.6 In addition, ulnar variance was predictive of secondary displacement. Nesbitt et al found that dorsal comminution was predictive of displacement, but intra-articular fractures and dorsal angulation were not risk factors.2 Makhni et al found a statistically nonsignificant increase in secondary displacement among severely comminuted fractures.9 Tahririan et al found that loss of radial height and inclination were predictive of instability, with dorsal comminution and intra-articular fractures not predictive of displacement.18 We found that dorsal angulation, ulnar variance, radial inclination, radial height, and intra-articular fractures were not predictive of displacement following temporary removal of immobilization. Lastly, a concurrent ulna fracture may be a risk factor for instability and secondary displacement; however, ulnar styloid fractures were not a risk factor in our cohort.2 5 8 18
This study has several weaknesses. First, radiographic measurements often have poor interobserver reliability.21 To account for this, we used predetermined cut-offs for discrepancy that were chosen to account for expected variation. Using these cut-offs, only four patients required repeated measurements for unacceptable variance, and following independent remeasurement these discrepancies were within acceptable limits. In addition, there are no guidelines for acceptable cut-offs for clinically meaningful displacement of distal radius fractures, as measured using radiographic parameters. Because of this, the authors of this study defined these criteria by consensus, using previously reported values in the literature as reference.7 9 10 11 Although the injury to exam interval was deliberately chosen based on previous literature, utilizing a shorter interval may have selected for fractures more likely to displace.2 11 Lastly, our study is only sufficiently powered to provide conclusions regarding patients who presented to their initial clinic visit with a sugar tong splint. A future study investigating patients who present to their initial clinic visit with cast immobilization may prove interesting.
The primary strength of this study is our cohort represents the population of a large level I trauma center, with a heterogeneous distribution of fracture types. In addition, this cohort was prospectively enrolled, and included all patients who met criteria during the enrollment period. As our institution is a teaching hospital, several different physicians participated in the emergency department and clinic visit evaluations; this surgeon heterogeneity improves the validity of our results. Lastly, the stability of distal radius fractures following splint removal at the initial clinic visit has previously been unreported.
In conclusion, it is safe to remove postreduction immobilization for clinical evaluation and cast or splint application in the acute postinjury period following distal radius fracture irrespective of radiographic instability, injury-to-clinic visit interval, and patient age.
Ethical Review Committee Statement
This study was approved by our institutional review board.
Footnotes
Conflict of Interest None.
References
- 1.Chung K C, Spilson S V. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Nesbitt K S, Failla J M, Les C. Assessment of instability factors in adult distal radius fractures. J Hand Surg Am. 2004;29(6):1128–1138. doi: 10.1016/j.jhsa.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Wilcke M K, Hammarberg H, Adolphson P Y. Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop. 2013;84(3):292–296. doi: 10.3109/17453674.2013.792035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lichtman D M, Bindra R R, Boyer M I. et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93(8):775–778. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 5.Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20(4):208–210. doi: 10.1016/0020-1383(89)90113-7. [DOI] [PubMed] [Google Scholar]
- 6.Mackenney P J, McQueen M M, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88(9):1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]
- 7.Roth K M, Blazar P E, Earp B E, Han R, Leung A. Incidence of displacement after nondisplaced distal radial fractures in adults. J Bone Joint Surg Am. 2013;95(15):1398–1402. doi: 10.2106/JBJS.L.00460. [DOI] [PubMed] [Google Scholar]
- 8.Zamzam M M, Khoshhal K I. Displaced fracture of the distal radius in children: factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br. 2005;87(6):841–843. doi: 10.1302/0301-620X.87B6.15648. [DOI] [PubMed] [Google Scholar]
- 9.Makhni E C, Ewald T J, Kelly S, Day C S. Effect of patient age on the radiographic outcomes of distal radius fractures subject to nonoperative treatment. J Hand Surg Am. 2008;33(8):1301–1308. doi: 10.1016/j.jhsa.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 10.Farah N, Nassar L, Farah Z, Schuind F. Secondary displacement of distal radius fractures treated by bridging external fixation. J Hand Surg Eur Vol. 2014;39(4):423–428. doi: 10.1177/1753193413483424. [DOI] [PubMed] [Google Scholar]
- 11.Bong M R, Egol K A, Leibman M, Koval K J. A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg Am. 2006;31(5):766–770. doi: 10.1016/j.jhsa.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Marsh J L Slongo T F Agel J et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee J Orthop Trauma 200721(10, Suppl):S1–S133. [DOI] [PubMed] [Google Scholar]
- 13.Varela C D, Vaughan T K, Carr J B, Slemmons B K. Fracture blisters: clinical and pathological aspects. J Orthop Trauma. 1993;7(5):417–427. doi: 10.1097/00005131-199310000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Halanski M, Noonan K J. Cast and splint immobilization: complications. J Am Acad Orthop Surg. 2008;16(1):30–40. doi: 10.5435/00124635-200801000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Kumar S, Penematsa S R, Sadri M, Deshmukh S C. How many clinic visits does it take to treat distal radial fractures? Int Orthop. 2008;32(1):91–96. doi: 10.1007/s00264-006-0282-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaMartina J, Jawa A, Stucken C, Merlin G, Tornetta P III. Predicting alignment after closed reduction and casting of distal radius fractures. J Hand Surg Am. 2015;40(5):934–939. doi: 10.1016/j.jhsa.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 17.Einhorn T A The science of fracture healing J Orthop Trauma 200519(10, Suppl):S4–S6. [DOI] [PubMed] [Google Scholar]
- 18.Tahririan M A, Javdan M, Nouraei M H, Dehghani M. Evaluation of instability factors in distal radius fractures. J Res Med Sci. 2013;18(10):892–896. [PMC free article] [PubMed] [Google Scholar]
- 19.Földhazy Z, Törnkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L. Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg Am. 2007;32(9):1374–1384. doi: 10.1016/j.jhsa.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 20.Jenkins N H. The unstable Colles' fracture. J Hand Surg [Br] 1989;14(2):149–154. doi: 10.1016/0266-7681_89_90116-2. [DOI] [PubMed] [Google Scholar]
- 21.Kreder H J, Hanel D P, McKee M, Jupiter J, McGillivary G, Swiontkowski M F. X-ray film measurements for healed distal radius fractures. J Hand Surg Am. 1996;21(1):31–39. doi: 10.1016/S0363-5023(96)80151-1. [DOI] [PubMed] [Google Scholar]


